Abstract
Visceral adiposity index (VAI) has been associated with various cardio-metabolic diseases; however, there is limited information about its association with cerebrovascular diseases. In this study, we evaluated the relationship between VAI and silent brain infarct (SBI). We evaluated a consecutive series of healthy volunteers over the age of 40 between January 2006 and December 2013. SBI was defined as an asymptomatic, well-defined lesion with a diameter ≥ 3 mm with the same signal characteristics as the cerebrospinal fluid. VAI was calculated using sex-specific equations as described in previous studies. A total of 2596 subjects were evaluated, and SBI was found in 218 (8%) participants. In multivariable analysis, VAI (adjusted odds ratio [aOR] = 1.30; 95% confidence interval [CI] 1.03–1.66; P = 0.030) remained a significant predictor of SBI after adjustment for confounders. The close relationship between VAI and SBI was prominent only in females (aOR = 1.44; 95% CI 1.00–2.07; P = 0.048). In the evaluation between VAI and the burden of SBI, VAI showed a positive dose–response relationship with the number of SBI lesions (P for trend = 0.037). High VAI was associated with a higher prevalence and burden of SBI in a neurologically healthy population.
Similar content being viewed by others
Introduction
Global obesity rates are currently increasing1, leading to serious health complications worldwide that include cardio/cerebrovascular diseases, atherosclerosis, and subclinical inflammation1,2. However, such obesity-related complications do not occur in all obese patients and vary depending on individual characteristics3,4. In recent years, it has been recognized that the distribution of fat plays a substantially more important role in obesity-related complications than dose the amount of total fat5,6,7. Visceral adipose tissue (VAT) has been shown to be associated with the risk of insulin resistance and cardio/cerebrovascular disease6,8,9, whereas subcutaneous adipose tissue (SAT) appears to be less influential and even rather protective6,10. Therefore, instead of using the traditional body mass index (BMI), various indicators reflecting fat distribution differences across individuals have been developed and used.
For accurate measurements of the distribution and amount of fat, imaging modalities such as magnetic resonance imaging (MRI) and computed tomography (CT) have been used11,12. However, as shown in recent studies on “metabolically healthy obesity”, in addition to problems with quantity of adipose tissue, functional aspects such as the presence of accompanying metabolic diseases must be considered1,4. On this theoretical basis, Amato et al. developed a sex-specific index for predicting VAT mass and function using waist circumference (WC), BMI, triglyceride (TG), and high-density lipoprotein (HDL) cholesterol 8. This visceral adiposity index (VAI) was closely associated with metabolic disease, cardiovascular disease, and even atherosclerosis10,11,12,13,14. However, studies on cerebrovascular disease is still lacking.
Silent brain infarct (SBI) is a subclinical pathological condition that is commonly found in elderly individuals15,16. SBI itself is asymptomatic but increases the risk of subsequent strokes16. Therefore, a clear understanding of the pathological mechanisms and risk factors of SBI may be helpful in the primary prevention of cerebrovascular disease in the subclinical stage. In this study, we evaluated the relationship between VAI and SBI in a neurologically healthy population to gain insight into underlying pathological mechanisms.
Results
A total of 2596 neurologically healthy participants (mean age 56 ± 7 years, male sex: 54%) were included. SBI was found in 218 (8%) participants, and the mean VAI was 1.66 ± 1.33. Other detailed baseline characteristics are presented in Supplementary Table 1.
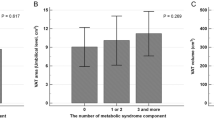
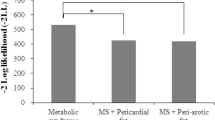
Univariate analysis showed that SBI was significantly associated with age, hypertension, diabetes, use of antiplatelet agents and antihypertensives, systolic and diastolic BP, hemoglobin A1c level, VAT, TAT, and VAI (Table 1). In a multivariable logistic regression analysis to find possible predictors for SBI, VAI remained significant after adjusting for confounders [adjusted odds ratio (aOR) = 1.30; 95% confidence interval (CI) 1.03–1.66; P = 0.030]. Age and hypertension were also positively associated with SBI, independent of VAI (Fig. 1). VAI even showed a dose–response relationship according to the number of SBI lesions (P for trend = 0.037) (Fig. 2). On the other hand, VAT did not show any statistically significant association with SBI (aOR = 1.29; 95% CI 0.94–1.77; P = 0.121) (Fig. 1).
