Abstract
We aimed to compare subjective (S) vs. objective (O) selective carious tissue removal using hand-excavation versus a self-limiting polymer bur, respectively. A community-based single-blind cluster-randomized controlled superiority trial was performed. This is a 1-year-interim analysis. 115 children (age 7–8 years) with ≥1 vital primary molar with a deep dentin lesion (>1/2 dentin depth) were included (60 S/55 O). The cluster was the child, with eligible molars being treated identically (91 S/86 O). Cavities were prepared and carious tissue on pulpo-proximal walls selectively removed using hand instruments (S), or a self-limiting polymer bur (Polybur P1, Komet). Cavities were restored using glass-hybrid material (Equia Forte, GC). Treatment times and children’s satisfaction were recorded. Generalized-linear models (GLM) and multi-level Cox-regression analysis were applied. Initial treatment times were not significantly different between protocols (mean; 95%CI S: 433; 404–462 sec; O: 412; 382-441 sec; p = 0.378/GLM). There was no significant difference in patients’ satisfaction (p = 0.164). No pulpal exposures occurred. 113 children were re-examined. Failures occurred in 22/84 O-molars (26.2%) and 26/90 S-molars (28.9%). Pulpal complications occurred in 5(6%) O and 2(2.2%) S molars, respectively. Risk of failure was not significantly associated with the removal protocol, age, sex, dental arch or tooth type (p > 0.05/Cox), but was nearly 5-times higher in multi-surface than single-surface restorations (HR: 4.60; 95% CI: 1.70-12.4). Within the limitations of this interim analysis, there was no significant difference in treatment time, satisfaction and risk of failure between O and S.
Similar content being viewed by others
Introduction
For deep carious lesions, selective carious tissue removal, where soft tissue remains in pulpal cavity areas and is sealed beneath a (mainly adhesive) restoration is recommended over more invasive non-selective (“complete”) removal, mainly as the risk of pulp exposure is significantly reduced1. Alternatively, such lesions in primary molars may be managed via sealing them beneath stainless steel crowns (Hall Technique), if available2. Avoiding pulp exposure is relevant, as oftentimes more invasive therapies like pulpotomy or removal of the tooth are needed if the pulp is exposed in primary teeth. Some children, e.g. those with limited compliance and dental fear, may not accept these under local anesthetics. They may further come with the risk of systemic adverse events and high costs1.
For selective removal, the current standard technique is to subjectively (i.e. arbitrarily and not necessarily reproducible) remove carious dentin (using hand or rotary instruments) until only hard dentin remains peripherally, and soft, leathery or firm dentin in pulp-proximal areas. An alternative and more objective removal technique involves self-limiting polymer burs (like Polybur P1, Komet, Lemgo, Germany)3. These are manufactured from medical-grade polyether-ketone-ketone4,5, and are harder than soft dentin but softer than firm or hard dentin6, on which the bur abrades and hence does not remove any further hard tissue7.
Self-limiting burs have been validated in vitro for selectivity (removing less sound dentin than conventional carious tissue removal)8. Also, adhesive bond strengths to the dentin walls remaining after using these burs instead of conventional excavation have been tested, demonstrating decreased bond strengths when using self-limiting burs9. Clinically, though, such self-limiting burs have only sparsely been applied, mainly on their impact on peri-operative pain or the required removal time10. Hence, at present, it remains unclear if clinically relevant outcomes like the risk of pulp exposure or pulpal and restorative success (absence of complications) and tooth survival are improved if performing such “objective” instead of “subjective” selective removal3,11,12.
Therefore, the aim of this study was to compare subjective (S) versus objective (O) carious tissue removal of deep dentin lesions in primary molars with vital and non-symptomatic pulps, by means of a community-based cluster-randomized trial. Our hypothesis was that O is significantly more efficacious (higher success) than S. We here present a 1-year interim analysis.
