Abstract
Background The clinical features and therapeutic strategies for gastric cancer with positive peritoneal washing cytology but without visible gross peritoneal metastasis have not been defined. The aim of this study was to evaluate the effect and clinical prognostic value of postoperative chemotherapy in gastric cancer patients with positive peritoneal washing cytology without gross peritoneal metastasis who underwent radical D2 gastrectomy in terms of disease-free survival (DFS) and overall survival (OS). Materials and Methods Intraoperative peritoneal washing cytology was performed in 285 patients who underwent radical D2 gastrectomy between April 2004 and May 2016. Of them, 88 patients with positive cytology but without gross peritoneal metastasis were included in the study. In total, 64 patients received postoperative chemotherapy, whereas 24 patients underwent surgery only. Results Most gastric cancer patients with positive cytology without gross peritoneal metastasis demonstrated pT4 and/or pN3 disease. Postoperative chemotherapy improved DFS and OS compared to surgery only in gastric cancer patients with positive cytology without gross peritoneal metastasis (median DFS 11.63 vs. 6.98 months, p < 0.001; median OS 25.50 vs. 12.11 months, p < 0.001). In multivariate analyses of gastric cancer patients with positive cytology without gross peritoneal metastasis, no chemotherapy was the strongest clinical factor for poorer DFS (hazard ratio [HR] 3.76, p < 0.001) or OS (HR 4.37, p < 0.001). Conclusion Postoperative chemotherapy improves the survival outcome compared to surgery alone in gastric cancer patients with positive peritoneal washing cytology but without visible gross peritoneal metastasis who underwent radical D2 gastrectomy.
Similar content being viewed by others
Introduction
Although the incidence of gastric cancer has been decreasing in developed countries, it remains the fifth most common cancer and the third leading cause of cancer mortality worldwide1. In Korea, gastric cancer ranks second in cancer incidence and third in cancer mortality2. The treatment of choice for locally advanced gastric cancer in Asian countries, including Korea and Japan, is radical surgery followed by adjuvant chemotherapy3,4,5,6.
Peritoneal metastasis is the most frequent site of gastric cancer recurrence or metastasis and is associated with a very dismal prognosis7,8. The treatment options for advanced gastric cancer with overt gross peritoneal metastasis are only palliative systemic chemotherapy with or without surgical resection and/or intraperitoneal chemotherapy9.
Staging laparoscopy and peritoneal washing cytology have been evaluated for patients with gastric cancer to identify occult metastatic disease that is not detected by preoperative cross-sectional imaging, and positive peritoneal washing cytology in the absence of visible gross peritoneal implants is considered to be a poor prognostic factor for advanced disease and early recurrence and is defined as pM1 disease10,11.
The clinical features and therapeutic strategies for gastric cancer with positive cytology but without visible gross peritoneal metastasis have not been fully defined. The present study evaluated the effect and prognostic value of postoperative chemotherapy in patients with positive cytology but without gross peritoneal metastasis who underwent radical D2 gastrectomy in terms of disease-free survival (DFS) and overall survival (OS).
Methods
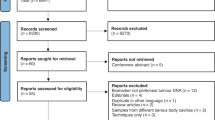
Patients
Intraoperative peritoneal washing cytology was performed in 285 patients who underwent radical D2 gastrectomy between April 2004 and May 2016. Of them, 88 patients with positive cytology but without gross peritoneal metastasis were included in the study. In total, 64 patients received postoperative chemotherapy and 24 patients underwent surgery only. Data from these patients were collected from our institutional database, and the survival data were updated at the time of analysis. The inclusion criteria were: patients with gastric adenocarcinoma who underwent radical gastrectomy and D2 lymph dissection with positive peritoneal washing cytology but without visible gross peritoneal metastasis. Patients with metastatic disease and patients with microscopically resection margin tumor-positive or macroscopically tumor-positive disease were excluded12. The Institutional Review Board of Chonnam National University Hwasun Hospital approved this study. All the procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional review board at Chonnam National University Hwasun Hospital in Jeonnam, Korea, and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study12.
