Abstract
We assessed anthropometry in 22,421 adult daughters in association with their mothers’ tobacco smoking early in pregnancy (at their first antenatal visit) in Sweden, particularly their risk of short stature and obesity. Adult daughters were grouped by maternal smoking levels during pregnancy: Non-smokers (58.5%), Light smokers (24.1%; smoked 1–9 cigarettes/day), and Heavier smokers (17.4%; smoked ≥10 cigarettes/day). Anthropometry was recorded on the adult daughters at approximately 26.0 years of age. Obesity was defined as BMI ≥30 kg/m2, and short stature as height more than two standard deviations below the population mean. Daughters whose mothers were Light and Heavier smokers in early pregnancy were 0.8 cm and 1.0 cm shorter, 2.3 kg and 2.6 kg heavier, and had BMI 0.84 kg/m2 and 1.15 kg/m2 greater, respectively, than daughters of Non-smokers. The adjusted relative risk of short stature was 55% higher in women born to smokers, irrespectively of smoking levels. Maternal smoking had a dose-dependent association with obesity risk, with offspring of Heavier smokers 61% and of Light smokers 37% more likely to be obese than the daughters of Non-smokers. In conclusion, maternal smoking in pregnancy was associated with an increased risk of short stature and obesity in their adult daughters.
Similar content being viewed by others
Introduction
The harmful effects of smoking are widely established. For pregnant women, these effects are known to extend to the fetus, leading to a variety of adverse pre- and post-natal health effects1. Trends in tobacco use vary between nations and age groups, but in general the number of people in developed nations who smoke has declined steadily over the last few decades2. This decline appears to be slower for younger women than other groups3, and importantly, women who smoke do not necessarily quit if they become pregnant4,5.
It is estimated that 5.5 to 7% of Swedish women currently smoke in early pregnancy, while approximately 25% smoke prior to pregnancy6,7. The number is much higher for teenage mothers in Sweden, of whom one in four smoke during pregnancy7. In New Zealand in 2015, 14.2% of women reported smoking in early pregnancy8. However, the actual proportion of women who smoke during pregnancy in both Sweden and New Zealand is likely to be higher than these estimates based on self-report. When compared to biological markers of smoking, self-reports have significantly underestimated both the number of women who smoke during pregnancy and the number of cigarettes they smoke in these two countries9,10.
Smoking during pregnancy increases the risk of pregnancy complications, birth defects, and miscarriage1,11. It is associated with an increased risk of sudden death in early life12, lower birth weight13,14,15,16,17, poorer newborn lung function18, and increased risk of asthma in childhood19.
The newborns whose mothers smoked during pregnancy are usually reported to be proportionally smaller on average, i.e. they are shorter at birth as well as weighing less than other infants16,20,21. Children exposed to tobacco in utero may remain up to a centimeter shorter on average than their peers in childhood16,20,22, but other studies have not observed an effect on stature23,24. The British longitudinal National Child Development Study (NCDS) reported that women who smoked more than 20 cigarettes per day during pregnancy in 1958 had offspring who were more than a centimeter shorter in adulthood than those whose mothers did not smoke25.
Importantly, children born to mothers who smoked during pregnancy have an increased risk of being obese21,26,27,28,29,30. The association between maternal smoking in pregnancy and obesity in the offspring may persist into adulthood; the NCDS demonstrated that offspring of British women who were pregnant in 1958 had an increased risk of obesity throughout childhood and into adulthood if their mothers smoked during late pregnancy31. In a more recent cohort, Mattsson et al. described a dose-dependent effect of maternal cigarette smoking during early pregnancy on obesity risk in Swedish women32. However, that study did not control for maternal anthropometry, which is strongly associated with offspring anthropometry at birth33 and in adulthood34.
Due to the changing rates of both smoking and obesity, it cannot be assumed that results of the NCDS are applicable to a younger cohort, or to the offspring of women who smoked earlier in pregnancy. In addition, little is known about the long-term effects of light or moderate maternal smoking during pregnancy on adult height. Thus, in the present study we aimed the examine the association between maternal smoking and adult anthropometry (particularly on the risks of obesity and short stature) in a large cohort of women born to mothers who smoked early in pregnancy (first trimester) between 1973 and 1988 in Sweden, while also accounting for the effects of maternal anthropometry.
Methods
Ethics
Ethics approval was obtained from Uppsala’s Regional Ethical Review Board. This investigation was carried out in accordance with approved national and international guidelines for medical research. This is a register-based study on anonymized data where participants were not contacted; thus, informed consent was not required.
Study design
Data were extracted from the Swedish Birth Register, which records information on >99% of all births in Sweden, with a low error rate for key parameters when compared to the original medical records35. Data are prospectively recorded in pregnancy starting at the first antenatal visit and then forwarded to the Birth Register. In this study, the data recorded at the mother’s first antenatal visit were linked to the medical records on their daughter’s own subsequent first antenatal visit.
Our study covers from the first antenatal visit (mostly 10–12 weeks of gestation) on 303,301 women born in 1973–1988 in Sweden, who gave birth in 1991–2009 and were aged ≥18 years. Exclusion criteria were non-Nordic ethnicity; extremely short stature (≤130 cm); being born preterm (<37 weeks of gestation)36, post-term (≥42 weeks of gestation)37, or <−3 standard deviation scores (SDS) below the Swedish population mean for birth weight and/or birth length38; or having congenital malformations (ICD-9 740–759 and ICD-10 Q0–Q99).
