Abstract
To investigate the changes and clinical significance of brain structural abnormalities in patients with Meige syndrome and related depressive symptoms. We retrospectively analysed clinical data, imaging examinations, and Hamilton Depression Rating scale scores in 46 patients with Meige syndrome from January 2017 to January 2019. We compared the Meige syndrome group with the healthy control group, and the definite depression group with the non-definite depression group. Voxel-based morphometry (VBM) was used to compare grey matter (GM) volumes. We conducted two-sample t-tests corrected for subject age and gender. We tested at a level of significance of p < 0.001 with a false discovery rate (FDR) correction. VBM demonstrated decreased GM volume (p < 0.001 and cluster size > 50 voxels) in the left hemisphere in the middle frontal orbital gyrus, temporal pole (superior temporal gyrus) and insula and in the right hemisphere in the temporal pole (middle temporal gyrus), precuneus, inferior parietal, inferior temporal and olfactory cortices in the Meige syndrome group. Comparing VBM-MRI measures in Meige syndrome patients with and without depression, decreased GM volume was found in the left hemisphere in the cuneus and hippocampus and in the right hemisphere in the angular gyrus, middle frontal gyrus and middle occipital gyrus in the definite depression group. Unlike other dystonia studies that have suggested an involvement of the basal ganglia and motor cortex in the pathophysiology of the disorder , we believe that the precuneus is involved in the development of Meige syndrome. Additionally, our findings suggest that the hippocampus plays a role in the pathogenesis of depression in patients with Meige syndrome.
Similar content being viewed by others
Introduction
Meige syndrome, also known as idiopathic blepharospasm-oromandibular dystonia syndrome, is a rare type of segmental dystonia disorder with features of adult hyperactivity disorder and characterized by blepharospasm and oromandibular dystonia disorder1,2,3. Meige syndrome usually occurs between 30 and 60 years of age, with rare cases appearing in teenage years4. This disease is more common in females, and the ratio of males to females is approximately 1:3. Meige syndrome can be divided into three types according to clinical manifestations: blepharospasm, blepharospasm-oromandibular dystonia, and oromandibular dystonia, among which blepharospasm with oromandibular dystonia is regarded as the complete type of Meige syndrome3. Meige syndrome is classified into primary and secondary Meige syndromes. Although plastic changes and reduced cortical inhibition have been documented by neurophysiological and neuroimaging techniques5, the aetiology of primary Meige syndrome is still unknown.
In recent years, the application of the voxel-based morphometry method of magnetic resonance imaging (VBM-MRI) for structural imaging research has provided a new and important method for structural research of neurologic movement disorders6. Some VBM-MRI studies have shown significant reductions in grey matter (GM) volume mainly in the cerebellar vermis and bilateral superior frontal gyri7,8. However, they did not study Meige patients, and the number of included patients was small. Therefore, a VBM study on Meige syndrome is necessary to clarify the pathogenesis of this disease. In addition to blepharospasm and oromandibular dystonia, Meige syndrome is more commonly associated with mood disorders, with a higher incidence of depression3. In this study, VBM analysis was used to investigate the changes and clinical significance of brain structural abnormalities in patients with Meige syndrome and related depressive symptoms.
Results
Baseline characteristics
A total of 46 cases (11 males; 35 females) were included, and the age of the participants ranged from 37 to 73 years (57.00 ± 8.86). The duration of Meige syndrome ranged from 3 to 8 years (4.57 ± 2.23). Blepharospasm was present in 18 patients, and 5 had oromandibular dystonia; 23 patients had both blepharospasm and oromandibular dystonia. The BFMDRS movement scores of participants ranged from 3.25 to 13.5 (7.87 ± 2.45). The HAMD scores of the participants ranged from 9 to 29 (16.96 ± 4.84). In the control group, a total of 64 individuals (25 males; 39 females) were included, and the average age was 52.71 ± 6.26. The BFMDRS and HAMD scores were significantly higher in the Meige syndrome group than in the healthy control group (P < 0.05) (Table 1).
