Abstract
To assess the role of sentinel lymph-node biopsy (SLNB) and FDG-PET in staging and radiation treatment (RT) of anal cancer patients. This retrospective study was performed on 80 patients (male: 32, female: 48) with a median age of 60 years (39–89 years) with anal squamous cell carcinoma who were treated from March 2008 to March 2018 at the IRCCS San Raffaele Hospital. Patients without clinical evidence of inguinal LNs metastases and/or with discordance between clinical evidence and imaging features were considered for SLNB. FDG-PET was performed in 69/80 patients. Patients with negative imaging in inguinal region and negative SLNB could avoid RT on groin to spare inguinal toxicity. CTV included GTV (primary tumour and positive LNs) and pelvic ± inguinal LNs. PTV1 and PTV2 corresponded to GTV and CTV, respectively, adding 0.5 cm. RT dose was 50.4 Gy/28 fractions to PTV2 and 64.8 Gy/36 fractions to PTV1, delivered with 3DCRT (n = 24) or IMRT (n = 56), concomitant to Mitomycin-C and 5-FU chemotherapy. FDG-PET showed inguinal uptake in 21/69 patients (30%) and was negative in 48/69 patients (70%). Lymphoscintigraphy was performed in 11/21 positive patients (4 patients SLNB confirmed inguinal metastases, 6 patients false positive and 1 patient SLN not found), and in 29/48 negative patients (5/29 showed metastases, 23/29 true negative and 1 SLN not found). Sensitivity, specificity, positive and negative predictive value of FDG-PET were 62%, 79%, 40% and 82%, respectively. Median follow-up time from diagnosis was 40.3 months (range: 4.6–136.4 months): 69 patients (86%) showed a complete response, 10 patients (13%) a partial response, 1 patient (1%) a stable disease. Patients treated on groin (n = 54) versus not treated (n = 26) showed more inguinal dermatitis (G1–G2: 50% vs. 12%; G3–G4: 17% vs. 0%, p < 0.05). For patients treated on groin, G3–G4 inguinal dermatitis, stomatitis and neutropenia were significantly reduced with IMRT against 3DCRT techniques (13% vs. 36%, p = 0.10; 3% vs. 36%, p = 0.003; 8% vs. 29%, p = 0.02, respectively). SLNB improves the FDG-PET inguinal LNs staging in guiding the decision to treat inguinal nodes. IMRT technique significantly reduced G3-G4 toxicities when patients are treated on groin.
Similar content being viewed by others
Introduction
Squamous cell carcinoma (SCC) of the anal canal is a relatively uncommon tumour constituting only 4% of all lower alimentary tract and 2% of all digestive system malignancies. The tumour size (T stage) and the nodal status are recognized as the main prognostic factors1. Chemo-radiotherapy (CRT) is the standard treatment for anal SCC; whereas mesorectal and internal iliac lymph nodes (LNs) are routinely included in the radiation fields, the need of prophylactic inguinal irradiation is controversial.
Accurate staging is crucial for radiotherapy (RT) treatment planning, aiming to select patients with localized disease. Fifteen-25% of patients with anal cancer show inguinal LNs metastases, while 44% of all LNs with positive metastases were reported to be smaller than 5 mm2 and this is the main reason explaining the low sensitivity of either clinical examination in the detection of positive inguinal LNs.
In a retrospective analysis of 270 patients who did not receive prophylactic inguinal irradiation, after a median follow-up of 72 months, the incidence of inguinal metastases was 8%3. Two retrospective studies reported the inguinal recurrence rate in patients staged with conventional examinations who did not receive prophylactic inguinal irradiation: Blinde et al.4 showed inguinal recurrence rate of 0% in T1, 10% in T2 and 20% in T3–T4 patients with a median follow-up of 65 months, and Ortholan et al.5 reported an inguinal recurrence rate of 12% for T1–T2, and 30% for T3–T4 patients with a median follow-up of 61 months. As a consequence, the prescription of prophylactic inguinal irradiation based only on the T stage would cause an unnecessary irradiation of about 70–80% of T3–T4 patients, submitting them to a risk of severe acute toxicity, especially when using conformal RT techniques6. Conversely, about 10% of T1-T2 patients would be undertreated if inguinal irradiation is not prescribed. Thus, a better detection of initial inguinal LNs involvement would be important for selecting those patients who really deserve the inguinal irradiation. Recently, FDG-PET was shown to detect more abnormal inguinal LNs than clinical7, ultrasound inguinal8 or CT9,10,11 examination while sentinel lymph-node biopsy (SLNB) has been shown to be superior to both CT and FDG-PET in detecting metastatic LNs12.
