Abstract
Molecular subtyping of muscle-invasive bladder cancer (MIBC) predicts disease progression and treatment response. However, standard subtyping based on transcriptomic analysis is relatively expensive. This study tried to use immunohistochemistry (IHC) to subtype MIBC based on GATA3, CK20, CK5/6, and CK14 protein expression. The IHC-based subtypes in MIBC subtypes were classified as luminal (GATA3+ CK5/6−, 38.6%), basal (GATA3−CK5/6+, 12.9%), mixed (GATA3+ CK5/6+, 37.9%), and double-negative (GATA3−CK5/6−, 10.6%) in 132 MIBC patients. All individual markers and clinicopathological parameters were analyzed against treatment outcomes after radical cystectomy. The mean patient age was 65.6 years, and the male to female ratio was 6.8:1. Positive IHC expression of GATA3, CK20, CK5/6, and CK14 were 80.3%, 50.8%, 42.4%, and 28.0%, respectively. Only GATA3 and CK5/6 were significantly associated with survival outcome (p values = 0.004 and 0.02). The mixed subtype was significantly better in 5-year OS at 42.8%, whereas the double-negative subtype had the worst prognosis (5-year OS 7.14%). The double-negative subtype had a hazard ratio of 3.29 (95% CI 1.71–6.32). Subtyping using GATA3 and CK5/6 was applicable in MIBCs, and patients with the double-negative subtype were at the highest risk and may require more intensive therapy.
Similar content being viewed by others
Introduction
Urinary bladder cancer is among the top 10 most frequent cancers and one of the most common causes of cancer-related deaths in humans with an estimated 500,000 new cases and 200,000 deaths per year worldwide1,2. In Thailand, the estimated incidence of bladder cancer from 2013 to 2015 was approximately 4.0 cases/100,000 population-years3. Bladder cancer is a disease with high heterogeneity in its pathology and clinical presentation. Urothelial carcinoma accounts for more than 90% of bladder cancers4. Generally, urothelial carcinoma is categorized into non-muscle-invasive bladder cancer (NMBC) and muscle-invasive bladder cancer (MIBC) according to bladder wall invasion5. While NMBC generally has a low risk of distant metastasis and better outcomes, MIBC is more aggressive and is more likely to metastasize. MIBC usually requires intensive management, which includes radical cystectomy with perioperative chemotherapy6,7. Despite complete surgery and adjuvant therapy, the 5-year overall survival (OS) of MIBC is approximately 36%8.
MIBC has a high level of genomic instability, and TP53 mutations are the most common genetic abnormalities found in the tumor tissue9. Studies of HER2/neu, E-cadherin, p53, and p16 expression in MIBC tumor tissue using immunohistochemistry (IHC) have been reported10. However, none of these markers has been applied in clinical practice. Recently, comprehensive mRNA expression profiles in bladder cancer were used to categorize MIBC into various molecular subtypes4,11,12,13. The primary molecular subtypes of MIBC are the luminal and basal subtypes13, which are similar to the initially reported molecular breast cancer subtypes14,15. Although further studies have extended the molecular classification of MIBC into 5 or 6 subtypes16,17, the luminal and basal subtypes remain the fundamental types.
Intrinsic subtypes of bladder cancer have demonstrated increased utility in predicting treatment outcomes, especially in patients with MIBC who undergo radical cystectomy followed by adjuvant chemotherapy18. The established molecular subtypes proposed in previous studies were primarily established by high-throughput molecular technology, especially transcriptomic analysis. Traditional IHC techniques are not technology-dependent, and hence it is more feasible to classify subtypes at the protein level using IHC. Discovery of potential IHC markers that can stratify molecular subtypes of MIBC may be useful in the prediction of disease progression. Previous studies have reported a correlation between mRNA expression profiles and IHC staining results in luminal (CK20 expression) and basal (CK5/6 expression) subtypes11 and also confirmed that GATA3 and CK5/6 expression by IHC may also identify these two subtypes with greater than 90% accuracy according to a meta-analysis19. Another study revealed that the basal/squamous-like subtype was correlated with poor clinical outcome20, as was decreased GATA3 expression21. In this study, GATA3, CK20, CK5/6, and CK14 staining was selected to be tested against clinical outcomes with respect to survival after a radical cystectomy. This study aimed to determine IHC markers or patterns that may predict prognosis in patients with MIBC.