We divided the patients into a definite depression group (< 18) and a non-definitive depression group (> 18) according to HAMD scores. Finally, there were 25 patients in the definitive depression group and 21 in the non-definitive depression group. There were no significant differences between the two groups in terms of age, gender or BFMDRS movement scores (P > 0.05) (Table 2).
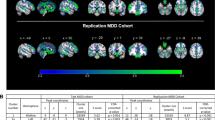
Comparison of VBM-MRI in patients with Meige syndrome and controls
Conventional MRI showed normal results in all patients with Meige syndrome and controls. The VBM analysis in the current study revealed multiple significant differences between the patients with Meige syndrome and controls. We found decreased GM volume (p < 0.001 and cluster size > 50 voxels) in the left hemisphere in the middle frontal orbital gyrus, temporal pole (superior temporal gyrus) and insula and in the right hemisphere in the temporal pole (middle temporal gyrus), precuneus, inferior parietal, inferior temporal and olfactory cortices (Table 3; Fig. 1).
Areas showing decreased GM volume in axial slices (p < 0.001) in Meige syndrome patients and control subjects. In the left hemisphere in the middle frontal orbital gyrus (t = − 8.83, p < 0.001), temporal pole superior temporal gyrus (t = − 8.20, p < 0.001) and insula (t = − 7.98, p < 0.001); in the right hemisphere in the temporal pole middle temporal gyrus (t = − 7.32, p < 0.001), precuneus (t = − 5.99, p < 0.001), inferior parietal (t = − 5.84, p < 0.001), inferior temporal (t = − 5.03, p < 0.001)and olfactory cortices (t = − 4.95, p < 0.001).
Comparison of VBM-MRI in patients with Meige syndrome with and without depression
We found decreased GM volume (p < 0.001 and cluster size > 50 voxels) in the left hemisphere in the cuneus and hippocampus and in the right hemisphere in the angular gyrus, middle frontal gyrus and middle occipital gyrus (Table 4; Fig. 2).
Areas showing decreased GM volume in axial slices in Meige syndrome patients with and without depression. In the left hemisphere in the cuneus (t = − 4.82, p < 0.001) and hippocampus (t = − 4.23, p < 0.001); in the right hemisphere in the angular gyrus(t = − 4.84, p < 0.001), middle frontal gyrus(t = − 6.29, p < 0.001) and middle occipital gyrus(t = − 5.80, p < 0.001).
Discussion
Meige syndrome was named after French neurologist Henry Meige. In 1910, Henry Meige described approximately 10 patients with blepharospasm, one of whom also had mandibular dystonia9. Currently, most researchers and clinicians prefer the term “Meige syndrome” to describe blepharospasm-oromandibular dystonia syndrome10. Meige syndrome usually occurs between 30 and 60 years of age, with rare cases presenting during teenage years4. This disease is more common in females, and the ratio of males to females is approximately 1:311. In our study, a total of 46 patients (11 males; 35 females) were included, and the age of the participants ranged from 37 to 73 years (57.00 ± 8.86), which was consistent with previous studies. Meige syndrome can be divided into three types according to clinical manifestations: blepharospasm, blepharospasm-oromandibular dystonia, and oromandibular dystonia, among which blepharospasm with oromandibular dystonia is regarded as the complete type of Meige syndrome10. In our study, blepharospasm was present in 18 patients, and 5 had oromandibular dystonia; 23 patients had both blepharospasm and oromandibular dystonia. The BFMDRS movement scores of participants ranged from 3.25 to 13.5 (7.87 ± 2.45).