Prophylactic RT including inguinal LNs irradiation was shown to decrease inguinal metastasis in several series3,5 but is unavoidably associated with increased toxicity. Better patient selection and the use of advanced RT techniques, such as intensity modulated RT (IMRT) and image guided RT (IGRT), may reduce toxicity13.
In the present study we reported our experience about the role of SLNB compared to FDG-PET in terms of disease staging and the clinical impact of inguinal irradiation with the use of advanced RT techniques.
Methods and materials
Characteristics of patients
Eighty patients with histologically proven anal SCC treated between March 2008 and March 2018 were enrolled in a retrospective study. Patients’ ages ranged from 39 to 89 years with a median of 60 years. Of these 32 (40%) were male and 48 (60%) were female. Only 27/80 (34%) were HIV positive, and 21/27 (78%) were male. The main characteristics of patients are summarized in Table 1.
Patients underwent complete workup with full physical examination (anorectal, vaginal, and inguinal sites), proctoscopy or colonoscopy, chest-abdomen CT and pelvic MRI. Patients with T1N+, T2–T4 with any N, M0, Karnofsky performance status ≥ 70, adequate bone marrow, renal and hepatic function were candidate to CRT. TNM staging was T1 in 14, T2 in 30, T3 in 24 and T4 in 12 patients due to involvement of vagina (n = 8), prostate (n = 3) and uterus (n = 1). N staging was N0: 29, N1: 17, N2: 14, and N3:20 patients.
Seven patients with limited metastatic disease were enrolled after collegial discussion and approval, despite the protocol violation (3 patients: external iliac LNs, 2 patients: liver (1 patient: liver + bone), 2 patients: retroperitoneal LNs). The protocol was approved by our Institutional Ethical Committee (IRCCS San Raffaele Hospital Clinical Research Office), and all patients signed an informed consent. A retrospective comparison between FDG-PET inguinal LNs evaluation and SLNB results was made.
SLNB protocol and treatment
Patients without clinical evidence of inguinal LNs involvement or with discordance between diagnostic imaging and clinical examination were considered for the SLNB protocol. The SLNB is a minimally invasive procedure which consists in submucosal injection of Technetium-99 labelled radio colloid around the primary tumour, patients in whom inguinal tracer uptake is detected undergo radio guided surgical removal of the inguinal sentinel LNs.
The methods relative to lymphoscintigraphy, surgical removal and histopathological examination of sentinel LNs have been already described14,15. Patients after positioning in supine position on Comby-Fix® underwent a contrast-enhanced CT and FDG-PET simulation. FDG-PET was used both for staging and target definition. CTV included the GTV (primary tumour and any positive LNs), the ischiorectal fossa, the mesorectum, and the internal and common iliac LNs until the L5-S1 space.
As the inguinal LNs irradiation is the standard treatment in anal cancer, all patients enrolled in this study with positive SLNB were treated on groin. Patients who had negative SLNB and negative imaging in inguinal region were considered for RT without groin irradiation, so as to spare inguinal toxicity; patients were also involved in the final clinical decision. PTV1 and PTV2 were defined as GTV and CTV, expanded with a margin of 0.5 cm, respectively. Median prescribed dose was 50.4 Gy in 28 fractions (1.8 Gy/fraction) to the PTV2, and 64.8 Gy in 36 fractions, delivered as sequential or concomitant boost, to the PTV1. RT techniques consisted of 3DCRT or IMRT (Volumetric Modulated Arc Therapy (VMAT) Rapid Arc or Helical Tomotherapy). The planned concomitant chemotherapy schedule was continuous infusion 5-FU 1,000 mg/mq2 delivered from day 1 to 4 and from day 29 to 32 combined to Mitomycin-C 10 mg/m2 delivered on day 1 to 29.
