Abstract
Abdominal pain is a common reason for medical visits. We examined the prevalence, gastrointestinal, and emotional significance of abdominal pain in a population-based cohort serially followed up from birth to 17 years. Children and adolescents from Generation 2 of the Raine Study participated in comprehensive cross-sectional assessments at ages 2, 5, 8, 10, 14 and 17 years. At 17 years, medical history, general health, gastrointestinal symptoms, medications, health practitioner attendance, and self-rated unhappiness were recorded. Longitudinal data regarding abdominal pain or unhappiness, from serial questionnaires, were analysed to identify factors associated with abdominal pain and adverse emotional health at age 17 years. Females experienced more abdominal pain than males at all ages (p < 0.05). Seventeen-year-old adolescents with abdominal pain reported a higher prevalence of depression, anxiety, being bullied at school, and poorer health status than those without abdominal pain (p < 0.05 for all). Abdominal pain and unhappiness during childhood and mid-adolescence were prospectively associated with recurrent abdominal pain, anxiety, depression and unhappiness during late adolescence (p < 0.05 for all). In conclusion, abdominal pain in children and adolescents associates with depression, anxiety, being bullied, unhappiness and reduced overall health-rating during adolescence. Awareness of these factors may guide management decisions.
Similar content being viewed by others
Introduction
Abdominal pain is one of the most common reasons for primary care, hospital outpatients or emergency department visits, hospitalisations, referrals to gastroenterologists and for imaging tests1,2,3,4,5,6,7. In 2016/2017, abdominal and pelvic pain was the most common principal diagnosis for emergency department presentations and hospitalisations in Australia, accounting for 4.3% of principal diagnoses8. Likewise, in the USA in 2014/2015, abdominal pain was the most frequent reason for gastrointestinal-related ambulatory medical visits to primary care and emergency departments, with an expenditure of US$10.2 billion2. In Australia, abdominal pain accounted for 2.1 per 100 patient primary care visits, and the aetiology was not confirmed in one third of males and half of females9. Only one third of patients were prescribed medications, primarily paracetamol or hyoscine butylbromide for the pain, while counselling was the most common non-pharmacological treatment. This suggests a suspected diagnosis of a functional abdominal pain disorder10. Rome IV diagnostic criteria for functional gastrointestinal disorders describe four main categories of functional abdominal pain disorders in children and adolescents. These comprise functional dyspepsia, irritable bowel syndrome, abdominal migraine and functional abdominal pain - not otherwise specified, which can coexist with each other and with other medical conditions associating with gastrointestinal symptoms in the same individual11.
Amongst Australian adolescents, females present to general practitioners with abdominal pain more frequently than males9,12. In adolescents in the Raine Study we recently described sex-specific patterns of gastrointestinal symptoms that were associated with diet, emotional health, health practitioner attendance, and adverse everyday wellbeing13. Also, in a large German survey 36% of children and 29% of adolescents reported recurrent abdominal pain over a 3-month period, with a higher prevalence in girls14. An association between childhood depressive symptoms and subsequent functional abdominal pain during adolescence has been described in a longitudinal study in the USA15. Chronic abdominal pain in adolescents is commonly associated with other somatic pain, interference with education, employment and quality of life16, and adversely affects mental health17. Consequently, abdominal pain present or persisting during adolescence risks progressing into chronic abdominal pain that adversely affects various facets of life, including relationships, enjoyment of food, and social and workforce participation during adulthood. Chronic abdominal pain may result in attendance with various health practitioners to address abdominal pain, other somatic pain, depression or anxiety, dietary interventions, or self-medication with prescription, over the counter medications or other substances. Consequently, chronic or persisting abdominal pain in adolescents may be negatively associated with physical and emotional wellbeing and is deserving of attention.
Aims
The aims of the current study were to describe (a) patterns of abdominal pain and the relationship between abdominal pain, other gastrointestinal symptoms and medication use in adolescents, (b) the prospective relationship between abdominal pain and unhappiness experienced during childhood and adolescence, and abdominal pain, depression, anxiety or unhappiness during late adolescence, and (c) to identify risk factors for frequent abdominal pain in a cohort of population-based adolescents.
Methods
This is an observational study examining gastrointestinal and emotional health correlates of abdominal pain in children and adolescents participating in the Raine Study.