Discussion
The aetiology of primary Meige syndrome is still unknown, but changes in plasticity and reduced cortical inhibition due to environmental triggers and genetic susceptibility may be associated with the onset of Meige syndrome5. Many movement disorders are not limited to a particular region but involve multiple brain regions12. Therefore, morphological studies of the whole brain are helpful to understand the pathogenesis of Meige syndrome. VBM techniques quantitatively analyses the GM and WM volumes in each voxel in MRI images, thereby allowing an evaluation of the anatomical structural differences across the whole brain13. Recently, researchers using VBM observed conflicting results of increased, decreased, or no change in GM volume in patients with primary blepharospasm and cervical dystonia8. A VBM study by Piccinin7 showed that patients with craniocervical dystonia had reduced GM volume in the cerebellar vermis, bilateral superior frontal gyri, precuneus, cingulate, insular cortex, and corpus callosum fissure. However, all of these studies examined patients with craniocervical dystonia, and to the best of our knowledge, there is no research on Meige syndrome.
In this study, VBM analysis was used to investigate the changes and clinical significance of brain structural abnormalities in patients with Meige syndrome. We found decreased GM volume (p < 0.001 and cluster size > 50 voxels) in the left hemisphere in the middle frontal orbital gyrus, temporal pole (superior temporal gyrus) and insula and in the right hemisphere in the temporal pole (middle temporal gyrus), precuneus, inferior parietal, inferior temporal and olfactory cortices. We failed to detect any abnormalities in the basal ganglia and motor cortex. The results from previous VBM-MRI-related studies in those with dystonia have shown varying increases and decreases in GM volume in the basal ganglia14,15, and no abnormalities have been found in the basal ganglia in recent years16, which is consistent with the results of this study. However, a recent study showed that the precentral gyrus, which plays an important role in motor planning and learning, is involved in the onset of craniocervical dystonia7. One of the reasons why our results differ from the above results is that the patients they selected were not typical Meige syndrome patients7,14,16. The present study is the first VBM-MRI study in patients with Meige syndrome, and the sample size of this study was larger than previous studies. Therefore, although functional changes in brain regions such as the basal ganglia are necessary for the development and maintenance of dystonia, they do not necessarily result in anatomical changes7.
In this study, we found a reduction in GM volume in the precuneus and inferior parietal cortex in patients with Meige syndrome. The precuneus lies deep in the parietal lobe and interacts with the adjacent posterior medial cortex (posterior cingulate and posterior compressed cortex). This internal connection is bilateral, providing communication between corresponding components in the two hemispheres and to some extent providing the anatomical basis for bilateral functional coordination17. The precuneus is also selectively associated with other parietal regions, such as the supraparietal lobule, and is involved in visual spatial information processing. Recent studies have found that the precuneus is associated with many higher cognitive functions, such as episodic memory, self-related information processing, and consciousness, and is no longer considered a simple extension of the lateral parietal cortex18. Therefore, abnormal findings in the precuneus also indicated that patients with Meige syndrome may have abnormal integration at the cortical level. The precuneus has been shown to have extensive connections with the auxiliary motor areas. At the subcortical level, the modular prefrontal lobe is primarily associated with the nuclei of the basal ganglia and projects fibres into the brainstem19. Therefore, we hypothesized that the precuneus plays an important role in the pathogenesis of Meige syndrome, which partly explains the lack of GM volume reductions in the basal ganglia and motor cortex.
In the frontal lobe, we found a reduction in GM volume in the left middle frontal orbital gyrus in the patients with Meige syndrome. The frontal lobe plays a key role in many of the brain’s higher functions, including attention regulation, learning and memory, behaviour planning, behavioural inhibition, thinking and reasoning20. At the same time, the frontal lobe is also an important part of “emotional centre” or “emotion-related pathways”21. The orbitofrontal cortex is involved in the encoding of external and internal information, reward-related behaviour, impulse control, and emotional regulation22. The prefrontal cortex is also extensively connected to the superior temporal gyrus and olfactory cortex22. In the temporal lobe, we also found that the patients with Meige syndrome had decreased GM volume in the superior temporal pole, middle temporal pole and inferior temporal regions. At present, it is believed that the temporal lobe plays an important role in visual and auditory integration and regulation23 and is closely related to face recognition, distance judgement and text comprehension in reading. Many Meige syndrome patients have varying degrees of depression and other emotional disorders. Therefore, we believe that the decrease in GM volume in the frontal lobe and temporal lobe in this study was mainly related to the non-motor symptoms of this disease. Finally, we found that the patients with Meige syndrome had decreased GM volume in the insula. The posterior insular cortex is mainly responsible for the integration of sensorimotor functions in the brain together with the primary motor cortex, sensorimotor cortex, auxiliary motor area and middle cingulate gyrus, while the anterior insular cortex is mainly responsible for emotional regulation together with the anterior cingulate gyrus, middle temporal gyrus and inferior temporal gyrus24,25. Therefore, we believe that the insula may be involved in the development of motor and non-motor symptoms of Meige syndrome.
