Abstract
The association between thiazide use and fracture risk is still controversial. We conducted an updated meta-analysis on the association between thiazide use and fracture risk. We systematically searched PubMed, Embase, and Cochrane library databases for all types of human studies, including observational and experimental studies that were published up until July 2019. We also manually searched the reference lists of relevant studies. The pooled relative risks (RRs) with 95% credible interval (CrI) were calculated using a Bayesian hierarchical random effect model. A total of 19 case-control (N = 496,568 subjects) and 21 cohort studies (N = 4,418,602 subjects) were included in this meta-analysis. The pooled RR for fractures associated with thiazide use was 0.87 (95% CrI: 0.70–0.99) in case-control and 0.95 (95% CrI: 0.85–1.08) in cohort studies. The probabilities that thiazide use reduces any fracture risk by more than 0% were 93% in case-control studies and 72% in cohort studies. Significant heterogeneity was found for both case-control (p < 0.001, I2 = 75%) and cohort studies (p < 0.001, I2 = 97.2%). Thiazide use was associated with reduced fracture risk in case-control studies, but not in cohort studies. The associations demonstrated in case-control studies might be driven by inherent biases, such as selection bias and recall bias. Thus, thiazide use may not be a protective factor for fractures.
Similar content being viewed by others
Introduction
Hypertension and osteoporotic fracture are two major public health problems because they result in a substantial financial burden among the elderly as well as considerable increases in morbidity and mortality1,2. Thiazide diuretics are one of the most common types of antihypertension medications3,4. There is evidence suggesting that thiazide diuretics reduce urinary calcium excretion5, and stimulate osteoblast differentiation and bone mineral formation6. Although a previous meta-analysis suggested that thiazide use was associated with reduced fracture risk7,8,9, results of individual studies are still inconsistent, ranging from positive to negative effects10,11,12,13,14,15,16,17,18,19. In addition, two previous meta-analyses were published over a decade ago7,8, and the most recent meta-analysis that was published in 2018 was limited to only prospective cohort studies9. Therefore, an updated meta-analysis that is inclusive of all types of study designs is warranted. We conducted a Bayesian meta-analysis on the association between thiazide use and fracture risk as it uses a probabilistic approach to make clinically relevant decisions in the face of uncertainty. For example, using the Bayesian method, we can determine the probability that thiazide use reduces fracture risk by more than 0%, 10% or 20%; this probability is unable to be provided by classical analysis20. Therefore, we utilized an advanced methodology in meta-analysis research to address the much controversial relationship between thiazide use and fracture risk that encapsulates all peer-reviewed publications in the field thus far.
Methods
Data searching
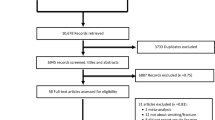
This study was undertaken according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)21. We systematically searched PubMed, Embase, and Cochrane library databases for all types of human studies, including observational and experimental studies that were published up until July 2019. The keywords and medical subject headings (MeSH) used for the search were: “thiazide” OR “Sodium Chloride Symporter Inhibitors” AND “Bone fracture” OR “Fracture” OR “Osteoporosis”. We also manually searched the reference lists of relevant studies. Studies were included in the meta-analysis if they met the following criteria: (a) were original human studies; (b) used thiazide as an exposure; (c) had risk estimates for fracture outcome. When more than one study used the same data, we included the most recent and best quality study in our meta-analysis.
Data extraction and quality assessment
Two investigators (TGC, SY) independently identified and extracted all potential articles for inclusion. Any disagreement between the above two investigators was resolved by discussing it with the third author (YL). The following information was retrieved from each study: first author’s name, year of publication, the percentage of female participants, sample size, fracture outcome, mean age, country, and fracture risk estimates. The Newcastle-Ottawa Scale (NOS) was used to assess the quality of each individual study22. Briefly, the NOS score was assessed using the following items: selection, comparability, exposure, and outcome; a NOS score of 7 or higher is considered as high quality23.
