Abstract
As increased oxidative stress causes increased mortality and morbidities like bronchopulmonary dysplasia (BPD) and retinopathy of prematurity (ROP) in very low birth weight infants (VLBWIs), the conundrum of improved survival but increased ROP observed with the high oxygen saturation target range of 91–95% is difficult to explain. To determine the survival rate-dependent variation in ROP treatment rate, 6292 surviving eligible VLBWIs registered in the Korean Neonatal Network were arbitrarily grouped according to the survival rate of infants at 23–24 weeks’ gestation as group I (> 70%, n = 1626), group II (40–70%, n = 2984) and group III (< 40%, n = 1682). Despite significantly higher survival and lower BPD rates in group I than in groups II and III, the ROP treatment rate was higher in group I than in groups II and III. However, the adjusted odds ratios for ROP treatment were not significantly different between the study groups, and the ROP treatment rate in the infants at 23–24 weeks’ gestation was 21-fold higher than the infants at ≥ 27 weeks’ gestation. The controversial association between improved survival and reduced BPD reflecting quality improvement of neonatal intensive care but increased ROP treatment rate might be primarily attributed to the improved survival of the most immature infants.
Similar content being viewed by others
Introduction
Increased oxidative stress is a causative factor for increased mortality and morbidities such as bronchopulmonary dysplasia (BPD) and retinopathy of prematurity (ROP) in very low birth weight infants (VLBWIs)1,2,3,4,5,6,7. Hence, the controversial association between improved survival and increased rates of ROP and BPD with higher oxygen saturation targets of 91–95% that have been observed in several randomized trials and meta-analyses8,9,10,11,12,13,14,15,16,17,18,19,20 is difficult to explain. Prematurity itself was reported to be a dominant risk factor, with infants born at < 25 weeks’ gestation having 20-fold higher chance of developing severe ROP than those born at 28 weeks’ gestation11. Therefore, these findings suggest that the conundrum of association between improved survival reflecting quality improvement of neonatal intensive care and increased ROP treatment rate might be primarily attributed to improved survival of the peri-viable infants born at < 25 weeks’ gestation at the highest risk for developing severe ROP requiring treatment2,7,21,22.
Single neonatal intensive care unit (NICU) based studies might have introduced bias into the results due to small sample sizes and/or variation in clinical practices. Therefore, a population based nationwide registry study might be the best way to analyze the complex relationship between mortality and prevalence of ROP and BPD in VLBWIs23,24,25,26. The Korean Neonatal Network (KNN) is a nationwide, multicenter, prospective and web-based cohort registry system for VLBWIs27,28,29. We observed in our previous studies that the survival rate in peri-viable infants born at 23–24 weeks’ gestation reflected the quality of perinatal and neonatal intensive care of each NICU, and improved survival of infants at 23–24 weeks’ gestation from ≤ 50 to > 50% was associated with significantly less BPD but not severe ROP in the more mature infants at 25–26 weeks’ gestation28,30,31. In our previous single center studies, improved survival of infants at 23–24 weeks’ gestation from 55 to 84% was associated with reduced incidence of not only BPD but also ROP in the more mature infants at 25–26 weeks’ gestation30,32. In the present study, we further subdivided the KNN data of VLBWIs according to the survival rate of infants at 23–24 weeks’ gestation at < 40%, 40–70% and > 70%, and stratified according to the presence or absence of BPD and gestational age as 23–24, 25–26 and ≥ 27 weeks’ gestation subgroups in order to determine whether the controversial association between improved survival and reduced BPD reflecting quality improvement of neonatal intensive care but increased ROP treatment might be primarily attributed to survival of the most immature infants at the highest risk of severe ROP requiring treatment.
Results
Survival and bronchopulmonary dysplasia rate
Table 1 presents the comparison of overall and gestational age-specific survival rates for VLBWIs in the three groups stratified by the survival rates of 23–24 weeks’ gestation. The overall and gestational age-specific survival rate and adjusted odds ratios (ORs) for survival were significantly higher in group I than in groups II and III, and higher in group II than in group III.
