Abstract
Atorvastatin (ATV) is a blood cholesterol-lowering drug used to prevent cardiovascular events, the leading cause of death worldwide. As pharmacokinetics, metabolism and response vary among individuals, we wanted to determine the most reliable metabolic ATV phenotypes and identify novel and preponderant genetic markers that affect ATV plasma levels. A controlled, randomized, crossover, single-blind, three-treatment, three-period, and six-sequence clinical study of ATV (single 80-mg oral dose) was conducted among 60 healthy Mexican men. ATV plasma levels were measured using high-performance liquid chromatography mass spectrometry. Genotyping was performed by real-time PCR with TaqMan probes. Four ATV metabolizer phenotypes were found: slow, intermediate, normal and fast. Six gene polymorphisms, SLCO1B1-rs4149056, ABCB1-rs1045642, CYP2D6-rs1135840, CYP2B6-rs3745274, NAT2-rs1208, and COMT- rs4680, had a significant effect on ATV pharmacokinetics (P < 0.05). The polymorphisms in SLCO1B1 and ABCB1 seemed to have a greater effect and were especially important for the shift from an intermediate to a normal metabolizer. This is the first study that demonstrates how the interaction of genetic variants affect metabolic phenotyping and improves understanding of how SLCO1B1 and ABCB1 variants that affect statin metabolism may partially explain the variability in drug response. Notwithstanding, the influence of other genetic and non-genetic factors is not ruled out.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVD) are the leading cause of death worldwide1 and in Mexico2. Diet, a lack of physical activity, and ageing are risk factors for CVD, but smoking, a high blood pressure and a high blood cholesterol level are at the top3. Statins are the first-choice drugs to treat hypercholesterolemia, and atorvastatin (ATV) is one of the most used statins4,5. However, interindividual variability in both ATV metabolism6,7,8 and therapeutic response9,10,11 have been reported. Three ATV metabolic phenotypes have been identified6,8,12 and non-validated massive genotyping methods identified genetic variants that seemed to impact ATV pharmacokinetics6,13.
The classification of metabolic phenotypes is challenging because of large datasets, variables at different scales, and limited knowledge on phenotyping data management14. Gene expression studies on large data sets of tissue samples15 and patients16 often apply cluster analysis, but its use is uncommon in pharmacogenomics and pharmacogenetics6,17. Cluster analysis of pharmacogenetics data could facilitate the screening for possible pharmacokinetic and metabolic profiles if the optimal number of groups and cut-off limits can be defined.
Several genes have been related to the variability in statin metabolism and response. Hepatic uptake and clearance largely depend on influx and efflux transporters such as those encoded by the genes ABCB1 and SLCO1B17,18. In biotransformation, genes encoding phase I metabolic enzymes, such as CYP3A4, CYP3A5, CYP2D6, and CYP2B6, are relevant, because they metabolize many drugs. Although it is known that CYP3A4 and CYP3A5 metabolize statins, the polymorphisms CYP3A4-rs2740574 and CYP3A5-rs776746 occurred at a low frequency in the Mexican population and no effect on ATV metabolism was detected. The contribution of CYP2D6 variants could not be tested due to a low call rate of the genotyping method. A potential effect of CYP2B6 has not been confirmed. Likewise, the effect on ATV metabolism could not be proven for variants of genes encoding phase II metabolic enzymes (NAT2 and COMT) for the same reasons6,13,19. In this study among a Mexican population, we applied a novel approach to identify and confirm ATV metabolic phenotypes and associated pharmacogenetic profiles. Hereto, we selected candidate genes involved in the metabolism and response to drugs, i.e. ABCB1, SLCO1B1 and CYP2D6, based on previous reports, frequency, and importance in the Mexican population and analyzed them under genetic models to identify or confirm their effect on the pharmacokinetics of ATV.
Results
Study population
All participants were healthy non-related male Mexicans who identified themselves as mestizos. Most (93.1%) were residents from northeastern Mexican states, namely Nuevo Leon (83.3%), Coahuila (1.6%), Tamaulipas (3.3%) and San Luis Potosi (4.9%). The volunteers had similar anthropometric data, and no significant differences in body composition. No adverse effects due to drug administration occurred6.
Mean peak plasma ATV concentration-time curves, according to phenotypes and genotypes. (a) Pharmacokinetic profiles of different metabolic phenotypes. (b) Pharmacokinetic profiles of different metabolic phenotypes with ABCB1-rs1045642 genotype C/C adjusting. For both (a,b): slow metabolizers (red), intermediate metabolizers (orange), normal metabolizers (green) and fast metabolizers (blue). (c) Pharmacokinetic profiles of ABCB1-rs1045642 genotypes: carriers of C/C genotype (blue) and carriers of C/T or T/T genotypes (orange) (d) Pharmacokinetic profiles of SLCO1B1-rs4149056 genotypes: carriers of C/C or C/T genotype (blue) and carriers of T/T genotypes (orange). Mean peak plasma concentration-time curves after single 80-mg dose of ATV. Data shown are mean ± standard error (SE) concentrations.
Pharmacokinetic analysis
Under controlled conditions, the mean ± standard deviation (SD) of adjusted pharmacokinetic parameters used for phenotyping were: maximum plasma concentration (Cmax) = 41.70 ± 21.51 ng/mL, the area under the plasma ATV concentration-time curve (AUC) from time 0 to the time of last measurement (AUC0-t) = 143.35 ± 84.64 ng/mL*h, AUC from time 0 extrapolated to infinity (AUC0-∞) = 155.84 ± 85.79 ng/mL*h, and the total drug clearance (Cl) = 0.65 ± 0.31 L/h*kg (Table 1). The coefficient of variation (CV) was greater than 50% for all parameters, except for Cl, which was 48%.
