Abstract
Predictive factors associated with postoperative mortality have not been extensively studied in plastic and reconstructive surgery. Neutrophil–lymphocyte ratio (NLR), a systemic inflammation index, has been shown to have a predictive value in surgery. We aimed to evaluate association between preoperative NLR and postoperative outcomes in patients undergoing plastic and reconstructive surgery. From January 2011 to July 2019, we identified 7089 consecutive adult patients undergoing plastic and reconstructive surgery. The patients were divided according to median value of preoperative NLR of 1.84. The low NLR group was composed of 3535 patients (49.9%), and 3554 patients (50.1%) were in the high NLR group. The primary outcome was mortality during the first year, and overall mortality and acute kidney injury were also compared. In further analysis, outcomes were compared according to quartile of NLR, and a receiver operating characteristic curve was constructed to estimate the threshold associated with 1-year mortality. This observational study showed that mortality during the first year after plastic and reconstructive surgery was significantly increased in the high NLR group (0.7% vs. 3.5%; hazard ratio, 4.23; 95% confidence interval, 2.69–6.63; p < 0.001), and a graded association was observed between preoperative NLR and 1-year mortality. The estimated threshold of preoperative NLR was 2.5, with an area under curve of 0.788. Preoperative NLR may be associated with 1-year mortality after plastic and reconstructive surgery. Further studies are needed to confirm our findings.
Similar content being viewed by others
Introduction
The applications of plastic and reconstructive surgery are various, and surgical procedures are complicated. On the other hand, these surgeries are generally considered relatively safe procedures with low risk of mortality. Compared to other major surgeries, the risk factors related to perioperative mortality in plastic and reconstructive surgery have not been extensively investigated1.
Neutrophil–lymphocyte ratio (NLR) is a simple index that reflects the systemic inflammatory response2. It has shown predictive value in various acute and chronic situations, including cardiovascular disease, liver cirrhosis, and cancer2,3,4,5,6,7,8. A high preoperative NLR has been reported to be associated with postoperative outcomes9. Specifically, these associations with NLR were demonstrated for mortality and acute kidney injury which could be found even after minor procedures10,11,12. However, these findings were demonstrated in limited types of surgeries, such as mortality after cardiac surgery or for recurrence after cancer resection9,13,14,15,16,17. Furthermore, neither the generalizability of the association between perioperative NLR and postoperative outcome nor the normal range of NLR for surgical patients has been fully established. Therefore, in this study, we aimed to evaluate the association between NLR and postoperative outcome in patients undergoing plastic and reconstructive surgery, a surgical subspecialty in which NLR has gained relatively less attention. In addition, we estimated the threshold of preoperative NLR level that was associated with mortality. Our findings may be helpful for clinicians to predict postoperative outcome using a simple index that can be calculated using only the results of a differential blood cell count.
Results
Baseline characteristics
From January 2011 to July 2019, a total of 7089 patients underwent plastic and reconstructive surgery and had an available preoperative NLR value. We divided the study patients into two groups according to median NLR (1.84): 3535 patients (49.9%) in the low NLR group and 3554 patients (50.1%) in the high NLR group. The patients’ baseline characteristics are summarized in Table 1. The high NLR group tended to be male and had higher creatinine level and Charlson comorbidity index score but shorter operative duration.