Results
Demographic and clinicopathological data
This study included 132 patients with MIBC who underwent radical cystectomy during the study period. Their mean age was 65.6 years, and the male to female ratio was 6.8:1. The demographic characteristics of the patients and immunoreactivity for each IHC marker are summarized in Table 1. Two patients who died at 3 and 7 days after surgery were considered to have operative mortality and were excluded from the survival analysis. As of January 2021, the median follow-up duration was 125 months (interquartile range 103–154 months). The median OS time was 12.2 months (interquartile range 4.7, 46.4 months), and the 5-year OS was 27.0% (95% CI 19.6%–35.0%). IHC showed positivity for GATA3, CK5/6, CK20, and CK14 with kappa value between 0.799–0.908 (93.2–96.2% agreement) (Table 2). The immunostains for GATA3, CK5/6, CK20, and CK14 showed positive results with 80.3%, 50.8%, 42.4%, and 28.0% of cases, respectively (Fig. 1). GATA3 and CK5/6 immunopositivity was significantly associated with OS by log-rank analysis (Table 1). Twenty-six cases received a median of 3 cycles of adjuvant chemotherapy. GATA3 expression was significantly inversely correlated with pT stage progression.
According to the Kaplan–Meier survival analysis, significant differences in outcomes with respect to OS were demonstrated among cases with positive GATA3 staining (p = 0.008) and in cases with positive CK5/6 staining (p = 0.038). The other markers did not show significant prognostication value for survival. The Kaplan–Meier survival curves for GATA3, CK5/6, CK14, and CK20 are depicted in Fig. 2.
The correlation between each individual marker was evaluated by Pearson correlation test. As showed in Table 2, the significant association of GATA3, CK5/6, and CK20 was found only in pathological stage 1 of patients. When the correlation between markers in the basal and luminal subtypes was assessed, moderate correlation was observed between GATA3 and CK20 expression, which indicated that the basal-like subtype was demonstrated by Pearson correlation at 0.46 (p = 0.022). The analysis showed small correlation between the luminal-like subtype markers, CK5/6 and CK14; 0.31 (p = 0.048) (Fig. 3).
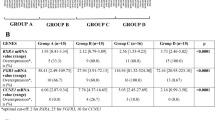
As GATA3 and CK5/6 were the only two markers representing different subtypes that were significantly associated with survival, we elected to categorize our cases into four groups according to those two markers: luminal-like (GATA3+ and CK5/6−), basal-like (GATA3− and CK5/6+), mixed (GATA3+ and CK5/6+), and double-negative (GATA3− and CK5/6−) subtypes. By this definition, the luminal-like, basal-like, mixed, and double-negative subtypes were observed in 38.6%, 12.9%, 37.9%, and 10.6% of cases, respectively. Associations between each subtype and clinicopathological factors including survival outcomes are displayed in Table 3. The double-negative subtype was significantly associated with higher incidence of pT4 disease.
CK20 immunopositivity, a marker of the luminal molecular subtype, was significantly associated with the GATA3-defined luminal subtype (p < 0.01), whereas CK14 positivity was significantly associated with the CK5/6-defined basal subtype (p < 0.01). In the 50 mixed subtype (GATA3+ and CK2/5+) cases in this study, an equal number of cases with CK20 and CK5/6 positivity was found (Table 3).
When clinicopathological parameters and IHC subtypes were analyzed against survival in a univariable Cox hazard model, tumor stage (pT and N), lymphovascular invasion, pathologic grade, loss of GATA3 immunoreactivity, and loss of CK5/6 immunoreactivity were significantly associated with poorer survival outcomes. Considering subtyping, while patients with the mixed subtype had the lowest risk, which was followed by patients with the luminal-like and basal-like subtypes, those with the double-negative subtype had the highest crude HR. In the multivariable analysis by stepwise Cox hazard regression, N stage (N > 0) and the double-negative subtype were significantly associated with higher risk (model p = 0.0001) (Table 4).