Postoperative chemotherapy
We recommended postoperative chemotherapy for 85 patients excluding 3 patients; 2 patients are very old (>85) and 1 patient had several co-morbidities (chronic kidney disease and heart failure). 21 patients refused the chemotherapy. We administered postoperative chemotherapy with TS-1 (Taiho Pharmaceutical, Tokyo, Japan), oxaliplatin plus capecitabine (Xelox), oxaliplatin plus 5-fluorouracil (5-FU) (FOLFOX), or cisplatin plus TS-1 (CS) according to the physician’s judgement and patient preference. The Xelox regimen was administered every 3 weeks, and consisted of capecitabine (1,000 mg/m2 twice daily on days 1–14) plus intravenous oxaliplatin (130 mg/m2 on day 1)13. The TS-1 dose was determined based on body surface area (BSA). Patients received one of the following doses, divided in two, after meals daily: 80 mg for patients with a BSA < 1.25 m2, 100 mg for those with a BSA of 1.25–1.49 m2, and 120 mg for those with a BSA ≥ 1.50 m2. TS-1 was administered for 4 weeks followed by a 2-week rest period. TS-1 was administered for 1 year after surgery or until recurrence according to the physician’s judgement and patient preference12,14. The FOLFOX regimen was administered every 2 weeks, and consisted of intravenous oxaliplatin (85 mg/m2 on day 1), and leucovorin (200 mg/m2 on day 1), followed by 5-FU (2,600 mg/m2 intravenous continuous infusion over 24 h on day 1)15. TS-1 was given orally twice daily for the first 2 weeks of a 3-week cycle for patients on the CS regimen. The TS-1 dose was determined based on BSA, as described above. Cisplatin was given as an intravenous infusion of 60 mg/m2 on day 116. Postoperative chemotherapy was administered for 6 months; however, in cases of Xelox, FOLFOX, and CS, capectabine, 5-FU, and TS-1 were administered over 6 months and/or until recurrence12.
Follow-up
A physical examination, chest radiography, complete blood count, and biochemical tests were performed before each chemotherapy cycle. Computed tomography scans were performed every 2 months during the chemotherapy period and every 4 months thereafter until 5 years after surgery to assess tumor recurrence. If clinical signs or symptoms suggested clinical recurrence or the development of a new gastric cancer, further investigation was performed to determine whether the patient was disease free12.
Statistical analyses
OS was defined as the time from the date of surgery to the date of death. DFS was defined as the time from the date of surgery to the date of recurrence or death, whichever occurred first. If neither event had occurred at the time of analysis, the patient was censored. Survival curves were estimated using the Kaplan-Meier method, and survival times were compared using the log-rank test. Factors associated with OS and DFS were identified by univariate and multivariate Cox proportional hazard regression models with hazard ratios (HRs) and 95% confidence intervals (CIs). Differences were detected using the chi-square test or Fisher’s exact test for categorical data and the t-test or the Mann-Whitney U test for continuous data. Statistical analyses were performed using SPSS version 24.0 (IBM Corp., Armonk, NY, USA) and R (R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org) software. All P-values were two-sided, and P < 0.05 was considered significant12.
Results
Patient characteristics
The clinicopathological characteristics of the gastric cancer patients with positive cytology but without visible gross peritoneal metastasis (n = 88) are shown in Table 1. All of the patients were M1 disease (positive cytology). A total of 64 patients in chemotherapy group were comprised of 8 (12.5%) patients with T1/2/3 tumor, 56 (81.5%) with T4, 13 (20.3%) with N0/1/2 status, and 51 (79.7%) with N3. A total of 24 patients in surgery alone group were comprised of 1 (4.2%) patients with T1/2/3 tumor, 23 (95.8%) with T4, 3 (12.5%) with N0/1/2 status, and 21 (87.5%) with N3. The administered chemotherapy regimens were FOLFOX (n = 24), Xelox (n = 22), CS (n = 13), and TS-1 (n = 5). No significant differences were observed between the surgery, the postoperative chemotherapy group, or the surgery alone group in terms of age, sex, tumor location, Lauren classification, T stage, N stage, or perineural invasion. Most patients demonstrated T4 (chemotherapy vs. surgery alone, 81.5% vs. 95.1%) and N3 (chemotherapy vs. surgery alone, 79.7% vs. 87.5%) in both treatment groups. The chemotherapy group included more patients with a poorly differentiated/undifferentiated tumor grade and positive lymphovascular invasion (LVI+).