ATV metabolizer phenotypes
Cluster analysis distinguished four clusters or phenotypes that most reliably explained the observed pharmacokinetic variability (Table 1). When we applied this algorithm, the adjusted R-square for Cmax was 0.519; for AUC0-t, 0.865; for AUC0-∞, 0.866; and for Cl, 0.783 (P < 0.05). The defined phenotypes were: slow metabolizers (n = 3), intermediate metabolizers (n = 15), normal metabolizers (n = 28) and fast metabolizers (n = 14) as shown in Fig. 1a. Aforementioned pharmacokinetic parameters were significantly different (P < 0.05) among the metabolizer phenotypes, except for the Cmax values between intermediate and normal metabolizers (P = 0.09). Mean ATV pharmacokinetic parameters differed more than 10-fold between the fastest and slowest metabolizer groups (Cmax = 8.80 ng/mL, AUC0-t = 38.42 ng/mL*h, AUC0-∞ = 46.92 ng/mL*h, Cl = 1.71 L/h*kg vs. Cmax = 89.86 ng/mL, AUC0-t = 467.93 ng/mL*h, AUC0-∞ = 477.81 ng/mL*h and Cl = 0.17 L/h*kg; respectively).
Pharmacogenetic tests
The call rate for the seven gene polymorphisms was 1.0. All genetic markers were in Hardy-Weinberg Equilibrium (P > 0.05) and had a minor allele frequency > 0.01. The haplotype analysis revealed that the most frequent haplotypes were CTTT (n = 26; 43%) CCTT (n = 12; 20%) and TTTT (n = 11; 18%), result of the combination of ABCB1-rs1045642 and SLCO1B1-rs4149056 polymorphisms.
Effect of gene polymorphisms and haplotypes on atorvastatin pharmacokinetics
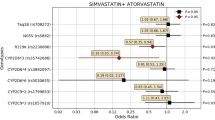
Five gene polymorphisms had a significant effect on different pharmacokinetic parameters. Cmax values were influenced by ABCB1-rs1045642 polymorphism under a dominant model. C/C carriers had a significant lower Cmax (P = 0.038) than C/T and T/T carriers (Table 2). With respect to SLCO1B1-rs4149056, C carriers (homozygous or heterozygous) had a higher AUC0-t, AUC0-∞, Cl and volume of distribution (Vd) than the homozygous T genotype (P ≤ 0.038; Table 2). Regarding the metabolizer enzyme variants, heterozygous carriers (C/G) of CYP2D6-rs1135840 had higher elimination rate constant in the terminal drug phase (Ke) values, but significantly lower half-life (T1/2) values than those with homozygous genotypes (P ≤ 0.022; Table 2). Similarly, COMT-rs4680 G/G carriers had a higher AUC0-∞, but lower Cl than A/A and A/G carriers (P ≤ 0.048; Table 2). We also found a significant effect of the CCTT haplotype (of the combination of ABCB1 and SLCO1B1 drug transporters) on Cmax, AUC0-t, AUC0-∞ and Cl parameters (P ≤ 0.040). Subjects with a CCTT genetic profile in drug transporter genes had lower Cmax, AUC0-t, and AUC0-∞, but a higher Cl than those with other combinations (Table 2). The regression analysis confirmed that three gene polymorphisms (ABCB1-rs1045642, SLCO1B1-rs4149056 and COMT-rs4680) had an impact on ATV pharmacokinetics (Table 3). The regression analysis also revealed that CYP2B6-rs3745274 and NAT2-rs1208 are involved in pharmacokinetic variability. The CYP2B6-rs3745274 polymorphisms influenced the variability of Cmax (in the over-dominant model; Table 3) and NAT2-rs1208 variants affect AUC0-∞ (under the co-dominant and dominant models; Table 3). No other polymorphisms had a significant effect on ATV pharmacokinetics.
Interaction of gene polymorphism on atorvastatin pharmacokinetics
The interaction of ABCB1-rs1045642 with CYP2B6-rs3745274, under the dominant and over-dominant model, respectively, predicted 11.1% of the Cmax variability (Table 3). Furthermore, under the co-dominant model, the interaction of SLCO1B1-rs4149056 with NAT2-rs1208 predicted 19.7% of the AUC0-∞ variation. In another approach to test gene polymorphism interactions, after a genotype adjustment of intermediate metabolizers, i.e. three subjects with a C/C genotype for ABCB1-rs1045642 were removed from the group, the normal and intermediate metabolizers became significantly different (Fig. 1b). The new mean ± SD for Cmax of intermediate metabolizers became 59.23 ± 20.12 ng/mL (cut-off 46.45–72.02 ng/mL) and the adjusted R-square increased to 0.700 (P < 0.005). In addition, CCTT carriers were only ones that were statistically different from other subjects (Table 4).
Phenotype-genotype association
When the association between phenotypes and genotypes was assessed, we found that, under the recessive model, SLCO1B1-rs4149056 is associated with fast/normal metabolizers while the presence of allele C is related to slow/intermediate metabolizers (Table 5). This association remained after Bonferroni correction and was supported by logistic regression (P = 0.002). No association was found between other haplotypes and phenotypes.
Discussion
Despite similar health conditions, body composition, and controlled experimental conditions, ATV pharmacokinetic parameters varied greatly among Mexican male individuals. We applied a novel approach (cluster analysis based on more pharmacokinetic parameters than a previous method) that distinguished four metabolizer phenotypes with higher accuracy and reliability than a previously reported classification method6. Furthermore, it allowed the selection of a model with the highest prediction percentage and best cut-off limits for each metabolizer phenotype. In addition, the analysis allowed identifying inconsistencies. For example, after phenotyping, considerable variability of Cmax values was observed in the intermediate metabolizer group, suggesting that there are important differences between individuals in the absorption process.
Although the clustering analysis method has been successfully applied for classification purposes in other areas of biomedical research14,15,16, it has been little used in pharmacokinetics, pharmacogenetics and pharmacogenomics6. A reason might be the need to realize multiple analyzes to select the ideal number of clusters. In our experience, the cluster analysis method proved to be a) effective in identifying the different groups within a population, b) useful to determine which are the groups or subgroups that require more focus, and c) practical to evaluate the absorption, distribution, metabolism and excretion (ADME) process when no metabolic data are available, as only pharmacokinetic data are required.