Multivaraible logistic regression analysis of possible predictors for silent brain infarct and subgroup analysis stratified by sex. In multivariable analysis, VAI (adjusted odds ratio [aOR] = 1.30; 95% confidence interval [CI] 1.03–1.66; P = 0.030) was associated with SBI after adjustment for confounders. On the other hand, VAT did not show any statistically significant association with SBI (aOR = 1.29; 95% CI 0.94–1.77; P = 0.121). This close relationship was prominent only in females (aOR = 1.44; 95% CI 1.00–2.07; P = 0.048), while no statistical significance was found in males.
Distribution of median visceral adiposity index (VAI) according to the burden of silent brain infarct (SBI). Patients with multiple SBI lesions had a higher VAI as compared to those with absent or a single lesion in a dose–response manner (P for trend = 0.037). This tendency was more pronounced in female participants (P for trend = 0.009) and not in male participants (P for trend = 0.643).
The close relationship between VAI and SBI was prominent only in females, both in their prevalence (aOR = 1.44; 95% CI 1.00–2.07, P = 0.048) and burden (P for trend = 0.009) (Figs. 1 and 2). Meanwhile, no statistical significance was found in male participants. These sex differences can be interpreted based on the results shown in Table 2. For most risk factors, similar results were found between male and female participants, but VAI was more strongly associated with hypertension or diabetes in female participants. Notably, males had a negative correlation between VAI and age, whereas females had a positive correlation (Table 2).
The reason why the direction of association between age, the most powerful risk factor for SBI, and VAI was apposite in male and female can be explained by the apposite change of anthropometric indices level as aging in both sex (Table 3). Male participants showed a decrease in anthropometric indices (e.g., BMI and SAT) as they grew older, while an increase was seen in females (e.g., BMI, WC, VAT, and TAT) (Table 3).
Discussion
In this study, we found that high VAI level was associated with both SBI prevalence and burden in a neurologically healthy population, while VAT area was not. Our findings suggest that VAI which encompasses metabolic susceptibility caused by visceral adiposity is more relevant predictor for SBI than simple VAT quantity. These meaningful findings were found only in female participants, consistent with previous studies13,17,18.
Although the exact pathological mechanisms underlying the relationship between VAI and SBI is not clear. Several plausible mechanisms can be considered. First, this may be due to synergistic effects of well-known risk factors included in the VAI calculation formula 8. High TG, low HDL cholesterol, and high WC are all well-known cerebrovascular risk factors19,20,21. Thus, the VAI developed from these combinations may be more strongly associated with SBI than for each individual risk factor. Second, the effects of metabolic comorbidities cannot be ignored. The aforementioned lipid profiles exhibited by high VAI are also called “atherogenic dyslipidemia”, a common finding in visceral obesity, insulin resistance, and metabolic syndrome12,22. Indeed, in both previous studies and our findings (Table 2), VAI has shown to be closely associated with metabolic diseases such as hypertension and diabetes, each of which is a major risk factor for SBI8,9,10,14,23. Third, endothelial dysfunction due to subclinical inflammation may be the main cause. Adipose tissue is not just a storage organ that actively releases various hormones or substances6. In particular, VAT tends to secrete more pro-inflammatory adipokines (e.g., IL-6, IL-8, TNF-a, and PAI-1) than SAT12,23,24,25. Therefore, subclinical inflammation might be severe in patients with high VAI5, which mainly reflects the function of VAT. This could be partly confirmed by the close relationship between VAI and WBC, hs-CRP, homocysteine in Table 2. Endothelial dysfunction in small arteries/arterioles may cause their occlusion or block perivascular glymphatic drainage, resulting in SBI development15,26. Lastly, high VAI can indicate an underlying higher atherosclerosis burden. Previous studies have shown that VAI is associated with intra- and extracranial atherosclerosis3,5,13, probably due to the aforementioned atherogenic dyslipidemia or subclinical inflammation. Advanced atherosclerotic lesions can develop SBI with chronic diffuse hypoperfusion and extravasation of toxic metabolites into neural tissues15,26.