The Raine Study
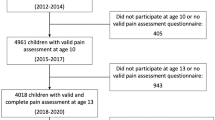
The Raine Study is a predominantly-Caucasian cohort study established between 1989–1991 as a randomised controlled trial evaluating the effects of repeated antenatal ultrasound on the course of pregnancy and pregnancy outcomes18. At the outset, the study involved serial assessments of 2868 women (Generation 1 or Gen1) at approximately 18 weeks into pregnancy. The offspring (Generation 2 or Gen2) have been prospectively followed from birth into adulthood19. References to children and adolescents in the analyses in this study relate to Gen2 Raine Study participants. Institutional ethics committee approval was obtained from the Princess Margaret Hospital for Children Human Research Ethics Committee. Signed informed consent from parents or legal guardians was obtained for each child and adolescent assessment, and adolescent assent at age 17 years was obtained. All research was performed in accordance with the approved guidelines.
Longitudinal assessments
During serial Raine Study follow up assessments at ages 2, 8 and 10 years the parent recorded the presence of abdominal pain related to bowel motions, while at age 17 years the Gen 2 adolescent reported the presence of abdominal pain. Abdominal pain was reported: (a) by frequency at ages 2, 8, 10 and 17 years, (b) as being present or absent with bowel motions at ages 2 and 10 years, and (c) severe enough to interfere with usual activities on at least three episodes during the preceding three months in eight-year-olds. Characteristics of the abdominal pain and associated gastrointestinal symptoms in children were described by the parent at different ages and by the adolescent at age 17 years. The primary care physician diagnosis for the abdominal pain was reported at age 10 years. Questionnaire data regarding abdominal pain was available for 1896, 2108, 2021 and 1281 children or adolescents who participated in the 2, 8, 10 or 17-year cross-sectional assessments, respectively, of the Raine Study. Whether the child or adolescent felt generally unhappy or sad or not was documented on an ordinal scale from ‘not true’ to ‘sometimes true’ to ‘often true’ by the parent for children aged 2–10 years, and subsequently by the adolescent during follow up at ages 14 and 17 years.
Seventeen-year cross-sectional assessment
Seventeen-year-old Gen2 adolescents in the Raine Study participated in a cross-sectional assessment that involved physical assessments and detailed self-administered questionnaires regarding health and lifestyle. Questions included medical history, incorporating gastrointestinal symptoms, diagnoses, health professional attendance and medications used. The questions asked about the presence and frequency of abdominal pain (excluding menstrual period pain) and associated gastrointestinal symptoms during the preceding 3 months. Use of classes of medications, including analgesics, laxatives, anti-diarrhoeal, and antidepressant medications were recorded. The consistency of stool was reported as ‘very hard’, ‘hard’, ‘not too hard and not too soft’, ‘very soft or mushy’, or ‘watery’. Health professional consultation and health professional-diagnosed medical conditions, including a past and/or current diagnosis of depression or anxiety during the preceding 12 months were also documented. Adolescents reported nausea and vomiting as absent, sometimes, or often, and rated their overall health status on a scale using the descriptors “poor”, “fair”, “good”, “very good” or “excellent”. We defined nausea or vomiting reported as often experienced as frequent nausea or frequent vomiting. The parent or primary care provider independently completed a questionnaire regarding the health and lifestyle of the adolescent, and this was used to verify medications, diagnoses and health professional attendance. The parent or primary care provider will henceforth be referred to as parent in this study. In this study, the term adolescent refers to the 17-year-old unless age 14 years is specified. Body mass index was calculated as weight (kg)/height(m)2.
Statistical analysis
Continuous descriptive data were summarised as means and standard deviations, with categorical variables as proportions. The main outcome variables were the presence and frequency of abdominal pain, report of being unhappy, and the self-rated health status. Differences in continuous variables were compared using the independent t test. Differences between categorical variables were determined with the Pearson chi-square test or Fisher’s exact test. All p values were reported as two-sided and were interpreted at the 5% level of significance. Multivariable logistic regression models were used to calculate the odds of abdominal pain, depression, anxiety or self-rated poor-severe health status from abdominal pain, other gastrointestinal symptoms, depression, anxiety, reported unhappiness at different childhood and adolescent ages, and medications that were statistically significant in univariate analysis. Interaction terms were tested between abdominal pain and depression, and between depression and sex but no significant interaction was identified. Data were analyzed using IBM SPSS statistics for Windows (version 20.0; IBM Corp., Armonk, NY).
