Abstract
Despite type 2 diabetes mellitus (T2D) is commonly considered a detrimental factor in dialysis, its clear effect on morbidity and mortality on waitlisted patients for kidney transplant (KT) has never been completely elucidated. We performed a retrospective analysis on 714 patients admitted to wait-list (WL) for their first kidney transplant from 2005 to 2010. Clinical characteristics at registration in WL (age, body mass index -BMI-, duration and modality of dialysis, underlying nephropathy, coronary artery -CAD- and/or peripheral vascular disease), mortality rates, and effective time on WL were investigated and compared according to T2D status (presence/absence). Data about therapy and management of T2D were also considered. At the time of WL registration T2D patients (n = 86) were older than non-T2D (n = 628) (58.7 ± 8.6 years vs 51.3 ± 12.9) with higher BMI (26.2 ± 3.8 kg/m2 vs 23.8 ± 3.6), more frequent history of CAD (33.3% vs 9.8%) and peripheral vascular disease (25.3% vs 5.8%) (p < 0.001 for all analyses). Considering overall population, T2D patients had reduced survival vs non-T2D (p < 0.001). Transplanted patients showed better survival in both T2D and non-T2D groups despite transplant rate are lower in T2D (75.6% vs 85.8%, p < 0.001). T2D was also associated to similar waiting time but longer periods between dialysis start and registration in WL (1.6 years vs 1.2, p = 0.008), comorbidity-related suspension from WL (571 days vs 257, p = 0.002), and increased mortality rate (33.7% vs 13.9% in the overall population, p < 0.001). In T2D patients admitted to WL, an history of vascular disease was significantly associated to low patient survival (p = 0.019). In conclusion, T2D significantly affects survival also on waitlisted patients. Allocation policies in T2D patients may be adjusted according to increased risk of mortality and WL suspension due to comorbidities.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2D) represents a real public health problem according to its increasing incidence and the severity of the disease with multi-organic involvement1. T2D long-term complications include disability, reduced quality of life, premature death, and end-stage kidney disease (ESKD)2 with a consequent spreading percentage of dialytic patients affected by T2D3. In this population a multi-specialistic approach to prevent and manage T2D-related comorbidity is mandatory. Despite improvements over the last decade have leaded to an amelioration in survival rates, both diabetes and ESKD increased risk of mortality, particularly due to cardiovascular complications, especially in cases who needed renal-replacement therapies2,4.
KT is considered the gold standard for ESKD for its superiority to dialysis for all outcomes (quality of life, overall survival, economic costs)5,6 and, despite some authors suggested negative or “not-so-positive” results in T2D patients7, recent reports outline favorable outcome also in T2D patients8. On the other hand few studies are focused on T2D patients who could be considered eligible for KT, and none of them at the best of our knowledge have evaluated if WL time—a variable directly correlated to negative outcome both for patient and KT7,8—could be influenced by the intrinsic T2D frailty for T2D-related comorbidities.
In this study we investigate the effect of T2D on morbidity and mortality on waitlisted patients also comparing the effective time on WL according to T2D status (presence/absence).
Results
Baseline characteristics
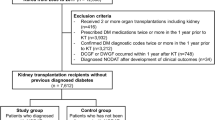
During the investigated period, 714 patients were registered in our WL and 86 out of 714 (12%) were affected by T2D. Clinical characteristics are summarized in Table 1.
Briefly, at the admission patients in T2D group were older than non-T2D (58.7 ± 8.6 years vs 51.3 ± 12.9) with higher BMI (26.2 ± 3.8 kg/m2 vs 23.8 ± 3.6), more frequent history of CAD (33.3% vs 9.8%) and peripheral vascular disease (25.3% vs 5.8%) (p < 0.001 for all analyses). No differences were observed regarding dialysis length and modality.
Pharmacological treatment of T2D and cardiovascular characteristics of our T2D patients admitted to WL were reported in Table 2.
In detail, 48 out of 86 patients (55.8%) received insulin therapy, 5/86 (5.8%) were treated with oral anti-diabetic drugs, and 22/86 (25.6%) followed diet alone. HbA1c value at the time of registration in WL were within the correct range of glycemic control [median HbA1c 50 mmol/mol (25° 40–75° 61)].
Despite a more frequent history of CAD and evidence of left ventricular hypertrophy in the majority of T2D patients (50/86, 58.1%), echocardiography assessment revealed a normal median ejection fraction [median 60% (25° 55–75° 64)]. Considering vascular disease, percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) were performed in 13/86 (15.1%) and 4/86 (4.7%) respectively; an history of cerebrovascular accident was also observed in 9/86 T2D patients (10.5%).