Association between molecular subtypes and survival outcomes
Kaplan–Meier curves compare the survival probability of 132 patients with MIBC following radical surgery (Fig. 4). The 5-year OS rates of patients with the mixed, basal, luminal, and double-negative subtypes were 42.5% (95% CI 28.9–56.1%), 23.5% (7.3–44.9%), 18.9% (9.2–31.1%), and 7.1% (0.4–27.5%), respectively.
In the 50 MIBCs of mixed subtype (GATA3+ and CK5/6+), if CK20 and CK14 were added to the subcategorization criteria, which means that mixed subtype cases with positive CK20 were reclassified as luminal, whereas mixed subtype cases with positive CK14 were reclassified as basal. The univariable hazard model did not improve. Using the mixed subtype as a reference, the HRs (and 95% CIs) for the luminal, basal, and double-negative subtypes were 1.17 (95% CI 0.62–2.20), 1.54 (0.76–3.10), and 2.64 (1.22–5.73) respectively.
Discussion
The molecular subtyping of bladder cancer represents disease heterogeneity. Previous gene expression profiling has revealed that MIBCs can be subcategorized into at least three intrinsic subtypes including the luminal, basal, and double-negative subtypes22. The characteristics of luminal tumors include high expression of markers (GATA3, CK20, and uroplakin 2) of terminally differentiated urothelial cells, which are also known as umbrella cells13. As umbrella cells have shorter longevity than basal cells, they are less susceptible to genomic alterations but usually exhibit greater changes in their chromatin landscape. Basal-like bladder cancer cells express biomarkers of mesenchymal stem cells (CK5/6 and CK14) and exhibit some squamous and sarcomatous features in tumor tissue23. Recent studies have suggested that GATA3 and CK5/6 expression can identify molecular subtypes in 80–90% of cases19,22. In our study, 62% of cases could be clearly categorized into luminal, basal, or double-negative subtypes based on GATA3 and CK5/6 expression, and only these two markers were associated with survival outcome. Loss of expression of either GATA3 or CK5/6 was associated with poorer survival probability, whereas loss of expression of both markers was a strong predictor of poor outcome. Although a significant association was observed between CK20 and GATA3 expression and between CK14 and CK5/6 expression, the addition of CK20 and CK14 to the criteria to categorize the subtypes did not appear to improve survival prediction.
MIBCs expressing GATA3 exhibited less aggressive characteristics and were associated with significantly better survival. GATA3, also known as GATA3 binding protein, is a transcription factor that regulates the expression of genes that function in the luminal differentiation of breast and urothelial epithelium24,25. In addition, GATA3 is expressed in T-lymphocytes, the central nervous system, and erythrocytes26. In breast cancers, reduced GATA3 expression was reported in the triple-negative subtype27. In urothelial cell line models, the loss of GATA3 expression promoted tumor cell migration and invasion via upregulation of oncogenes28,29. Several clinical studies of GATA3 in bladder cancer have been conducted30,31,32. Loss of GATA3 expression was associated with high-grade cancer32, and patients with GATA3-negative bladder cancer had poorer survival outcomes in most studies30,31,33. Taken together, those reports and our data demonstrate that GATA3 is a promising biomarker of MIBC. Another luminal marker evaluated in this study, CK20, has been reported to be correlated with higher tumor grade and stage in papillary urothelial carcinoma34. However, our study did not reveal a significant association between CK20 and any clinicopathological factor or survival outcome.
CK5/6 is a cytokeratin expressed in a squamous epithelial lineage and is generally used as a marker of squamous differentiation, which indicates the basal subtype35. Expression of CK5/6 in urothelial carcinoma was associated with poorer survival in several reports35,36. In contrast, some reports also demonstrated that loss of CK5/6 expression was associated with decreased survival probability in patients with transitional cell carcinoma of the upper urinary tract36,37. In our study, loss of CK5/6 expression was associated with significantly worse survival outcome. CK14 is another marker of the basal subtype, and its expression has been reported to be negatively correlated with survival in MIBC.