Results
Abdominal pain
Age 17 years
The three-month prevalence of abdominal pain was 457/1281 (35.7%), including at least once per week in 7% of adolescents. The usual stool frequency and consistency patterns in adolescents with or without abdominal pain are summarized in Table 1. Those with abdominal pain experienced more abdominal bloating, hard stool, nausea and vomiting than those without abdominal pain and were more commonly female (Table 1). The duration of abdominal pain was three hours or longer per episode in 117 (25.7%) and improved after having a bowel motion in 352 (77.9%). When abdominal pain was experienced ≥1 day per week (n = 89), there was an associated change in frequency or consistency of bowel motions in 72/89 (80.9%). Abdominal pain ≥1 day per week in adolescents was associated with bloating ≥1 day per week (unadjusted OR 5.96, 95% CI 3.04–11.73, p < 0.001). There was no difference in BMI between those with abdominal pain and those without abdominal pain. Amongst the adolescents, there was no prevalent diagnosis of inflammatory bowel disease.
Age 10 years
At age 10 years, 111/2014 (5.5%) children had abdominal pain during at least 12 weeks of the preceding year (6.7% girls vs. 4.4% boys, p = 0.02). Abdominal pain was predominantly experienced in the lower abdomen (49.8%) vs. peri-umbilical (37.2%) vs. upper abdomen (13.0%). There were no sex differences in the location of the abdominal pain. Further, abdominal pain was associated with painful bowel motions in 159/1999 (8.0%), improved with bowel motions in 457/1963 (23.3%), was associated with a change in stool consistency in 231/1916 (12.1%) and with a change in stool frequency in 234/1932 (12.1%). The prevalence of severe abdominal pain increased with the presence of constipation (none or mild abdominal pain 12.1% vs. severe abdominal pain 29.1%, p < 0.001). Similarly, the prevalence of painful bowel motions increased with the frequency of constipation (no constipation 4.3% vs. sometimes/ often constipated 40.9%, p < 0.001). Children with abdominal pain at 10 years were more likely to experience abdominal pain ≥1 day per week at age 17 years (unadjusted OR 5.17, 95% CI 2.75–9.73, p < 0.001) (Table 2). Abdominal pain described as sometimes or always severe in 10-year-olds, was associated with increased likelihood of abdominal pain occurring on ≥1 day per week at age 17 years (unadjusted OR 2.25, 95% CI 1.32–3.84, p = 0.003). Also, lower abdominal pain, compared with central plus upper abdominal pain, at age 10 years was associated with abdominal pain at age 17 years (unadjusted OR 1.49, 95% CI 1.04–2.13, p = 0.03).
Age 8 years
At age 8 years, 142/2108 (6.7%) children had ≥3 episodes of abdominal pain severe enough to interfere with their usual activities during the preceding three months. The frequency of abdominal pain increased with the presence of constipation (no constipation 1.8% vs. sometimes/ often constipated 11.7%, p < 0.001). Abdominal pain was more common in girls than boys (8.5% vs. 5.1%, p = 0.002) and was associated with subsequent abdominal pain at age 10 years (unadjusted OR 9.53, 95% CI 5.32–17.10, p < 0.001), and with abdominal pain ≥1 day per week at age 17 years (unadjusted OR 2.32, 95% CI 1.21–4.48, p = 0.01). (Table 2).
Age 2 years
At age 2 years, 193/1896 (10.2%) of children had painful bowel motions, according to the parent (11.7% girls vs. 8.7% boys, p = 0.03). The prevalence of painful bowel motions increased with the presence of constipation (no constipation 4.6% vs. sometimes/ often constipated 59.4%, p < 0.001). Painful bowel motions at age 2 years were associated with subsequent abdominal pain at age 8 years (unadjusted OR 3.67, 95% CI 2.06–6.51, p < 0.001) and abdominal pain ≥1 day per week at age 17 years (unadjusted OR 2.36, 95% CI 1.28–4.32, p = 0.006) (Table 2).
Emotional wellbeing - Depression, anxiety, bullying and self-reported unhappiness
Depression and anxiety at age 17 years
A past and/or current diagnosis of depression was reported in 6.2% (8.6% female vs. 3.7% male, p = 0.001) and a diagnosis of anxiety in 10.2% (12.7% female vs. 7.6% male, p = 0.001) of 17-year old adolescents. Children and adolescents reporting abdominal pain had a higher prevalence of depression and anxiety at age 17 years, compared with those without abdominal pain (Tables 3 and 4). In particular, adolescents with abdominal pain on one or more days per week were three times more likely to have a diagnosis of depression than other adolescents.
Victims of bullying at school
In the cohort, 41.7% of adolescents (50.7% with abdominal pain vs. 36.7% without abdominal pain, p < 0.001) reported that they had been bullied at school. Adolescents with recurrent abdominal pain were twice as likely to have been bullied at school. The prevalence of abdominal pain increased with the frequency of being bullied at school; from not bullied to bullied less than twice per month to bullied more than once per week (30.9% to 42.3% to 47.6%, p = 0.006).