Analyses
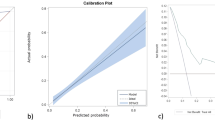
Sensitivity, specificity, area under the curve (AUC), positive and negative predictive values of FDG-PET against SLNB were assessed in the subgroup of patients that performed both examinations.
Acute toxicities were scored according to the NCI-CTC for Adverse Events (Version 3); treatment interruptions were also reported. In order to assess the gain in avoiding to treat the inguinal LNs, a comparison in terms of inguinal LNs outcome and toxicity was made between the inguinal RT “IRT” and non-inguinal RT “NIRT” groups, also taking into account RT technique (3DCRT vs. IMRT).
The differences between proportions (“IRT” vs. “NIRT”, 3DCRT vs. IMRT) were tested by the two-tailed Fisher exact test.
Time to progression (TTP) was calculated from the end of treatment and overall survival (OS) from the time of diagnosis to progression, last follow-up or death. Survival outcomes were evaluated using the Kaplan–Meier method. Statistical analyses were performed using MedCalc software (Version 12.1.4, MedCalc, Ostend, Belgium).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Research Committee and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Results
Comparison between FDG-PET data and SLNB
Sixty-nine/80 patients (86%) underwent FDG-PET that showed inguinal uptake in 21/69 patients (30%). Lymphoscintigraphy was performed in 11/21 (52%) patients: SLNB confirmed inguinal metastases in 4/10 patients (40%), 6/10 patients (60%) were false positive and SLN was not found in 1 patient. FDG-PET was negative in 48/69 patients (70%): lymphoscintigraphy was performed in 29/48 PET-negative patients: 5/28 (18%) showed metastasis despite the PET result, 23/28 (82%) were true negative and SLN was not found in 1 patient. The comparison between FDG-PET inguinal uptakes and SLNB is reported in Table 2.
The resulting sensitivity, specificity, positive and negative predictive value of FDG-PET were 62%, 79%, 40% and 82%, respectively as reported in Table 3.
Treatment feasibility
All patients received the planned dose of 50.4 Gy in 28 fractions to the pelvis and ischiorectal fossa. The median dose of boost to T stage was 64.8 (61.4–72.4 Gy). Fifty-four/80 patients received prophylactic (n = 34) or curative (n = 20) inguinal irradiation (the “IRT” group) and 26/80 patients did not (the “NIRT” group). Boost was delivered sequentially in 96% of patients and concomitant in the remaining 4%. The median dose to the “IRT” group was 50.4 Gy (50.4–70.2 Gy). Twenty-five/26 patients of the “NIRT” group underwent SLNB procedure: 24/25 patients with histologically negative SLNB (2/24 patient with FDG-PET, MRI and CT negative), and 1/25 SLN not found.
In the “NIRT” group the percentage of patients with T1-T2 disease was higher than the percentage of patients with T3–T4 (73% vs. 27%, p = 0.002), while in the “IRT” group the rates were similar (53% vs. 47%, respectively), as reported in Table 4.
For N staging we took into account any information from CT, MRI and FDG-PET. In the “NIRT” group the percentage of N0-N1 was higher than the percentage of N2–N3 (77% vs. 23%, p = 0.0003), while in “IRT” they were similar (52% vs. 48%), as reported in Table 4.
Mean duration of RT was 58 days (36–88 days): 42 patients (53%) needed a temporary suspension of RT (“IRT”: 29 patients and “NIRT”: 13 patients). Mean duration of suspension was 11 days (2–38 days); the mean duration in “IRT” was 11 days (2–38 days) and 12 days (3–23 days) in “NIRT”. Mean dose to suspension: 37.7 Gy (16.2–55.8 Gy) (“IRT”: 34.4 Gy (16.2–55.8 Gy) and “NIRT”: 44.7 Gy (34.2–57.6 Gy)).
RT was delivered with 3DCRT in 24/80 patients (30%), 14/24 patients in the “IRT” group and 10/24 patients in the “NIRT” group. Fifty-six/80 (70%) patients were treated with IMRT: 18/80 patients (22%) were treated with Tomotherapy, (“IRT”: 14/18; “NIRT”: 4/18); 38/80 patients (47%) with VMAT (“IRT”: 26/38; “NIRT”:12/38).
