Abstract
Our study evaluated the association between Demodex infestation and recurrent hordeola and examined the clinical features associated with these eyelid lesions. This was an observational, comparative study. We reviewed 250 patients and divided them into the recurrent hordeolum (n = 153) and control (n = 97) groups. Demodex infestation was detected by epilating eyelashes around the lesion/s and viewing them under a light microscope. Patient medical records and photographs were retrospectively analyzed to identify the clinical characteristics of Demodex-associated recurrent hordeola. Demodex was detected in 91 (59.5%) and 17 (17.5%) patients in the recurrent hordeolum and control groups (p < 0.001), respectively. In the recurrent hordeolum group, Demodex mites were found in 74 (68.5%) and 17 (37.8%) of the adult and pediatric patients (p < 0.001), respectively. Among patients with recurrent hordeola, patients in their 20s were most likely to have concomitant Demodex infestation. Patients with Demodex infestations were also more likely to develop recurrent lesions within a shorter period of time from the primary incision and curettage. The most common presentation of Demodex-associated recurrent lesions was external hordeola (67%) (p = 0.002). Demodex infestation may cause recurrent hordeola in adults and children. These mites may play a greater role in the development of lesions in adult patients. The strongest association between Demodex infestation and recurrent lesions was seen in patients in their 20s. Our results suggest that if the hordeola recur within a short period of time with the clinical characteristics of external location of eyelid, multiple numbers of lesions, or anterior blepharitis, eyelash epilation should be performed to identify the presence of Demodex mites.
Similar content being viewed by others
Introduction
Demodex mites are normal inhabitants of the pilosebaceous unit and considered part of the normal skin flora1. Recent studies have reported that ocular demodicidosis, which is considered be a new type of blepharitis is a potential risk factor for chalazia2,3,4,5. In particular, recent studies by Yam and Liang reported that Demodex infestation is associated with chalazion recurrence2,3. However, Liang’s study did not include patients in the acute stage, which may be a limitation in presenting the exact clinical characteristics of chalazion recurrence. Although sufficient medication may have been administered and surgical removal performed, chalazion or hordeolum recurrence in a relatively short period of time is embarrassing for ophthalmologists. However, the treatment of these patients may be relatively easy if ophthalmologists are aware of the clinical features of recurrent Demodex infestations. The medical and surgical treatment of mite-associated chalazion and/or hordeolum cannot prevent their recurrence; however, tea tree oil (TTO), Terpinen-4-ol, 4% pilocarpine gel, and systemic ivermectin have been advocated as the primary treatment for patients with Demodex blepharitis6,7. We conducted an observational, comparative study to examine the association between Demodex infestations and recurrent hordeola and a retrospective review of the medial records and photographs of patients with recurrent lesions to identify the clinical features of these lesions.
Methods
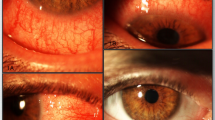
This was an observational, comparative study. The study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board and Ethics Committee of the HanGil Eye Hospital (HanGil IRB-17008). The same review board waived the requirement for written informed consent, but the representative patients whose photographs were included in this manuscript provided written informed consent (Fig. 1). In total, 250 patients who underwent light microscopic examination to detect Demodex infestation between July 2015 to March 2021 were analyzed.
Patient photographs of Demodex-associated recurrent hordeola. A 54-year-old man (A,B), 21-year-old man (C,D), and 63-year-old-woman (E,F) demonstrate external hordeola (arrows), which recurred after a short period of time following incision and curettage. All of these patients had Demodex mites on the cilia surrounding the lesions.