The classification for this Mexican population should not be extrapolated indiscriminately to other populations, because population-specific intrinsic genetic variation may shift pharmacokinetics. Thus, population-specific ATV pharmacokinetic stratification criteria should be determined. Hereto, we recommend to develop an analogous cluster analysis which can be applied retrospectively. The pharmacokinetic variability of ATV observed in our population differed from the one reported for a Bengali population20. In both studies, the volunteers were young adult males, but the dose (40 vs. 80 mg) and race (Bengali vs. Mexican genetic background) differed between the studies.
We assessed common genetic variants involved in drug metabolism to verify and confirm their influence on ATV pharmacokinetic variability. After genotyping validation, the genotype distribution of ABCB1-rs1045642 (0.23 for C/C; 0.53 for C/T and 0.23 for T/T) differed from a previously reported distribution that had been obtained with microarrays6. Importantly, the effect on Cmax values remains significant. The ABCB1 gene encodes a transporter protein that has affinity for multiple substrates, both endogenous and exogenous ones21. The polymorphism rs1045642 is located in exon 26 and produces a synonymous substitution, so the role of the ABCB1 variant in plasma drug concentrations is controversial22. Even so, rs1045642 variant may influence the folding time of the protein, alter its specificity, and therefore influence the concentration of a given drug23. In addition, synergistic or antagonistic interactions with other gene variants may create variability. So far, evidence on synergistic or antagonistic effect of ABCB1 on ATV plasma concentrations is scarce13.The significantly lower values in C/C carriers and the dominant effect of allele T suggest that the rs1045642 polymorphism significantly affects the absorption, bioavailability and blood concentrations of ATV. This hypothesis is supported by the intestinal expression of ABCB1, where this transporter actively participates in drug absorption24. These data on rs1045642 are consistent with previous findings, even for different drugs and populations. T/T carriers had a higher Cmax for ATV among Americans and for rosuvastatin among Chinese, while C/C carriers had a lower Cmax and AUC for edoxaban and also in Mexicans for amfepramone17,18,25,26. Contrasting data, however, were found in a Korean population, where T/T carriers had a lower Cmax and longer half-life than C allele carriers. The group size was small (n = 3), though27. As far as we know, there is no other report about the effect of ABCB1-rs1045642 on the pharmacokinetics of other statins28,29. Our findings suggest that a lower concentration of drug may yield a lower response, whereas an increased exposure to the medicine could cause adverse effects. Conversely, the lack of pharmacodynamic data did not allow us to evaluate the response to treatment and confirm our hypothesis. Despite this limitation, the association between ABCB1-rs1045642 and the pharmacological response to ATV has been well documented. For example, the C/C genotype among Australian patients treated with ATV associated with a lower treatment efficiency (i.e. less decrease in LDL values) as compared to other genotypes30. Similar data have been reported for Egyptian males9, Iranian31 and Polish populations32, and in a meta-analysis where 395 patients were included and treated with statins33. Regarding adverse effects, a higher frequency of the T allele has been found in patients who presented with myalgia, but no association has been reported30.
In our analysis, the genotype frequency of SLCO1B1-rs4149056 was similar to the one we have previously reported6. The new clustering analysis method confirmed the effect of SLCO1B1-rs4149056 on ATV pharmacokinetics. The SLCO1B1 gene codes for a protein responsible for the transport of organic anions and other compounds, such as drugs. This gene is expressed exclusively in the liver, where it has an important role in metabolism34. The rs4149056 polymorphism generates a p.V174A substitution that causes a decrease in expression and transport activity35. SLCO1B1-rs4149056 had the greatest effect on ATV pharmacokinetics. The presence of the C allele in SLCO1B1-rs4149056 seemed to affect AUC0-t, AUC0-∞, Cl, Vd, and therefore impact the exposure to ATV, which was consistent with its occurrence in normal/faster phenotypes. The association between SLCO1B1-rs4149056 and aforementioned pharmacokinetic parameters indicates that the variant mainly affects the metabolism and excretion phases of ATV in the Mexican population as opposed to ABCB1-rs1045642, which apparently affects the absorption phase. This assumption is consistent with ATV pharmacokinetics in Chinese (n = 32), Japanese (n = 31), Caucasian (n = 30), and Korean (n = 28) populations where the presence of the C allele of polymorphism rs4149056 was associated with higher Cmax and/or AUC values7,27,36. In our study, rs4149056 has a preponderant role on ATV metabolism, since it was the only one that showed an association with metabolic phenotypes. Again, the higher AUC and slower clearance in C allele carriers could result in a better response or a higher susceptibility to adverse effects. The latter, may be explained by the statin response studies, where the C allele has been related to the risk of myopathy37,38. In all studies, the C/C genotype was the least frequent.
CYP2D6 codes for one of the main drug metabolizing enzymes, since it participates in the biotransformation of around 25% of all drugs39. The CYP2D6-rs1135840 polymorphism creates an alternative splicing site that eliminates exon 6, without a significant impact on gene expression40. Another CYP2D6 polymorphism, CYP2D6-rs3892097, has been associated with ATV-induced adverse effects on muscle41. However, there is little information about the role of CYP2D6 in ATV metabolism or pharmacokinetics. In a previous study, CYP2D6-rs1135840 seemed to have a significant effect on AUC values13, but this finding was not confirmed in this study. Here, we identified that CYP2D6-rs1135840 has a significant effect on Ke and T1/2 parameters, but this was not confirmed with the regression analyses, so its effect on the metabolism and excretion phases is not clear.
The catechol-O-methyltransferase, encoded by the COMT gene, is an enzyme that helps to eliminate endogenous or toxic metabolites, as well as exogenous polycyclic compounds42,43. Due to its regulatory function of catecholamines, more is known about its role in pharmacodynamics than its role in pharmacokinetics44. The A allele related to susceptibility to coronary artery disease44. We discovered a significant effect of the COMT-rs4680 polymorphism on the Cmax, AUC0-∞ and Cl of ATV, although this effect was not supported by regression analysis. The rs4680 variant produces a non-synonymous amino acid change (p.V158M) causing impaired COMT activity44,45. As far as we know this is the first study that reports a possible effect of COMT-rs4680 on ATV pharmacokinetics.