Although molecular subtyping has been accepted for its correlation with disease progression and treatment outcome in MIBC, RNA expression profiling is not a widely available technology. The evaluation of IHC panels for intrinsic subtype categorization of MIBC has been reported in several studies31,36,38. However, except for GATA3, the prognostic value of other IHC markers has remained intriguing. Variation in staining techniques and interpretation may partly explain the disparity in results. Since our study revealed significant associations between survival and GATA3 and CK5/6 expression, these markers were combined in a simple subgroup as luminal when the tumor had exclusive expression of GATA3 and as basal for exclusive CK5/6 expression. Our study also found that the double-negative subtype, which is indicated by negative staining of both markers, predicted the poorest outcome. Other combinations that have been reported in previous studies, such as CK20 with CK5/6 or CK20 with CK14, have been investigated with no interesting findings.
The limitations of our study included the small sample size and the lack of gene expression profiling to validate concordance between molecular subtypes and IHC marker expression. However, the transcriptomic profiling study using the markers from this study as a part of clustering is running and will be launched in the next year. In addition, only 20% of our patients received chemotherapy after radical cystectomy because the physical status of most patients did not allow for chemotherapy. As neoadjuvant chemotherapy is becoming a new trend in MIBC treatment, the results of our study may help in the selection of patients at a high risk for treatment failure who should receive upfront chemotherapy before definitive surgery.
Methods
Patients and specimens
This study included 132 patients with urinary bladder cancer who underwent radical cystectomy and who received standard adjuvant chemotherapy at Songklanagarind Hospital, Thailand from 2008 to 2016. Inclusion criteria were patients with bladder cancer aged older than 15 years who underwent surgery primarily at our institute and who completed adjuvant treatment according to the standard of the Thai Urological Association8. All eligible cases were reviewed for clinical stage, and their histopathology was confirmed by a pathologist who specializes in genitourinary tract pathology (KK). Staging was performed according to the TNM classification, whereas stage grouping was performed according to the eighth version of the American Joint Committee on Cancer Staging Manual. Cases without muscularis propria invasion and those with subtypes other than non-urothelial carcinoma were excluded. Clinical data were extracted from the electronic medical records of the hospital (HIS system). Data on survival status combined with the clinical follow-up records and death registry data from the Thai citizen registration system were analyzed and archived by the Cancer Unit, Songklanagarind Hospital. Cases with operative mortality were excluded from the survival analysis. The study protocol was approved by the Human Research Ethic Committee of the Faculty of Medicine, Prince of Songkla University (REC61-222-10-1). All methods were carried out in accordance with the World Medical Association Declaration of Helsinki. Informed consent was obtained from all patients or legally authorized representatives included in the study.
IHC study by tissue microarray
Sampling of the tumor part for this pilot study was performed by a collaborative work between the attending surgeon who know the orientation of the specimen and the pathologist who examined the histopathology. Bladder carcinoma in situ and flat lesions were excluded in this study. Several areas of tumor in the same patients for the pathological morphology and selected the representative areas that have both richness in tumor cells and the morphology was like other areas in the same cases were selected for examination. Archived pathological specimens from all included cases were retrieved as formalin-fixed paraffin-embedded tissue blocks, which were then selected and prepared as 5-μm sections for a tissue microarray (TMA) using a tissue arrayer (Beecher Instruments, Silver Spring, MD, USA). Immunostaining procedures were conducted with 3 (triplicate) TMA cores per section by a pathology technician who specializes in this technique. In cases of multiple foci, all foci were selected for examinations. Subtype-specific primary antibodies used here are as follows: GATA3 (UMAB218, 1:100 dilution; OriGene, MD, USA), CK5/6 (D5/16, 1:50 dilution; Dako, Glostrup, Denmark), CK14 (OIT4A7, 1:100 dilution; OriGene), and CK20 (OTI4A, 21:50 dilution; OriGene). These antibodies were used to identify potential markers to establish molecular subtypes in the tissue sections contained in the TMA. A pathologist (KK) blinded to the clinical outcomes examined the results using a light microscope and scored all TMA sections. For mixed and/or borderline cases, the positive immunostains were interpreted especially by the consensus of two pathologists. The positivity and intensity of tumor cell nuclei stained for GATA3 and membranous or cytoplasmic staining for CK20, CK5/6, and CK14 were recorded. Staining intensity was assessed as 0 (negative; 0–10%) or 1 (positive; 10–100%).