Statistical analysis
We synthesized the data using both classical and Bayesian hierarchical random-effects models24,25,26. In classical meta-analysis, we used the DerSimonian-Laird method27 to calculate the pooled risk ratio. In the Bayesian model, the risk ratios (RRs) for all the studies were converted into a logarithmic scale (denoted as \(\,{\phi }_{i}\)). Each \({\phi }_{i}\) was assumed to have a normal distribution with a true, but unknown effect size (\({\theta }_{i}\)) and known within-study variance (\({{\delta }_{i}}^{2}\)). The collection of \({\theta }_{i}\,\) across the studies was assumed to have a normal distribution, with unknown mean (\(\mu )\) and variance \(\,({\tau }^{2}\)), where μ was the estimate of the overall log (RR), and \({\tau }^{2}\) was a measure of variation between the studies. The prior information of \({\tau }^{2}\) was assumed to be an inverse gamma distribution (0.001, 0.001). The prior function for μ was assumed equivocal prior; i.e., thiazide use does not affect fracture risk (\(\mu \) = 0, variance = 10,000). We also examined the probability that thiazide use reduces fracture risk by more than 0%, 10%, and 20% (i.e., RR < 1.0, 0.9, 0.8). Heterogeneity of the included studies was assessed with Cochran’s Q-statistic test, and inconsistency was quantified by I2 statistic28,29. Funnel plots were generated to identify potential publication bias using Egger’s test30. All analyses were performed by the programs WinBUGS (Version 1.4.3, MRC Biostatistics Unit, Cambridge, UK) and R (Version: 3.4.3; R Foundation for Statistical Computing, Vienna, Austria).
Results
Characteristics of studies
We identified a total of 959 articles from different electronic databases and other sources. Of these, 633 duplicate articles and 181 irrelevance articles were excluded after reading the title or abstract. Finally, 19 case-control studies and 21 cohort studies were met for inclusion in this meta-analysis (Fig. 1). A majority (72.5%) of the included studies were considered as high quality based on NOS standards (Table 1). In the case-control studies, approximately 79% of the participants (Total sample size = 496,568) were female; the average participant age in the case-control studies was 72 years old. Approximately 63% of the subjects (Total sample size = 4,418,602) were female in cohort studies. The average participant age in the cohort studies was 73 years old.
Thiazide use and fracture risk in case-control studies
In the classical meta-analysis of case-control studies, we found a negative association between thiazide use and fracture risk (Risk ratio (RR): 0.87, 95% confidence interval (CI): 0.76–0.98). We observed moderate heterogeneity between studies (p < 0.001, I2 = 75%; Fig. 2). In the Bayesian analysis, the pooled RR for fractures associated with thiazide use was 0.87 (95% credible interval (CrI) 0.70–0.99). The probabilities that thiazide use reduces fracture risk by more than 0%, 10%, and 20% were 93%, 66%, and 23%, respectively (Table 2).
Thiazide use and fracture risk in cohort studies
In the classical meta-analysis of cohort studies, there was no significant association between thiazide use and fracture risk (RR: 0.93, 95% CI: 0.83–1.05). The heterogeneity between studies was significant (p < 0.001, I2 = 97.2%; Fig. 3). In the Bayesian analysis, the pooled RR for fractures associated with thiazide use was 0.95 (95% CrI: 0.85–1.08). The probabilities that thiazide use reduces fracture risk by more than 0%, 10%, and 20% were 72%, 23%, and 2%, respectively (Table 2).
Publication bias
The funnel plot of risk ratio versus standard error for the association between thiazide use and fracture risk was shown in Fig. 4. No significant publication bias was observed for both case-control studies (Egger’s test: p = 0.65; Fig. 4a) and cohort studies (Egger’s test: p = 0.52; Fig. 4b).
Discussion
This meta-analysis provides evidence to support that thiazide exposure is associated with a 13% reduction of fracture risk in case-control studies. However, while an inverse association was noted in cohort studies, it failed to reach statistical significance.
Our findings were partly comparable with the effect shown in the previous two meta-analyses reported by Wiens et al.8 and Xiao et al.9; both studies suggested that thiazide was associated with the reduction of any fracture risk by 14%. However, to the best of our knowledge, our meta-analysis is the first to distinguish a difference in the relationship between thiazide use and fracture risk by study design. We found that there is a null relationship between thiazide use and fracture risk in cohort studies. A recently published meta-analysis also suggested that the effect of thiazide use on fracture risk was weaker in cohort studies9. Although the results from the Bayesian meta-analysis were consistent with that generated from the classical meta-analysis approach, the Bayesian meta-analysis provides additional regarding the probabilities that thiazide use reduces fracture risk by certain percentages. Such information is useful for making clinically relevant decisions about the use of thiazides, and cannot be obtained using the traditional meta-analysis methodology.
The controversial relationship between thiazide diuretics and fractures involves conflicting mechanisms. On the one hand, thiazide could exert beneficial effects on the bone via decreasing urinary calcium excretion by 25–40%31,32. In addition, thiazides are associated with an increased level of metabolic alkalosis, which is an inhibitor of bone resorption33,34. On the other hand, thiazides diuretics could induce hyponatremia, which has a negative impact on the metabolism and integrity of the bone35,36. In addition, thiazide induced-hyponatremia could have harmful neurological side effects, such as gait disturbances and imbalance, which leads to an increased risk of falls and fractures37.