Meige syndrome with mood disorders is also common, with a higher incidence of depression than in the general population3. In our study, the severity of depression was determined by the psychological 21-item Hamilton Depression Rating scale (HAMD)26. There were 25 patients in the definite depression group. When we compared VBM-MRI measures in Meige syndrome patients with and without depression, we found decreased GM volume (p < 0.001 and cluster size > 50 voxels) in the left hemisphere in the cuneus and hippocampus and in the right hemisphere in the angular gyrus, middle frontal gyrus and middle occipital gyrus (Table 4; Fig. 2). The results of this study suggest that, in addition to the frontal lobes mentioned above, the hippocampus plays an important role in the pathogenesis of depression in patients with Meige syndrome. A previous study has shown not only that depression is manifested by bilateral hippocampal volume reduction but also that the degree of reduction is related to the severity of symptoms, the course of disease and the number of recurrences27. The patients in that study had a long duration of illness (4.57 ± 2.23 years), and the hippocampal changes accompanying depression also showed a process of gradual accumulation, which finally manifested as volume reduction, which was consistent with the results of the present study. The occipital lobe is involved in attention, visual memory, visual movement, language movement and other neuropsychological activities28. In the process of visual information processing of external positive stimuli in the basic state of chronic or recurrent depression, the function of the relevant cortex was weaker than that in healthy controls. The cuneus is also part of the occipital lobe, and we believe that it is involved in the development of depression in patients with Meige syndrome.
Conclusion
At present, there are few imaging studies on the pathogenesis of Meige syndrome, and most of them include a heterogeneous collection of patients with dystonias. In this present study, VBM analysis was used to investigate the changes and clinical significance of brain structural abnormalities in patients with Meige syndrome and related depressive symptoms. First, unlike previous imaging studies with patients with dystonia, we found no abnormalities in the basal ganglia and motor cortex. However, the important role of the precuneus in the pathogenesis of Meige syndrome may have been revealed in our study. Second, the decrease in GM volume in the frontal lobe and temporal lobe in this study was mainly related to the non-motor symptoms of this disease. Finally, we compared VBM-MRI in Meige syndrome patients with and without depression and found that the hippocampus plays an important role in the pathogenesis of depression in patients with Meige syndrome.
The limitation of this study is that it is only a cross-sectional study with a relatively small sample size. The sample size can be further expanded in the future. In addition, positron emission tomography (PET) is an in vivo method that reflects the level of brain metabolism. Combined with VBM-MRI, a better understanding of the changes in brain function and morphology in Meige syndrome can be obtained. Another limitation of our study is that the cohort is composed of a mix of significantly different phenotypes of Meige syndrome (oromandibular, blepharospasm and combined oromandibular and blepharospasm). In the future, our team plans to investigate into the similarities and differences in gray matter volume across these disorders.
Methods
Patients
Clinical data of 46 right-handed patients with primary Meige syndrome were collected between January 2017 and January 2019 at the Department of Neurosurgery, Peking University People’s Hospital. Primary Meige syndrome diagnosed by an experienced neurologist, Ruen Liu. The diagnostic criteria are mainly based on blepharospasm, oral and mandibular dystonia, increased blink rates and other symptoms. Laboratory and imaging examinations showed no abnormalities. Patients with histories of drug or alcohol use disorders, psychiatric disorders and other secondary factors were excluded. Based on the clinical manifestations, the patients were divided into three types: (1) blepharospasm; (2) blepharospasm with oromandibular dystonia; and (3) oromandibular dystonia. In this study, 64 right-handed healthy people with age and education levels matching the Meige syndrome group were included as the healthy control group.