CYP2B6 is a P450 family pharmacogene responsible for the metabolism of 4% of the main drugs19,46. The CYP2B6 gene is expressed primarily in the liver19,47 and its expression can be induced by different substrates including ATV48. The rs3745274 is located in exon 4 and produces a p.Q172H substitution, which is related with a slight reduction in expression and activity19. The T allele variant of rs3745274 has been related to a lower propofol dose49 and an increased exposure to efavirenz50. Although ATV induced CYP2B6 expression in cultured human hepatocytes51, the role of CYP2B6 on ATV pharmacokinetics in vivo is unknown. Our results show that, under an over-dominant model, rs3745274 affects the variation of Cmax, suggesting a slight role in ATV absorption of an unknown mechanism.
The N-acetyltransferase 2 gene (NAT2) encodes a phase II metabolic enzyme involved in the biotransformation of drugs and carcinogens. NAT2 has many variations and has been associated with different metabolic phenotypes52, especially for anti-tuberculosis drugs53. The NAT2-rs1208 produces a p.K268R substitution that associates with a rapid acetylation52. To date, the influence of NAT2-rs1208 on statin pharmacokinetics has not been reported. We found that NAT2-rs1208 affected AUC0-∞ under co-dominant and dominant models.
Although the effect of ABCB1 and SLCO1B1 transporters on pharmacokinetics and pharmacodynamics, as well as on susceptibility to adverse effects has been well documented, there are few studies that assess the interaction of these genes and their relationship with the effectiveness of treatment. Pharmacogenetics data from 1844 subjects suggest that ABCB1 and SLCO1B1 variants may be useful for improving effectiveness and preventing the risks of adverse effects of statin treatment10. Our data on a Mexican population confirm that the transporters ABCB1 and SLCO1B1 have a significant impact on ATV metabolism (Fig. 1c,d). Although the SLCO1B1 transporter had the greatest impact on ATV metabolism, the influence of ABCB1 is underscored by the fact that the presence of the ABCB1-rs1045642 C/C variant is sufficient to shift from an intermediate to a normal metabolism phenotype. Thus, different combinations of these two variants may generate a broad spectrum of metabolism and therefore a variable response to treatment. In our knowledge, this is the first study that demonstrates how the interaction of genetic variants affect metabolic phenotyping and improves understanding of how SLCO1B1 and ABCB1 variants that affect statin metabolism may explain the variability in drug response.
In the present study, some limitations remain. First, as only men were included in this study, our findings should be confirmed in women. Second, the lack of data on secondary metabolites of ATV did not allow us to validate the metabolic classification by another method. Third, this study was limited to candidate polymorphisms. Thus, other polymorphisms or genes that could have an impact on the metabolism of ATV were not investigated.
Conclusions
Variants of the transporter-encoding genes ABCB1 and SLCO1B1 have an important impact on ATV pharmacokinetics in a Mexican male population. Hence, the metabolism also varies from population to population, even for the same drug. So, it is important that each study perform its metabolic classification. Our results improve the understanding of the mechanism by which variation in transporters may affect the therapeutic response to ATV in a Mexican population. ABCB1 and SLCO1B1 variants were not only congruent with, but could also explain, the metabolic phenotype classification at a genetic level.
Material and methods
Design
This pharmacogenetic study used pharmacokinetic data from a controlled, randomized, crossover, single-blind, three-treatment, three-period, and six-sequence clinical study after a single 80-mg oral dose of ATV (tablets; Pfizer Pharmaceuticals LLC, Caguas Site, Caguas, PR), conducted in 60 healthy Mexican men. The clinical protocol complied with national and international ethical regulations, guidelines and norms, as described previously6, and was performed under medical supervision. The clinical protocol was approved by the Research and Ethics Committee of the Clinical and Experimental Pharmacology Center, Ipharma S. A. (Monterrey, NL, MEX), and registered at the Federal Commission for Protection Against Health Risks (COFEPRIS code: Atorvastatina/A95-10Bis) and the Australian New Zealand Clinical Trials Registry (ACTRN12614000851662, registration date: 08/08/2014). The pharmacogenetic procedure was approved by the Ethics, Research and Biosecurity Committees of the University of Monterrey (San Pedro Garza Garcia, NL, MEX; registry number 042014-CIE). Volunteers provided a written informed consent.
Study population
Between January and February 2011, sixty healthy, 18-to-45-year-old, non-smoking, Mexican males with a weight ≥ 50 kg and a body mass index between 20 and 26 kg/m2 participated in the bioequivalence study. Their health status was assessed based on physical examination, medical history, and clinical and biochemical tests. Exclusion criteria included abnormal laboratory results, drug abuse, ingestion of alcohol 1 week prior to the study, the use of medication three weeks before enrollment, and participation in a clinical research study within the previous 3 months.
Dosing regimen and sampling
The dosing and sampling involved a three-treatment (R = reference drug, T1 = Test 1 and T2 = Test 2 drugs are first and second treatment, respectively), three-period, and six-sequence schedule with a 2-week washout period between treatments. Before starting any drug administration, the statistical department of Ipharma S.A. randomized drug allocation (R, T1 or T2, file code, and subject code) with a balanced design using the Mersenne Twister algorithm and R statistical software. The participants were blinded to treatment. About 18 h before the first dose administration, the subjects were admitted to the clinical site and served a standard dinner (<800 kcal). The next morning, after an overnight fast, ATV was administered orally as a single 80-mg dose tablet (Pfizer, New York, NY, USA) with 240 mL of water. A standardized lunch was served 4 h after dosing and standardized dinner at 12 h after dosing. Peripheral blood (4-mL samples) was collected in K2EDTA-coated Vacutainers (BD Diagnostics, Franklin Lakes, NJ, USA), a pre-dose sample was taken (time 0), while other samples were taken at 0.25, 0.5, 0.75, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 12, 24, 36 and 48 h after drug administration. Cells and plasma were separated (10 min at 1600 × g at 4 °C). Plasma was stored at −65 ± 15 °C until use while DNA was extracted from cells.