Recurrence was defined as a focal inflamed lesion occurring on the same or another site of the eyelid within 3 months after incision and curettage of the primary lesion. Incision and curettage of the primary lesions was performed by a single surgeon (SC KIM). Postoperatively, all patients received oral antibiotics (amoxicillin hydrate and clavulanate) thrice daily, combined steroid (Fluorometholone 0.1%, Santen Pharmaceutical Korea Co., Ltd.) and antibiotics (Cravit®, Levofloxacin 0.5%, Santen Pharmaceutical Korea Co., Ltd.) eyedrops four times daily, and an antibiotic ointment (Tarivid®, Ofloxain 0.3%, Santen Pharmaceutical Korea Co., Ltd.) thrice daily for 2 weeks on skin, if transcutaneous incision was done. The group with recurrent lesions (n = 153) were analyzed as adult (≥ 15-years, n = 108) and pediatric (< 15-years, n = 45) patients. We analyzed the lesions according to age because Demodex infestations have been demonstrated to increase with age3. The control group (n = 97) consisted of patients who showed no evidence of focal inflammation on slit microscopic examination, underwent lid surgeries, such as blepharoplasty, entropion repair, epiblepharon repair, and congenital ptosis repair, and lacrimal procedures, for example, dacryocystorhinostomy for acquired and congenital lacrimal duct obstruction, were included (Table 1). Patients with acute conjunctivitis and keratitis and those taking topical or systemic immunosuppressants when hordeolum recurrence was confirmed were excluded. We also excluded patients with any other types of dermatoses such as rosacea, periocular dermatitis, and discoid lupus erythematosus due to their known strong association with Demodex infestation.
Patient medical records and photographs were examined retrospectively to identify the clinical characteristics of recurrent lesions and classified according to the presence of Demodex mites (Table 2). We examined the lid margin to check for (1) signs of blepharitis, such as margin hyperemia, scaling, crusting, and margin hypertrophy; (2) differentiating features, such as involvement of the lid margin in external hordeola, involvement of the tarsal plate in internal hordeola, and the presence of firm, painless tarsal plate lesions in chalazia; and (3) location and number of the lesions.
To evaluate for the presence of Demodex mites, we epilated approximately 10 eyelashes around the lesions in the recurrent lesion group. Lash sampling in the pediatric group was performed under general anesthesia prior to surgery. The epilated lashes were placed on a slide glass, moistened with a drop of normal saline, sealed with a cover glass, and observed under a light microscope (Olympus®, Tokyo, Japan) (Fig. 2). Demodex was considered as present if at least one Demodex mite was identified on microscopic examination, whether it was alive or not. Additionally, in the 19 recurrent patients, Demodex counting was performed by an independent doctor who had no knowledge of each patient’s clinical information.
Statistical analyses were performed using SPSS for Windows version 25.0 (SPSS Inc., Chicago, Illinois, USA). The chi-square test was used to compare the proportion of Demodex mites between adult and pediatric patients in each group. Odds ratios were used to compare between the groups. All values were presented as means ± standard deviations. A p-value < 0.05 was considered as statistically significant.
Results
This study examined 153 patients with recurrent hordeola and 97 patients as controls. The recurrent hordeolum group included 108 and 45 adult and pediatric patients, respectively, whereas the control group included 66 and 31 adult and pediatric patients, respectively. In the recurrent hordeolum group, the mean ages of the adult and pediatric patients were 36.03 ± 14.99-years (range, 14–66 years) and 4.98 ± 2.86 years (range, 1–13 years), respectively. In the control group, the mean ages of the adult and pediatric patients were 46.82 ± 18.15-years (range, 14–75 years) and 4.90 ± 2.73-years (range, 1–10 years), respectively (Table 1).
Demodex was detected in 91 (59.5%) and 17 (17.5%) patients in the recurrent hordeolum and control groups, respectively; the difference was statistically significant (p < 0.001) (Table 1). When the recurrent hordeolum group was analyzed according to age, Demodex was detected in 74 (68.5%) and 17 (37.8%) of the adult and pediatric patients, respectively; Demodex was significantly more prevalent in adult patients (p < 0.05). The number of mites was counted in 19 recurrent patients, and 1–15 mites were found in 15 patients (14 adults, 1 pediatric patient). In contrast, in the control group, Demodex was detected in 14 (21.2%) and 3 (9.7%) of the adult and pediatric patients, respectively. The rate of Demodex detection was significantly higher among adult patients than among pediatric patients in the recurrent hordeolum group than in the control group (padult < 0.001, ppediatric = 0.006) (Fig. 3).