During the follow-up (mean 8.4 ± 3 years) 604 patients underwent KT (84.6%) with a significantly lower KT rate in T2D group (75.6% vs 85.8%, p = 0.013). The number of living donors was similar in each group but, in deceased donors, donor’s age was higher in T2D group.
Survival analysis
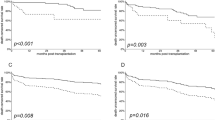
Survival rates were investigated both considering the f/up starting at the beginning of dialysis or at the time of registration in WL. Patients in T2D group had a reduced survival than non-T2D (Fig. 1 a–b) and transplanted patients had a better survival than those who remain in WL (Fig. 2 a–b); comprehensively, all transplanted patients had a better survival than those remaining on WL. This favorable outcome of KT patients was confirmed in the intra-group analysis both for T2D and non-T2D groups, despite T2D showed lower survival rates (Fig. 3).
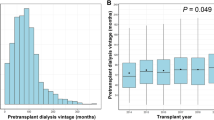
Analyzing the possible impact of dialysis duration on survival we noted that patients who died during the f/up have a longer dialysis history before the registration in WL [19.8 months (25° 10–75° 34.5) vs 15 months (25° 8.9–75° 26.2), p < 0.01]; stratifying this data to patients who underwent KT this variable remained significant in the overall population and in non-T2D group.
Among both the overall population and the subgroup of patients who did not receive KT the mortality rate was significantly higher in T2D (Table 1); focusing on this group (which is not biased by transplant-related events) cardiovascular events and infections, as expected, were the most common causes of death in both T2D and non-T2D (Table 3). Cox regression analysis showed a 2.4 fold higher mortality risk (OR 2.4, IC 95% 1.5–3.6) in T2D vs non-T2D group, 7.5 fold higher (OR 7.5, IC 95% 5.2–10.7) in patients who remained in WL vs KT, and 18.5 fold higher (OR 18.5, IC 95% 4.9–10.1) for the group with lower survival (non-transplanted patients in T2D group) vs patients with favorable one (non-T2D who underwent KT).
A stratification of survival analysis in T2D group revealed the significant negative impact of an history of vascular accident (intended as PCI, CABG and/or cerebrovascular accident) on this population (Supplementary Figure S1, p = 0.015); also insulin therapy and a worst glycemic control showed a negative trend on patients survival (Supplementary Figures S2 and S3).
Waiting list period
The median waiting time for KT was not statistically different between T2D and non-T2D group [466.5 days (25° 104.5–75° 1182) vs 620 (25° 174–75° 1619) respectively, p = 0.095].
Despite the percentage of patients who experienced at least one temporary suspension from the WL was quite similar in T2D and non-T2D (36% vs 39.7% respectively; p = 0.3), the period of suspension was longer in T2D group (571 days, 25° 289–75° 1073 vs 257, 25° 83.5–75° 802; p < 0.001). T2D group also experienced an higher percentage of patients definitively dropped out from WL for clinical reasons (17.4% vs 8.4%, p = 0.008) and a longer time elapsed between dialysis start and WL registration (1.6 years, 25° 1.1–75° 2.5 vs 1.2, 25° 0.72–75° 2.2; p = 0.008) (Table 1).
Discussion
T2D is now considered the leading cause of ESKD in western countries, with a percentage of affected patients that range from 30% in European area2,9 to 45% in USA10,11. In our population the prevalence of T2D in dialytic population significantly increased over time, from 25% (2004–2008) to 29.1% (2009–2013)2. In subjects who ultimately needed renal-replacement therapies, T2D also negatively affect patient survival12. In 2009 Report of United States Renal Data system the 10-year survival of T2D patient on hemodialysis stands around 10%13; in another study in France 32% of patients with T2D died after a mean f/up of about 7 months14.
Despite its increasing incidence, the proportion of T2D patients admitted to WL is relatively low (ranging from 15–20% in Europe to about 30% in USA) as reported in literature5,15,16,17,18,19,20, and confirmed in our experience.
The prevalence of T2D among dialytic population in our region where KT Center is located (Piemonte e Valle d’Aosta) is about 29%2; however, considering the average age of patients who started dialysis (≈ 70 years)21, it is conceivable that only a portion of these T2D patients would be considered eligible for KT.