Table 2 presents the comparison of overall and gestational age-specific BPD rates for survived VLBWIs in the three groups. The overall and gestational age-specific BPD rate in the infants at 25–26 weeks’ gestation and adjusted ORs for BPD in surviving VLBWIs were significantly lower in group I than in groups II and III, but no significant differences were seen between group II and group III.
Clinical characteristics
Table 3 demonstrates clinical characteristics according to ROP treatment in the three groups. Clinical characteristics including gestational age and birth weight were significantly lower, and morbidities including BPD and sepsis were significantly higher in surviving VLBWIs with ROP treatment than those without ROP treatment in all three groups. Regardless of ROP treatment, both gestational age and birth weight were significantly lower in group I than in groups II and III, and lower in group II than in group III. BPD and periventricular leukomalacia (PVL) were significantly lower, and symptomatic patent ductus arteriosus (PDA) was significantly higher in group I than in groups II and III.
Retinopathy of prematurity treatment rate
Table 4 presents the rate and adjusted ORs of ROP treatment according to the presence or absence of BPD. The ROP treatment rate was significantly higher in surviving VLBWIs with BPD than those without BPD in all three groups. In the comparison between the study groups according to the presence or absence of BPD, the ROP treatment rate was significantly higher in group I than in groups II and III. However, the overall and gestational age-specific adjusted ORs for ROP treatment was not significantly different between the study groups.
Discussion
In the present study, we assessed the quality of neonatal intensive care in each hospital solely according to the survival rate of peri-viable infants at 23–24 weeks’ gestation without specific information about care and diagnosis during pregnancy, perinatal and neonatal care, variations in oxygen saturation targets, ROP screening and treatment criteria, and man-power and socioeconomic circumstances. For international comparison, the network ranking according to the survival rate of infants at 24 weeks’ gestation remained largely unchanged as gestational age increased26. In our previous and present studies, improved survival rates of infants at 23–24 weeks’ gestation were associated with reduced morbidities such as BPD in the more mature infants at 25–26 weeks’ gestation28,30,32. Overall, these findings suggest that quality improvement of perinatal and neonatal intensive care as evidenced by improved survival of peri-viable infants at 23–24 weeks’ gestation could not only improve survival but also reduce morbidity rates of extremely preterm infants7,28,30,31,33.
Given that oxygen toxicity increases the risk of death, BPD and ROP in the premature infants3,4,5,6,29,34,35, the controversial association of decreased ROP, BPD and survival observed in the lower oxygen saturation setting of 85–89%, and the increased ROP, BPD and survival observed in the higher oxygen saturation setting of 91–95%12,13,14,15,16,17,18,19,20,21,22,23,24 is difficult to explain. For international comparison of neonatal research networks, the Japanese neonatal research network with the highest survival rate and proportion of infants at 24 weeks’ gestation reported the highest BPD and ROP treatment rates, whereas the Swiss neonatal network with a low survival and proportion of infants at 24 weeks’ gestation reported the lowest BPD and ROP treatment rates2,25. In the present nationwide population based KNN cohort study of surviving VLBWIs at ≥ 23 weeks’ gestation, despite its best survival and lowest BPD rates indicative of the best quality of neonatal intensive care, the ROP treatment rate was highest in group I compared with group II and/or group III. However, in multivariate analyses, the adjusted ORs for ROP treatment were not significantly different between the study groups. Moreover, the ROP treatment rate was 21-fold higher in the infants at 23–24 weeks’ gestation than in the infants at > 27 weeks’ gestation in this study. Taken together, these findings suggest that as extreme immaturity itself is a primary factor for severe ROP requiring treatment, improved survival of peri-viable infants born at 23–24 weeks’ gestation is primarily responsible for the apparent association between improved survival rate and increased rate of ROP treatment in VLBWIs.