Methods
Overview
This is a community-based single-blinded cluster-randomized controlled superiority trial. Reporting manuscript follows the CONSORT (Consolidated Standards of Reporting Trials) guidelines. The trial was approved by the Research Ethics Committee of the University of Brasília Medical School (1.400.687/2016) and registered at Clinicaltrials.gov (NCT02754466) 28.04.2016. We confirm that all research was performed in accordance with relevant guidelines (Declaration of Helsinki) and regulations. The protocol to this trial was published elsewhere13 and deviations from this protocol are laid out below. The CONSORT checklist is available within the supplementary files. The study flowchart is shown in Fig. 1.
Sample size estimation
The unit of analysis was the tooth. Hence, this a multilayered cluster-randomized trial, with the patient and the school being the clusters. Clustering was taken into account using the so-called Lee, Wei and Amato (LWA) model for clustered survival data14. Sample size estimation for this model was based on the ideas of Xie and Waksman15. It was assumed that at 36 months (planned total follow-up time), 90% of O-molars and 80% of S-molars would show no complication (success). The assumption of superiority of the polymer bur protocol (O) was justified given the higher cost associated with this strategy and the ease of performing the conventional S protocol. Considering α = 0.05 and 1 − β = 0.9, as well as an intra-cluster correlation of 0.8 and a mean of 1.5 teeth treated per child, the required sample was 45 per group. Assuming an annual sample loss of 20%, the required sample was 57 per group. A total of 115 patients (177 teeth) participated in the study.
Sample selection
This clinical trial is part of a larger study that aimed to evaluate the impact of oral health in children’s quality of life, anthropometric and cognitive development. Overall, 926 children were examined in six public schools of Paranoá, a deprived suburban area of Brasilia, the capital of Brazil. Given that children in this area of Brasilia come from a low socio-economic background and show a high mean d3mft at baseline, and considering this community having limited access to dental services16, we assume all children to show high caries risk. Note, though, that no formal caries risk assessment was provided in the present study.
All children received dietary advice and oral hygiene instructions. Two calibrated dentists performed the recruitment and treatment for this trial. The inclusion criteria were as follows: (1) age between 7–8 years; (2) good general health; (3) informed consent of the parents and/or carers (4) cooperation of the children for the required treatment steps; (5) at least one vital, clinically and radiographically non-symptomatic, retainable, deeply carious primary molar; and (6) the child being a student in one of the six schools of Paranoa (which was relevant to ensure follow-up).
The lesion needed to be active and to radiographically extend into the inner half of the dentin. An external examiner, previously calibrated, was responsible for measuring the depth of the lesions on radiographs. Single and multiple surface lesions were included; the size of the cavity (single or multiple surface) was recorded after carious tissue removal and preparation (see below).
Patients that were participating in another study or planning to move away, as well as those who were not residents of Paranoa, patients with systemic diseases or disabilities, with known allergies to dental materials used within the study, as well as those with expected limited compliance, and patients with teeth expected to exfoliate within the next 18 months were not included. Non-eligible patients were treated according to their need via referral to the pedodontics service of the University of Brasília.
Patients and their parents/carers were provided with information leaflets concerning the study and fully informed about the study verbally, too. Informed consent was obtained from all the parents/legally authorized representative of the participants included in the study when attending the second, treatment appointment in the mobile unit (see below). There were minimum 24 h and maximum one week between the first and second appointment.
Sequence generation, allocation and blinding
A random sequence was generated via random numbers tables. The allocation was concealed using opaque sealed envelopes, with an overall 120 envelopes (60 per group) being used. Envelopes were only opened when the child was seated in the chair and ready for treatment. As 115 children were included on the study, study groups are not perfectly balanced (five envelopes were never opened).
Due the obvious differences between the restorative protocols, blinding of the operator and the patient was not possible. Nevertheless, since the restorative material was the same in both groups, examiners’ blinding during follow-up was feasible. In addition, the participants and their caregivers were informed about the importance of not providing information to the examiners about the study arm. Follow-up radiographs were not performed due to radiation protection reasons.
Treatment procedure
Treatment was carried out between May and December 2017. During the treatment, data for each tooth and patient was collected using pilot-tested case report forms. We collected data on the treated tooth (dental arch and tooth number), the surfaces involved, the time needed for treatment, and the satisfaction of the patient with the treatment.
