Abstract
Background and objectives
The Reporting and Data System (RADS) have been used in the attempts to standardize the results of oncological scans in different scenarios, such as lymph nodes, adding configuration criteria to size determination. We analyze the predictive value of preoperative Node-RADS determination at imaging for pelvic lymph node (PLN) involvement in cases of prostate cancer (PC) considered for radical prostatectomy (RP) with extended lymph node dissection (eLND) and we compare it with validate predictive nomograms (MSKCC, Briganti and Gandaglia).
Methods
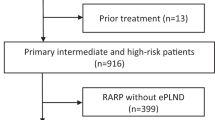
150 patients with a histological diagnosis of PC (high risk or intermediate with an estimated risk for pN+ higher than 5% using the Briganti or 7% using the Gandaglia nomogram) submitted for RP with an ePLND from 2018 and 2021 were retrospectively examined. Node-RADS determination was performed in all cases using the preoperative magnetic resonance (MR), performed by a radiologist blinded for pathologic results and compared with the MSKCC, Briganti 2012, Gandaglia 2017 and Gandaglia 2019 nomograms.
Results
PLN involvement at final pathology (pN+) was found in 36/150 (24.0%) of cases and the mean percentage of positive LNs in pN+ cases was 15.90 ± 13.40. The mean number of PLNs removed at RP was similar (p = 0.188) between pN0 (23.9 ± 8.0) and pN+ (25.3 ± 8.0) cases. Considering a Node RADS 4–5 positive and a Node RADS 1–2 negative, the PPV was 100% and the NPV was 79.6%. A Node RADS score 4–5 showed a lower sensitivity (0.167 versus 0.972, 1.000, 0.971, 0.960 respectively), a higher specificity (1.000 versus 0.079, 0.096, 0.138, 0.186 respectively) and a similar AUC (0.583 versus 0.591, 0.581, 0.574, 0.597 respectively) when compared to MSKCC, Briganti 2012, Gandaglia 2017 and Gandaglia 2019 nomograms.
Conclusions
Our evaluation suggests that Node RADS score, combining configuration criteria to size determination could improve specificity in terms of pathologic PLN prediction but a very low sensitivity has been also described.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Database including all data obtained for this analysis is available with the code: #9645 A at the following mail address for request: alessandro.sciarra@uniroma1.it.
References
Sciarra A, Voria G, Monti S, Mazzone L, Mariotti G, Pozza M, et al. Clinical understaging in patients with prostate adenocarcinoma submitted to radical prostatectomy: predictive value of serum chromogranin A. Prostate 2004;58:421–8.
Mottet N, van den Bergh RCN: Prostate Cancer: European Association of Urology (EAU) guidelines 2021. https://uroweb.org/guideline/prostate-cancer/
Briganti A, Larcher A, Abdollah F, Capitanio U, Gallina A, Suardi N, et al. Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol. 2012;61:480.
Gandaglia G, Fosati N, Zaffuto E, Bandini M, Dell’Oglio P, Bravi CA, et al. Development and internal validation of a novel model to identify the candidates for extended pelvic lymph node dissection in prostate cancer. Eur Urol. 2017;72:632.
Fossati N, Willemse PM, Van den Broeck T, van den Bergh RCN, Yuan CY, Briers E, et al. The benefits and harms of different extents of lymph node dissection during radical prostatectomy for prostate cancer: a systematic review. Eur Urol. 2017;72:84.
Lestingi JFP, Guglielmetti GB, Trinh QD, Coelho RF, Pontes J Jr, Bastos DA, et al. Extended versus limited pelvic lymph node dissection during radical prostatectomy for intermediate- and high-risk prostate cancer: early oncological outcomes from a randomized phase 3 trial. Eur Urol. 2021;79:595–604.
Gandaglia G, Ploussard G, Valerio M, Mattei A, Fiori C, Fossati N, et al. A novel nomogram to identify candidates for extended pelvic lymph node dissection among patients with clinically localized prostate cancer diagnosed with magnetic resonance imaging-targeted and systematic biopsies. Eur Urol. 2019;75:506.
Milonas D, Venclovas Z, Muilwijk T, Jievaltas M, Joniau S. External validation of MSKCC nomogram and prediction of optimal candidate for lymph node dissection in clinically localized prostate cancer: Cetral Eur. J Urol. 2020;73:25.
Brown G, Richards CJ, Bourne MW. Morphologic predictors of lymph node status in reactal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology. 2003;227:371–377.
Curtin HD, Ishwaran H, Mancuso AA, Dalley RW, Caudry DJ, McNeil BJ. Comparison of CT and MR imaging in staging of neck metastases. Radiology. 1998;207:123–130.
D’Orsi CJ, Kopans DB. Mammography interpretation: the BI-RADS method. Am Fam Phys. 1997;55:1548–1552.