Recurrent hordeola were the most common in patients aged < 10 years, but Demodex mites were most frequently observed (84.4%) among patients in their 20s in the recurrent hordeolum group (Fig. 4). Among the patients with Demodex infestations, two-thirds of the recurrent eyelid lesions were characterized by focal inflammation of the lid margin such as external hordeola, whereas one-third were deep, roundish inflammatory lesions in the tarsal plate such as internal hordeola. The majority of patients (80.2%) in the Demodex group also had anterior blepharitis; anterior blepharitis was more common in the Demodex group than in the control group. Recurrent lesions were more likely to be located in the upper eyelid (57.1%) than in the lower eyelid (32.9%). Eyelids with Demodex infestations were significantly more likely to have more than one hordeolum than those without Demodex infestation (p = 0.008). Among adult patients with recurrent hordeola and Demodex infestations, the interval period between the primary incision and curettage and lesion recurrence was shorter (8.02 ± 5.42 weeks) than among patients without Demodex infestations (12.31 ± 7.05 weeks). In contrast, the interval period in pediatric patients, while also short, demonstrated no significant difference with or without Demodex infestation (Table 3). Our results suggested that Demodex infestation plays a more important role in hordeolum recurrence in adult eyelids than in pediatric eyelids.
Age-specific distribution of recurrent hordeola and Demodex infestation. The graph demonstrates the highest frequency of hordeolum recurrence in patients aged < 10 years (A); however, patients in their 20s with recurrent hordeola had the highest case number of Demodex infestation (B) and the highest Demodex infestation rate (84.4%) (C) among the various age groups.
Discussion
Internal and external hordeola are infections of the internal meibomian glands and external glands of Zeis and/or Moll, respectively, whereas chalazia are chronic lipogranulomatous inflammatory lesions that develop secondary to blockage of the meibomian gland orifices or stagnation of sebaceous secretions8. It is often challenging to distinguish between a chalazion and an internal hordeolum during the acute inflammatory phase of the chalazia9. Blepharitis, acne rosacea, trichiasis, and cicatricial ectropion have been found to be associated with internal hordeola10,11,12. In children, immunodeficiency, malnutrition, and vitamin A deficiency have been reported to be associated with chalazia13,14. A recurrent hordeolum usually occurs when the treatment fails to eliminate the bacteria that are present, completely and rarely is it due to a new infection15. Recurrent lesions should be assessed for the clinical features of malignancy, such as the presence of ulceration, telangiectatic vessels, or irregular or indistinct borders.
Demodex mites are normal inhabitants of human hair follicles and considered part of the normal flora of the pilosebaceous unit1. There are many species of Demodex, but only Demodex folliculorum and D. brevis are found in the human body16. D. folliculorum inhabits the eyelash hair follicles, whereas D. brevis lives deep within the meibomian glands17.
The prevalence of Demodex increases in older individuals, as well as in malnourished or immunosuppressed patients18,19. Several studies have shown that Demodex infestation is closely related to blepharitis; blepharitis has been identified as a major risk factor for chalazia5,19,20. Yam et al. demonstrated that 72.9% of adults with recurrent chalazia also had Demodex infestations2. Liang et al. reported that 69.2% of patients with chronic chalazia had Demodex infestations3. Schear et al. conducted a histopathologic study of eyelids with chalazia and reported that the average mite count per specimen was significantly higher than that in controls21. We found that Demodex was more prevalent among adult and pediatric patients (padult < 0.001, ppediatric = 0.006) in the recurrent hordeolum group than in the control group (Table 1). This suggested that Demodex infestation has a potential pathogenic role in the development of recurrent hordeola in adult and pediatric patients.
Our study also found that recurrent eyelid lesions associated with Demodex infestations mostly showed external hordeolum (67%), while the rest looked like internal hordeola (23%) (Table 2). This means that Demodex-related lesions were more likely to involve the anterior lamella of the eyelid.
Recurrent hordeola developed after primary incision and curettage at shorter time intervals in the Demodex group than in the group without Demodex (Table 3), which indicated that Demodex infestation may be the most significant factor in the pathogenesis of hordeolum recurrence.