Written informed consent was obtained from each participant, and the study was approved by the institutional review board of Peking University People’s Hospital. All methods were carried out in accordance with relevant guidelines and regulations.
Magnetic resonance imaging
Imaging was conducted on a Discovery 750 3.0 T (GE Healthcare, Waukesha, WI) MRI scanner. T1-weighted anatomical images in the sagittal plane were collected with a 3D fast spoiled gradient echo sequence: repetition time (TR) = 4.9 ms, echo time (TE) = 2 ms, flip angle = 15°, field of view (FOV) = 240 mm, in-plane resolution = 1 × 1 mm2, slice thickness = 1 mm, and 170 slices. All scans were performed by the same imaging physician.
Image data analysis
Structural images were processed with SPM8 (https://www.fil.ion.ucl.ac.uk/spm) and VBM8 toolbox (https://dbm.neuro.unijena.de/vbm) within the MATLAB R2016a programming environment (The MathWorks, Natick, MA).
Preprocessing of the data involved spatial normalization, GM segmentation and spatial smoothing with a Gaussian kernel. Image preprocessing mainly included the following steps: (1) with the aid of the MATLAB platform, SPM8 converted the collected images to a format that can be recognized and uses MRIcro software (https://www.mccauslandcenter.sc.edu/mricro/mricro/mricro.html) to adjust the spatial coordinates of each image such that the data from all subjects had the spatial coordinates of the image adjusted and all participants' images were located in a closed spatial coordinate system. Since the brain structure of each subject greatly varied, we needed to conduct spatial standardization on all the images from the subjects and convert them into standardized images with the same size and direction; (2) according to the distribution template of GM, white matter (WM) and cerebrospinal fluid (CSF) in the brain, each element in the image was judged to be GM, WM or CSF to segment the GM, WM or CSF and generate different brain tissue images29; (3) the last step is Gaussian smoothing of the standardized image. The image obtained in the previous step was smoothed by a Gaussian kernel of 8 mm × 8 mm × 8 mm at half height and width. This step can eliminate high-frequency noise and improve the signal-to-noise ratio of the image. In addition, the image can be made to have the characteristics of a random Gaussian field and meet the requirements of the statistical analyses of SPM.
Data collection
Baseline data and medical histories were obtained from patient medical records. Baseline data included age, sex, and dystonia and depressive status. Dystonia was evaluated using the Burke–Fahn–Marsden Dystonia Rating Scale (BFMDRS)30. The severity of depression was determined by the psychological 21-item Hamilton Depression Rating scale (HAMD)26. A score of less than 7 was considered normal; 7–17 indicated possible depression; 18 to 24 indicated definite depression; and greater than 24 was considered severe depression. Finally, we divided the patients into a definite depression group (< 18) and a non-definite depression group (> 18).
Statistical analysis
SPSS 19.0 statistical software (IBM Corp., Armonk, NY, USA) was used for data analysis31. Numerical variables are expressed as the mean ± standard deviation. Qualitative variables are described by absolute values of cases in different groups. Statistical significance between the quantitative variables was assessed by X2 tests, corrected by Yates or Fisher if necessary. Student’s t-tests were performed to evaluate data that followed a normal distribution. P < 0.05 was considered statistically significant differences.
Two-sample t-tests corrected for subject age, gender and total intracranial volume were used for VBM-MRI comparisons between groups7. Significant differences between groups were indicated when P < 0.001 (false discovery rate corrected). Only sets with more than 50 voxels were considered statistically significant brain regions. The t-test results are superimposed on the template of the T1 structural image, and the results are presented by the xjView software (version 9.6, https://www.alivelearn.net/xjView).
Ethics approval
The present study was approved by the Medical Ethics Committee of Peking University People’s Hospital. All methods were carried out in accordance with relevant guidelines and regulations.