Statistical analysis
Categorical and continuous parameters were compared using the Chi-square test and were analyzed using the Spearman rank correlation test. The median differences between groups for non-normally distributed variables were evaluated by independent sample Kruskal–Wallis test. Differences in the percentages of IHC staining between or among comparable groups were analyzed using the Student’s t test and one-way analysis of variance. The hazard ratios (HRs) and 95% confidence intervals (CIs) were also calculated. In all patients who underwent radical cystectomy with adjuvant chemotherapy, the OS after radical cystectomy was calculated using the Kaplan–Meier method. Survival probabilities were estimated using the Kaplan–Meier method, whereas the log-rank test was adopted to compare survival probabilities between each variable. All variables with p ≤ 0.1 in the univariable analyses were entered into the multivariable regression analysis. Multivariable analyses were also performed using Cox regression. Two-sided p values < 0.05 were considered statistically significant. The R program (version 4.0.1) was used for statistical analyses.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 69, 7–34 (2019).
Lenis, A. T., Lec, P. M., Chamie, K. & Mshs, M. D. Bladder cancer: A review. JAMA 324, 1980–1991 (2020).
Imsamran, W. et al. Cancer in Thailand VIII, 2010–2012 (New Thammada Press, 2015).
Sjödahl, G. et al. A molecular taxonomy for urothelial carcinoma. Clin. Cancer Res. 18, 3377–3386 (2012).
McConkey, D. J. & Choi, W. Molecular subtypes of bladder cancer. Curr. Oncol. Rep. 20, 77 (2018).
Gakis, G. Management of muscle-invasive bladder cancer in the 2020s: Challenges and perspectives. Eur. Urol. Focus 6, 632–638 (2020).
Flaig, T. W. et al. Bladder cancer, version 3.2020, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 18, 329–354 (2020).
Bejrananda, T., Pripatnanont, C., Tanthanuch, M. & Karnjanawanichkul, W. Oncological outcomes of radical cystectomy for transitional cell carcinoma of bladder. J. Med. Assoc. Thai. 100, 24–32 (2017).
Lindgren, D. et al. Combined gene expression and genomic profiling define two intrinsic molecular subtypes of urothelial carcinoma and gene signatures for molecular grading and outcome. Cancer Res. 70, 3463–3472 (2010).
Netto, G. J. & Cheng, L. Emerging critical role of molecular testing in diagnostic genitourinary pathology. Arch. Pathol. Lab. Med. 136, 372–390 (2012).
Choi, W. et al. Identification of distinct basal and luminal subtypes of muscle-invasive bladder cancer with different sensitivities to frontline chemotherapy. Cancer Cell 25, 152–165 (2014).
Cancer Genome Atlas Research Network. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature 507, 315–322 (2014).
Damrauer, J. S. et al. Intrinsic subtypes of high-grade bladder cancer reflect the hallmarks of breast cancer biology. Proc. Natl. Acad. Sci. USA 111, 3110–3115 (2014).
Sørlie, T. et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc. Natl. Acad. Sci. USA 98, 10869–10874 (2001).
Perou, C. M. et al. Molecular portraits of human breast tumours. Nature 406, 747–752 (2000).
Fishbein, L. et al. Comprehensive molecular characterization of pheochromocytoma and paraganglioma. Cancer Cell 31, 181–193 (2017).
Robertson, A. G. et al. Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell 174, 1033 (2018).
Kojima, T., Kawai, K., Miyazaki, J. & Nishiyama, H. Biomarkers for precision medicine in bladder cancer. Int. J. Clin. Oncol. 22, 207–213 (2017).
Dadhania, V. et al. Meta-analysis of the luminal and basal subtypes of bladder cancer and the identification of signature immunohistochemical markers for clinical use. EBioMedicine 12, 105–117 (2016).
Lerner, S. P. et al. Bladder cancer molecular taxonomy: Summary from a consensus meeting. Bladder Cancer 2, 37–47 (2016).
Miyamoto, H. et al. GATA binding protein 3 is down-regulated in bladder cancer yet strong expression is an independent predictor of poor prognosis in invasive tumor. Hum. Pathol. 43, 2033–2040 (2012).
Guo, C. C. et al. Assessment of luminal and basal phenotypes in bladder cancer. Sci. Rep. 10, 9743 (2020).
Blaveri, E. et al. Bladder cancer stage and outcome by array-based comparative genomic hybridization. Clin. Cancer Res. 11, 7012–7022 (2005).