The pathophysiology of Demodex-associated eyelid lesions remains unclear; these lesions are believed to develop as an inflammatory foreign body granulomatous reaction to the chitinous exoskeleton of Demodex mites22. Mechanical obstruction of the meibomian glands results in a vicious cycle that contributes to Demodex overgrowth2,3,20,23. The Demodex mites also consume the epithelial cells of the eyelids, which induces micro-abrasions, epithelial hyperplasia, and reactive hyper-keratinization around the base of the lashes, forming cylindrical dandruff17. Demodex mites may also act as vectors for other pathogenic organisms that promote meibomian gland infection3,23. Overall, Demodex infestation can cause chronic blepharitis, conjunctival inflammation, and meibomian gland dysfunction. In addition, Demodex mites can penetrate the dermis and cause dermatological diseases, such as acne, rosacea, and folliculitis24,25.
Demodex infestation increases with age, and the mites are rarely found in newborns or children19,26,27. Arzola et al. reported that Demodex mites are observed in 64%, 75%, and 100% of patients belonging to 76–85-years, 86–95-years, and over 95-years of age groups, respectively. In contrast, only 11% of patients between 15 and 25-years of age demonstrated Demodex mites upon inspection28. In our study, the positivity rates for Demodex infestation in adult and pediatric patients with recurrent hordeola were 68.5% and 37.8%, respectively (Table 1). Demodex infestation in the recurrent hordeolum group was significantly more prevalent in adults than in children (p < 0.001) (Fig. 3). In the control group, the prevalence of Demodex showed no significant difference between adults and children (p = 0.123). Our data demonstrated that Demodex mites play a greater role in the development of recurrent lesions in adults than in children and may be due to an age-related difference in the Demodex infestation rate26,27. The maturity of the pilosebaceous unit may also be a factor29,30,31,32. Studies have reported that while sebum secretion in children is typically low, it reaches maximal rates at approximately 20-years of age29,30,31 and then, declines steadily, thereafter32. The low sebum secretion in children may provide poor environments for Demodex infestations. We also noted that the highest frequency of recurrent hordeola was observed in patients < 10 years of age (Fig. 4A); however, patients in their 20s with recurrent hordeola were the most likely group to have the highest concomitant Demodex infestation rate (84.4%) as well as the highest case number of Demodex infections among the overall enrolled recurrent hordeolum group (Fig. 4B,C). Moreover, the Demodex infestation rate in patients aged < 10 years with recurrent hordeola was 37.5% (Fig. 4C). These data suggest that the etiology of recurrent hordeola in the < 10 years age group could be related to factors other than Demodex infestation, and that the abundant sebum secretion rate which has been reported to be highest around 20 years of age31 or between 15 and 35 years of age32 may play an important role in Demodex survival in the 20s group.
TTO, Terpinen-4-ol, 4% pilocarpine gel, and systemic ivermectin have been advocated as the primary treatment for patients with Demodex blepharitis6. TTO is a natural essential oil that is steam-distilled from the leaf of Melaleuca alternifolia. It is an aboriginal, traditional, Australian medication that treats wounds and cutaneous infections and has antibacterial, antifungal, anti-inflammatory, and acaricidal properties33. Gao et al. evaluated the efficacy of various concentrations of TTO and other agents in eradicating Demodex mites33,34,35. Pure 100% concentrations of TTO, alcohol, dill weed oil, and caraway oil all demonstrated strong anti-Demodex effects, but these treatments had limited clinical use because of corneal toxicity and irritation. As such, lid scrub daily with tea tree shampoo and weekly application of 50% TTO is currently recommended for the eradication of ocular Demodex mites33,34,35. TTO is thought to work by washing out Demodex mites emerging from the cilia before they can mate and providing a sterilizing effect through its anti-cholinesterase activity33,36. Yam et al. noted that lid scrubs reduced chalazion recurrence by 96.8%2. In contrast, Koo et al. examined patients with Demodex blepharitis who were treated twice-daily with 10% TTO and once-weekly with 50% TTO lid scrubs in a clinical setting over 4 weeks. Their study reported a low Demodex eradication rate of 23.6%7.
This study has several limitations. First, we instilled a drop of saline on the epilated eyelashes when we mounted the specimens on the glass slide. This could have resulted in the underdiagnosis of Demodex infestations. Saline is also unable to dissolve cylindrical dandruffs, which can hide Demodex and allow them to remain in the follicle instead of taken along with the epilated eyelash. This can also reduce the total number of mites reported. Second, we did not analyze Demodex mites according to their species (folliculorum vs. brevis), which was done in previous studies, because we believed that identifying the species does not change the final treatment. Third, we did not count the mites in all study patients but only in 19 recurrent patients and found that there were 1–15 mites in 15 patients (14 adults, 1 pediatric patient). Therefore, while the cut-off level could not be exactly calculated between normal Demodex flora and demodicosis, we demonstrated a significant association between Demodex infestation and recurrent hordeola in the Demodex group compared to in the control group.