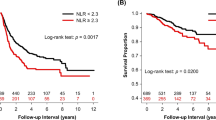
The mortality rate was 2.1% (149/7089) during the first year after surgery and 4.9% (348/7089) during the overall follow-up period. The median follow-up duration was 365 days (interquartile range: 258–365 days) for 1-year mortality and 902 days (interquartile range: 258–1717 days) during the overall follow-up period. After an adjustment, mortality during the first year was significantly higher in the high NLR group (0.7% vs. 3.5%; HR, 4.23; 95% CI 2.69–6.63; p < 0.001) (Table 2). Similar results were found for mortality during the overall follow-up period (3.0% vs. 6.8%; HR, 2.06.; 95% CI 1.64–2.60; p < 0.001) and for postoperative acute kidney injury (0.3% vs. 1.5%; OR, 3.38; 95% CI 1.74–6.59; p < 0.001) After dividing patients into four groups according to quartile of NLR, the 1-year mortalities of patients in the 3rd and 4th quartile groups were higher than those of patients in the 1st quartile group (0.5% vs. 1.1%; HR, 1.51.; 95% CI 0.02–2.23; P = 0.04 for the 3rd quartile group and 0.5% vs. 6.0%; OR, 2.30; 95% CI 1.84–2.89; p < 0.001 for the 4th quartile group) (Table 3). Survival curves are presented in Figs. 1 and 2. The subgroup analysis was conducted according to types of surgery and general anesthesia (Figs. 3 and 4), and there was no significant interaction.
The threshold for preoperative NLR associated with 1-year mortality for plastic and reconstructive surgery was estimated to be 2.5 in ROC analysis. The area under the ROC curve was 0.788; based on this value, sensitivity and specificity were 73.8% and 73.5%, respectively (Fig. 5).
Discussion
The main finding of this study was that preoperative NLR was associated with mortality and acute kidney injury after plastic and reconstructive surgery. This association showed a graded response, and the threshold of preoperative NLR level associated with 1-year mortality was estimated to be 2.5. These findings indicate that preoperative NLR may be used to predict postoperative risk in plastic and reconstructive surgery.
Although plastic and reconstructive surgeries cover a broad range of sites with various procedures, little attention has been paid to patients’ preoperative status for risk prediction because patients undergoing these surgeries are relatively healthy compared to patients undergoing other major surgeries. Previously reported perioperative factors associated with one-month mortality in plastic and reconstructive surgery include age older than 65 years, inpatient surgery, hepatorenal disease, recent chemotherapy, and partial and dependent functional status1.
Our study showed that preoperative NLR may be associated with postoperative mortality for plastic and reconstructive surgery. By reflecting systemic inflammation, preoperative NLR has consistently shown an association with postoperative mortality in many other areas of surgery9,13,14,15,16,17. In addition, this index in clinical practice is simple, inexpensive, reproducible, and readily available by routine blood cell count measurements. Several other biomarkers identified to measure systemic inflammation consume additional time and cost2, and NLR may be an adequate biomarker to predict risk in plastic and reconstructive surgery, where postoperative mortality is low. As well as mortality, NLR was associated with acute kidney injury which is a common postoperative complication12. The incidence of acute kidney injury was reported to be more common after the major surgical procedures, reflecting the relation with systemic inflammation from surgical stress12. So, our finding that NLR, an indicator of systemic inflammation, is associated with both mortality and acute kidney injury can be well explained.
The normal range of NLR has not been fully established2. In this study, we divided the patients at the median value for main analysis and according to quartile in further analyses. In the analysis using quartile values, the HR for mortality increased in a graded manner with NLR value, but the HR of the 4th quartile group was much higher than that of the other groups. So, the threshold of NLR associated with 1-year mortality was estimated. The estimated threshold was 2.5, which is lower than most of the values reported from other studies of NLR in surgical patients9,13,14,15,16,17. This may be related to the relatively fewer underlying diseases and overall good health of the patients undergoing plastic and reconstructive surgery compared to those with other surgery. Our result suggests that mild elevation of preoperative NLR may have predictive value in plastic and reconstructive surgery. However, need for a different threshold for NLR to be applied in plastic and reconstructive surgery and the clinical efficacy of correcting high preoperative NLR before surgery could not be fully answered in this study.
Our study should be appraised considering the following limitations. First, as a single-center retrospective study, our results may have been affected by confounding factors. Despite statistical adjustments, the effects of unmeasured variables could not be adjusted. Also, due to the long study period, advancements in both surgical techniques and postoperative management could have biased the results. Second, an adequate management for patients with high NLR remains unclear. A well-designed randomized trial may be needed. Despite these limitations, this is the first study to report an association between preoperative NLR and outcomes in plastic and reconstructive surgery.