The treatment was provided by two previously trained and calibrated dentists in a mobile dental unit. Operators were trained on all steps of both protocols, including the pressure to be exerted with the polymer bur using a precision scale. Both protocols were trained on a total of 24 extracted teeth. Moreover, training was conducted clinically in four molars of two children that were not part of the study.
Preparation was similar for both protocols. To prepare the patients prior to the treatment, the management technique “tell-show-do”17 was applied. After cleaning the tooth with a rotatory brush, relative moisture control using cotton wool rolls and suction was performed. If needed, cavities were opened using water-cooled diamond burs (1012 e 1014, KG, Sorensen, Cotia, Brazil). Conventional stainless steel rose head burs (3 and 5, Maillefer, Dentsply, Konstanz, Germany) were used in low rotation to remove peripheral carious dentin until only hard, dry dentin remained. The removal of the pulp-axial carious dentin was performed differently in both arms:
O: Objective, self-limiting polymer bur removal. The polymer bur (PolyBur) was used on low rotation until the bur abraded and further removal of softened dentin was not possible.
S: Subjective removal using hand excavation. Removal of carious dentin was performed using hand instruments (Duflex, Rio de Janeiro, Brazil), and selective removal to leathery, slightly moist and reasonably soft dentin (i.e., dentin which cannot be removed using an excavator without force) was performed1.
Local anesthesia (Alphacaine 100, Nova DFL, Rio de Janeiro, Brazil) was applied only if the child reported pain during de procedure (only two cases in the O group). All cavities were restored with a glass hybrid restorative system (Equia Forte, GC, Tokyo, Japan) following the manufactures’ instructions as follows. The cavity was conditioned with the GC Cavity Conditioner for 10 seconds, then rinsed and the excess of water removed with a cotton pellet. After capsule activation and mixing, the material was inserted into the cavity, using the capsule applier. Digital compression, excess removal and occlusal checking were performed before the surface was coated with Equia Forte Coat, which was light cured for 20 seconds. On multi-surfaces cavities, the use of a metallic matrix was required.
Recording of treatment times was only started when the operator removed the first instrument from the tray; the assistant set the timer. The timing was completed when the operator stated that the Equia Forte Coat was finally cured. If several restorations were performed in the same patient, this time measurement was performed for each restoration.
Upon completion of each restoration, patients were asked by the assistant in the absence of the operator ‘how satisfied were you with this treatment?’. For this purpose, a Likert Scale was used, with five satisfaction points (very satisfied, satisfied, neutral, dissatisfied and very dissatisfied), illustrated by facial expression figures, with the purpose of facilitating the comprehension of the child.
Follow-up
The restorations were evaluated by two independent trained evaluators, who did not take part in the treatment phase, using the ART criteria18,19. Calibration and training of the evaluators on the ART criteria was performed before the study in children that attended the pedodontics service of the University Dental Clinic until a good agreement was observed. Duplicate examinations during follow-up were performed in 15 children to enable Kappa calculation (inter-examiner agreement: 0.85) and repeated after 30 days (intra-examiner agreement: 0.87 for both examiners). Moisture control was performed using cotton rolls and continuous aspiration. The restorations were classified as ‘success’ if they were present and satisfactory, or if a slight marginal defect was observed (scores 00 and 01). Codes 2–6 featured restorative failures that could be arising from fracture or a secondary carious lesion. Restorations with codes 7–9 indicated censored information. Pulpal complications were determined via the assessment of pain, sensitivity to percussion or cold/hot, swelling, sinus formation or the resulting need for extraction. The evaluators were equipped with headlamps (Kudos, Hong Kong, China), dental mirrors and CPITN probes (Golgran, São Caetano do Sul, Brazil).
Statistical analysis
Descriptive statistics and pairwise testing using t- and Chi-square test were applied. Time and patient satisfaction data were statistically analyzed by generalized linear mixed models, with the covariates protocol (S vs. O), dental arch (upper vs. lower), primary molar (first vs. second), cavity extension (single- versus multi-surfaced) and operators (1 vs. 2); the patient and the school were introduced as random factors. Restoration survival was evaluated using multi-level Cox-test, accounting for clustering. The confidence level was set at 95% (α = 0.05). The analyses were performed using SPSS 24 (IBM, Armonk, USA). Multiple imputation and sensitivity analyses are planned for the final evaluation but were not conducted for the present interim evaluation.