Plasma ATV quantitation
Proteins were eliminated by acetonitrile precipitation. Briefly, 400 µL acetonitrile was added to a 100-µL plasma sample, vortexed (70 rpm, 4 min), and centrifuged (9600 × g, 10 min, 10 °C). The supernatant (300 µL) was injected into a high-performance liquid chromatography-tandem mass spectrometry equipped with an Agilent 1100 control system (Agilent Technologies, Inc., Santa Clara, CA, USA) using a method validated by Ipharma S.A6. that respects Mexican regulations54 and guidelines for the validation of bioanalytical methods of the European Medicines Agency (EMA)55. An electrospray ionization tandem mass spectrometry system with a precursor ion (+) 559.3 m/z and a product ion (+) 440.3 m/z was used for detection. The linearity of the analytical method was assessed with calibration curves (0.5, 2.5, 5, 10, 25, 50 and 100 ng/mL), which yielded a correlation coefficient (r) = 0.99292 and a lower limit of quantification (LLOQ) = 0.5 ng/mL of ATV in plasma. Precision was assessed with control samples (1.7, 7.5, 35, and 75 ng/mL) and was considered within an acceptable range: intraday CV < 5% and interday CV < 8%. An accuracy error ≤7% was considered to be acceptable. The recovery was 87% and no effects were detected for the matrix, hemolyzed, and lipemic plasma (CV < 4%).
Pharmacokinetic analysis
The Cmax and time to reach Cmax (Tmax) were obtained from the concentration-time data. The pharmacokinetics parameters were determined by non-compartmental methods. The AUC0-t and AUC0-∞ were calculated with the log-linear trapezoidal rule. The Ke was estimated via log-linear regression from the terminal portion of the log-transformed concentration-time plots. T1/2 was estimated by dividing 0.693 by Ke. The Cl was calculated by dividing the dose by AUC0-∞ and adjusting for weight. The Vd was calculated as Cl divided by Ke. The AUC’s and Cmax values were adjusted for dose and weight (AUC’s/dW and Cmax/dW)17,56. The pharmacokinetic analysis was performed using WinNonlin software v5.3 (Pharsight Corp., Mountain View, CA, USA).
Determination of ATV metabolizer phenotypes
To estimate the ideal number of phenotypes, we applied a modified four-step multivariate analysis of the combined dose-and-weight-adjusted pharmacokinetic parameters Cmax, AUC0-t, AUC0-∞ and Cl6,14,16,57. First, hierarchical cluster analysis (HCA) was performed with the Ward linkage method and the distance matrix was calculated with the Manhattan measure. These analyses were applied to z-score transformed pharmacokinetic values to circumvent the comparability problems caused by the different scales of the non-transformed pharmacokinetic values. Aforementioned analysis were carried out with Minitab 16 software (Minitab Inc., State College, PA, USA). Second, we identified the subjects in each cluster, calculated the means of the adjusted pharmacokinetic parameters, and assigned the clusters to metabolizer phenotypes based on the means of the pharmacokinetic parameters. Third, we validated the phenotyping model by automatic linear modeling with the forward stepwise method, the Akaike Information Criterion (AICC) and the Overfit Prevention Criterion (ASE); followed by linear and logistic regression analysis. Finally, the cut-off limits were assessed by one-way analysis of variance and the Kruskal-Wallis test, considering P < 0.05 to be statistically significant different, with SPSS for Windows V.25 (IBM Corp., NY, USA).
Genotyping tests
Genomic DNA that had been isolated with the alkaline lysis method58 was quantified by fluorometry using the Qubit dsDNA BR assay kit and a Qubit 3.0 fluorometer (Invitrogen; Thermo Fisher Scientific, Waltham, MA, USA). Compliance with DNA purity (OD260/OD280 between 1.8 and 2) was assessed with a Nanodrop 1000 spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA). DNA was stored at 10 ng/µL at −20 °C until analysis.
The polymorphisms ABCB1-rs1045642, SLCO1B1-rs4149056, CYP2B6-rs3745274, CYP2D6-rs16947, CYP2D6-rs1135840, NAT2-rs1208 and COMT-rs4680 were genotyped using a QuantStudio 1 real-time PCR system and TaqMan genotyping assays (Applied Biosystems; Thermo Fisher Scientific, Wilmington, MA, USA) according to the manufacturer’s protocol. Briefly, the PCR was prepared with 1X TaqMan Universal PCR Master Mix (Thermo Fisher Scientific, Inc.), 1X TaqMan genotyping assay mix, 10 ng DNA, and nuclease-free water to a total volume of 10 µl. Thermal cycling conditions were as follows: 95 °C for 10 min, 40 cycles of 95 °C for 15 sec and 60 °C for 1 min. Quality controls included a genotyping control using previously genotyped samples across different platforms, genotype call rate equal to 1.0, a Hardy-Weinberg equilibrium test with P > 0.05, and a minor allele frequency> 0.01. To detect the combination of the most important variants in the study population, a haplotype analysis was performed using the Haplotype Analysis Software V.1.0559, under a modified data entry method for diploid genomes.
Statistical analysis
The sample size calculation considered an intrasubject coefficient of variation (CV) of 45% for Cmax and AUC, a confidence interval (CI) of 90%, a significance level of 5%, a minimum power of 80%, and a Ω of 0.25. Thus, a sample size of 58 would suffice. The Hardy-Weinberg equilibrium was determined by comparing the genotype frequencies with the expected values using the maximum likelihood method60. To assess the effects of polymorphisms on the ATV pharmacokinetic parameters, comparisons between two and three groups were made. The Student’s t-test and one-way analysis of variance were used for parametric distributions, while Mann-Whitney U and Kruskal-Wallis H tests were used for nonparametric distributions. Post hoc tests (Bonferroni’s and Tamhane’s T2) were used for pairwise comparisons. To confirm the contribution of genetic factors to the variability of pharmacokinetic parameters, automatic linear modeling with the forward stepwise method, AICC and ASE was performed, as well as linear regression analysis with various modes (default mode, stepwise, remove, backward and forward). Possible associations of genotypes or combinations of genotypes with phenotypes were evaluated using X2 and Fisher’s exact tests and validated by logistic regression analysis. The evaluation effect of polymorphisms and associations were assessed under four different models (co-dominant, dominant, over-dominant and recessive). The odds ratio (OR) was estimated with a 95% CI. All P values were two-tailed. Corrected P values (Pc) were obtained using the Bonferroni correction for exclusion of spurious associations. P < 0.05 was interpreted as statistically significant. The statistical analyses were performed with SPSS for Windows, V.25 (IBM Corp., NY, USA).