Survival analyses
Postoperative chemotherapy improved DFS and OS compared to surgery alone in gastric cancer patients with positive cytology but without visible gross peritoneal metastasis [chemotherapy (+) vs. surgery alone, median DFS 11.63 months (95% CI 9.28–13.98), vs. 6.98 months (95% CI 5.54–8.42), p < 0.001; median OS 25.50 months (95% CI 21.22–29.78) vs. 12.11 months (95% CI 10.47–13.75), p < 0.001]. The 1-year DFS rate was 46.9% in the chemotherapy group and 12.5% in the surgery alone group. The 1-year OS rate was 88.7% in the chemotherapy group and 50% in the surgery alone group (Fig. 1). There was no relationship between the survival and the regimen of postoperative chemotherapy.
In univariate analyses of risk factors for DFS, no chemotherapy and N3 status were significantly associated with poor DFS [chemotherapy (−), HR 3.41 (95% CI 1.95–5.95), p < 0.001; N3, HR 2.92 (95% CI 1.39–6.10), p = 0.004]. In univariate analyses of risk factors for OS, age ≥ 62 years, no chemotherapy, and N3 status were significantly associated with poor OS [age ≥ 62 years, HR 1.66 (95% CI 1.01–2.72), p = 0.045; no chemotherapy, HR 5.78 (95% CI 3.12–10.68), p < 0.001; N3, HR 2.58 (95% CI 1.23–5.41), p = 0.012] (Table 2). In multivariate analyses, no chemotherapy was the strongest independent clinical factor for poorer DFS [HR 3.76 (95% CI 1.95–7.24), p < 0.001] and OS [HR 4.37 (95% CI 2.24–8.49), p < 0.001].
We also performed binary logistic regression analyses to identify clinical factors associated with positive peritoneal washing cytology (Table 3). For this analysis, we included D2-resected stage II or III gastric cancer patients with negative peritoneal washing cytology (n = 197) (Supplementary Table 1). Gastroesophageal junction cancer and pT4 and pN3 status were significant independent clinical predictors for positive peritoneal washing cytology.
Discussion
The peritoneum is the most common metastatic site of recurrent or initially metastatic gastric cancer. Gastric cancer cells shed into the peritoneal space are believed to develop into peritoneal metastases. The presence of peritoneal metastasis at surgery is a poor prognostic marker, and radical gastrectomy should be reserved only for selected patients with an obstruction or bleeding17,18.
Gastric cancer patients with positive cytology but without visible gross peritoneal metastasis are classified as having M1 disease. However, the optimal therapeutic treatment modalities have not been established for these patients. Recent studies have demonstrated that neoadjuvant chemotherapy may improve survival if the cytology results become negative after treatment19,20. Another recent study also reported that gastric cancer patients with positive cytology and/or localized peritoneum metastasis who received surgical resection that leaves no macroscopically visible disease benefited from postoperative chemotherapy. They demonstrated median OS was from 24.7 months to 29.5 in the chemotherapy group, and 9.9 months in the no chemotherapy group21. In this study, we demonstrated that postoperative chemotherapy also improved OS and DFS compared to surgery alone in this gastric cancer population [chemotherapy (+) vs. surgery alone, median DFS 11.63 months vs. 6.98, p < 0.001; median OS 25.50 months vs. 12.11, p < 0.001].
Gastrectomy followed by chemotherapy did not result in any survival benefit compared with chemotherapy alone in gastric cancer patients with a visible peritoneal metastasis. Gastrectomy cannot be justified for treating patients with these tumors18. However, in this study, all patients underwent radical gastrectomy with D2 lymph node dissection because there were no visible peritoneal metastases at surgery, including other non-curable factors such as distant lymph node metastasis or liver metastasis.