Perhaps, the most interesting finding in this study is that even though VAI was created by adjusting for sex differences8, it is meaningful only in females. Previous studies investigating atherosclerosis or cardiovascular diseases have shown similar results, but the cause of these results is not clear13,17,18. They speculate that the hormonal difference between males and females or differences in composition of VAT and SAT underlie these results17. Based on our findings, we propose a slightly different reason. Firstly, the relationship between age and VAI may affect this sexual difference. Age is the strongest risk factor for cerebrovascular disease, including SBI. As shown in Tables 2 and 3, there is no significant increase in VAT with age in male patients, but rather a negative relationship between VAI and age with decreasing SAT. On the other hand, as females get older, anthropometric indicators (e.g., WC, VAT, and TAT) increase markedly and VAI increases. As a result, in females, VAI also serves as an indicator of age and may have more pronounced results. In addition, females had a lower prevalence of metabolic disease, but association between metabolic disease and VAI was stronger than in males (Table 2 and Supplementary Table 1). In other words, visceral obesity is more likely to be involved in the development of potent risk factors such as hypertension and diabetes, and there are fewer other confounders that can influence VAI’s impact on SBI. This may make VAI more influential in females.
In addition, our study presents two more interesting insights. First, VAI had a stronger predictive power on the prevalence of SBI than VAT. This may indicate that functional activity is more important than the amount of visceral fat5,10,14, and is consistent with recent recognition that metabolic status is more important than the severity of obesity4. Second, the cut-off value of VAI considering sensitivity and specificity for SBI prediction in our data was 1.22. The value is lower than the cut-off value of previous studies about the relationship with metabolic syndrome or cardiovascular disease10,14, but similar to those dealing with subclinical atherosclerosis12,13. These results indicate that subclinical pathology is also being carried out in patients with a VAI value of less than 2.00 which was thought to be traditional “normal range”, and that screening brain MRI and MRA may be required.
There are several caveats to interpret our findings. First, the current study is a retrospective observational study. We included a relatively homogeneous and large population; however, the possibility of selection bias still remains. Second, due to the limitations of cross-sectional analysis, we could only prove the association, not causality. Further prospective studies are needed to confirm our results. Third, because we only included a healthy population, the prevalence of SBI and cardiovascular risk factors were relatively small. Therefore, the results of this study cannot be easily generalized and applied to clinical fields. However, despite the small number of outcome events, VAI and SBI showed a strong relationship.
We demonstrated that high VAI level is associated with SBI prevalence and burden in a neurologically healthy population, especially in females. VAI can be calculated from the results of simple laboratory examinations commonly used in the clinical fields, and its predictive power for SBI is superior to VAT in our data. Thus, our findings indicate that VAI could be used as a simple and convenient predictive marker for the prevalence and burden of SBI.
Methods
Patients and population
From a consecutive registry of health check-ups at Seoul National University Hospital Health Promotion Center between January 2006 and December 2013, we retrospectively included subjects over the age of 40 years (n = 2904). Among them, 49 participants who had a history of stroke or clinically meaningful neurological deficit were excluded. Participants using lipid lowering agents (n = 219) and having missing data regarding covariates (n = 40) were also excluded. Finally, a total of 2596 neurologically healthy participants were included in the final cross-sectional analyses.
This retrospective cross-sectional study was approved by the Institutional Review Board (Number: H-1502-026-647) at Seoul National University Hospital. Requirement of informed consent from participants was waived by the Institutional Review Board of Seoul National University Hospital due to the retrospective study design using anonymized information. All experiments were performed in accordance with the Declaration of Helsinki and relevant guidelines and regulations.
Clinical assessment
As part of routine health check-ups, we evaluated demographic factors, clinical factors, and cardiovascular risk factors in all participants. Age, sex, BMI, hypertension, diabetes, ischemic heart disease, current smoking, use of medications (e.g., antiplatelet agents, antihypertensives, and glucose lowering agents), systolic and diastolic blood pressure (BP) were assessed4,6. Laboratory examinations were conducted after 12 h overnight fasting, including glucose profiles, lipid profiles, white blood cell (WBC) counts, high-sensitivity C-reactive protein (hs-CRP) and homocysteine levels4,6.