Data availability
All data generated and analyzed during this study are included in this published article, but if necessary, some additional information is available from the corresponding author on reasonable request.
References
World Health Organization. Noncommunicable diseases, https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (2018).
National Institute of Statistics and Geography (INEGI). Mortality, https://www.inegi.org.mx/programas/mortalidad/ (2018).
Catapano, A. L. et al. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. European heart journal 37, 2999–3058, https://doi.org/10.1093/eurheartj/ehw272 (2016).
U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health & National Heart, L., and Blood Institute,. (ed. U.S. Department of Health and Human Services) 6 (National Institutes of Health, USA, 2005).
Jackevicius, C. A. et al. Comparative Effectiveness of Generic Atorvastatin and Lipitor(R) in Patients Hospitalized with an Acute Coronary Syndrome. Journal of the American Heart Association 5, e003350, https://doi.org/10.1161/JAHA.116.003350 (2016).
Leon-Cachon, R. B. R. et al. A pharmacogenetic pilot study reveals MTHFR, DRD3, and MDR1 polymorphisms as biomarker candidates for slow atorvastatin metabolizers. BMC cancer 16, 74, https://doi.org/10.1186/s12885-016-2062-2 (2016).
Woo, H. I., Kim, S. R., Huh, W., Ko, J. W. & Lee, S. Y. Association of genetic variations with pharmacokinetics and lipid-lowering response to atorvastatin in healthy Korean subjects. Drug design, development and therapy 11, 1135–1146, https://doi.org/10.2147/DDDT.S131487 (2017).
Huang, Q. et al. A Pharmacometabonomic Approach To Predicting Metabolic Phenotypes and Pharmacokinetic Parameters of Atorvastatin in Healthy Volunteers. Journal of proteome research 14, 3970–3981, https://doi.org/10.1021/acs.jproteome.5b00440 (2015).
Shabana, M. F., Mishriki, A. A., Issac, M. S. & Bakhoum, S. W. Do MDR1 and SLCO1B1 polymorphisms influence the therapeutic response to atorvastatin? A study on a cohort of Egyptian patients with hypercholesterolemia. Molecular diagnosis & therapy 17, 299–309, https://doi.org/10.1007/s40291-013-0038-3 (2013).
Peters, B. J. et al. Pharmacogenetic interactions between ABCB1 and SLCO1B1 tagging SNPs and the effectiveness of statins in the prevention of myocardial infarction. Pharmacogenomics 11, 1065–1076, https://doi.org/10.2217/pgs.10.81 (2010).
Xiang, Q. et al. Association between SLCO1B1 T521C polymorphism and risk of statin-induced myopathy: a meta-analysis. The pharmacogenomics journal 18, 721–729, https://doi.org/10.1038/s41397-018-0054-0 (2018).
Herrera-Gonzalez, S. et al. Effect of AGTR1 and BDKRB2 gene polymorphisms on atorvastatin metabolism in a Mexican population. Biomedical reports 7, 579–584, https://doi.org/10.3892/br.2017.1009 (2017).
Cruz-Correa, O. F., Leon-Cachon, R. B., Barrera-Saldana, H. A. & Soberon, X. Prediction of atorvastatin plasmatic concentrations in healthy volunteers using integrated pharmacogenetics sequencing. Pharmacogenomics 18, 121–131, https://doi.org/10.2217/pgs-2016-0072 (2017).
Hu, C. W., Kornblau, S. M., Slater, J. H. & Qutub, A. A. Progeny Clustering: A Method to Identify Biological Phenotypes. Scientific reports 5, 12894, https://doi.org/10.1038/srep12894 (2015).
Pirim, H., Eksioglu, B., Perkins, A. & Yuceer, C. Clustering of High Throughput Gene Expression Data. Computers & operations research 39, 3046–3061, https://doi.org/10.1016/j.cor.2012.03.008 (2012).
Green, M. A. et al. Who are the obese? A cluster analysis exploring subgroups of the obese. Journal of public health 38, 258–264, https://doi.org/10.1093/pubmed/fdv040 (2016).
Gomez-Silva, M. et al. Pharmacogenetics of amfepramone in healthy Mexican subjects reveals potential markers for tailoring pharmacotherapy of obesity: results of a randomised trial. Scientific reports 9, 17833, https://doi.org/10.1038/s41598-019-54436-z (2019).
Aquilante, C. L., Wempe, M. F., Sidhom, M. S., Kosmiski, L. A. & Predhomme, J. A. Effect of ABCB1 polymorphisms and atorvastatin on sitagliptin pharmacokinetics in healthy volunteers. European journal of clinical pharmacology 69, 1401–1409, https://doi.org/10.1007/s00228-013-1475-y (2013).
Zanger, U. M. & Klein, K. Pharmacogenetics of cytochrome P450 2B6 (CYP2B6): advances on polymorphisms, mechanisms, and clinical relevance. Frontiers in genetics 4, 24, https://doi.org/10.3389/fgene.2013.00024 (2013).
Khan S. I. et al. Bioequivalence studies and pharmacokinetic properties of atorvastatin 40mg tablet in healthy bengali subjects. MOJ Bioequiv Availab 4, 241–246, doi: 10.15406/mojbb.2017.04.00064 (2017).
