Abstract
Aims To assess the radiographic and periodontal healing of combined endo-perio lesions in anterior teeth treated with orthograde root canal treatment (RCT), with and without guided tissue regeneration (GTR) and bone grafting.
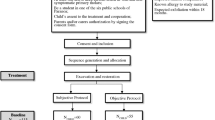
Sample selection A total of 120 individuals attending the Dental University Hospital in Riyadh, Saudi Arabia, diagnosed with true combined endo-perio lesions were selected. Inclusion criteria included being between 25 and 55 years old and having a single-rooted non-vital maxillary anterior tooth with a true combined endo-perio lesion, assessed using a cone beam computed tomography (CBCT) scan. Exclusion criteria included uncontrolled systemic disease, a history of oral cancer or sepsis, recent use of antibiotics, the use of bone metabolism modifying drugs and the presence of fractures, resorption or associated pathological cysts. Power calculations were used to set a minimum sample size of 120 teeth.
Design A randomised controlled trial involving four treatment arms: root canal treatment (RCT) with gutta percha (GP) obturation; RCT with mineral trioxide aggregate (MTA) obturation; RCT with GP obturation and guided tissue regeneration (GTR); and RCT with MTA obturation and GTR. Participants were randomly assigned using computer software to each treatment arm via block randomisation.
Baseline periodontal measurements (gingival phenotype, keratinised tissue width, pocket depth and clinical attachment level) and a CBCT scan to obtain a CBCT periapical index (CBCTPAI) score were taken at visit one. Visit two involved scaling, root planing and a RCT performed using hand files and a thermoplastic obturation technique for the GP obturation arm (Obtura II, Obtura Spartan, USA) and vertical compaction for the MTA obturation arm (ProRoot White, Dentsply, USA). Visit three (for the GTR and bone-grafting arms), one week later, included regenerative periodontal surgery - raising a three-sided buccal flap, removal of granulation tissue, filling the defect with demineralised, freeze-dried bone allograft, coverage with a resorbable collagen membrane and closure with resorbable sutures. Visit two was performed by a single endodontist and visit three, for the GTR and bone grafting arms, was performed by a single periodontist. Previous or future planned treatment was concealed to operators and they were only informed of the treatment to be performed on the day. All teeth received definitive restorations.
The follow-up schedule was one, three, six and twelve months post-treatment. CBCT scans were repeated at six and twelve months; clinical periodontal measurements were repeated at three, six and twelve months.
Data analysis Descriptive analysis was performed and results were presented as cross-tabulations and a bar chart. Inferential statistics were used; one-way analysis of variance with Tukey's multiple comparison test to compare the mean value of measurements between treatment arms at follow-up visits and Kruskal-Wallis test to compare mean CBCTPAI scores between arms at follow-up visits. The p-value was set at ≤0.05.
Results Baseline comparison showed no statistically significant differences between treatment arms. No participants were lost to follow up. At 12 months, GTR showed improved healing, with 98% of cases showing CBCTPAI scores better than 1, compared to 100% cases scoring 1 + D or worse without GTR. Statistically significant differences were found between treatment arms with respect to CBCTPAI score and pocket depth at 12 months.
Conclusions GTR may improve radiographically-assessed healing of combined endo-perio lesions. MTA obturation may play a role in the management of combined endo-perio lesions. Study limitations do not allow for more definitive conclusions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Change history
25 March 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41432-022-0234-2
References
Rotstein I, Simon J H. The endo-perio lesion: a critical appraisal of the disease condition. Endod Topics 2006; 13: 34-56.
Schmidt J C, Walter C, Amato M, Weiger R. Treatment of periodontal-endodontic lesions a systematic review. J Clin Periodontol 2014; 41: 779-790.
Simon J H, Glick D H, Frank A L. The relationship of endodontic-periodontic lesions. J Periodontol 1972; 43: 202-208.
Estrela C, Bueno M R, Azevedo B C, Azevedo J R, Pecora J D. A new periapical index based on cone beam computed tomography. J Endod 2008; 34: 1325-1331.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Adam, M. 'Combined endo-perio lesions' - what is the best treatment?. Evid Based Dent 22, 158–159 (2021). https://doi.org/10.1038/s41432-021-0230-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-021-0230-y