Despite the recently reported benefits of a combination of chemotherapy plus trastuzumab, the prognosis of unresectable advanced or metastatic gastric cancer remains poor. In the ToGA trial, the median OS was 13.8 months in patients assigned to chemotherapy plus trastuzumab, and the median OS was 16.0 months in HER2-overexpressed patients assigned to chemotherapy plus trastuzumab22. More recently, a phase II study of nivolumab plus chemotherapy demonstrated promising progression-free survival of about 10 months, and OS was not reached23. In future clinical trials or retrospective analyses of chemotherapy, not only conventional chemotherapy, but also chemotherapy plus targeted agent such as trastuzumab or immune-oncologic drug such as nivolumab could be considered in this patient group.
This study has some limitations. This was a retrospective analysis involving a single institution. Second, the gross findings of peritoneal metastasis depended only on the surgeon’s skills and perspective. To some extent this could be subjective. We did not report the adverse events of the chemotherapy regimens; however, all regimens are widely used in a clinical setting, and all toxicities were manageable and did not differ from those reported previously. The gastric cancer treatment modalities used in Eastern and Western countries could be different. Perioperative treatment modalities are used in advanced gastric cancer cases in Western countries12,24.
In conclusion, postoperative chemotherapy improves the survival outcome compared to surgery alone in gastric cancer patients with positive peritoneal washing cytology but without visible gross peritoneal metastasis who underwent radical D2 gastrectomy.
References
Fitzmaurice, C. et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA oncology 3, 524–548, https://doi.org/10.1001/jamaoncol.2016.5688 (2017).
Jung, K. W. et al. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2014. Cancer research and treatment: official journal of Korean Cancer Association 49, 292–305, https://doi.org/10.4143/crt.2017.118 (2017).
Sakuramoto, S. et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. The New England journal of medicine 357, 1810–1820, https://doi.org/10.1056/NEJMoa072252 (2007).
Bang, Y. J. et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet (London, England) 379, 315–321, https://doi.org/10.1016/s0140-6736(11)61873-4 (2012).
Sasako, M. et al. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 29, 4387–4393, https://doi.org/10.1200/jco.2011.36.5908 (2011).
Noh, S. H. et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. The Lancet. Oncology 15, 1389–1396, https://doi.org/10.1016/s1470-2045(14)70473-5 (2014).
D’Angelica, M. et al. Patterns of initial recurrence in completely resected gastric adenocarcinoma. Annals of surgery 240, 808–816 (2004).
Brigand, C., Arvieux, C., Gilly, F. N. & Glehen, O. Treatment of peritoneal carcinomatosis in gastric cancers. Digestive diseases (Basel, Switzerland) 22, 366–373, https://doi.org/10.1159/000083600 (2004).
Coccolini, F. et al. Intraperitoneal chemotherapy in advanced gastric cancer. Meta-analysis of randomized trials. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 40, 12–26, https://doi.org/10.1016/j.ejso.2013.10.019 (2014).
De Andrade, J. P. & Mezhir, J. J. The critical role of peritoneal cytology in the staging of gastric cancer: an evidence-based review. Journal of surgical oncology 110, 291–297, https://doi.org/10.1002/jso.23632 (2014).
Bentrem, D., Wilton, A., Mazumdar, M., Brennan, M. & Coit, D. The value of peritoneal cytology as a preoperative predictor in patients with gastric carcinoma undergoing a curative resection. Annals of surgical oncology 12, 347–353, https://doi.org/10.1245/aso.2005.03.065 (2005).
Hwang, J. E. et al. Lymph-node ratio is an important clinical determinant for selecting the appropriate adjuvant chemotherapy regimen for curative D2-resected gastric cancer. Journal of cancer research and clinical oncology 145, 2157–2166, https://doi.org/10.1007/s00432-019-02963-7 (2019).
Kim, G. M. et al. A randomized phase II trial of S-1-oxaliplatin versus capecitabine-oxaliplatin in advanced gastric cancer. European journal of cancer (Oxford, England: 1990) 48, 518–526, https://doi.org/10.1016/j.ejca.2011.12.017 (2012).
Koizumi, W. et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. The Lancet. Oncology 9, 215–221, https://doi.org/10.1016/s1470-2045(08)70035-4 (2008).