The strengths of this study included the prospective, nationwide, population-based design, which included, at least, one ROP examination on surviving VLBWIs born at ≥ 23 weeks’ gestation during admission. However, the lack of available data on the timing and frequency of the examinations, and the zone and extent of the disease are some limitations of this study.
In conclusion, in this nationwide prospective cohort study of surviving VLBWIs born at ≥ 23 weeks’ gestation with at least, one ROP examination during admission, despite the best survival and lowest BPD rates indicative of the best quality of neonatal intensive care, the highest rate of severe ROP requiring treatment occurred in the group of infants with a survival rate > 70% at 23–24 weeks’ gestation. However, the adjusted odds ratios for ROP treatment were not significantly different between the study groups, and the ROP treatment rate in the infants at 23–24 weeks’ gestation was 21-fold higher than the infants at ≥ 27 weeks’ gestation. The controversial association between improved survival and reduced BPD reflecting quality improvement of neonatal intensive care but increased ROP treatment rate might be primarily attributed to the improved survival of the most immature infants at the highest risk for developing severe ROP requiring treatment.
Methods
Patients
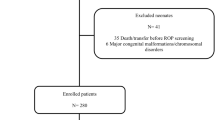
The database registry of the KNN prospectively registered the clinical information of VLBWIs defined as birth weight < 1500 g admitted to the 67 voluntarily participating neonatal intensive care units (NICUs) covering > 80% of VLBWIs in South Korea36. Between January 1, 2013, and December 31, 2016, 8287 VLBWIs were registered in the KNN database (Fig. 1). As previous studies on the KNN database had already identified prominent institutional differences in the survival rates of infants born at 23–24 weeks’ gestation, we divided the enrolled institutions into three groups based on the survival rate of infants born at 23–24 weeks’ gestation. Of the 67 institutions participating in KNN, only 53 were registered with the KNN database for extremely preterm infants born at 23–24 weeks’ gestation. Therefore, we excluded 370 VLBWIs enrolled at institutions that did not have a registration for infants born at 23–24 weeks’ gestation. To reduce the skew of study outcomes as a result of other causes, we also excluded 297 VLBWIs with major congenital anomalies and 109 born at < 23 weeks’ gestation. Thus, group I included 1829 VLBWIs born at institutions with a survival rate of infants born at 23–24 weeks’ gestation > 70%, group II included 3493 VLBWIs born at institutions with that of 40–70%, and group III included 2189 VLBWIs born at institutions with that < 40%. To investigate the severity of BPD, we excluded 934 infants who died and 60 infants with missing BPD data. To investigate the rate of ROP treatment, we also excluded 225 infants who did not undergo ophthalmic examination before discharge. Considering the difference in survival rate as well as BPD or ROP treatment rates according to gestational age at birth, the infants were stratified into gestational age-specific subgroups of 23–24, 25–26, and ≥ 27 weeks’ gestation.
We recorded the highest stage of ROP using the International Classification of ROP37, along with any treatment to prevent vision loss including anti-vascular endothelial growth factor (VEGF) and/or laser ablative and/or surgical treatment37, however, other data on the timing and frequency of examination, and zone and extent of disease were not available in this study. We compared perinatal characteristics, including gestational age (GA), birth weight, sex, mode of delivery, Apgar score at 1 and 5 min, presence of small for gestational age (SGA), maternal gestational diabetes mellitus (GDM), pregnancy-induced hypertension (PIH), premature rupture of membrane (PROM), antenatal corticosteroid, oligohydramnios, and chorioamnionitis among the three groups. We also compared neonatal morbidities, including respiratory distress syndrome (RDS), air leak syndrome, pulmonary hypertension, symptomatic PDA, surgical ligation of PDA, BPD, sepsis, necrotizing enterocolitis (NEC), intraventricular hemorrhage (IVH), PVL, and the duration of invasive ventilation representing mechanical respiratory support with invasive artificial airway, non-invasive ventilation representing nasal respiratory support including nasal continuous positive airway pressure or high flow nasal cannula, oxygen supplementation, and hospital stay among the three groups. In addition, we compared the overall and gestational age-specific ROP treatment rates with or without BPD among the three groups.