Wolking, S., Schaeffeler, E., Lerche, H., Schwab, M. & Nies, A. T. Impact of Genetic Polymorphisms of ABCB1 (MDR1, P-Glycoprotein) on Drug Disposition and Potential Clinical Implications: Update of the Literature. Clinical pharmacokinetics 54, 709–735, https://doi.org/10.1007/s40262-015-0267-1 (2015).
Kajinami, K., Brousseau, M. E., Ordovas, J. M. & Schaefer, E. J. Polymorphisms in the multidrug resistance-1 (MDR1) gene influence the response to atorvastatin treatment in a gender-specific manner. The American journal of cardiology 93, 1046–1050, https://doi.org/10.1016/j.amjcard.2004.01.014 (2004).
Kimchi-Sarfaty, C. et al. A “silent” polymorphism in the MDR1 gene changes substrate specificity. Science 315, 525–528, https://doi.org/10.1126/science.1135308 (2007).
Brinkmann, U. & Eichelbaum, M. Polymorphisms in the ABC drug transporter gene MDR1. The pharmacogenomics journal 1, 59–64 (2001).
Zhou, Q., Ruan, Z. R., Yuan, H., Xu, D. H. & Zeng, S. ABCB1 gene polymorphisms, ABCB1 haplotypes and ABCG2 c.421c> A are determinants of inter-subject variability in rosuvastatin pharmacokinetics. Die Pharmazie 68, 129–134 (2013).
Vandell, A. G. et al. An integrated pharmacokinetic/pharmacogenomic analysis of ABCB1 and SLCO1B1 polymorphisms on edoxaban exposure. The pharmacogenomics journal 18, 153–159, https://doi.org/10.1038/tpj.2016.82 (2018).
Lee, Y. J., Lee, M. G., Lim, L. A., Jang, S. B. & Chung, J. Y. Effects of SLCO1B1 and ABCB1 genotypes on the pharmacokinetics of atorvastatin and 2-hydroxyatorvastatin in healthy Korean subjects. International journal of clinical pharmacology and therapeutics 48, 36–45, https://doi.org/10.5414/cpp48036 (2010).
Jiang, F. et al. The influences of SLCO1B1 and ABCB1 genotypes on the pharmacokinetics of simvastatin, in relation to CYP3A4 inhibition. Pharmacogenomics 18, 459–469, https://doi.org/10.2217/pgs-2016-0199 (2017).
Keskitalo, J. E. et al. No significant effect of ABCB1 haplotypes on the pharmacokinetics of fluvastatin, pravastatin, lovastatin, and rosuvastatin. British journal of clinical pharmacology 68, 207–213, https://doi.org/10.1111/j.1365-2125.2009.03440.x (2009).
Hoenig, M. R., Walker, P. J., Gurnsey, C., Beadle, K. & Johnson, L. The C3435T polymorphism in ABCB1 influences atorvastatin efficacy and muscle symptoms in a high-risk vascular cohort. Journal of clinical lipidology 5, 91–96, https://doi.org/10.1016/j.jacl.2011.01.001 (2011).
Behdad, N., Kojuri, J., Azarpira, N., Masoomi, A. & Namazi, S. Association of ABCB1 (C3435T) and ABCC1 (G2012T) Polymorphisms with Clinical Response to Atorvastatin in Iranian Patients with Primary Hyperlipidemia. Iranian biomedical journal 21, 120–125, https://doi.org/10.18869/acadpub.ibj.21.2.120 (2017).
Salacka, A. et al. Possible association of ABCB1:c.3435T>C polymorphism with high-density-lipoprotein-cholesterol response to statin treatment–a pilot study. Bosnian journal of basic medical sciences 14, 144–149, https://doi.org/10.17305/bjbms.2014.3.43 (2014).
Su, J. et al. ABCB1 C3435T polymorphism and the lipid-lowering response in hypercholesterolemic patients on statins: a meta-analysis. Lipids in health and disease 14, 122, https://doi.org/10.1186/s12944-015-0114-2 (2015).
Romaine, S. P., Bailey, K. M., Hall, A. S. & Balmforth, A. J. The influence of SLCO1B1 (OATP1B1) gene polymorphisms on response to statin therapy. The pharmacogenomics journal 10, 1–11, https://doi.org/10.1038/tpj.2009.54 (2010).
Brunham, L. R. et al. Differential effect of the rs4149056 variant in SLCO1B1 on myopathy associated with simvastatin and atorvastatin. The pharmacogenomics journal 12, 233–237, https://doi.org/10.1038/tpj.2010.92 (2012).
Birmingham, B. K. et al. Impact of ABCG2 and SLCO1B1 polymorphisms on pharmacokinetics of rosuvastatin, atorvastatin and simvastatin acid in Caucasian and Asian subjects: a class effect? European journal of clinical pharmacology 71, 341–355, https://doi.org/10.1007/s00228-014-1801-z (2015).
Bai, X. et al. Effects of SLCO1B1 and GATM gene variants on rosuvastatin-induced myopathy are unrelated to high plasma exposure of rosuvastatin and its metabolites. Acta pharmacologica Sinica 40, 492–499, https://doi.org/10.1038/s41401-018-0013-y (2019).
Hou, Q. et al. Association Between SLCO1B1 Gene T521C Polymorphism and Statin-Related Myopathy Risk: A Meta-Analysis of Case-Control Studies. Medicine 94, e1268, https://doi.org/10.1097/MD.0000000000001268 (2015).
Gaedigk, A., Sangkuhl, K., Whirl-Carrillo, M., Klein, T. & Leeder, J. S. Prediction of CYP2D6 phenotype from genotype across world populations. Genetics in medicine: official journal of the American College of Medical Genetics 19, 69–76, https://doi.org/10.1038/gim.2016.80 (2017).
Wang, D. et al. Common CYP2D6 polymorphisms affecting alternative splicing and transcription: long-range haplotypes with two regulatory variants modulate CYP2D6 activity. Human molecular genetics 23, 268–278, https://doi.org/10.1093/hmg/ddt417 (2014).