Ethical approval and informed consent
The trial was approved by the Research Ethics Committee of the University of Brasília Medical School (1.400.687/2016) and registered at Clinicaltrials.gov (NCT02754466). Informed consent was obtained from all the parents/legally authorized representative of the participants included in the study. We confirm that all research was performed in accordance with relevant guidelines (Declaration of Helsinki) and regulations.
Results
The sample characteristics are presented in Table 1. A total of 177 restorations were placed, 86 using the objective protocol (O) and 91 using the subjective protocol (S), in 115 children (55 O, 60 S). There were no significant differences (p > 0.05) between the patients in both arms with regards to patients’ age or sex, or dental arch, primary molar, or surface extension of the treated lesions.
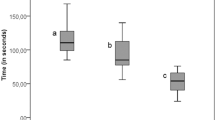
The mean (95% CI) treatment time (Table 2) was 412 (382–441) s and 433 (404–462) s in O and S, respectively (p > 0.05). Also, no significant differences in time according to molar, lesion extension or operator emerged (p > 0.05). Treatment time was significantly shorter in lower than upper molars (p = 0.004).
Patients were generally highly satisfied with their treatment (Table 3), without significant differences between groups (p > 0.05).
No pulp exposures occurred. Two patients, both in group O, reported pain during restorative treatment, with local anesthesia being provided.
After a mean (SD, range) 13 (2; 8–18) months, 90 restorations in S and 84 in O were evaluated. Most complications were restorative (Table 4). Pulpal complications occurred in 5 (6%) and 2 (2.2%) molars of O and S, respectively. In all cases where a pulpal complication occurred, a restorative failure was also present. There were more failures in multiple surface restorations than in single surface restorations in both groups. Risk of failure was not significantly associated with the removal protocol, age, sex, dental arch or tooth type (p > 0.05/Cox). The only significant association was found between surface extension and survival (Table 5).
If using ART criteria, the total loss of the restoration (code 6) was most frequent, followed by restoration fracture (code 3) and by margin defects (code 2). Details are presented in Table 6.
Discussion
The present study reports an interim analysis of a randomized trial comparing objective versus subjective carious tissue removal in deep carious lesions in primary molars. Using a removal method which determines when to stop removal could increase the uptake of selective removal among practitioners (who only slowly tend to adopt this technique), mainly as the endpoint of removal is more reliable. It may also allow standardizing removal for scientific purposes. We found that, after 1 year, no significant differences in success or survival occurred, with most failures being restorative. Generally, the annual failure rate was high. Treatment time was not statistically different between the two protocols, while patients rated both strategies as highly satisfying.
While there is only limited clinical data on self-limiting, objective carious tissue removal, it has been reported that such burs allow a reproducible level of selectivity20,21, while it remains unclear if this yields any advantage when compared with subjective selective removal. We assessed the success and survival in O and S groups. In the present study, the low number of pulp exposures that occurred for both groups may be related to the training provided to both operators and to the fact that operators could gauge the radiographic extend and lesion depth prior to the intervention. We also found the risk of failure to be similar in both groups, with annual failure rates being slightly higher than what was reported by other studies on primary teeth that also used a glass hybrid restorative system22,23. One plausible explanation may be that we only included deep and mainly extended cavities, which might have had a negative influence on restoration survival. Clearly, even using selective (instead of non-selective) removal, the management of deep lesions in primary molars with a direct restorative approach is challenging. Our study calls for a more biologically grounded approach, e.g. involving the Hall Technique or non-restorative cavity control (where lesions are not restored, but inactivated). The latter, however, has been found to come with limited efficacy in non-adherent groups24.
Overall, our study does not confirm that O is superior (which may be demanded given the possibly higher costs) but indicates that both strategies perform similar when it comes to pulpal and restorative complications. Hence, if desiring a more standardized, reproducible endpoint of removal, O may be justified. More long-term data are needed to confirm if different removal strategies truly do not come with different pulpal or restorative risks.