Miettinen, M. et al. GATA3: A multispecific but potentially useful marker in surgical pathology: A systematic analysis of 2500 epithelial and nonepithelial tumors. Am. J. Surg. Pathol. 38, 13–22 (2014).
Liu, H., Shi, J., Wilkerson, M. L. & Lin, F. Immunohistochemical evaluation of GATA3 expression in tumors and normal tissues: A useful immunomarker for breast and urothelial carcinomas. Am. J. Clin. Pathol. 138, 57–64 (2012).
Lentjes, M. H. F. M. et al. The emerging role of GATA transcription factors in development and disease. Expert Rev. Mol. Med. 18, e3 (2016).
Cimino-Mathews, A. et al. GATA3 expression in breast carcinoma: Utility in triple-negative, sarcomatoid, and metastatic carcinomas. Hum. Pathol. 44, 1341–1349 (2013).
Li, Y. et al. GATA3 in the urinary bladder: Suppression of neoplastic transformation and down-regulation by androgens. Am. J. Cancer Res. 4, 461–473 (2014).
Li, Y. et al. Loss of GATA3 in bladder cancer promotes cell migration and invasion. Cancer Biol. Ther. 15, 428–435 (2014).
Jangir, H. et al. Prognostic stratification of muscle invasive urothelial carcinomas using limited immunohistochemical panel of Gata3 and cytokeratins 5/6, 14 and 20. Ann Diagn Pathol 43, 151397 (2019).
Wang, C.-C., Tsai, Y.-C. & Jeng, Y.-M. Biological significance of GATA3, cytokeratin 20, cytokeratin 5/6 and p53 expression in muscle-invasive bladder cancer. PLoS ONE 14, e0221785 (2019).
Naik, M. et al. GATA-3 expression in all grades and different variants of primary and metastatic urothelial carcinoma. Indian J. Surg. Oncol. 12, 72–78 (2021).
Kamel, N. A., Abdelzaher, E., Elgebaly, O. & Ibrahim, S. A. Reduced expression of GATA3 predicts progression in non-muscle invasive urothelial carcinoma of the urinary bladder. J. Histotechnol. 43, 21–28 (2020).
Desai, S. et al. Relationship of cytokeratin 20 and CD44 protein expression with WHO/ISUP grade in pTa and pT1 papillary urothelial neoplasia. Mod. Pathol. 13, 1315–1323 (2000).
Hashmi, A. A. et al. Cytokeratin 5/6 expression in bladder cancer: Association with clinicopathologic parameters and prognosis. BMC Res. Notes 11, 207 (2018).
Calvete, J. et al. The coexpression of fibroblast activation protein (FAP) and basal-type markers (CK 5/6 and CD44) predicts prognosis in high-grade invasive urothelial carcinoma of the bladder. Hum. Pathol. 91, 61–68 (2019).
Langner, C., Wegscheider, B. J., Rehak, P., Ratschek, M. & Zigeuner, R. Prognostic value of keratin subtyping in transitional cell carcinoma of the upper urinary tract. Virchows Arch. 445, 442–448 (2004).
Akhtar, M., Rashid, S., Gashir, M. B., Taha, N. M. & Al Bozom, I. CK20 and CK5/6 immunohistochemical staining of urothelial neoplasms: A perspective. Adv. Urol. 2020, e4920236 (2020).
Acknowledgements
We thank Mrs. Thitapa Khanarak and Ms. Kanda Tongmitr from the Department of Pathology for their assistance in tissue microarray preparation and immunohistochemistry techniques.
Funding
The study was supported by a grant-in-aid from the Health Systems Research Institute and the Faculty of Medicine, Prince of Songkla University.
Author information
Authors and Affiliations
Contributions
T.B. designed the study; T.B., K.K., and S.S. analyzed the data; T.B., J.S., and S.S. drafted and revised the paper; T.B., and J.S. draw figures; all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bejrananda, T., Kanjanapradit, K., Saetang, J. et al. Impact of immunohistochemistry-based subtyping of GATA3, CK20, CK5/6, and CK14 expression on survival after radical cystectomy for muscle-invasive bladder cancer. Sci Rep 11, 21186 (2021). https://doi.org/10.1038/s41598-021-00628-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00628-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.