This difference is probably referred to T2D-related comorbidities (i.e. CAD, peripheral vascular disease, infections) who may determine an a-priori exclusion or a delay/interruption in WL process for acute clinical events (i.e. conditions requiring surgical or angiographic procedures as coronary artery intervention). A demonstration derived from the paper by Villar et al.5 where T2D and elderly age (> 60 years) are identified as the leading causes for WL exclusion, and both elderly and diabetic patients need a longer time for the pre-transplantation balance.
Data are still lacking about morbidity and mortality in the subgroup of T2D patients considered eligible for WL. Schold et al.22 reported that T2D patients are more prone to be removed from WL and Ningyan et al.23 underlined that a great proportion of patients were dropped-out from WL due to a cardiovascular event, a condition extensively related to T2D.
In our analysis, as expected, T2D patients at the time of WL registration were older, with higher BMI and more frequent history of CAD and peripheral vascular disease. Despite the pre-admission balance demonstrates that the majority of patients had a normal ejection fraction and were on-target for HbA1c according to international guidelines24, our adjunctive analysis revealed the significant role of an history of vascular accident on reducing patient survival, with also a univocal trend for patients with poor glycemic control: all these information stressed the importance of good T2D management also in the subgroup of patients admitted to WL.
As also expected, KT determined a significant outcome amelioration in both T2D and non- T2D group. Many studies showed similar results4,25 also suggesting an adjunctive benefit for pre-emptive transplantation26,27. Despite slightly better results were observed in non-T2D group, as outlined by Cosio et al.6 mortality in KT recipients with T2D has progressively declined over time, thanks to the improvements in the management of both T2D and KT, and the beneficial effect of KT as also observed in our population is overwhelming. In accordance with K-DOQI guidelines all ESKD patients, especially those with T2D, need to be referred to a nephrological center also for a prompt pre-transplant evaluation28.
On the other hand, despite patients in T2D and non-T2D group have a similar median WL-time and percentage of temporary drop-out from WL, transplant rate was lower in T2D patients; moreover, T2D experienced a threefold higher mortality after waitlisting which remained extremely high in not transplanted patients, suspension periods were longer and associated with a higher definitive drop-out rate in T2D group suggesting a significant negative impact of T2D-related comorbidities. Previous studies identify T2D and cardiovascular disease as major dominants of lower odds of being on the WL29,30,31.
Similar to Lee et al.8 T2D patients experienced a higher mortality during WL also in our study and, as expected, cardiovascular events (probably underestimated due to the absence of a determined death cause in the majority of patients) were the most common cause of death in this group. Cardiovascular disease are typical comorbidities affecting all ESKD patients, with higher prevalence and incidence than in general population: they can aggravate the underlying medical condition and limit the access to KT7. Successful KT accords major benefits by reducing cardiovascular risk in these patients, and efforts are needed to minimize WL time32.
Based on our study design, not influenced by a negative-selection bias, we speculate that the reduced likelihood of KT among T2D group may also suggest a per-se negative effect of T2D on KT rate. In one recent study by Jeon et al. the occurrence of cardiovascular disease but not diabetes determined lower transplant rates7, so it could be important to investigate the possible negative T2D effect in larger cohorts.
Despite the obvious limitations (low percentage of T2D patients admitted to WL, retrospective design) which also affected the majority of the reported experiences in this area, our study demonstrates that (a) T2D significantly affects patients survival also on patients who are eligible for WL (b) T2D patients, probably due to T2D-related conditions (especially vascular disease), have a reduced probability of being transplanted (c) KT also in T2D patients is clearly associated with better survival. In our opinion efforts are needed in order to estimate as earlier as possible the eligibility of T2D patients for WL and, at the same time, allocation policies may be adjusted according to the increased risk of mortality and WL suspension due to comorbidities in T2D patients.
Methods
Retrospective study on the waitlisted population of our center (Renal Transplantation Center “A. Vercellone”, Turin, Italy) including all patients who are considered eligible and included in active WL in the period between January 2005 and December 2010, and transplanted until February 2016. The analysis included patients from two regions of northern Italy (Piemonte and Valle d’Aosta) and at first KT; type 1 and post-transplant diabetes mellitus, and patients with glycated hemoglobin (HbA1c) > 64 mmol/mol at the time of inclusion in WL were excluded. Diagnosis of T2D was made according to the American Diabetes Association recommendations24. Recorded variables at registration in WL included age, sex, dialysis duration and modality (hemodialysis or peritoneal dialysis), body mass index (BMI), history of coronary artery (CAD) and/or peripheral vascular disease. All these conditions were compared to T2D presence/absence. Data were collected from the database of our transplantation center (ITR02, Dialysis and Transplantation Registry of Piemonte) and are thereafter elaborated in anonymous format. This study is covered by Ethical Committee approval, resolution number 1449/2019 on 11/08/2019 ("TGT" observational study).