This meta-analysis has several limitations. First, due to the absence of relevant experimental studies in humans, our meta-analysis included only observational studies. A meta-analysis based on observational studies cannot make causal inferences about thiazide use and fracture risk. Second, we observed considerable heterogeneity between individual studies, which might bias our results. Lastly, due to insufficient data from individual studies, we did not evaluate the effect of dose and duration of thiazide use on bone fractures.
In conclusion, this meta-analysis included 19 case-control and 21 cohort studies to examine the relationship between thiazide use and fracture risk. Our results suggest that thiazide use was associated with reduced fracture risk in case-control studies, but not in cohort studies. The associations demonstrated in case-control studies might be driven by inherent biases such as selection bias and recall bias. Thus, thiazide use may not be a protective factor for fractures. Randomized clinical trials are still warranted to confirm our findings.
Data availability
The data analyzed for the current study are all available from the published individual studies.
References
Cappuccio, F. P., Meilahn, E., Zmuda, J. M. & Cauley, J. A. High blood pressure and bone-mineral loss in elderly white women: a prospectjive study. Study of Osteoporotic Fractures Research Group. Lancet 354, 971–975 (1999).
Johnell, O. & Kanis, J. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17, 1726–1733 (2006).
Ilic, K., Obradovic, N. & Vujasinovic-Stupar, N. The relationship among hypertension, antihypertensive medications, and osteoporosis: a narrative review. Calcif Tissue Int 92, 217–227 (2013).
Wright, J. & Musini, V. First-line drugs for hypertension. Cochrane Database Syst Rev, CD001841 (2009).
Butt, D. A. et al. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med 172, 1739–1744 (2012).
Dvorak, M. M. et al. Thiazide diuretics directly induce osteoblast differentiation and mineralized nodule formation by interacting with a sodium chloride co-transporter in bone. J Am Soc Nephrol 18, 2509–2516 (2007).
Jones, G., Nguyen, T., Sambrook, P. N. & Eisman, J. A. Thiazide diuretics and fractures: can meta-analysis help? J Bone Miner Res 10, 106–111 (1995).
Wiens, M., Etminan, M., Gill, S. & Takkouche, B. Effects of antihypertensive drug treatments on fracture outcomes: a meta-analysis of observational studies. J Intern Med 260, 350–362 (2006).
Xiao, X., Xu, Y. & Wu, Q. Thiazide diuretic usage and risk of fracture: a meta-analysis of cohort studies. Osteoporos Int 29, 1515–1524 (2018).
Kim, S. Y. et al. Number of daily antihypertensive drugs and the risk of osteoporotic fractures in older hypertensive adults: National health insurance service-senior cohort. J Cardiol 70, 80–85 (2017).
Kruse, C., Eiken, P. & Vestergaard, P. Continuous and long-term treatment is more important than dosage for the protective effect of thiazide use on bone metabolism and fracture risk. Journal of Internal Medicine 279 (2016).
Lin, S. M., Yang, S. H., Cheng, H. Y., Liang, C. C. & Huang, H. K. Thiazide diuretics and the risk of hip fracture after stroke: a population-based propensity-matched cohort study using Taiwan’s National Health Insurance Research Database. BMJ Open 7, e016992 (2017).
Lin, S. M., Yang, S. H., Wang, C. Y. & Huang, H. K. Association between diuretic use and the risk of vertebral fracture after stroke: a population-based retrospective cohort study. BMC Musculoskelet Disord 20, 96 (2019).
Paik, J. M., Rosen, H. N., Gordon, C. M. & Curhan, G. C. Diuretic Use and Risk of Vertebral Fracture in Women. Am J Med 129, 1299–1306 (2016).
Puttnam, R. et al. Antihypertensive, Lipid-Lowering Treatment to Prevent Heart Attack Trial Collaborative Research, Group. Association of 3 Different Antihypertensive Medications With Hip and Pelvic Fracture Risk in Older Adults: Secondary Analysis of a Randomized Clinical Trial. JAMA. Intern Med 177, 67–76 (2017).
Rashiq, S. & Logan, R. F. A. Role of drugs in fractures of the femoral neck. Br Med J 292, 861–863 (1986).
Rejnmark, L., Vestergaard, P. & Mosekilde, L. Reduced fracture risk in users of thiazide diuretics. Calcif Tissue Int 76, 167–175 (2005).