Frudakis, T. N. et al. CYP2D6*4 polymorphism is associated with statin-induced muscle effects. Pharmacogenetics and genomics 17, 695–707, https://doi.org/10.1097/FPC.0b013e328012d0a9 (2007).
Zhang, L. et al. Detoxication of structurally diverse polycyclic aromatic hydrocarbon (PAH) o-quinones by human recombinant catechol-O-methyltransferase (COMT) via O-methylation of PAH catechols. The Journal of biological chemistry 286, 25644–25654, https://doi.org/10.1074/jbc.M111.240739 (2011).
Shield, A. J., Thomae, B. A., Eckloff, B. W., Wieben, E. D. & Weinshilboum, R. M. Human catechol O-methyltransferase genetic variation: gene resequencing and functional characterization of variant allozymes. Molecular psychiatry 9, 151–160, https://doi.org/10.1038/sj.mp.4001386 (2004).
Mir, R. et al. Potential Impact of COMT-rs4680 G> A Gene Polymorphism in Coronary Artery Disease. Journal of cardiovascular development and disease 5, https://doi.org/10.3390/jcdd5030038 (2018).
Lin, C. H. et al. Depression and Catechol-O-methyltransferase (COMT) genetic variants are associated with pain in Parkinson’s disease. Scientific reports 7, 6306, https://doi.org/10.1038/s41598-017-06782-z (2017).
Zanger, U. M., Turpeinen, M., Klein, K. & Schwab, M. Functional pharmacogenetics/genomics of human cytochromes P450 involved in drug biotransformation. Analytical and bioanalytical chemistry 392, 1093–1108, https://doi.org/10.1007/s00216-008-2291-6 (2008).
Wang, H. & Tompkins, L. M. CYP2B6: new insights into a historically overlooked cytochrome P450 isozyme. Current drug metabolism 9, 598–610 (2008).
Kocarek, T. A., Dahn, M. S., Cai, H., Strom, S. C. & Mercer-Haines, N. A. Regulation of CYP2B6 and CYP3A expression by hydroxymethylglutaryl coenzyme A inhibitors in primary cultured human hepatocytes. Drug metabolism and disposition: the biological fate of chemicals 30, 1400–1405, https://doi.org/10.1124/dmd.30.12.1400 (2002).
Mourao, A. L., de Abreu, F. G. & Fiegenbaum, M. Impact of the Cytochrome P450 2B6 (CYP2B6) Gene Polymorphism c.516G>T (rs3745274) on Propofol Dose Variability. European journal of drug metabolism and pharmacokinetics 41, 511–515, https://doi.org/10.1007/s13318-015-0289-y (2016).
Rohrich, C. R. et al. CYP2B6*6 and CYP2B6*18 Predict Long-Term Efavirenz Exposure Measured in Hair Samples in HIV-Positive South African Women. AIDS research and human retroviruses 32, 529–538, https://doi.org/10.1089/AID.2015.0048 (2016).
Korhonova, M., Doricakova, A. & Dvorak, Z. Optical Isomers of Atorvastatin, Rosuvastatin and Fluvastatin Enantiospecifically Activate Pregnane X Receptor PXR and Induce CYP2A6, CYP2B6 and CYP3A4 in Human Hepatocytes. PloS one 10, e0137720, https://doi.org/10.1371/journal.pone.0137720 (2015).
McDonagh, E. M. et al. PharmGKB summary: very important pharmacogene information for N-acetyltransferase 2. Pharmacogenetics and genomics 24, 409–425, https://doi.org/10.1097/FPC.0000000000000062 (2014).
Yuliwulandari, R. et al. NAT2 variants are associated with drug-induced liver injury caused by anti-tuberculosis drugs in Indonesian patients with tuberculosis. Journal of human genetics 61, 533–537, https://doi.org/10.1038/jhg.2016.10 (2016).
Secretaría de Salud & Comisión Federal para la Protección Contra Riesgos Sanitarios. (Secretaría de Gobernación, México, DF, 1998).
European Medicines Agency. Science Medicines Health. (European Medicines Agency, London, UK, 2011).
Saiz-Rodriguez, M. et al. Effect of Polymorphisms on the Pharmacokinetics, Pharmacodynamics and Safety of Sertraline in Healthy Volunteers. Basic & clinical pharmacology & toxicology 122, 501–511, https://doi.org/10.1111/bcpt.12938 (2018).
Lindon, J. C. & Nicholson, J. K. The emergent role of metabolic phenotyping in dynamic patient stratification. Expert opinion on drug metabolism & toxicology 10, 915–919, https://doi.org/10.1517/17425255.2014.922954 (2014).
Sambrook J & Russell D W. In Molecular cloning: a laboratory manual (ed Cold Spring Harbor) (Cold Spring Harbor Laboratory Press, 2001).
Eliades N-G. & Eliades D.G. HAPLOTYPE ANALYSIS: Software for analysis of haplotype data, https://www.uni-goettingen.de/en/134935.html (2009).
Reed, T. E. & Schull, W. J. A general maximum likelihood estimation program. American journal of human genetics 20, 579–580 (1968).
Acknowledgements
The authors would like to thank QBP Marcelino Aguirre Garza from the University of Monterrey and the technical staff of Ipharma, S.A. for facilities, advice and technical support. Pharmacogenetic study by University of Monterrey, UIN20508.
Author information
Authors and Affiliations
Contributions
R.B.R.L.C. designed research and conception. R.B.R.L.C. collected samples and acquired clinical data of volunteers. M.G.S., conducted analytical determination A.D.B. and M.F.G.B. performed genetic studies of the study subjects. R.B.R.L.C. carried out the pharmacokinetic analysis data. R.B.R.L.C., I.M., H.A.B.S. and A.D.B. data interpretation. R.B.R.L.C., A.D.B., I.M. and H.A.B.S. wrote and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
León-Cachón, R.B.R., Bamford, AD., Meester, I. et al. The atorvastatin metabolic phenotype shift is influenced by interaction of drug-transporter polymorphisms in Mexican population: results of a randomized trial. Sci Rep 10, 8900 (2020). https://doi.org/10.1038/s41598-020-65843-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65843-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.