Concomitant Mitomycin-C and 5-FU was prescribed for 71/80 patients (89%), 2/80 patients (2.5%) received only Capecitabine and other 2/80 patients (2.5%) received Cisplatine. Median cycle of chemotherapy was 2 cycles (1 to 4 cycles). The 5/80 remaining patients (6%) who did not received concomitant chemotherapy: 3/5 patients were affected by hepatic cirrhosis and 2/5 patients were > 80 years old.
Toxicity
There was no significant difference between G1–G2 and G3–G4 toxicities in “IRT” group compared to “NIRT” group except for inguinal dermatitis, as expected (G1–G2: 27/54 patients (50%) vs. 3/26 patients (12%), p = 0.001; and G3–G4: 9/54 patients (17%) vs. 0/26 patients (0%) (p = 0.03)). Toxicity data are reported in Table 5. When comparing 3DCRT vs. IMRT, for diarrhoea and stomatitis the differences in term of G1–G4 toxicities were statistically significant (21/24 (88%) vs. 26/56 (46%), p < 0.01; and 11/24 (46%) vs. 2/56 (4%), p < 0.01). Moreover, in patients treated on groin, IMRT showed reduced G3–G4 inguinal toxicity (5/40 (13%) vs. 5/14 (36%), p = 0.10) stomatitis (1/40 (3%) vs. 5/14 (36%), p = 0.003) and neutropenia (3/40 (8%) vs. 4/14 (29%), p = 0.02) compared to 3DCRT, as reported in Table 6.
Outcome
Sixty-nine/80 patients achieved the complete response, 10/80 patients had a partial remission and 1/80 patient had stable disease. Nineteen/80 patients had progression disease, 8/19 had local relapse (5/8: only local relapse, 3/8: local + distant relapse), and 11/19 had only distant relapse. No patient treated or not on groin experienced inguinal relapse. Sixty-four/80 patients are alive and 16/80 patients died for progression disease at the last follow-up.
Median time to local relapse was 38.9 months (4.8–123.2 months). Median time to progression was 35.2 months (3.0–133.0 months), excluded patients with metastasis at the time of diagnosis. Median OS from the time of diagnosis was 40.3 months (4.6–136.4 months), 46/80 patients (58%) achieved a 3 years OS and 32/80 patients (40%) were alive at 5 years from the end of treatment. Nine/80 patients underwent surgery (7/9 abdominal-perineal amputation, 2/9 tumour resection), mean time to surgery was 12.1 months (3.1–23.3 months).
Discussion
CRT is the standard treatment for anal SCC. The indication of prophylactic inguinal irradiation is, however, controversial. According to the two largest retrospective studies4,5 it is clear that treating or not the inguinal LNs based only on the T stage has a large risk of over/under-treatment. A better detection of early inguinal LNs involvement could properly select patients who really deserve inguinal irradiation.
FDG-PET detects more abnormal inguinal LNs than clinical examination7, inguinal ultrasound8, and CT9,10,11, and, more in general, changing the TMN stage in 41% of patients with anal cancer; thus it has been recommended for the initial staging16. The low incidence of metachronous metastases and the side effects after radiotherapy could not justify a prophylactic treatment. A refined staging system with precise identification of disease extent could allow individualized therapy, ensuring the accurate coverage of disease while sparing disease-free organs. Feasibility and efficacy of SLNB has been addressed by several reports and the clinical utility of this procedure in improving disease staging and selecting patients for inguinal radiation and changing the therapeutic plan has also been outlined14,15.
To our knowledge, only the study by Mistrangelo et al.1 compared FDG-PET and SLNB in 27 patients. Pathologic inguinal uptake was found in 7 patients. SLNB confirmed inguinal metastases in 3/7 (42%) vs. our 4/10 (40%) patients, with 4/7 (57%) false positives vs. 6/10 (60%) in our patients, and did not show inguinal metastases in the 20 patients with no pathologic inguinal uptake. They reported positive and negative predictive value equal to 43% and 100% respectively, quite consistent with the values found in current study (40% and 82%, respectively (Table 3), although, differently from our findings which showed 18% of false PET negative they did not report any false PET negative.