Al-Batran, S. E. et al. Phase III trial in metastatic gastroesophageal adenocarcinoma with fluorouracil, leucovorin plus either oxaliplatin or cisplatin: a study of the Arbeitsgemeinschaft Internistische Onkologie. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 26, 1435–1442, https://doi.org/10.1200/jco.2007.13.9378 (2008).
Koo, D. H. et al. Three-week combination chemotherapy with S-1 and cisplatin as first-line treatment in patients with advanced gastric cancer: a retrospective study with 159 patients. Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association 15, 305–312, https://doi.org/10.1007/s10120-011-0117-2 (2012).
Kobayashi, D. & Kodera, Y. Intraperitoneal chemotherapy for gastric cancer with peritoneal metastasis. Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association 20, 111–121, https://doi.org/10.1007/s10120-016-0662-9 (2017).
Fujitani, K. et al. Gastrectomy plus chemotherapy versus chemotherapy alone for advanced gastric cancer with a single non-curable factor (REGATTA): a phase 3, randomised controlled trial. The Lancet. Oncology 17, 309–318, https://doi.org/10.1016/s1470-2045(15)00553-7 (2016).
Jamel, S. et al. Prognostic significance of peritoneal lavage cytology in staging gastric cancer: systematic review and meta-analysis. Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association 21, 10–18, https://doi.org/10.1007/s10120-017-0749-y (2018).
Yamamoto, M. et al. Comparison of Neoadjuvant Chemotherapy to Surgery Followed by Adjuvant Chemotherapy in Japanese Patients with Peritoneal Lavage Cytology Positive for Gastric Carcinoma. Anticancer research 35, 4859–4863 (2015).
Yamaguchi, T. et al. Efficacy of postoperative chemotherapy after resection that leaves no macroscopically visible disease of gastric cancer with positive peritoneal lavage cytology (CY1) or localized peritoneum metastasis (P1a): A multicenter retrospective study. Annals of surgical oncology 27, 284–292, https://doi.org/10.1245/s10434-019-07697-x (2020).
Bang, Y. J. et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet (London, England) 376, 687–697, https://doi.org/10.1016/s0140-6736(10)61121-x (2010).
Boku, N. et al. Safety and efficacy of nivolumab in combination with S-1/capecitabine plus oxaliplatin in patients with previously untreated, unresectable, advanced, or recurrent gastric/gastroesophageal junction cancer: interim results of a randomized, phase II trial (ATTRACTION-4). Annals of oncology: official journal of the European Society for Medical Oncology 30, 250–258, https://doi.org/10.1093/annonc/mdy540 (2019).
Smyth, E. C. et al. Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of oncology: official journal of the European Society for Medical Oncology 27, v38–v49, https://doi.org/10.1093/annonc/mdw350 (2016).
Acknowledgements
This study was supported by a grant (HCRI20052) of the Chonnam National University Hwasun Hospital Research Institute of Clinical Medicine.
Author information
Authors and Affiliations
Contributions
H.J. Shim and H.J. Kim wrote the main manuscript text. S.H. Lee prepared Figure 1. E.C. Hwang made substantial contributions to the statistical analysis. H.J. Bang, W.K. Bae, S.H. Cho, and I.J. Chung performed the chemotherapy for patients and revised the manuscript. J.E. Hwang conceived of the study and controlled all steps of drafting the manuscript . All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shim, HJ., Kim, HJ., Lee, S.H. et al. Observational Study of Peritoneal Washing Cytology-Positive Gastric Cancer without Gross Peritoneal Metastasis in Patients who Underwent Radical D2 Gastrectomy. Sci Rep 10, 9549 (2020). https://doi.org/10.1038/s41598-020-66637-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-66637-y
This article is cited by
-
Preoperative neutrophil-to-platelet ratio as a potential prognostic factor for gastric cancer with positive peritoneal lavage cytology in the absence of other non-curative factors: a multi-institutional dataset analysis
Surgery Today (2023)
-
ARHGAP–RhoA signaling provokes homotypic adhesion-triggered cell death of metastasized diffuse-type gastric cancer
Oncogene (2022)
-
Prognostic factors for cytology-positive gastric cancer: a multicenter retrospective analysis
International Journal of Clinical Oncology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.