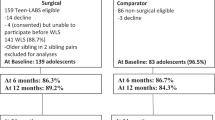
Parent-reported and self-reported unhappiness
The prevalence of parent reports of the child being unhappy and subsequent adolescent self-reports of feeling unhappy increased with age from 4.4% at age 2 years to 32.6% at age 17 years (Fig. 1). During childhood, painful bowel motions were associated with corresponding parent reports of the child being unhappy (OR 2.43, 95% CI 1.39–4.24, p = 0.002 at 2 years; OR 1.81, 95% CI 1.23–2.65 at 10 years). Similarly, frequent abdominal pain was associated with parent report of child unhappiness at age 8 years (OR 2.57, 95% CI 1.47–4.48, p = 0.001) and at 10 years (OR 3.07, 95% CI 2.03–4.65, p < 0.001). Reports of the child or adolescent being unhappy at ages 5, 8, 10 and 14 years were significantly associated with a subsequent report of being unhappy, having anxiety, depression, or experiencing abdominal pain as a 17-year-old adolescent (p < 0.05 for all, data not shown). However, being unhappy during childhood or adolescence was not consistently associated with the frequency of abdominal pain during adolescence (Table 5). Abdominal pain was more likely if one parent did not live in the household (OR 1.79, 95% CI 1.01–3.18) or the adolescent felt unhappy (OR 2.38, 95% CI 1.66–3.40), after adjusting for anxiety and depression. Recurrent abdominal pain in adolescents was associated with child reports of being unhappy at age 8 years and teacher reports that the child was unhappy at age 10 years (OR 1.75, 95% CI 1.02–2.99 and OR 2.14, 95% CI 1.21–3.78, respectively). Adolescent self-report of feeling unhappy, and parent report that the adolescent was unhappy when aged 14 and 17 years were associated with abdominal pain at age 17 years (p < 0.001, Fig. 2a,b respectively).
(a,b) Relationship between abdominal pain and unhappiness in adolescents in the Raine Study at age (a) 17 years and (b) 14 years. Bars represent unhappiness in the adolescent based on self-report or parent report, respectively. Adolescents with abdominal pain were significantly more unhappy than those not experiencing abdominal pain (p < 0.001).
Prediction of abdominal pain
Using multivariable logistic regression analysis, recurrent abdominal pain at age 17 years was associated with reports of being unhappy at age 8 years, recurrent abdominal pain at age 10 years and frequent abdominal bloating at age 17 years after adjusting for sex, diarrhoea, constipation, bullying, anxiety and depression at age 17 years (Table 5).
Medication use and health practitioner attendance
Medication use
Medication use by 17-year-old adolescents in the cohort, and associations between medication use and abdominal pain are summarized in Table 6. Medications most commonly used by adolescents were analgesics (54.1%) and vitamins or minerals (25.6%). There was a higher likelihood of use of analgesics, antidepressants, laxatives, and vitamins and minerals in adolescents with abdominal pain compared with those without abdominal pain (p < 0.05 for all). Adolescents with abdominal pain had a higher prevalence of analgesic medication use (64.9% vs. 48.2%, p < 0.001) and antidepressant medication use (3.6% vs. 0.7%, p = 0.001) compared with adolescents without abdominal pain. Female sex and use of analgesics or antidepressants were independently associated with abdominal pain after adjusting for use of laxatives, anti-emetics, intestinal motility, anti-diarrhoeal medications, or vitamins and minerals (Table 6).
Health practitioner attendance
Adolescents with abdominal pain were more likely to have attended a primary care physician, psychologist or psychiatrist, dietitian, or school nurse during the preceding 12 months than those without abdominal pain (p < 0.05 for all).
Perceived health status
Adolescents with abdominal pain self-reported their health as being mostly, or definitely, not excellent twice as often as those without abdominal pain (23.6% vs. 11.2%, p < 0.001). Frequent abdominal pain was more likely to be associated with “poor” or “fair” health, and less likely to be associated with “very good” or “excellent” health than less frequent abdominal pain. Table 7 summarises the association between adolescent characteristics and poor-fair overall health rating in adolescents with abdominal pain. In univariate analysis, factors associated with increased odds of describing poor-fair health status in adolescents with abdominal pain were depression, nausea, feeling unhappy and anxiety. In multivariate analysis, depression, nausea and feeling unhappy were associated with poorer self-reported health status after adjusting for other variables (Table 7).