Consent to participate
All patients provided written informed consent to participate.
Consent for publication
The study participants provided their consent for the publication of any data/associated images.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Tolosa, E. S. Clinical features of Meige’s disease (idiopathic orofacial dystonia): a report of 17 cases. Arch. Neurol. 38, 147–151. https://doi.org/10.1001/archneur.1981.00510030041005 (1981).
Miao, J. et al. Meige’s syndrome and hemichorea associated with hyperthyroidism. J. Neurol. Sci. 288, 175–177. https://doi.org/10.1016/j.jns.2009.10.018 (2010).
Jahngir, M. U. & Patel, B. C. StatPearls (Springer, New York, 2020).
Sabesan, T. Meige syndrome: a rare form of cranial dystonia that was treated successfully with botulinum toxin. Br. J. Oral. Maxillofac. Surg. 46, 588–590. https://doi.org/10.1016/j.bjoms.2008.02.002 (2008).
Hallett, M. Blepharospasm: recent advances. Neurology 59, 1306–1312. https://doi.org/10.1212/01.wnl.0000027361.73814.0e (2002).
Barrett, M. J. et al. Lower volume, more impairment: reduced cholinergic basal forebrain grey matter density is associated with impaired cognition in Parkinson disease. J. Neurol. Neurosurg. Psychiatry 90, 1251–1256. https://doi.org/10.1136/jnnp-2019-320450 (2019).
Piccinin, C. C. et al. Diffuse decreased gray matter in patients with idiopathic craniocervical dystonia: a voxel-based morphometry study. Front. Neurol. 5, 283. https://doi.org/10.3389/fneur.2014.00283 (2014).
Valls-Sole, J. & Defazio, G. Blepharospasm: update on epidemiology, clinical aspects, and pathophysiology. Front. Neurol. 7, 45. https://doi.org/10.3389/fneur.2016.00045 (2016).
Pandey, S. & Sharma, S. Meige’s syndrome: history, epidemiology, clinical features, pathogenesis and treatment. J. Neurol. Sci. 372, 162–170. https://doi.org/10.1016/j.jns.2016.11.053 (2017).
LeDoux, M. S. Meige syndrome: what’s in a name?. Parkinsonism Relat. Disord. 15, 483–489. https://doi.org/10.1016/j.parkreldis.2009.04.006 (2009).
Soland, V. L., Bhatia, K. P. & Marsden, C. D. Sex prevalence of focal dystonias. J. Neurol. Neurosurg. Psychiatry 60, 204–205. https://doi.org/10.1136/jnnp.60.2.204 (1996).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 24, 197–211. https://doi.org/10.1016/s0197-4580(02)00065-9 (2003).
Good, C. D. et al. A voxel-based morphometric study of ageing in 465 normal adult human brains. Neuroimage 14, 21–36. https://doi.org/10.1006/nimg.2001.0786 (2001).
Pantano, P. et al. A transverse and longitudinal MR imaging voxel-based morphometry study in patients with primary cervical dystonia. AJNR Am. J. Neuroradiol. 32, 81–84. https://doi.org/10.3174/ajnr.A2242 (2011).
Draganski, B., Thun-Hohenstein, C., Bogdahn, U., Winkler, J. & May, A. “Motor circuit” gray matter changes in idiopathic cervical dystonia. Neurology 61, 1228–1231. https://doi.org/10.1212/01.wnl.0000094240.93745.83 (2003).
Martino, D. et al. Cortical gray matter changes in primary blepharospasm: a voxel-based morphometry study. Mov. Disord. 26, 1907–1912. https://doi.org/10.1002/mds.23724 (2011).
Seitz, R. J. & Binkofski, F. Modular organization of parietal lobe functions as revealed by functional activation studies. Adv. Neurol. 93, 281–292 (2003).
Vogeley, K. et al. Neural correlates of first-person perspective as one constituent of human self-consciousness. J. Cogn. Neurosci. 16, 817–827. https://doi.org/10.1162/089892904970799 (2004).