Definitions
We complied with the KNN database operation manual to define patient characteristics. In the manual, gestational age was determined from the obstetric history based on the last menstrual period. ROP treatment was defined as any treatment, including anti-VEGF and/or laser ablative and/or surgical treatment, performed on the VLBWIs to prevent visual loss37. Maternal steroid use was defined as the administration of any corticosteroid to the mother at any time before delivery to accelerate fetal lung maturity. Chorioamnionitis was confirmed by placental pathology38, and PROM was defined as rupture of membranes over 24 h before the onset of labor. BPD was defined as the use of more than supplemental oxygen at 36 weeks’ gestational age, corresponding to moderate to severe BPD using the severity-based definition for BPD of the National Institutes of Health consensus39. RDS was defined as respiratory distress requiring ventilator care and surfactant treatment with diagnosis based on chest radiographic findings. Pulmonary hypertension was defined only when accompanied by medical treatment after diagnosis based on echocardiography. Symptomatic PDA was defined as clinical symptoms of PDA, such as ventilator dependence, deteriorating respiratory status, increasing recurrent apnea, pulmonary hemorrhage and hypotension. IVH was defined as grade ≥ 3 according to the classification of Papile et al.40 PVL was defined as cystic PVL based on either head ultrasound or cranial magnetic resonance imaging scans performed at ≥ 2 weeks of age41. NEC was defined as ≥ stage 2b according to the modified Bell criteria42. Sepsis was defined as a positive blood culture in symptomatic infants suggestive of septicemia and more than 5 days of antibiotic treatment27,28.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) and categorical variables as numbers and proportions. Comparisons between categorical variables were performed using the chi-square test or Fisher’s exact test, and those between continuous variables using one-way analysis of variance (ANOVA). Post-hoc tests of one-way ANOVA were used for pairwise comparisons among the three groups, which were arbitrarily divided according to the survival rates of infants born at 23–24 weeks’ gestation. The comparison was further examined in a subgroup analysis with stratification according to gestational ages. A multivariate logistic regression analysis adjusted for covariates such as gestational age, duration of invasive ventilation and non-invasive ventilation, and duration of supplement oxygen was used to estimate the OR with 95% confidence intervals (CI) to identify the relationship between BPD and ROP requiring treatment in the three groups, which were stratified by survival. Analyses were performed using SAS V9.4 (SAS, Cary, NC, USA). A P value of < 0.05 was considered statistically significant.
Ethics statement
The KNN registry was approved by the institutional review board at each participating hospital. Informed consent was obtained from each infant’s parents at enrollment by the NICUs participating in the KNN according to the Korean Privacy Act, and was waived only in the case of infants who died in the delivery room or early after admission to the NICU before informed consent was obtained.
References
Hwang, J. H., Lee, E. H. & Kim, E. A. Retinopathy of prematurity among very-low-birth-weight infants in Korea: incidence, treatment, and risk factors. J. Korean Med. Sci. 30(Suppl 1), S88-94 (2015).
Darlow, B. A. et al. International variations and trends in the treatment for retinopathy of prematurity. Br. J. Ophthalmol. 101, 1399–1404 (2017).
Rabi, Y., Rabi, D. & Yee, W. Room air resuscitation of the depressed newborn: a systematic review and meta-analysis. Resuscitation 72, 353–363 (2007).
Silvers, K. M., Gibson, A. T., Russell, J. M. & Powers, H. J. Antioxidant activity, packed cell transfusions, and outcome in premature infants. Arch. Dis. Child. Fetal Neonatal Ed. 78, F214-219 (1998).
Zin, A. & Gole, G. A. Retinopathy of prematurity-incidence today. Clin. Perinatol. 40, 185–200 (2013).
Singh, J. K. et al. Relationship between severe bronchopulmonary dysplasia and severe retinopathy of prematurity in premature newborns. J. AAPOS 23(209), e201-209.e204. https://doi.org/10.1016/j.jaapos.2019.02.008 (2019).