Discussion
In our study, abdominal pain was common in children and adolescents, particularly females. About one-third of 17-year-old adolescents experienced abdominal pain, lasting at least three hours in one quarter. Abdominal pain was associated with hard stool consistency, nausea and depression in adolescents. Further, adolescents with abdominal pain were more than twice as likely to have a history of depression. Children with frequent or recurrent abdominal pain or painful bowel motions had a higher likelihood of constipation during childhood, and frequent abdominal pain, depression or anxiety during adolescence, compared with other children. Also, feeling unhappy during childhood was prospectively associated with recurrent abdominal pain at age 17 years.
Consistent with previous reports, females reported more frequent abdominal pain than males9,12,20 that was associated with a higher prevalence of depression and anxiety21,22,23,24. The bidirectional relationship between abdominal pain and depression or anxiety in adolescents highlights the risk of progression of one in relation to the other21. The improvement in abdominal pain with bowel motions in the majority of adolescents in our study, and the association with depression and anxiety raises the possibility of a functional abdominal pain disorder such as irritable bowel syndrome in some of the adolescents. An association between persistent abdominal pain in children, prevalent poor health and emotional disorders in parents, and increased future risk of adult psychiatric disorders has previously been described in a population-based longitudinal study25. Our observation that adolescents living in single parent homes had a higher prevalence of abdominal pain is consistent with a previous report regarding the influence of family composition and functioning on abdominal pain in children26.
Co-existing non-organic abdominal complaints, depression, anxiety and fatigue identify individuals at risk of chronicity of symptoms, who may benefit from interventions to ameliorate their symptom complaints and illness behaviour27. This is reinforced by our observation that self-reported unhappiness was associated with recurrent abdominal pain independent of a diagnosis of depression or anxiety. This suggests that the emotional burden of abdominal pain may be substantial and under-appreciated in the absence of a formal diagnosis of depression or anxiety. Recurrent abdominal pain could be a source of unhappiness or conversely unhappiness could manifest somatically as abdominal pain. A holistic approach to caring for patients with abdominal pain and/ or emotional concerns is therefore important.
The fact that abdominal pain increased with the frequency of being bullied at school is concerning. Bullying may have considerable effects on emotional wellbeing in adolescents, with anxiety, depression and gastrointestinal symptoms as related somatic consequences. Bullying may not only serve as a direct trigger of emotional difficulties, but may also perpetuate symptoms of distress. Conversely, the adolescent experiencing distress may also be more vulnerable to being bullied by others. Victims of bullying have been shown to experience more psychosomatic symptoms, including abdominal pain, than non-victims28,29 and also subsequent adverse health-related quality of life30. Thus, abdominal pain in bullied adolescents could be a somatic feature of school anxiety.
Strengths of our study are the large cohort size derived from a well-characterized population-based cohort with comprehensive longitudinal assessments and examined domains including gastrointestinal symptoms, prospectively recorded medications and medical diagnoses. During the 17-year follow-up, the Raine Cohort was considered to be representative of the broader Western Australian population from birth through to adolescence, with characteristics of the families being similar to contemporaneous Western Australian families19.
Our study has several limitations, as it is an observational study and with serial assessment there has been cohort attrition. Symptoms relied on recall during each cross-sectional assessment, particularly parent report for children, as is common in clinical practice and many studies on functional gastrointestinal disorders using the Rome criteria10. Abdominal pain-related questions applied in the various cross-sectional assessments during childhood and adolescence were different, without standardized diagnostic criteria and relying on parent report for children but self-report by adolescents aged 17 years. A history of anxiety or depression relied on a diagnosis by the primary care physician, reported by the parent and/or adolescent. Also, child unhappiness was reported by parents during childhood ages, with potential for over- or underestimation of symptoms compared with adolescent self-report of unhappiness at ages 14 and 17 years. Consequently, changes in the incidence and types of presumed functional abdominal pain disorders from early childhood into adolescence, and influence of parental anxiety on these could not be determined from the study design. While these factors could potentially increase the risk of bias, the relationship between abdominal pain and unhappiness, depression or anxiety in longitudinal analysis remained consistent during longitudinal assessments. While our study describes associations, we are unable to ascribe causality, account for potential medication side effects that could contribute to abdominal pain or other gastrointestinal symptoms and could not determine whether antidepressants were used for depression, anxiety or adjuncts to analgesia. However, given the stringent guidance on antidepressant medication use in children and adolescents the most likely indications would be depression and anxiety. Since somatic pain at other sites is common in individuals with abdominal pain, use of analgesics cannot be attributed to abdominal pain alone23. Associations between abdominal and extra-abdominal somatic pain was beyond the scope of this study. We are also unable to ascertain the direction of association between abdominal pain and other gastrointestinal symptoms, depression, anxiety or bullying from this study, as both abdominal pain and reports of unhappiness were commonly reported. However, chronic or recurrent physical health problems, particularly pain, are known to associate with higher rates and severity of depression and often precede depression31.