In this present study, we identified cases where the hordeola was associated with the clinical characteristics of external location, multiple numbers of lesions, or anterior blepharitis, without any signs of malignancy, but with recurrence within a short period of time despite the use of conservative treatment, and recommended that eyelash epilation be performed to identify the presence of Demodex mite. Alternately, eyelashes around recurrent hordeola should be observed carefully to identify Demodex migration or the presence of cylindrical dandruff at the base of eyelash because it is considered as the pathognomonic of Demodex infestation. In addition, we believe that further studies are required to determine the efficacy of eyelid cleansers for Demodex-associated recurrent eyelid lesions.
References
Elston, C. A. & Elston, D. M. Demodex mites. Clin. Dermatol. 32(6), 739–743 (2014).
Yam, J. C., Tang, B. S., Chan, T. M. & Cheng, A. C. Ocular demodicidosis as a risk factor of adult recurrent chalazion. Eur. J. Ophthalmol 24(2), 159–163 (2014).
Liang, L., Ding, X. & Tseng, S. C. High prevalence of demodex brevis infestation in chalazia. Am. J. Ophthalmol. 157(2), 342–348.e1 (2014).
Cheng, A. M., Sheha, H. & Tseng, S. C. Recent advances on ocular Demodex infestation. Curr. Opin. Ophthalmol. 26(4), 295–300 (2015).
Liang, L. et al. Significant correlation between meibomian gland dysfunction and keratitis in young patients with Demodex brevis infestation. Br. J. Ophthalmol. 102(8), 1098–1102 (2018).
Navel, V. et al. Efficacy of treatments for Demodex blepharitis: A systematic review and meta-analysis. Ocul. Surf. 17(4), 655–669 (2019).
Koo, H. et al. Ocular surface discomfort and Demodex: Effect of tea tree oil eyelid scrub in Demodex blepharitis. J. Korean Med. Sci. 27(12), 1574–1579 (2012).
Carlisle, R. T. & Digiovanni, J. Differential diagnosis of the swollen red eyelid. Am. Fam. Physician 92(2), 106–112 (2015).
Lindsley, K., Nichols, J. J. & Dickersin, K. Interventions for acute internal hordeolum. Cochrane Database Syst. Rev. 4(4), CD007742 (2013).
Fuchs, E. Text-Book of Ophthalmology (JB Lippincott Company, 1911).
Wald, E. R. Periorbital and orbital infections. Infect. Dis. Clin. North Am. 21(2), 393–408,vi (2007).
Moriarty, P. A. & Collin, J. R. Eyelid problems. Practitioner 226(1367), 901–923 (1982).
Chen, L. et al. Prevalence of low serum vitamin a levels in young children with chalazia in southwest china. Am. J. Ophthalmol. 157(5), 1103–1108.e2 (2014).
Kaya, S., Selimoglu, M. A., Kaya, O. A. & Ozgen, U. Prevalence of Demodex folliculorum and Demodex brevis in childhood malnutrition and malignancy. Pediatr. Int. 55(1), 85–89 (2013).
Roodyn, L. Staphylococcal infections in general practice. Br. Med. J. 2(4900), 1322–1325 (1954).
Lacey, N., Kavanagh, K. & Tseng, S. C. Under the lash: Demodex mites in human diseases. Biochemist 31(4), 2–6 (2009).
Liu, J., Sheha, H. & Tseng, S. C. Pathogenic role of Demodex mites in blepharitis. Curr. Opin. Allergy Clin. Immunol. 10(5), 505–510 (2010).
Litwin, D., Chen, W., Dzika, E. & Korycinska, J. Human permanent ectoparasites; recent advances on biology and clinical significance of Demodex mites: Narrative review article. Iran J. Parasitol. 12(1), 12–21 (2017).