Leichnetz, G. R. Connections of the medial posterior parietal cortex (area 7m) in the monkey. Anat. Rec. 263, 215–236. https://doi.org/10.1002/ar.1082 (2001).
Miller, E. K. & Cohen, J. D. An integrative theory of prefrontal cortex function. Annu. Rev. Neurosci. 24, 167–202. https://doi.org/10.1146/annurev.neuro.24.1.167 (2001).
Cacioppo, J. T. & Gardner, W. L. Emotion. Annu. Rev. Psychol. 50, 191–214. https://doi.org/10.1146/annurev.psych.50.1.191 (1999).
Price, J. L. & Drevets, W. C. Neural circuits underlying the pathophysiology of mood disorders. Trends Cogn. Sci. 16, 61–71. https://doi.org/10.1016/j.tics.2011.12.011 (2012).
Ono, Y. et al. Frontotemporal oxyhemoglobin dynamics predict performance accuracy of dance simulation gameplay: temporal characteristics of top-down and bottom-up cortical activities. Neuroimage 85(Pt 1), 461–470. https://doi.org/10.1016/j.neuroimage.2013.05.071 (2014).
Le Berre, A. P. et al. Deviant functional activation and connectivity of the right insula are associated with lack of awareness of episodic memory impairment in nonamnesic alcoholism. Cortex 95, 15–28. https://doi.org/10.1016/j.cortex.2017.07.016 (2017).
Zhang, Y. et al. Abnormal functional connectivity of ventral anterior insula in asthmatic patients with depression. Neural Plast 2017, 7838035. https://doi.org/10.1155/2017/7838035 (2017).
Williams, J. B. A structured interview guide for the Hamilton depression rating scale. Arch. Gen. Psychiatry 45, 742–747. https://doi.org/10.1001/archpsyc.1988.01800320058007 (1988).
Cole, J., Costafreda, S. G., McGuffin, P. & Fu, C. H. Hippocampal atrophy in first episode depression: a meta-analysis of magnetic resonance imaging studies. J. Affect Disord. 134, 483–487. https://doi.org/10.1016/j.jad.2011.05.057 (2011).
Jiang, T., He, Y., Zang, Y. & Weng, X. Modulation of functional connectivity during the resting state and the motor task. Hum. Brain Mapp. 22, 63–71. https://doi.org/10.1002/hbm.20012 (2004).
Ashburner, J. & Friston, K. Multimodal image coregistration and partitioning: a unified framework. Neuroimage 6, 209–217. https://doi.org/10.1006/nimg.1997.0290 (1997).
Burke, R. E. et al. Validity and reliability of a rating scale for the primary torsion dystonias. Neurology 35, 73–77. https://doi.org/10.1212/wnl.35.1.73 (1985).
Liu, J. et al. Clinical analysis of patients with ipsilateral coexistence of hemifacial spasm and trigeminal neuralgia. World Neurosurg. https://doi.org/10.1016/j.wneu.2020.03.040 (2020).
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
J.L.: conceptualization, data curation, methodology, investigation, formal analysis, software, writing—original draft, reviewing and editing; L.L.: formal analysis, writing—reviewing and editing, Supervision; R.L.: conceptualization, methodology, supervision, writing—reviewing and editing, resources. L.C., Y.J., J.F., D.W., Z.L., J.O.: writing—reviewing and editing, validation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, J., Li, L., Chen, L. et al. Grey matter changes in Meige syndrome: a voxel-based morphology analysis. Sci Rep 10, 14533 (2020). https://doi.org/10.1038/s41598-020-71479-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71479-9
This article is cited by
-
Micro lesion effect of pallidal deep‑brain stimulation for meige syndrome
Scientific Reports (2022)
-
Voxel-based meta-analysis of gray matter abnormalities in idiopathic dystonia
Journal of Neurology (2022)
-
Cognitive and Neuropsychiatric Impairment in Dystonia
Current Neurology and Neuroscience Reports (2022)
-
Regional metabolic and network changes in Meige syndrome
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.