Darlow, B. A. et al. Prenatal risk factors for severe retinopathy of prematurity among very preterm infants of the Australian and New Zealand Neonatal Network. Pediatrics 115, 990–996 (2005).
Askie, L. M. et al. Effects of targeting lower versus higher arterial oxygen saturations on death or disability in preterm infants. Cochrane Database Syst. Rev. 4, Cd011190. https://doi.org/10.1002/14651858.CD011190.pub2 (2017).
Manja, V., Lakshminrusimha, S. & Cook, D. J. Oxygen saturation target range for extremely preterm infants: a systematic review and meta-analysis. JAMA Pediatr. 169, 332–340 (2015).
Cummings, J. J. & Polin, R. A. Oxygen targeting in extremely low birth weight infants. Pediatrics 138, e20161576. https://doi.org/10.1542/peds.2016-1576 (2016).
Hartnett, M. E. & Lane, R. H. Effects of oxygen on the development and severity of retinopathy of prematurity. J. AAPOS 17, 229–234 (2013).
Castillo, A. et al. Pulse oxygen saturation levels and arterial oxygen tension values in newborns receiving oxygen therapy in the neonatal intensive care unit: is 85% to 93% an acceptable range?. Pediatrics 121, 882–889 (2008).
Hauspurg, A. K. et al. Blood gases and retinopathy of prematurity: the ELGAN Study. Neonatology 99, 104–111 (2011).
Gaynon, M. W. Rethinking STOP-ROP: is it worthwhile trying to modulate excessive VEGF levels in prethreshold ROP eyes by systemic intervention? A review of the role of oxygen, light adaptation state, and anemia in prethreshold ROP. Retina 26, S18-23 (2006).
Wallace, D. K., Veness-Meehan, K. A. & Miller, W. C. Incidence of severe retinopathy of prematurity before and after a modest reduction in target oxygen saturation levels. J. AAPOS 11, 170–174 (2007).
Vanderveen, D. K., Mansfield, T. A. & Eichenwald, E. C. Lower oxygen saturation alarm limits decrease the severity of retinopathy of prematurity. J. AAPOS 10, 445–448 (2006).
Carlo, W. A. et al. Target ranges of oxygen saturation in extremely preterm infants. N. Engl. J. Med. 362, 1959–1969 (2010).
Finer, N. N. et al. Early CPAP versus surfactant in extremely preterm infants. N. Engl. J. Med. 362, 1970–1979 (2010).
Stenson, B., Brocklehurst, P. & Tarnow-Mordi, W. Increased 36-week survival with high oxygen saturation target in extremely preterm infants. N. Engl. J. Med. 364, 1680–1682 (2011).
Darlow, B. A. & Morley, C. J. Oxygen saturation targeting and bronchopulmonary dysplasia. Clin. Perinatol. 42, 807–823 (2015).
Todd, D., Cassell, C., Kennedy, J. & John, E. Retinopathy of prematurity in infants < 32 weeks’ gestation at birth in New South Wales in 1993 and 1994. J. Paediatr. Child Health 35, 355–357 (1999).
Allegaert, K., de Coen, K. & Devlieger, H. Threshold retinopathy at threshold of viability: the EpiBel study. Br. J. Ophthalmol. 88, 239–242 (2004).
Hussain, N., Clive, J. & Bhandari, V. Current incidence of retinopathy of prematurity, 1989–1997. Pediatrics 104, e26. https://doi.org/10.1542/peds.104.3.e26 (1999).
Termote, J., Schalij-Delfos, N. E., Brouwers, H. A., Donders, A. R. & Cats, B. P. New developments in neonatology: less severe retinopathy of prematurity?. J. Pediatr. Ophthalmol. Strabismus 37, 142–148 (2000).
Lui, K. et al. Trends in Outcomes for Neonates Born Very Preterm and Very Low Birth Weight in 11 High-Income Countries. J. Pediatr. 215, 32-40.e14 (2019).