Lacey, N., Russell-Hallinan, A. & Powell, F. C. Study of Demodex mites: Challenges and solutions. J. Eur. Acad. Dermatol. Venereol. 30(5), 764–775 (2016).
Nicholls, S. G., Oakley, C. L., Tan, A. & Vote, B. J. Demodex treatment in external ocular disease: The outcomes of a Tasmanian case series. Int. Ophthalmol. 36(5), 691–696 (2016).
Schear, M. J. et al. The association of Demodex with chalazia: A histopathologic study of the eyelid. Ophthalmic Plast. Reconstr. Surg. 32(4), 275–278 (2016).
Woolley, T. A. Acarology: Mites and Human Welfare, 1 ed (1988).
Tarkowski, W., Owczynska, M., Blaszczyk-Tyszka, A. & Mlocicki, D. Demodex mites as potential etiological factor in chalazion—A study in Poland. Acta Parasitol. 60(4), 777–783 (2015).
Aroni, K., Tsagroni, E., Lazaris, A. C., Patsouris, E. & Agapitos, E. Rosacea: A clinicopathological approach. Dermatology 209(3), 177–182 (2004).
Karincaoglu, Y., Bayram, N., Aycan, O. & Esrefoglu, M. The clinical importance of demodex folliculorum presenting with nonspecific facial signs and symptoms. J. Dermatol. 31(8), 618–626 (2004).
Ku, Q. An epidemiological investigation of human demodicidosis. Chin. J. Dermatol. 15, 89–93 (1982).
Norn, M. S. Demodex folliculorum. Incidence and possible pathogenic role in the human eyelid. Acta Ophthalmol. Suppl. 108, 7–85 (1970).
Vargas-Arzola, J. et al. Prevalence of Demodex mites in eyelashes among people of Oaxaca, Mexico. . Acta Microbiol. Immunol. Hung. 59(2), 257–262 (2012).
Stewart, M. E. & Downing, D. T. Measurement of sebum secretion rates in young children. J. Investig. Dermatol. 84(1), 59–61 (1985).
Mourelatos, K., Eady, E. A., Cunliffe, W. J., Clark, S. M. & Cove, J. H. Temporal changes in sebum excretion and propionibacterial colonization in preadolescent children with and without acne. Br. J. Dermatol. 156(1), 22–31 (2007).
Downing, D. T., Stewart, M. E. & Strauss, J. S. Changes in sebum secretion and the sebaceous gland. Dermatol. Clin. 4(3), 419–423 (1986).
Jacobsen, E. et al. Age-related changes in sebaceous wax ester secretion rates in men and women. J. Investig. Dermatol. 85(5), 483–485 (1985).
Gao, Y. Y. et al. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br. J. Ophthalmol. 89(11), 1468–1473 (2005).
Gao, Y. Y., Xu, D. L., Wang, R. & Tseng, S. C. Treatment of ocular itching associated with ocular demodicosis by 5% tea tree oil ointment. Cornea 31(1), 14–17 (2012).
Gao, Y. Y., Di Pascuale, M. A., Elizondo, A. & Tseng, S. C. Clinical treatment of ocular demodecosis by lid scrub with tea tree oil. Cornea 26(2), 136–143 (2007).
Mills, C., Cleary, B. J., Gilmer, J. F. & Walsh, J. J. Inhibition of acetylcholinesterase by Tea Tree oil. J. Pharm. Pharmacol. 56(3), 375–379 (2004).
Acknowledgements
The authors have no financial interests related to this article.
Author information
Authors and Affiliations
Contributions
S.Y.J., Y.J.C. and S.C.K. conducted the study, analyzed the data, and a major contributor in writing the manuscript. S.Y.J., Y.J.C., and B.R.L. prepared all figures and tables. S.C.K. helped in the design of the study. S.C.K. helped S.Y.J. to verify analytic methods in statistics and the analysis of the data and critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jun, S.Y., Choi, Y.J., Lee, B.R. et al. Clinical characteristics of Demodex-associated recurrent hordeola: an observational, comparative study. Sci Rep 11, 21398 (2021). https://doi.org/10.1038/s41598-021-00599-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00599-7
This article is cited by
-
Demodex Blepharitis: Its Role and Treatment in Ocular Surface Disease
Current Ophthalmology Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.