Ruths, S. et al. Risk of hip fracture among older people using antihypertensive drugs: a nationwide cohort study. BMC Geriatr 15, 153 (2015).
Solomon, D. H., Mogun, H., Garneau, K. & Fischer, M. A. Risk of fractures in older adults using antihypertensive medications. J Bone Miner Res 26, 1561–1567 (2011).
Burton, P. R., Gurrin, L. C. & Campbell, M. J. Clinical significance not statistical significance: a simple Bayesian alternative to p-values. J Epidemiol Community Health 52, 318–323 (1998).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62, e1–34 (2009).
Zeng, X. et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 8, 2–10 (2015).
Poorolajal, J. & Darvishi, N. Smoking, and Suicide: A Meta-Analysis. PLoS One 11, e0156348 (2016).
Spiegelhalter, D., Myles, J., Jones, D. & Abrams, K. Bayesian methods in health technology assessment: a review. Health Technol Assess 4, 1–130 (2000).
Abrams, K. & Sanso, B. Approximate Bayesian inference for random-effects meta-analysis. Stat Med 17, 201–218 (1998).
Gelman, A., Carlin, J. B., Stern, H. S. & Rubin, D. B. Bayesian Data Analysis (Chapman & Hall/CRC, New York, 1996).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin Trials 7, 177–188 (1986).
Cochran, W. G. The combination of estimates from different experiments. Biometrics 3, 101–129 (1954).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Egger, M. D., Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997).
Duarte, C. G., Winnacker, J. L., Becker, K. L. & Pace, A. Thiazide-induced hypercalcemia. The New England Journal of Medicine 284, 828–830 (1971).
Lamberg, B. A. & Kuhlback, B. Effect of chlorothiazide and hydrochlorothiazide on the excretion of calcium in urine. Scandinavian Journal of Clinical and Laboratory Investigation 11, 351–357 (1959).
Arnett, T. R. & Spowage, M. Modulation of the resorptive activity of rat osteoclasts by small changes in extracellular pH near the physiological range. Bone 18, 277–279 (1996).
Peh, C. A. et al. The effect of chlorothiazide on bone-related biochemical variables in normal post-menopausal women. J Am Geriatr Soc 41, 513–516 (1993).
Upala, S. & Sanguankeo, A. Association Between Hyponatremia, Osteoporosis, and Fracture: A Systematic Review and Meta-analysis. J Clin Endocrinol Metab 101, 1880–1886 (2016).
Hovis, J. G. et al. Intracellular calcium regulates insulin-like growth factor-I messenger ribonucleic acid levels. Endocrinology 132, 1931–1938 (1993).
Renneboog, B., Musch, W., Vandemergel, X., Manto, M. U. & Decaux, G. Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits. Am J Med 119, 71 e71–78 (2006).
Ray, W. A., Griffin, M. R., Downey, W. & Melton, L. J. Long-term use of thiazide diuretics and the risk of hip fracture. Lancet 1, 687–690 (1989).
Stevens, A. & Mulrow, C. Drug’s affecting postural stability and other risk factors in the hip fracture epidemic case-control study. Community Med 7, 27–34 (1989).
Heidrich, F. E., Stergachis, A. & Gross, K. M. Diuretic drug use and the risk for hip fracture. Ann Intern Med 115, 1–6 (1991).
Felson, D. T., Sloutskis, D., Anderson, J. J., Anthony, J. M. & Kiel, D. P. Thiazide Diuretics and the Risk of Hip Fracture. Results From the Framingham Study. JAMA Intern Med 265, 370–373 (1991).
Jensen, J., Nielsen, L., Lyhne, N., Hallas, J. & Brosen, K. Drugs and femoral neck fracture: a case-control study. J Intern Med 229, 29–33 (1991).
Cumming, R. G. & Klineberg, R. J. Psychotropics, thiazide diuretics and hip fractures in the elderly. Med J Aust 158, 414–417 (1993).
Herings, R. M. C. et al. Current use of thiazide diuretics and prevention of femur fractures. J Clin Epidemiol 49, 115–119 (1996).
Barengolts, E., Karanouh, D., Kolodny, L. & Kukreja, S. Risk factors for hip fracture in predominantly African American veteran male population. J Bone Miner Res 16 (2001).
Weiland, S. K. et al. Thiazide diuretics and the risk of hip fracture among 70–79 year old women treated for hypertension. Eur J Public Health 7, 335–340 (1997).
Wang, P. S., Bohn, R. L., Glynn, R. J., Mogun, H. & Avorn, J. Zolpidem use and hip fractures in older people. J Am Geriatr Soc 49, 1685–1690 (2001).