Other possible explanations for the association between abdominal pain and depression are abdominal pain as an autonomic and somatic symptom of depression, anxiety or somatization disorder31,32. Thus, recurrent abdominal pain may be a somatic manifestation of emotional distress, legitimise the experience of distress or represent less stigmatised help-seeking behaviour. For instance, in the Raine Cohort, back and neck pain have also been linked with depression and anxiety in adolescents33. Arguably, a number of children and adolescents may find somatic communication of emotional distress more convenient than describing low mood or anxiety at home, school and among peers, and with a more engaging universal response than communicating emotional distress. A previous study concluded that maternal anxiety was the most consistent predictor of subsequent abdominal pain, school absence and anxiety disorders in children34. One could hypothesise that somatic complaints may be conditioned in a small proportion of youth. With a high proportion of individuals not receiving a satisfactory explanation for their abdominal pain9, there is a risk of chronicity of inadequately treated abdominal pain that may be associated with anxiety, depression and self-medication with analgesics, other drugs or substance use. In our study, adolescents with abdominal pain described themselves as being more unhappy than those without abdominal pain, at both ages 14 and 17 years, suggesting potential chronicity of dysphoria or unhappiness. This description was unrelated to diagnosed depression, highlighting the importance of understanding the significance of, and possibly enquiry regarding, the state of happiness or unhappiness in children and adolescents. Notably, adolescents experiencing abdominal pain were also twice as likely to describe their health as not excellent, compared with those not experiencing abdominal pain. These findings underscore the importance of considering the mental health burden of physical illness and vice versa. Nevertheless, there are inconclusive reports of benefits of antidepressant medications for treatment of recurrent abdominal pain in children and adolescents35. Sex-differences in the gut microbiome through the life-course have been associated with mental health disorders, including anxiety and depression36,37, as well as with functional gastrointestinal disorders38. Consequently, influences of the gut microbiome on the gut-brain axis may contribute to the link between abdominal pain and the mental health of adolescents. Knowledge regarding impacts of the gut microbiome on gut-to-brain and brain-to-gut pathways associated with gastrointestinal and neuropsychiatric phenotypes of functional abdominal pain continue to evolve39. In the interim, in the absence of alarm symptoms from history and physical examination, primary care physicians should explain to the parent, adolescent or child that abdominal pain is common and rarely associated with disease40.
In conclusion, recurrent abdominal pain is common in children and adolescents and is frequently associated with other gastrointestinal symptoms, and adverse emotional wellbeing, including current or subsequent history of depression, anxiety, unhappiness, being bullied at school, and lower self-perceived health status. Adolescents with abdominal pain demonstrate increased health-seeking behavior, including health professional consultation or medication use, and ill-health. Abdominal pain may also be a somatic feature of underlying emotional distress, masking or delaying psychological help-seeking in children and adolescents. The “duration of unrecognized or untreated distress” may further contribute to chronicity. A comprehensive approach to assessment and management of adolescents suffering from recurrent, persistent or chronic abdominal pain should involve an understanding of the burden of the somatic symptom pattern, psychosocial factors, and family factors on severity and chronicity. Health practitioners have an important role to play in identifying and managing risk associations in adolescents with abdominal pain. Since chronic abdominal pain often precedes depression and chronic use of analgesics, appropriate psychological or pharmacological intervention to manage abdominal pain are critical before a worsening trajectory of depression or anxiety develops in children and adolescents. This temporal relationship is worth further exploration as recurrent and persistent abdominal pain symptoms may be a prodrome of depression and anxiety or vice versa in youth. Future studies should explore not only the “gut - feelings” relationships between abdominal pain, gastrointestinal symptoms, other somatic pain sites and mental health, but also the influence of parent factors and family functioning. Finally, the impact of chronic abdominal pain on parents and siblings of the child or adolescent experiencing abdominal pain should not be overlooked.
References
Australian Institute of Health and Welfare. Australia’s health 2016. Australia’s health series no. 15. Cat. no. AUS 199. Canberra: AIHW (2016). https://www.aihw.gov.au/getmedia/9844cefb-7745-4dd8-9ee2-f4d1c3d6a727/19787-AH16.pdf.aspx (accessed January 2019).
Peery, A. F. et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology. 156, 254–272.e111 (2019).
Park, R. et al. Inpatient burden of childhood functional GI disorders in the USA: an analysis of national trends in the USA from 1997 to 2009. Neurogastroenterol. Motil. 27, 684–692 (2015).