The VAI was calculated using the sex-specific equations as described in previous studies: VAI = [WC/(39.68 + 1.88 × BMI)] × (TG/1.03) × (1.31/HDL cholesterol) for males and VAI = [WC/(36.58 + 1.89 × BMI)] × (TG/0.81) x (1.52/HDL cholesterol) for females8.
Radiological assessment
All participants underwent brain MRI using 1.5-T MR scanners (SIGNA [GE Healthcare, Milwaukee, WI, USA] or Magnetom SONATA [Siemens, Munich, Germany]). The detailed descriptions of MRI acquisitions were as follows: basic slice thickness, 5 mm; T1-weighted images, repetition time (TR)/echo time (TE) = 500/11 ms; T2-weighted images, TR/TE = 5000/127 ms; T2-gradient echo images, TR/TE = 57/20 ms; and T2 fluid-attenuated inversion recovery images, TR/TE = 8800/127 ms. SBI was defined as asymptomatic, well-defined lesions, > 3 mm in size with the same signal characteristics as cerebrospinal fluid on T1 and T2 images4,15. We also rated the burden of SBI as absent, single, or multiple, based on their number4.
In this dataset, most participants (n = 2136) conducted abdominal fat CT scans using a 16-detector row CT scanner (Somatom Sensation 16, Siemens Medical Solutions, Forchheim, Germany)6. To obtain the adipose tissue area, we used a technique that we have previously validated6. We first obtained a single slice at the umbilicus level at 5 mm thickness with a scan time of 0.5 s. Then, we calculated the cross-sectional surface area (in cm2) of the different abdominal compartment using commercially available CT software (Rapidia 2.8; INFINITT, Seoul, Korea)6. The adipose tissue area was determined electronically using the setting of attenuation levels from -250 to -50 Hounsfield units. VAT was identified as the intra-abdominal fat that was surrounded by the parietal peritoneum or transversalis fascia, and excluding the vertebral column and paraspinal muscles. SAT was calculated by subtracting the VAT from the total adipose tissue (TAT) area6.
Statistical analysis
We performed all statistical analyses using SPSS version21.0 (IBM SPSS, Chicago, IL, USA). Univariate analyses for assessing possible predictors for SBI were performed using Student’s t-test or Mann–Whitney u-test for continuous variables and Chi-squared test or Fisher’s exact test for categorical variables. Variables with severely skewed data were transformed into a log scale. Based on the results of univariate analysis, variables with P < 0.10 were introduced into the multivariable logistic regression analysis. We wondered how the VAI was related to the burden as well as to the prevalence of SBI, and compared the median VAI values according to the SBI burden using the Jonckheere–Terpstra test (P for trend.). In addition, we conducted additional sensitivity analyses to compare the predictive power between VAI and VAT on fat CT.
Males and females differ in composition of VAT and SAT6. Thus, VAI was formulated differently for males and females in consideration of sex differences8. Nevertheless, previous studies have shown that VAI is more influential in females13,17,18. We, therefore, conducted a stratified multivariable analysis by sex to confirm these results. All variables with P < 0.05 were considered significant in this study.
References
Hinnouho, G.-M. et al. Metabolically healthy obesity and risk of mortality: Does the definition of metabolic health matter?. Diabetes Care 36, 2294–2300 (2013).
Bradshaw, P. T., Monda, K. L. & Stevens, J. Metabolic syndrome in healthy obese, overweight, and normal weight individuals: the atherosclerosis risk in communities study. Obesity 21, 203–209 (2013).
Yang, F. et al. Visceral adiposity index may be a surrogate marker for the assessment of the effects of obesity on arterial stiffness. PLoS ONE 9, e104365 (2014).
Nam, K.-W. et al. Obesity without metabolic disorder and silent brain infarcts in aneurologically healthy population. Int. J. Obes. 44, 1–6 (2019).
Randrianarisoa, E. et al. Visceral adiposity index as an independent marker of subclinical atherosclerosis in individuals prone to diabetes mellitus. J. Atheroscler. Thromb. 26, 821–834 (2019).
Nam, K.-W. et al. Abdominal fatness and cerebral white matter hyperintensity. J. Neurol. Sci. 404, 52–57 (2019).