In terms of time, it has already been shown that primary molar cavity preparation with rotary burs tends to be faster than with manual instruments. However when the total time to complete the procedure (including placement of the restoration) is added, no significant difference remains25. Our data corroborate this assumption, as the total time spent for both O and S groups was not significantly different. However, it is important to highlight that the variance in treatment times was generally high, and our study was likely underpowered to detect significant differences. Given that the material costs for O (which are single-use instruments) are higher, it may well be that treatment costs are higher using O than S.
Procedures involving rotary instruments might induce anxiety in children during dental treatment26. We hence expected to detect a difference in the immediate patient satisfaction rates between O and S but could not confirm this assumption. It might be that applying the “tell-show-do” technique17 as part of the clinical routine to psychologically prepare patients26,27 might have facilitated favorable treatment conditions and patients’ satisfaction. Further, the treatment was performed at school and not a dental clinic, which may again be favorable for patients’ perceptions26.
In our study, multiple surface restorations were about five times more likely to fail compared to single-surface restorations, which is consistent with a large body of evidence18,28,29. Especially for such multi-surface cavities, the described biological approaches involving stainless steel crowns may be advantageous.
This study has a number of limitations. First, this is an interim analysis, and we cannot deduce longer term results. It should be highlighted that interim analyses may come with risks of erroneous conclusions due to repeated testing, but also limited robustness of the yielded data (given that the study was powered for the final follow-up). Notably, we decided to nevertheless conduct such analysis as our study may give guidance to practitioners who, at present, do not have any clinical evidence as to the efficacy of self-limiting burs. Also note that endpoints like pulp exposure, satisfaction or treatment time will not be affected by follow-up. As a caveat, further outcomes which we plan to assess during follow-up (like cost-effectiveness) could not be reported here. Second, this is a superiority study, while one might argue that for similar treatments like O vs. S, one could also conduct a non-inferiority trial, which comes with different concepts in sample size estimation and statistical power. We, however, strongly believe that the self-limiting excavation should prove superiority given that there is a valid, established, applicable and easy way to conduct selective removal using subjective criteria and a hand excavator or conventional bur. Even when considering alternative outcomes like treatment time or comfort, which may justify the use of the self-limiting excavation in case the clinical efficacy may not be significantly different from that of conventional excavation, the notion of superiority is upheld. Third, given that no radiographic follow-up was performed due to radiation protection, we are likely to underestimate the true risk of pulpal failures (e.g. inter-radicular lesions or resorptions might not have been detected). Fourth, we used the child’s satisfaction as patient-reported outcome, while admittedly, pain during treatment could have been measured, too. It is known that measuring pain in children is challenging, especially when the pain level is low, and that different scales do not necessarily agree with each other30. Last, dropouts were handled as missing at random, and no imputation was performed for the present interim analysis. We will consider more extensive handling of attrition in the final report, and generally assume the extremely low attrition in this analysis to not have a relevant impact on our findings.
Conclusion
Within the limitations of this interim analysis, objective and subjective selective carious tissue removal did not present significantly different success and survival. Despite deep lesions being managed, the risk of pulpal complications was low, and most failures were restorative by nature (regardless of the study arm). Both treatment time and immediate patient satisfaction did also not differ significantly between protocols. As expected, multiple surface restorations had a higher failure rate than single surface restorations. It is important to emphasize that these data stem from a one-year interim evaluation, and that longer follow-up assessments may provide important additional information. Based on the outcomes of this analysis, though, dentists may consider both objective and subjective selective carious tissue removal for deep lesions in primary molars.
Data availability
The database can be made available on request provided data protection rules can be fulfilled.
References
Schwendicke, F. et al. Managing Carious Lesions: Consensus Recommendations on Carious Tissue Removal. Adv Dent Res 28, 58–67, https://doi.org/10.1177/0022034516639271 (2016).
Innes, N. P., Evans, D. J. & Stirrups, D. R. Sealing caries in primary molars: randomized control trial, 5-year results. J Dent Res 90, 1405–1410, https://doi.org/10.1177/0022034511422064 (2011).