Breckan, R. K. et al. Prevalence, comorbidity, and risk factors for functional bowel symptoms: a population-based survey in Northern Norway. Scand. J. Gastroenterol. 47, 1274–1282 (2012).
Shraim, M. et al. Repeated primary care consultations for non-specific physical symptoms in children in UK: a cohort study. BMC Fam. Pract. 15, 195 (2014).
Myer, P. A. et al. Clinical and economic burden of emergency department visits due to gastrointestinal diseases in the United States. Am. J. Gastroenterol. 108, 1496–1507 (2013).
Britt, H. et al. General practice activity in Australia 2015–16. General practice series no. 40. Sydney: Sydney University Press (2016), purl.library.usyd.edu.au/sup/9781743325131 (accessed Janaury 2019).
Australian Institute of Health and Welfare. Emergency department care 2016–17: Australian hospital statistics. Health services series no. 80. Cat. no. HSE 194. Canberra: AIHW (2017). https://www.aihw.gov.au/getmedia/981140ee-3957-4d47-9032-18ca89b519b0/aihw-hse-194.pdf.aspx?inline=true (accessed January 2019).
BEACH Program, AIHW General Practice Statistics and Classification Unit. Presentations of abdominal pain in Australian general practice. Aust Fam Physician. 33, 968–969 (2004).
Drossman, D. A. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology 150, 1262–1279 (2016).
Hyams, J. S. et al. Functional Disorders: Children and Adolescents. Gastroenterology 150, 1456–1468 (2016).
Bayram, C., Britt, H. & Fahridin, S. Adolescent attendances in general practice. Aust. Fam. Physician. 36, 586–587 (2007).
Ayonrinde, O. T. et al. Bowel patterns, gastrointestinal symptoms and emotional well-being in adolescents - A cohort study. J. Gastroenterol. Hepatol. 34, 1946–1954 (2019).
Schwille, I. J. et al. A Community-Based Survey of Abdominal Pain Prevalence, Characteristics, and Health Care Use Among Children. Clin. Gastroenterol. Hepatol. 7, 1062–1068 (2009).
Horst, S., Shelby, G. & Anderson, J. Predicting persistence of functional abdominal pain from childhood into young adulthood. Clin. Gastroenterol. Hepatol. 12, 2026–2032 (2014).
Swain, M. S. et al. An international survey of pain in adolescents. BMC Public. Health. 14, 447 (2014).
Velly, A. M. & Mohit, S. Epidemiology of pain and relation to psychiatric disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 87(Pt B), 159–167 (2018).
Newnham, J. P., Evans, S. F., Michael, C. A., Stanley, F. J. & Landau, L. I. Effects of frequent ultrasound during pregnancy: a randomised controlled trial. Lancet. 342, 887–891 (1993).
Straker, L., Mountain, J. & Jacques, A. Cohort Profile: The Western Australian Pregnancy Cohort (Raine) Study-Generation 2. Int. J. Epidemiol. 46, 1384–1385j (2017).
Kristjánsdóttir, G. Sociodemographic differences in the prevalence of self-reported stomach pain in school children. Eur. J. Pediatr. 155, 981–983 (1996).
Breivik, H. Depression and anxiety in adolescents aggravate abdominal pain, and abdominal pain deepens depression which increases suffering from chronic pain. Scand. J. Pain. 5, 182–183 (2014).
von Gontard, A. et al. Abdominal pain symptoms are associated with anxiety and depression in young children. Acta Paediatr. 104, 1156–1163 (2015).
Gerrits, M. M. et al. Pain, not chronic disease, is associated with the recurrence of depressive and anxiety disorders. BMC Psychiatry. 14, 187 (2014).
Walter, S. A. et al. Abdominal pain is associated with anxiety and depression scores in a sample of the general adult population with no signs of organic gastrointestinal disease. Neurogastroenterol. Motil. 25, 741–e576 (2013).
Hotopf, M., Carr, S., Mayou, R., Wadsworth, M. & Wessely, S. Why do children have chronic abdominal pain, and what happens to them when they grow up? Population based cohort study. BMJ 316(7139), 1196–1200 (1998).
Bode, G., Brenner, H., Adler, G. & Rothenbacher, D. Recurrent abdominal pain in children - Evidence from a population-based study that social and familial factors play a major role but not Helicobacter pylori infection. J. Psychosom. Res. 54, 417–421 (2003).
Colgan, S., Creed, F. & Klass, H. Symptom complaints, psychiatric disorder and abnormal illness behaviour in patients with upper abdominal pain. Psychol. Med. 18, 887–892 (1988).
Gini, G. & Pozzoli, T. Association Between Bullying and Psychosomatic Problems: A Meta-analysis. Pediatrics 123, 1059–1065 (2009).