Elsholtz FHJ, Asbach P, Haas M, Becker M, Beets-tan RGH, Thoeny HC, et al. Introducing the node reporting and Data System 1.0 (Node RADS): a concept for standardized assessment of lymph nodes in cancer. Eur Radio. 2021;31:6116–6124.
Venclovas Z, Muilwijk T, Matjosaitis A, Jievaltas M, Joniau S, Milonas D. Head-to-head comparison of two nomograms predicting probability of lymph node invasion in prostate cancer and the therapeutic impact of higher nomogram threshold. J Clin Med. 2021;10-1:11.
Gandaglia G, Martini A, Ploussard G, Fossati N, Stabile A, De, et al. External validation of th 2019 Briganti nomogram for the identification of prostate cancer patients who should be considered for an extended pelvic lymph node dissection. Eur Urol. 2020;78:138–142.
Fossati N, Willemse PP, Van den Broeck T, van den Bergh RCN, Yuan CY, Mottet N, et al. The benefit and harms of different extents of lymph node dissection during radical prostatectomy for prostate cancer: a systematic review. Eur Urol. 2017;72:84–109.
Thoeny H, Barbieri S, Froehlich J, Tukhey B, Choyke P. Functional and targeted lymph node imaging in prostate cancer. Radiology. 2017;285:728–742.
Meijer D, van Leeuwen PJ, Roberts MJ, Siriwardana AR, Morton A, Yaxley JW, et al. External validation and addition of prostate specific membrane antigen positron emission tomography to the most frequently used nomograms for the prediction of pelvic lymph node metastases: an international multicenter study. Eur Urol. 2021;80:234–242.
Washington SL 3rd, Cowan JE, Herlemann A, Zuniga KB, Masic S, Nguyen HG, et al. Influence of pelvic lymph node dissection and node-positive diseaseon biochemical recurrence, secondary treatment, and survival after radicalprostatectomy in men with prostate cancer. Prostate 2021;81:102–108.
Touijer KA, Sjoberg DD, Benfante N, Laudone VP, Ehdaie B, Eastham JA, et al. Limited versus Extended Pelvic Lymph Node Dissection for Prostate Cancer: A Randomized Clinical Trial. Eur Urol Oncol. 2021;4:532–539.
Sciarra A, Panebianco V, Salciccia S, Cattarino S, Lisi D, Gentilucci A, et al. Modern role of magnetic resonance and spectroscopy in the imaging of prostate cancer. Urol Oncol. 2011;29:12–20.
Bass EJ, Pantovic A, Connor M, Gabe R, Padhani AR, Rockall A, et al. A systematic review and meta-analysis of the diagnostic accuracy of biparametric prostate MRI for prostate cancer in men at risk. Prostate Cancer Prostatic Dis. 2021;24:596–611.
Hovels A, Heesakkers R, Adang E, Jager G, Trum S. The diagnostic accuracy of CT and MRI in the staging of pelvic lymph nodes in patients with prostate cancer: a meta-analysis. Clin Radio. 2008;63:387–95.
Author information
Authors and Affiliations
Contributions
SL: radiologic evaluation of data. MLP: radiologic evaluation of data. MF: data acquisition and data analysis. FM: pathological analysis. AG: data acquisition. FDG: data analysis and statistical analysis. VC: data acquisition and statistical analysis. ES: data acquisition. GMB: data acquisition. GC: data analysis. LC: data acquisition. AC: data acquisition. AP: data acquisition CDN: data acquisition and data analysis. AT: data acquisition. CL: data acquisition. GF: data acquisition. GDP: data acquisition. SS: study design and concept; drafting of the manuscript. AS: study design and concept; drafting of the manuscript. VP: study design and concept.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lucciola, S., Pisciotti, M.L., Frisenda, M. et al. Predictive role of node-rads score in patients with prostate cancer candidates for radical prostatectomy with extended lymph node dissection: comparative analysis with validated nomograms. Prostate Cancer Prostatic Dis 26, 379–387 (2023). https://doi.org/10.1038/s41391-022-00564-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00564-z
This article is cited by
-
Performance of node reporting and data system (node-RADS): a preliminary study in cervical cancer
BMC Medical Imaging (2024)
-
Benefit and harm of lymphadenectomy in intermediate risk prostate cancer: comparison of five nomograms
BMC Urology (2023)
-
The predictive value of machine learning and nomograms for lymph node metastasis of prostate cancer: a systematic review and meta-analysis
Prostate Cancer and Prostatic Diseases (2023)
-
Nomograms in PCa: where do we stand
Prostate Cancer and Prostatic Diseases (2023)
-
Relative impact of lymph-node metastasis and seminal vesical invasion on oncologic outcomes following radical prostatectomy
Prostate Cancer and Prostatic Diseases (2023)