Statistical analysis was performed with SPSS (IBM SPSS Statistics, vers.25.0.0). Continuous variables are presented as mean ± standard deviation or as median (25°-75° percentile), according to their distribution analysed with Kolmogorov–Smirnov test. The difference between groups was analysed, respectively, with t-test or Mann–Whitney test. Some cut-off levels were with ROC curves. Categorical variables are presented as fraction and Pearson’s or, for small samples, Fisher’s exact test was employed to compare groups. The odds ratios (OR) with 95% Confidence Interval were used as a measure of relative risk. Univariate Survival analysis was performed by means of the Kaplan–Meier method with Log Rank test to compare strata. Cox proportional-hazards model was used to investigate the association between the survival time of patients and predictor variables. Significance level for all tests was set at p < 0.05.
Ethical statement
This study is covered by Ethical Committee approval, Resolution Number 1449/2019 on 11/08/2019 ("TGT" observational study) for which all patients sign an informed consent. The study was conducted in accordance with Declaration of Helsinki.
Data availability
All data and datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Guariguata, L. et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res. Clin. Pract. 103, 137–149 (2014).
Giorda, C. B. et al. Ten-year comparative analysis of incidence, prognosis, and associated factors for dialysis and renal transplantation in type 1 and type 2 diabetes versus non-diabetes. Acta Diabetol. 55, 733–740 (2018).
Boucek, P. et al. Kidney transplantation in type 2 diabetic patients: A comparison with matched non-diabetic subjects. Nephrol Dial Transplant 17, 1678–1683 (2002).
Keddis, M. T. et al. Enhanced posttransplant management of patients with diabetes improves patient outcomes. Kidney Int. 86, 610–618 (2014).
Villar, E. et al. A multicentre study of registration on renal transplantation waiting list of the elderly and patients with type 2 diabetes. Nephrol. Dial. Transplant 19, 207–214 (2004).
Cosio, F. G., Hickson, L. J., Griffin, M. D., Stegall, M. D. & Kudva, Y. Patient survival and cardiovascular risk after kidney transplantation: The challenge of diabetes. Am. J. Transplant 8, 593–599 (2008).
Jeon, H. J. et al. Outcomes of end-stage renal disease patients on the waiting list for deceased donor kidney transplantation: A single-center study. Kidney Res. Clin. Pract. 38, 116–123 (2019).
Lee, S. et al. Factors affecting mortality during the waiting time for kidney transplantation: A nationwide population-based cohort study using the Korean Network for Organ Sharing ( KONOS ) database. PLoS ONE 14, 1–13 (2019).
Atkins, R. C. The epidemiology of chronic kidney disease. Kidney Int. Suppl. 67, 14–18 (2005).
Ritz, E. et al. End-stage renal failure in Type 2 Diabetes: A medical catastrophe of worldwide dimensions. Am. J. Kidney Dis. 34, 795–808 (1999).
Collins, A. J. et al. US renal data system 2013 annual data report: Preface. Am. J. Kidney Dis. 63, A7 (2014).
Seshasai, S. R. K. et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 364, 829–841 (2011).
Collins, A. J. et al. Excerpts from the US Renal Data System 2009 annual data report. Am. J. Kidney Dis. 55, A6–A7 (2010).
Ghaderian, S. B., Hayati, F., Shayanpour, S. & Beladi Mousavi, S. S. Diabetes and end-stage renal disease: A review article on new concepts. J. Ren. Inj. Prev. 4, 28–33 (2015).
Wolfe, R. A. et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N. Engl. J. Med. 341, 1725–1730 (1999).
Meier-Kriesche, H. U. et al. Effect of waiting time on renal transplant outcome. Kidney Int. 58, 1311–1317 (2000).
Guthoff, M. et al. Diabetes mellitus and prediabetes on kidney transplant waiting list-prevalence, metabolic phenotyping and risk stratification approach. PLoS ONE 10, 1–13 (2015).
de Freminville, J.-B. et al. The association between renal resistive index and premature mortality after kidney transplantation is modified by pre-transplant diabetes status: A cohort study. Nephrol. Dial. Transplant. 35, 1577–1584. https://doi.org/10.1093/ndt/gfz067 (2019).
Oniscu, G. et al. Equity of access to renal transplant waiting list and renal transplantation in Scotland: Cohort study. BMJ 29, 327 (2003).