Engledow et al.17 reported pathologic inguinal uptake in 9/40 patients. Fine needle aspiration or conventional histology confirmed inguinal metastases in 7/9 (78%) patients. Despite the relatively small number of patients of these studies and of our, results are quite consistent and show that: a) despite recommended for initial staging, the FDG-PET results on inguinal LNs should be interpreted with caution, showing a large number of false positives; b) SLNB can further improve inguinal staging reducing FDG-PET false positive and false negative rates. In the present study FDG-PET importantly showed a false positive rate of 60% (6/10 patients), and a false negative rate of 18% (5/28 patients) when compared to SLNB.
For these reasons, SLNB can be considered as a good tool when comparing new modalities such as FDG-PET.
In particular, the reduction of the false negative rate could be very important, especially in case of stage T1-T2, as a positive SLNB would possibly suggest the radiation oncologist to treat the groins even in presence of a negative FDG-PET. Mistrangelo et al.12 reviewed the literature and found 6 studies reporting SLNB positivity rate stratified by T stage: summing his results to the data from all these studies, SLNB found metastases in 6/27 (22%) T1 patients and in 17/98 (17%) T2 patients. In our population, selecting T1 and T2 patients without considering N stage, SLNB found metastasis in 2/14 (14%) and 6/30 (20%) patients, respectively. Considering patients with T1 and T2 N0 stage at diagnostic imaging, who would probably be selected to skip inguinal RT, SLNB showed metastases in 1/9 (11%) and 1/12 (8%) patients, respectively. In short, with the limitation of the small number of patients in the present study and in literature, SLNB seems to be the most effective procedure to select patients for inguinal RT.
Interestingly, with a median OS of 48.5 months (1.3–109.2 months) none of the 26/80 patients, who did not receive inguinal irradiation, had inguinal relapse. Considered that the median time of inguinal recurrence has been reported to be around 16 months3, the absence of inguinal relapse in the “NIRT” group indicates that SLNB is likely to be able to identify the true negative patients.
Another relevant issue concerns the impact of advanced RT techniques in sparing the normal tissues with/without treating the inguinal LNs. In the current study, the only significantly toxicity more frequent in the “IRT” group versus “NIRT” group was the inguinal dermatitis. Interestingly, the increase of inguinal dermatitis in the “IRT” group did not translate in an increased rate of treatment suspension, neither of the duration of the suspension compared to “NIRT” group. It is important to note that the median dose to suspension was 37.7 Gy, lower in “IRT” group than “NIRT” group (34.4 Gy vs. 44.7 Gy, respectively). Genito-urinary and gastro-intestinal toxicities were similar in the two groups; in particular G3-G4 diarrhoea occurred in 3/54 and 2/26 patients, respectively.
The incidence of G ≥ 3 diarrhoea and genito-urinary toxicity in the Mitomycin-C groups reported by the two more recent phase III trials of CRT for anal cancer was 9% and 2% in the ACT II18, 23% and 11% in the RTOG 98116, respectively. Both trials used conventional RT techniques. The use of IMRT seems to reduce the incidence of G ≥ 3 GI toxicity in a range from 019 to 11–15.1%20,21, with most studies reporting an incidence from 7 to 9%22,23, without impairing the efficacy compared with traditional RT techniques24. A comparable range of G ≥ 3 GI toxicity, from 5 to 10%, was reported with the use of VMAT25 and Tomotherapy26. IMRT, VMAT and Tomotherapy, seem to reduce also G ≥ 3 genito-urinary toxicity to 0–3%13,19,20,21,23,24,27. Similarly to the two recent phase III trial, all the above reported trials using IMRT, VMAT or Tomotherapy, treated the inguinal LNs, then it is impossible to ascertain whether the exclusion of inguinal nodal area may translate into a further reduction of gastro-intestinal and genito-urinary toxicity.
Conclusion
SLNB staging of inguinal LNs seems to be superior compared to the FDG-PET, it allows to better identify false positive and false negative FDG-PET patients. Combination of FDG-PET and SLNB could guide the therapeutic decision and advanced RT techniques should better avoid toxicity, especially if patients are treated on groin.
References
Mistrangelo, M. et al. Comparison of positron emission tomography scanning and sentinel node biopsy in the detection of inguinal node metastases in patients with anal cancer. Int. J. Radiat. Oncol. Biol. Phys. 77, 73–78. https://doi.org/10.1016/j.ijrobp.2009.04.020 (2010).