In conclusion, preoperative high NLR may be associated with increased risk of acute kidney injury and mortality after plastic and reconstructive surgery. Further studies are needed for clinical application of our findings.
Materials and methods
This retrospective, observational, cohort study was approved by the institutional review board at Samsung Medical Center (SMC 2020-09-001), and the need for written informed consent was waived also by the institutional review board at Samsung Medical Center considering the minimal risk for participants and retrospective nature of the study. The research was conducted following the Declaration of Helsinki and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology guideline.
Study population and data collection
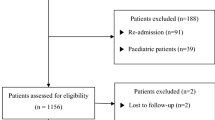
From January 2011 to July 2019, consecutive adult patients undergoing plastic and reconstructive surgery at Samsung Medical Center with an available preoperative NLR level were selected for this study. The study population was divided into two groups according to median preoperative NLR of 1.84. For further analysis, the study patients were divided according to quartile of NLR as < 1.35, < 1.84, < 2.61, and ≧ 2.61. Medical records of the study patients were curated in a deidentified form using the “Clinical Data Warehouse Darwin-C,” an electronic system in which investigators search and retrieve data from the electronic archive system containing more than 2.2 million surgeries, one billion laboratory findings, 100 million disease codes, and 200 million prescriptions. In this system, mortality data from other institutions are consistently validated and updated according to the National Population Registry of the Korea National Statistical Office. Medical records were manually reviewed by an independent investigator.
Study outcomes and definitions
The primary endpoint of this study was graft failure during a 1-year follow-up period. Secondary outcomes were mortality during overall follow-up and postoperative acute kidney injury, which was defined by the Kidney Disease: Improving Global Outcomes criteria using creatinine level18. The Charlson comorbidity index was calculated using the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10)19.
Statistical analysis
Continuous data were presented as mean ± standard deviation and compared using the t-test or the Mann–Whitney test when applicable. Differences of categorical data were compared using χ2 or Fishers exact test and presented as number and incidence. We used Cox regression analysis to evaluate the association between NLR and mortality and reported the hazard ratio (HR) with a 95% confidence interval (CI). Postoperative acute kidney injury was compared using logistic regression analysis and was reported as odds ratio (OR). The following clinically relevant variables, those with p < 0.05, were retained in the multivariable models: age, male, alcohol consumption, preoperative creatinine level, Charlson comorbidity index, operative duration, and general anesthesia. Kaplan–Meier estimates were used to construct survival curves and were compared using the log-rank test. Subgroup analyses were performed according to types of surgery and general anesthesia and presented in forest plots. We estimated the threshold of preoperative NLR to predict 1-year mortality by constructing receiver-operating characteristic (ROC) plots, and we assessed the efficacy with Pearson’s correlation coefficient. All statistical analyses were performed with SPSS 20.0 (IBM Corp., Chicago, IL). All tests were two-tailed, and p < 0.05 was considered statistically significant.
Abbreviations
- NLR:
-
Neutrophil–lymphocyte ratio
References
Fischer, J. P. et al. Predictive risk model of 30-day mortality in plastic and reconstructive surgery patients. Plast. Reconstr. Surg. 134, 156–164. https://doi.org/10.1097/PRS.0000000000000273 (2014).
Imtiaz, F. et al. Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int. Arch. Med. 5, 2. https://doi.org/10.1186/1755-7682-5-2 (2012).
Biyik, M. et al. Blood neutrophil-to-lymphocyte ratio independently predicts survival in patients with liver cirrhosis. Eur. J. Gastroenterol. Hepatol. 25, 435–441. https://doi.org/10.1097/MEG.0b013e32835c2af3 (2013).
Proctor, M. J. et al. A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br. J. Cancer 107, 695–699. https://doi.org/10.1038/bjc.2012.292 (2012).