Leutters, C. M., Keegan, T. H. M. & Sidney, S. Risk factors for foot fracture among individuals aged 45 years and older. Osteoporos Int 15, 957–963 (2004).
Schlienger, R. G., Kraenzlin, M. E., Jick, S. S. & Meier, C. R. Use of b-blockers and risk of fracture. JAMA 292, 1326–1332 (2004).
Kelsey, J. L., Prill, M., Keegan, T. H. M., Quesenberry, C. P. & Sidney, S. Risk factors for pelvis fracture in older persons. Am J Epidemiol 162, 879–886 (2005).
Kelsey, J. L., Keegan, T. H. M., Prill, M. M., Quesenberry, C. P. & Sidney, S. Risk factors for fractures of the shafts of the tibia and fibula in older individuals. Osteoporos Int 17, 143–149 (2006).
Peters, R. et al. The effect of treatment based on a diuretic (indapamide) +/− ACE inhibitor (perindopril) on fractures in the Hypertension in the Very Elderly Trial (HYVET). Age Ageing 39, 609–616 (2010).
Berry, S. D., Zhu, Y., Choi, H., Kiel, D. P. & Zhang, Y. Diuretic initiation and the acute risk of hip fracture. Osteoporos Int 24, 689–695 (2013).
De Vecchis, R., Ariano, C., Di Biase, G. & Noutsias, M. Thiazides and Osteoporotic Spinal Fractures: A Suspected Linkage Investigated by Means of a Two-Center, Case-control Study. J Clin Med Res 9, 943–949 (2017).
Cauley, J. A. et al. Effects of thiazide diuretic therapy on bone mass, fractures, and falls. The Study of Osteoporotic fracture Research Group. Ann Intern Med 118, 666–673 (1993).
Cummings, S. R. et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332, 767–773 (1995).
Nguyen, T. V., Eisman, J. A., Kelly, P. J. & Sambrook, P. N. Risk factors for osteoporotic fractures in elderly men. Am J Epidemiol 144, 255–263 (1996).
Guo, Z., Wills, P., Viitanen, M., Fastbom, J. & Winblad, B. Cognitive impairment, drug use, and the risk of hip fracture in persons over 75 years old: a community-based prospective study. Am J Epidemiol 148, 887–892 (1998).
Feskanich, D., Willett, W. C., Stampfer, M. J. & Colditz, G. A. A prospective study of thiazide use and fractures in women. Osteoporosis Int 7, 79–88 (1997).
Schoofs, M. W. et al. Thiazide Diuretics and the Risk for Hip Fracture. Ann Intern Med 139, 476–482 (2003).
LaCroix, A. Z. et al. Thiazide diuretic agents and the incidence of hip fracture. N Engl J Med 322, 286–290 (1990).
Chow, K. et al. Fracture risk after thiazide-associated hyponatremia. Intern Med J 42, 760–764 (2012).
Carbone, L. D. et al. Thiazide use is associated with reduced risk for incident lower extremity fractures in men with spinal cord injury. Arch Phys Med Rehabil 95, 1015–1020 (2014).
Bokrantz, T. et al. Thiazide diuretics and the risk of osteoporotic fractures in hypertensive patients. Results from the Swedish Primary Care Cardiovascular Database. J Hypertens 35, 188–197 (2017).
Chen, H. Y., Ma, K. Y., Hsieh, P. L., Liou, Y. S. & Jong, G. P. Long-term Effects of Antihypertensive Drug Use and New-onset Osteoporotic Fracture in Elderly Patients: A Population-based Longitudinal Cohort Study. Chin Med J (Engl) 129, 2907–2912 (2016).
Torstensson, M. et al. Danish register-based study on the association between specific cardiovascular drugs and fragility fractures. BMJ Open 5, e009522 (2015).
Acknowledgements
The authors would like to thank Dr. Ann Vuong for the critical proofreading of this manuscript.
Author information
Authors and Affiliations
Contributions
Concept and study design: T.G.C. and S.Y. Data searching and collection: T.G.C. and S.Y. Data analysis: T.G.C. Interpretation of the results: T.G.C. and S.Y. Drafting manuscript: T.G.C. and S.Y. Revising manuscript content: T.G.C., S.Y., J.L. and Y.L. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Charkos, T.G., Liu, Y., Jin, L. et al. Thiazide Use and Fracture Risk: An updated Bayesian Meta-Analysis. Sci Rep 9, 19754 (2019). https://doi.org/10.1038/s41598-019-56108-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-56108-4
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.