Helenius, K. et al. Survival in very preterm infants: an international comparison of 10 national neonatal networks. Pediatrics 140, e20171264. https://doi.org/10.1542/peds.2017-1264 (2017).
Park, J. H., Chang, Y. S., Sung, S. & Park, W. S. Mortality rate-dependent variations in the timing and causes of death in extremely preterm infants born at 23–24 weeks’ gestation. Pediatr. Crit. Care Med. 20, 630–637 (2019).
Kim, J. K., Chang, Y. S., Sung, S. & Park, W. S. Mortality rate-dependent variations in the survival without major morbidities rate of extremely preterm infants. Sci. Rep. 9, 7371. https://doi.org/10.1038/s41598-019-43879-z (2019).
Capasso, L. et al. Oxidative stress and bronchopulmonary dysplasia: evidences from microbiomics, metabolomics, and proteomics. Front. Pediatr. 7, 30. https://doi.org/10.3389/fped.2019.00030 (2019).
Kim, J. K. et al. Trends in survival and incidence of bronchopulmonary dysplasia in extremely preterm infants at 23–26 weeks gestation. J. Korean Med. Sci. 31, 423–429 (2016).
Park, J. H., Chang, Y. S., Sung, S., Ahn, S. Y. & Park, W. S. Trends in overall mortality, and timing and cause of death among extremely preterm infants near the limit of viability. PLoS ONE 12, e0170220. https://doi.org/10.1371/journal.pone.0170220 (2017).
Kim, J. K., Chang, Y. S., Sung, S. & Park, W. S. Trends in the incidence and associated factors of late-onset sepsis associated with improved survival in extremely preterm infants born at 23–26 weeks’ gestation: a retrospective study. BMC Pediatr. 18, 172 (2018).
Zin, A. A., Moreira, M. E., Bunce, C., Darlow, B. A. & Gilbert, C. E. Retinopathy of prematurity in 7 neonatal units in Rio de Janeiro: screening criteria and workload implications. Pediatrics 126, e410-417. https://doi.org/10.1542/peds.2010-0090 (2010).
Saugstad, O. D. Hypoxanthine as an indicator of hypoxia: its role in health and disease through free radical production. Pediatr. Res. 23, 143–150 (1988).
Poggi, C. & Dani, C. Antioxidant strategies and respiratory disease of the preterm newborn: an update. Oxid. Med. Cell. Longev. 2014, 721043. https://doi.org/10.1155/2014/721043 (2014).
Chang, Y. S., Park, H. Y. & Park, W. S. The Korean Neonatal Network: an overview. J. Korean Med. Sci. 30(Suppl 1), S3–S11 (2015).
The international classification of retinopathy of prematurity revisited. Arch. Ophthalmol. 123, 991–999 (2005).
Yoon, B. H. et al. Amniotic fluid interleukin-6: a sensitive test for antenatal diagnosis of acute inflammatory lesions of preterm placenta and prediction of perinatal morbidity. Am. J. Obstet. Gynecol. 172, 960–970 (1995).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 163, 1723–1729 (2001).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Sarkar, S. et al. Screening cranial imaging at multiple time points improves cystic periventricular leukomalacia detection. Am. J. Perinatol. 32, 973–979 (2015).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Funding
This research was supported by a fund (2019-ER7103-00#) from the Research of Korea Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
W.S.P. conceptualized and designed the study and reviewed and revised the manuscript. Y.S.C. coordinated and supervised data collection and critically reviewed the manuscript for important intellectual content. J.H.P. and J.H.H. designed the data collection instruments, collected data, carried out the initial analyses, and drafted the initial manuscript. M.H.L. carried out the statistical analyses. All authors approved the final manuscripts as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, J.H., Hwang, J.H., Chang, Y.S. et al. Survival rate dependent variations in retinopathy of prematurity treatment rates in very low birth weight infants. Sci Rep 10, 19401 (2020). https://doi.org/10.1038/s41598-020-76472-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-76472-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.