Boey, C. C. & Goh, K. L. The significance of life-events as contributing factors in childhood recurrent abdominal pain in an urban community in Malaysia. J. Psychosom. Res. 51, 559–562 (2001).
Allison, S., Roeger, L. & Reinfeld-Kirkman, N. Does school bullying affect adult health? Population survey of health-related quality of life and past victimization. Aust. N. Z. J. Psychiatry. 43, 1163–1170 (2009).
Hilderink, P. H. et al. The temporal relation between pain and depression: Results from the Longitudinal Aging Study Amsterdam. Psychol. Med. 74, 945–951 (2012).
Dunn, K. M., Jordan, K. P. & Mancl, L. Trajectories of pain in adolescents: A prospective cohort study. Pain. 152, 66–73 (2011).
Rees, C. S. et al. Back and neck pain are related to mental health problems in adolescence. BMC Public Health. (2011).
Ramchandani, P. G. et al. The impact of recurrent abdominal pain: predictors of outcome in a large population cohort. Acta Paediatrica 96, 697–701 (2007).
Martin, A. E. et al. Pharmacological interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev. 3, CD010973, https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010973.pub2/full (accessed September 2019) (2017).
Jaggar, M., Rea, K., Spicak, S., Dinan, T. G., Cryan, J. F. You’ve got male: Sex and the microbiota-gut brain axis across the lifespan. Front Neuroendocrinol, https://doi.org/10.1016/j.yfrne.2019.100815 [Epub ahead of print] (2019).
Mohajeri, M. H., La Fata, G., Steinert, R. E. & Weber, P. Relationship between the gut microbiome and brain function. Nutr. Rev. 76, 481–496 (2018).
Shin, A., Preidis, G. A., Shulman, R. & Kashyap, P. C. The Gut microbiome in adult and pediatric functional gastrointestinal disorders. Clin. Gastroenterol. Hepatol. 17, 256–274 (2019).
Koloski, N. A., Jones, M. & Talley, N. J. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment. Pharmacol. Ther. 44, 592–600 (2016).
Berger, M. Y., Gieteling, M. J. & Benninga, M. A. Chronic abdominal pain in children. BMJ 334, 997–1002 (2007).
Acknowledgements
We thank the Raine Study participants and their families. We also thank the Raine Study team for cohort coordination and data collection. The National Health and Medical Research Council for long term contribution to funding the Raine Study since inception, the Raine Medical Research Foundation, The University of Western Australia (UWA), Curtin University, Telethon Kids Institute, UWA Faculty of Medicine, Dentistry and Health Sciences, Women’s and Infants Research Foundation, Edith Cowan University, Murdoch University and The University of Notre Dame Australia are acknowledged for their support and funding of the core management of the Raine Study. The 17 year follow-up of the Raine Cohort was funded by National Health and Medical Research Council Program grant 353514 and Project grants 403981. Dr OT Ayonrinde is funded by a Western Australia Department of Health and Raine Medical Research Foundation Clinician Research Fellowship.
Author information
Authors and Affiliations
Contributions
Oyekoya T. Ayonrinde - study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis; obtained funding. Oyedeji A. Ayonrinde - study concept and design; critical revision of the manuscript for important intellectual content. Leon A. Adams - study concept and design; acquisition of data; critical revision of the manuscript for important intellectual content; obtained funding. Frank M Sanfilippo - study concept and design; critical revision of the manuscript for important intellectual content; obtained funding. Therese A. O’Sullivan - study concept and design; critical revision of the manuscript for important intellectual content; obtained funding. Monique Robinson - study concept and design; critical revision of the manuscript for important intellectual content; obtained funding. Wendy H. Oddy - critical revision of the manuscript for important intellectual content. John K. Olynyk - study concept and design; acquisition of data; critical revision of the manuscript for important intellectual content; obtained funding.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ayonrinde, O.T., Ayonrinde, O.A., Adams, L.A. et al. The relationship between abdominal pain and emotional wellbeing in children and adolescents in the Raine Study. Sci Rep 10, 1646 (2020). https://doi.org/10.1038/s41598-020-58543-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-58543-0
This article is cited by
-
The Cost-Effectiveness of a Dance and Yoga Intervention for Girls with Functional Abdominal Pain Disorders
PharmacoEconomics - Open (2023)
-
Identifying threshold sizes for enlarged abdominal lymph nodes in different age ranges from about 200,000 individual’s data
Scientific Reports (2021)
-
Schmerzmedizinische Versorgung chronisch schmerzkranker Kinder und Jugendlicher in Deutschland
Der Schmerz (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.