Afari, M. E. & Bhat, T. Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: An update. Expert Rev. Cardiovasc. Ther. 14, 573–577. https://doi.org/10.1586/14779072.2016.1154788 (2016).
Liu, H. et al. Neutrophil-lymphocyte ratio: A novel predictor for short-term prognosis in acute-on-chronic hepatitis B liver failure. J. Viral Hepat. 21, 499–507. https://doi.org/10.1111/jvh.12160 (2014).
Azab, B. et al. Neutrophil-lymphocyte ratio as a predictor of adverse outcomes of acute pancreatitis. Pancreatology 11, 445–452. https://doi.org/10.1159/000331494 (2011).
Zahorec, R. Ratio of neutrophil to lymphocyte counts-rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl. Lek. Listy 102, 5–14 (2001).
Paramanathan, A., Saxena, A. & Morris, D. L. A systematic review and meta-analysis on the impact of pre-operative neutrophil lymphocyte ratio on long term outcomes after curative intent resection of solid tumours. Surg. Oncol. 23, 31–39. https://doi.org/10.1016/j.suronc.2013.12.001 (2014).
Kim, W. H., Park, J. Y., Ok, S. H., Shin, I. W. & Sohn, J. T. Association between the neutrophil/lymphocyte ratio and acute kidney injury after cardiovascular surgery: A retrospective observational study. Medicine (Baltimore) 94, e1867. https://doi.org/10.1097/MD.0000000000001867 (2015).
Fan, L. L., Wang, Y. J., Nan, C. J., Chen, Y. H. & Su, H. X. Neutrophil-lymphocyte ratio is associated with all-cause mortality among critically ill patients with acute kidney injury. Clin. Chim. Acta 490, 207–213. https://doi.org/10.1016/j.cca.2018.09.014 (2019).
Gumbert, S. D. et al. Perioperative acute kidney injury. Anesthesiology 132, 180–204. https://doi.org/10.1097/ALN.0000000000002968 (2020).
Gibson, P. H. et al. Preoperative neutrophil-lymphocyte ratio and outcome from coronary artery bypass grafting. Am. Heart J. 154, 995–1002. https://doi.org/10.1016/j.ahj.2007.06.043 (2007).
Yamanaka, T. et al. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology 73, 215–220. https://doi.org/10.1159/000127412 (2007).
Gibson, P. H. et al. Usefulness of neutrophil/lymphocyte ratio as predictor of new-onset atrial fibrillation after coronary artery bypass grafting. Am. J. Cardiol. 105, 186–191. https://doi.org/10.1016/j.amjcard.2009.09.007 (2010).
Koo, C. H. et al. Neutrophil, lymphocyte, and platelet counts and acute kidney injury after cardiovascular surgery. J. Cardiothorac. Vasc. Anesth. 32, 212–222. https://doi.org/10.1053/j.jvca.2017.08.033 (2018).
Kubo, T. et al. Impact of the perioperative neutrophil-to-lymphocyte ratio on the long-term survival following an elective resection of colorectal carcinoma. Int. J. Colorectal Dis. 29, 1091–1099. https://doi.org/10.1007/s00384-014-1964-1 (2014).
Kellum, J. A. et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2, 1–138 (2012).
Sundararajan, V. et al. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J. Clin. Epidemiol. 57, 1288–1294. https://doi.org/10.1016/j.jclinepi.2004.03.012 (2004).
Author information
Authors and Affiliations
Contributions
H.M.S., S.H.L., J.P.: conceptualization. H.M.S., S.H.L.: wrote the manuscript. A.R.O., S.K., J.K., J.G., and J.N.J.: curated the data. J.P.: supervised and revised the manuscript. All authors reviewed the manuscript and contributed to discussions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sung, H.M., Lee, SH., Oh, A.R. et al. Association between preoperative neutrophil–lymphocyte ratio and mortality after plastic and reconstructive surgery. Sci Rep 11, 21541 (2021). https://doi.org/10.1038/s41598-021-00901-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00901-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.