Ott, U. et al. Presence of cardiovascular disease in patients on a waiting list for renal transplantation and in patients after kidney transplantation in a single center. Transplant. Proc. 42, 3450–3454 (2010).
Limido, A. et al. Come cambia la popolazione uremica nel Registro Nazionale di Dialisi e Trapianto [Changes in the uremic population overtime: Data from the Italian Registry of Dialysis and Transplantation (RIDT)]. G. Ital. Nefrol. 29, S21–S26 (2012).
Schold, J. D., Buccini, L. D., Poggio, E. D., Flechner, S. M. & Goldfarb, D. A. Association of candidate removals from the kidney transplant waiting list and center performance oversight. Am. J. Transplant. 16, 1276–1284 (2016).
Ningyan, W. et al. Risk factors for cardiovascular events among Asian patients without pre-existing cardiovascular disease on the renal transplant wait list. ASEAN Heart J. 23, 1–7 (2015).
American Diabetes Association 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2019. Diabetes Care 42, S13–S28 (2019).
Chadban, S. J. & Staplin, N. D. Is it time to increase access to transplantation for those with diabetic end-stage kidney disease?. Kidney Int. 86, 464–466 (2014).
Kasiske, B. L. et al. Preemptive kidney transplantation: The advantage and the advantaged. J. Am. Soc. Nephrol. 13, 1358–1364 (2002).
Gill, J. S., Tonelli, M., Johnson, N. & Pereira, B. J. G. Why do preemptive kidney transplant recipients have an allograft survival advantage?. Transplantation 78, 873–879 (2004).
K/DOQI Work Group. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am. J. Kidney Dis. 45, 16–153 (2005).
Szeifert, L. et al. Psychosocial variables are associated with being wait-listed, but not with receiving a kidney transplant in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol. Dial. Transplant 27, 2107–2113 (2012).
Bayat, S. et al. Medical and non-medical determinants of access to renal transplant waiting list in a French community-based network of care. Nephrol. Dial. Transplant 21, 2900–2907 (2006).
Akolekar, D., Forsythe, J. L. R. & Oniscu, G. C. Impact of patient characteristics and comorbidity profile on activation of patients on the kidney transplantation waiting list. Transplant Proc. 45, 2115–2122 (2013).
Stoumpos, S., Jardine, A. G. & Mark, P. B. Cardiovascular morbidity and mortality after kidney transplantation. Transplant Int. 28, 10–21 (2015).
Aknowlegements
We thank Antonio Amoroso, MD for the technical support of the Regional Transplant Center to this work and the following nephrologists for sharing patients’ clinical data: Andrea Campo and Giusto Viglino (San Lazzaro Hospital, Alba), Michela Tamagnone, Daniela Falconi and Marco Formica (ASL CN1), Laura Biselli and Mario Salomone (Ospedale Maggiore, Chieri), Maria Carla Deabate, Guido Martina, Franca Giacchino and Silvana Savoldi (ASL TO4 Ciriè, Chivasso, Ivrea), Carlo Ferrando, Alfonso Pacitti and Luca Besso (ASO S. Croce e Carle, Cuneo), Andrea Molino, Pier Eugenio Nebiolo and Massimo Manes (Parini Hospital, Aosta), Fulvia Caligaris and Stefano Maffei (Cardinal Massaia Hospital, Asti), Roberto Boero (Martini Hospital, Torino), Giorgio Soragna and Corrado Vitale (Mauriziano Hospital, Torino), Antonella Rizzuto and Marco Saltarelli (E. Agnelli Hospital, Pinerolo), Dib Hamido and Marco Saltarelli (Ospedale degli Infermi, Rivoli), Bruno Basolo and Dario Roccatello (S. Giovanni Bosco Hospital, Torino).
Funding
The authors declare no funding was received for this study.
Author information
Authors and Affiliations
Contributions
C.D.: concept design, data collection, analysis and interpretation and drafting article; E.N., A.A.: data collection, analysis and interpretation and drafting article; A.M.: data analysis and interpretation and drafting article; R.G., M.C.T., E.G., A.L.: critical revision; S.B.V.: waiting list data manager; F.F.: statistics; L.B.: concept design, analysis and interpretation and critical revision. All authors provided intellectual content of critical importance to the work described and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dolla, C., Naso, E., Mella, A. et al. Impact of type 2 diabetes mellitus on kidney transplant rates and clinical outcomes among waitlisted candidates in a single center European experience. Sci Rep 10, 22000 (2020). https://doi.org/10.1038/s41598-020-78938-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-78938-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.