Wade, D. S., Herrera, L., Castillo, N. B. & Petrelli, N. J. Metastases to the lymph nodes in epidermoid carcinoma of the anal canal studied by a clearing technique. Surg. Gynecol. Obstet. 169, 238–242 (1989).
Gerard, J. P. et al. Management of inguinal lymph node metastases in patients with carcinoma of the anal canal: Experience in a series of 270 patients treated in Lyon and review of the literature. Cancer 92, 77–84 (2001).
Blinde, S. E. et al. Inguinal lymph node recurrence in the untreated groin of patients with anal carcinoma. Dis. Colon Rectum 57, 578–584. https://doi.org/10.1097/DCR.0000000000000050 (2014).
Ortholan, C. et al. Anal canal cancer: Management of inguinal nodes and benefit of prophylactic inguinal irradiation (CORS-03 Study). Int. J. Radiat. Oncol. Biol. Phys. 82, 1988–1995. https://doi.org/10.1016/j.ijrobp.2011.02.010 (2012).
Ajani, J. A. et al. Fluorouracil, mitomycin, and radiotherapy vs fluorouracil, cisplatin, and radiotherapy for carcinoma of the anal canal: A randomized controlled trial. JAMA 299, 1914–1921. https://doi.org/10.1001/jama.299.16.1914 (2008).
De Nardi, P. et al. Prognostic value of FDG-PET/CT and inguinal sentinel lymph node biopsy in patients with anal cancer. Colorectal Dis. https://doi.org/10.1111/codi.14691 (2019).
Sveistrup, J. et al. Positron emission tomography/computed tomography in the staging and treatment of anal cancer. Int. J. Radiat. Oncol. Biol. Phys. 83, 134–141. https://doi.org/10.1016/j.ijrobp.2011.06.1955 (2012).
Mistrangelo, M. et al. Role of positron emission tomography-computed tomography in the management of anal cancer. Int. J. Radiat. Oncol. Biol. Phys. 84, 66–72. https://doi.org/10.1016/j.ijrobp.2011.10.048 (2012).
Cotter, S. E. et al. FDG-PET/CT in the evaluation of anal carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 65, 720–725. https://doi.org/10.1016/j.ijrobp.2006.01.009 (2006).
Bannas, P. et al. Contrast-enhanced [(18)F]fluorodeoxyglucose-positron emission tomography/computed tomography for staging and radiotherapy planning in patients with anal cancer. Int. J. Radiat. Oncol. Biol. Phys. 81, 445–451. https://doi.org/10.1016/j.ijrobp.2010.05.050 (2011).
Mistrangelo, D. M. et al. Value of staging squamous cell carcinoma of the anal margin and canal using the sentinel lymph node procedure: An update of the series and a review of the literature. Br. J. Cancer 108, 527–532. https://doi.org/10.1038/bjc.2012.600 (2013).
Kachnic, L. A. et al. RTOG 0529: A phase 2 evaluation of dose-painted intensity modulated radiation therapy in combination with 5-fluorouracil and mitomycin-C for the reduction of acute morbidity in carcinoma of the anal canal. Int. J. Radiat. Oncol. Biol. Phys. 86, 27–33. https://doi.org/10.1016/j.ijrobp.2012.09.023 (2013).
De Nardi, P., Carvello, M. & Staudacher, C. New approach to anal cancer: Individualized therapy based on sentinel lymph node biopsy. World J. Gastroenterol. 18, 6349–6356. https://doi.org/10.3748/wjg.v18.i44.6349 (2012).
De Nardi, P., Carvello, M., Canevari, C., Passoni, P. & Staudacher, C. Sentinel node biopsy in squamous-cell carcinoma of the anal canal. Ann. Surg. Oncol. 18, 365–370. https://doi.org/10.1245/s10434-010-1275-x (2011).
Jones, M., Hruby, G., Solomon, M., Rutherford, N. & Martin, J. The role of FDG-PET in the initial staging and response assessment of anal cancer: A systematic review and meta-analysis. Ann. Surg. Oncol. 22, 3574–3581. https://doi.org/10.1245/s10434-015-4391-9 (2015).