Alberti, K. et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 120, 1640–1645 (2009).
Amato, M. C. et al. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 33, 920–922 (2010).
Borruel, S. et al. Surrogate markers of visceral adiposity in young adults: waist circumference and body mass index are more accurate than waist hip ratio, model of adipose distribution and visceral adiposity index. PLoS ONE 9, e114112 (2014).
Amato, M. C., Giordano, C., Pitrone, M. & Galluzzo, A. Cut-off points of the visceral adiposity index (VAI) identifying a visceral adipose dysfunction associated with cardiometabolic risk in a Caucasian Sicilian population. Lipids Health Dis. 10, 183 (2011).
Han, L. et al. Visceral adiposity index score indicated the severity of coronary heart disease in Chinese adults. Diabetol. Metab. Syndrome 6, 143 (2014).
Park, H.-J. et al. Increased risk of subclinical atherosclerosis associated with high visceral adiposity index in apparently healthy Korean adults: the Kangbuk Samsung Health Study. Ann. Med. 48, 410–416 (2016).
Li, R. et al. Visceral adiposity index, lipid accumulation product and intracranial atherosclerotic stenosis in middle-aged and elderly Chinese. Sci. Rep. 7, 1–9 (2017).
Dereziński, T., Zozulińska-Ziółkiewicz, D., Uruska, A. & Dąbrowski, M. Visceral adiposity index as a useful tool for the assessment of cardiometabolic disease risk in women aged 65 to 74. Diabetes Metab. Res. Rev. 34, e3052 (2018).
Wardlaw, J. M. et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 12, 822–838 (2013).
Vermeer, S. E., Longstreth, W. T. Jr. & Koudstaal, P. J. Silent brain infarcts: a systematic review. Lancet Neurol. 6, 611–619 (2007).
Nakagomi, A., Sunami, Y., Kawasaki, Y., Fujisawa, T. & Kobayashi, Y. Sex difference in the association between surrogate markers of insulin resistance and arterial stiffness. J. Diabetes Complicat. 34, 107442 (2019).
Mohammadreza, B., Farzad, H. & Davoud, K. Prognostic significance of the complex" visceral adiposity index" vs. simple anthropometric measures: Tehran lipid and glucose study. Cardiovasc. Diabetol. 11, 20 (2012).
Freiberg, J. J., Tybjærg-Hansen, A., Jensen, J. S. & Nordestgaard, B. G. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA 300, 2142–2152 (2008).
Furukawa, Y. et al. The relationship between waist circumference and the risk of stroke and myocardial infarction in a Japanese urban cohort: the Suita study. Stroke 41, 550–553 (2010).
Wannamethee, S. G., Shaper, A. G. & Ebrahim, S. HDL-cholesterol, total cholesterol, and the risk of stroke in middle-aged British men. Stroke 31, 1882–1888 (2000).
Grundy, S. M. Small LDL, atherogenic dyslipidemia, and the metabolic syndrome. Circulation 95, 1–4 (1997).
Ding, Y. et al. Significantly increased visceral adiposity index in prehypertension. PLoS ONE 10, e0123414 (2015).
Després, J. P. Is visceral obesity the cause of the metabolic syndrome?. Ann. Med. 38, 52–63 (2006).
Farb, M. G. et al. Arteriolar function in visceral adipose tissue is impaired in human obesity. Arterioscler. thromb. Vasc. Biol. 32, 467–473 (2012).
Pantoni, L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 9, 689–701 (2010).
Author information
Authors and Affiliations
Contributions
Study concept and design: K.-W.N., H.-M.K., and J.-H.P.; Acquisition, analysis, or interpretation of data: K.-W.N., H.-Y.J., HT.K., S.-M.J., and H.-J.K.; Drafting of the manuscript: K.-W.N.; Critical revision of the manuscript for important intellectual content: H.-M.K. and J.-H.P.; Statistical analysis: K.-W.N.; Obtained funding: not applicable; Supervision: H.-M.K. and J.-H.P.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nam, KW., Kwon, HM., Jeong, HY. et al. Visceral adiposity index is associated with silent brain infarct in a healthy population. Sci Rep 10, 17271 (2020). https://doi.org/10.1038/s41598-020-74454-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-74454-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.