Boston, D. W. New device for selective dentin caries removal. Quintessence Int 34, 678–685 (2003).
Soni, H. K., Sharma, A. & Sood, P. B. A comparative clinical study of various methods of caries removal in children. Eur Arch Paediatr Dent 16, 19–26, https://doi.org/10.1007/s40368-014-0140-1 (2015).
Aswathi, K. K. et al. Comparison of efficacy of caries removal using polymer bur and chemomechanical caries removal agent: A clinical and microbiological assessment - An in vivo study. J Indian Soc Pedod Prev Dent 35, 6–13, https://doi.org/10.4103/0970-4388.199232 (2017).
Innes, N. P. et al. Managing Carious Lesions: Consensus Recommendations on Terminology. Adv Dent Res 28, 49–57, https://doi.org/10.1177/0022034516639276 (2016).
Jingarwar, M., Bajwa, N. & Pathak, A. Minimal intervention dentistry - a new frontier in clinical dentistry. J Clin Diagn Res 8, ZE04–08, https://doi.org/10.7860/JCDR/2014/9128.4583 (2014).
Lohmann, J., Schafer, E. & Dammaschke, T. Histological determination of cariously altered collagen after dentin caries excavation with the polymer bur PolyBur P1 in comparison to a conventional bud bur. Head Face Med 15, 19, https://doi.org/10.1186/s13005-019-0205-9 (2019).
Silva, N. R., Carvalho, R. M., Pegoraro, L. F., Tay, F. R. & Thompson, V. P. Evaluation of a self-limiting concept in dentinal caries removal. J Dent Res 85, 282–286 (2006).
Prabhakar, A. & Kiran, N. K. Clinical evaluation of polyamide polymer burs for selective carious dentin removal. J Contemp Dent Pract 10, 26–34 (2009).
Schwendicke, F., Paris, S. & Tu, Y. K. Effects of using different criteria for caries removal: a systematic review and network meta-analysis. J Dent 43, 1–15, https://doi.org/10.1016/j.jdent.2014.10.004 (2015).
Meller, C., Welk, A., Zeligowski, T. & Splieth, C. Comparison of dentin caries excavation with polymer and conventional tungsten carbide burs. Quintessence Int 38, 565–569 (2007).
Schwendicke, F. et al. Selective carious tissue removal using subjective criteria or polymer bur: study protocol for a randomised controlled trial (SelecCT). BMJ Open 8, e022952, https://doi.org/10.1136/bmjopen-2018-022952 (2018).
Lee E, W. L., Amato D. A. Cox-type Regression Analysis for Large Number of Small Groups of Correlated Failure Time Observations. Survival Analysis: State of the Art, 237–247 (1992).
Xie, T. & Waksman, J. Design and sample size estimation in clinical trials with clustered survival times as the primary endpoint. Stat Med 22, 2835–2846, https://doi.org/10.1002/sim.1536 (2003).
Amorim, R., Figueiredo, M., Leal, S., Mulder, J. & Frencken, J. Caries experience in a child population in a deprived area of Brazil, using ICDAS II. Clinical Oral Investigations 16, 513–520, https://doi.org/10.1007/s00784-011-0528-9 (2012).
Lyons, R. A. Understanding basic behavioral support techniques as an alternative to sedation and anesthesia. Spec Care Dentist 29, 39–50, https://doi.org/10.1111/j.1754-4505.2008.00061.x (2009).
Hilgert, L. A., Frencken, J. E., de Amorim, R. G., Mulder, J. & Leal, S. C. A study on the survival of primary molars with intact and with defective restorations. Int J Paediatr Dent 26, 383–390, https://doi.org/10.1111/ipd.12215 (2016).
Hilgert, L. A. et al. Is high-viscosity glass-ionomer-cement a successor to amalgam for treating primary molars? Dent Mater 30, 1172–1178, https://doi.org/10.1016/j.dental.2014.07.010 (2014).
Rima Maarouf, S. B. Hala Ragab. Clinical Efficiency of Polymer Burs in Caries Removal in Primary Molars and Relevant Pain Perception: A Randomized Controlled Trial. International Arab Journal of Dentistry 9, 9–14 (2018).