Engledow, A. H. et al. The role of (1)(8)fluoro-deoxy glucose combined position emission and computed tomography in the clinical management of anal squamous cell carcinoma. Colorectal Dis. 13, 532–537. https://doi.org/10.1111/j.1463-1318.2010.02193.x (2011).
James, R. D. et al. Mitomycin or cisplatin chemoradiation with or without maintenance chemotherapy for treatment of squamous-cell carcinoma of the anus (ACT II): A randomised, phase 3, open-label, 2 × 2 factorial trial. Lancet Oncol. 14, 516–524. https://doi.org/10.1016/S1470-2045(13)70086-X (2013).
Janssen, S. et al. Clinical experience of SIB-IMRT in anal cancer and selective literature review. Radiat. Oncol. 9, 199. https://doi.org/10.1186/1748-717X-9-199 (2014).
Salama, J. K. et al. Concurrent chemotherapy and intensity-modulated radiation therapy for anal canal cancer patients: A multicenter experience. J. Clin. Oncol. 25, 4581–4586. https://doi.org/10.1200/JCO.2007.12.0170 (2007).
Call, J. A. et al. Intensity-modulated radiation therapy for anal cancer: Results from a multi-institutional retrospective cohort study. Am. J. Clin. Oncol. 39, 8–12. https://doi.org/10.1097/COC.0000000000000009 (2016).
Bazan, J. G. et al. Intensity-modulated radiation therapy versus conventional radiation therapy for squamous cell carcinoma of the anal canal. Cancer 117, 3342–3351. https://doi.org/10.1002/cncr.25901 (2011).
Han, K. et al. Prospective evaluation of acute toxicity and quality of life after IMRT and concurrent chemotherapy for anal canal and perianal cancer. Int. J. Radiat. Oncol. Biol. Phys. 90, 587–594. https://doi.org/10.1016/j.ijrobp.2014.06.061 (2014).
Dasgupta, T. et al. Intensity-modulated radiotherapy vs. conventional radiotherapy in the treatment of anal squamous cell carcinoma: A propensity score analysis. Radiother. Oncol. 107, 189–194. https://doi.org/10.1016/j.radonc.2013.03.012 (2013).
Franco, P. et al. Volumetric modulated arc therapy (VMAT) in the combined modality treatment of anal cancer patients. Br. J. Radiol. 89, 20150832. https://doi.org/10.1259/bjr.20150832 (2016).
Joseph, K. et al. Prospective phase II study of tomotherapy based chemoradiation treatment for locally advanced anal cancer. Radiother. Oncol. 117, 234–239. https://doi.org/10.1016/j.radonc.2015.08.008 (2015).
Pepek, J. M. et al. Intensity-modulated radiation therapy for anal malignancies: A preliminary toxicity and disease outcomes analysis. Int. J. Radiat. Oncol. Biol. Phys. 78, 1413–1419. https://doi.org/10.1016/j.ijrobp.2009.09.046 (2010).
Acknowledgements
AIRC, Associazione Italiana Ricerca su Cancro, is gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
N.S.: project development, design of the work, treatment planning, interpretation of data, manuscript writing and editing, final approval of the version to be published. P.P.: conception and design of the work, treatment planning, interpretation of data, manuscript writing and editing, final approval of the version to be published. E.I.: content planning, interpretation of data, manuscript writing and editing, final approval of the version to be published. G.M.C., C.F.: statistical analysis, interpretation of data, manuscript writing and editing, final approval of the version to be published. R.T., C.G., N.D.M.: data collection, treatment planning, manuscript editing, final approval of the version to be published. C.C., L.G.: imaging evaluation, final approval of the version to be published. M.R., V.B.: clinical evaluation, final approval of the version to be published. P.D.N., A.M.T.: surgical procedure, final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Slim, N., Passoni, P., Incerti, E. et al. Impact of sentinel lymph-node biopsy and FDG-PET in staging and radiation treatment of anal cancer patients. Sci Rep 10, 14613 (2020). https://doi.org/10.1038/s41598-020-71577-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71577-8
This article is cited by
-
[18F]-FDG PET in anal canal cancer: a systematic review and meta-analysis
European Journal of Nuclear Medicine and Molecular Imaging (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.