Celiberti, P., Francescut, P. & Lussi, A. Performance of four dentine excavation methods in deciduous teeth. Caries Res 40, 117–123, https://doi.org/10.1159/000091057 (2006).
Kupietzky, A., Atia Joachim, D., Tal, E. & Moskovitz, M. Long-term clinical performance of heat-cured high-viscosity glass ionomer class II restorations versus resin-based composites in primary molars: a randomized comparison trial. European Archives of Paediatric Dentistry 41, 264–270, https://doi.org/10.1007/s40368-019-00423-x (2019).
de França Lopes CMC, S. E., Martins AS, Loguercio AD, Reis A, Chibinski ACR, Wambier DS. Randomized Clinical Trial of ART Class II Restorations Using Two Glass Ionomer Cements: One-Year Follow-Up. Pediatric Dentistry 40, 98–104 (2018).
Santamaria, R. M. et al. Alternative Caries Management Options for Primary Molars: 2.5-Year Outcomes of a Randomised Clinical Trial. Caries Res 51, 605–614, https://doi.org/10.1159/000477855 (2018).
de Amorim, R. G., Leal, S. C., Mulder, J., Creugers, N. H. & Frencken, J. E. Amalgam and ART restorations in children: a controlled clinical trial. Clin Oral Investig 18, 117–124, https://doi.org/10.1007/s00784-013-0955-x (2014).
de Menezes Abreu, D. M., Leal, S. C., Mulder, J. & Frencken, J. E. Patterns of dental anxiety in children after sequential dental visits. European Archives of Paediatric Dentistry 12, 298–302, https://doi.org/10.1007/bf03262827 (2012).
Ishan et al. Anxiety Levels among Five-Year-Old Children Undergoing ART Restoration-A Cross-Sectional Study. J Clin Diagn Res 11, 45–48, https://doi.org/10.7860/JCDR/2017/19194.9667 (2017).
Schwendicke, F., Meyer-Lueckel, H., Dorfer, C. & Paris, S. Failure of incompletely excavated teeth-a systematic review. J Dent 41, 569–580, https://doi.org/10.1016/j.jdent.2013.05.004 (2013).
Demarco, F. F., Correa, M. B., Cenci, M. S., Moraes, R. R. & Opdam, N. J. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater 28, 87–101, https://doi.org/10.1016/j.dental.2011.09.003 (2012).
Bringuier, S. et al. A prospective comparison of post-surgical behavioral pain scales in preschoolers highlighting the risk of false evaluations. Pain 145, 60–68, https://doi.org/10.1016/j.pain.2009.05.012 (2009).
Acknowledgements
This study was supported by Komet, Lemgo, Germany, with materials and some material costs, as well as GC Europe with restoration material. The study was supported by the Brazilian Federal District Research Support Foundation (FAPDF grant number 0193.001463/2016).
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: Marta Gomes Marques, Leandro Augusto Hilgert, Falk Schwendicke, Soraya Coelho Leal. Contributed to acquisition, analysis, or interpretation of data: Marta Gomes Marques, Leandro Augusto Hilgert, Larissa Ribeiro Silva, Karine Medeiros Demarchi, Patrícia Magno dos Santos Matias, Ana Paula Dias Ribeiro, Soraya Coelho Leal, Sebastian Paris, Falk Schwendicke. Drafted the manuscript: Marta Gomes Marques, Leandro Augusto Hilgert, Falk Schwendicke, Soraya Coelho Leal. Critically revised the manuscript for important intellectual content: All authors. Have approved submission of the version and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. All authors.
Corresponding author
Ethics declarations
Competing interests
The authors would like to thank Komet, Lemgo, Germany, for kindly supporting this study with materials and covering some material costs. The authors would like to thank GC Europe for providing the restoration material. These funders had no influence on the design, conduct or reporting of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Marques, M.G., Hilgert, L.A., Silva, L.R. et al. Subjective versus objective, polymer bur-based selective carious tissue removal: 1-year interim analysis of a randomized clinical trial. Sci Rep 10, 9130 (2020). https://doi.org/10.1038/s41598-020-66074-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-66074-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.