Weight and height were measured, although height was self-reported in some cases. Gestational age at their birth (extracted from the Swedish Birth Register) was estimated from the date of the last menstrual period for the majority of participants, otherwise estimates were based on ultrasound scans. Overweight was defined as body mass index (BMI) ≥25 kg/m2 and <30 kg/m2, and obese as ≥30 kg/m2. Short stature was defined as height >2 SDS below the study population mean (<155 cm). Ponderal index (g/cm3) was calculated as per Röhrer’s formula [(100 x weight)/length].
Statistical analyses
Stratified analyses were carried out to examine differences in outcomes between daughters of smokers vs non-smokers, with the latter group also split into Light smokers (reported smoking between one and nine cigarettes per day) and Heavier smokers (10 or more cigarettes daily). Parameters at birth were compared between groups using univariable general linear regression models. Adult anthropometry, risk of obesity, and risk of short stature were examined with generalized linear regression models. The adjusted models included the following variables: birth order, age, and year of birth (to account for population-wide trends); in addition, models on daughter’s weight, BMI, and overweight/obesity risk adjusted for their current smoking habits, as well as their mothers’ weight or BMI; while the models on women’s stature were also adjusted for maternal height.
Binary outcomes are expressed as adjusted relative risks (aRR) and respective 95% confidence intervals. Analyses were performed in SAS v9.4 (SAS Institute, Cary, USA) and SPSS v24 (IBM Corp, Armonk, NY, USA). All tests were two-tailed, without adjustment for multiple comparisons.
Results
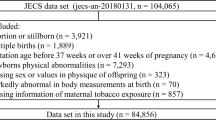
From the original sample of 303,301 women, 22,421 met the inclusion criteria and had recorded information on the mother’s BMI and smoking status during pregnancy; 9,311 mothers (41.5%) had reported they were smoking at their first antenatal visit (Fig. 1). From this group of women, 5,406 had mothers (24.1% overall) who had been Light smokers and 3,905 (17.4% overall) Heavier smokers during pregnancy. Of note, the demographic and anthropometric characteristics of the 22,421 women included in this study were similar to those who were excluded (Supplementary Table 1).
At birth
Women born to mothers who smoked in early pregnancy, on average, weighed 208 g less, were 8 mm shorter, and had a ponderal index that was 0.03 g/cm3 lower than those born of Non-smokers (Table 1). There was a dose-dependent relationship between maternal smoking level and the daughter’s weight and length at birth, with Heavier smokers giving birth to daughters 241 g lighter and 10 mm shorter than Non-smokers on average (Table 1).
Adult anthropometry
Women born to mothers who smoked were 1.1 cm shorter and 1.5 kg heavier on average in adulthood than those whose mothers did not smoke early in pregnancy, with an average BMI that was 0.84 kg/m2 higher (Table 2). There was a dose-dependent association with body mass (but not with height), so that women born to mothers who were Heavier smokers were 1.9 kg heavier and had a BMI that was 1.04 kg/m2 greater than the offspring of Non-smokers (Table 2).
The association between maternal smoking in early pregnancy and daughters’ heights in adulthood was slightly altered after adjustment for confounding factors, with evidence of a subtle dose-dependent relationship (Table 2). Women born to Light and Heavier smokers were 0.8 and 1.0 cm shorter, respectively, than those born to Non-smokers (Table 2).
In contrast, the possible effects of maternal smoking during pregnancy were accentuated for body mass (Table 2). Compared to daughters of mothers who did not smoke, those whose mothers were Light and Heavier smokers were 2.3 and 2.9 kg heavier, respectively, with BMI that was 0.84 and 1.15 kg/m2 greater (Table 2).
Risk of short stature
Rates of short stature were higher in daughters of smoking mothers, irrespective of smoking levels (Table 2). Women whose mothers smoked during pregnancy were 55% more likely to have short stature in adulthood (Table 3). However, unlike the obesity risk, the likelihood of short stature did not appear to be associated with the level of maternal smoking in early pregnancy (Table 3).
Obesity risk
A higher proportion of women whose mothers smoked during pregnancy were overweight and/or obese as adults than the daughters of Non-smokers (Table 2). Obesity rates increased with smoking levels, from 10.2% amongst daughters of Non-smokers to 13.9% and 16.9% in those born to Light and Heavier smokers, respectively (Table 2).
The adjusted relative risk (aRR) of obesity for women whose mothers smoked during pregnancy was 1.47 times higher than for daughters whose mothers were Non-smokers (Table 4). There was a dose-dependent association with obesity risk, which was 1.37 for women born to Light smokers and 1.61 for those born to Heavier smokers (Table 4).
Sensitivity analyses
Exploratory analyses were carried out without the exclusion of women who were born preterm or post-term. The associations between maternal smoking and anthropometric measurements on adult daughters were unchanged when compared to the findings for just those who were born at term (Supplementary Table 2). The risk of obesity in association with maternal smoking was also unchanged (Supplementary Table 3). However, in contrast to the findings on women born at term, there was some evidence of a dose-dependent effect of maternal smoking on their daughters’ stature, with the adjusted relative risk increasing from 1.48 in those born to Light smokers to 1.63 among daughters of Heavier smokers (Supplementary Table 3).
Of note, our data suggest that the association with a risk of obesity in adulthood was stronger with maternal smoking than with the daughters’ current smoking habits (Supplementary Table 4). Further, there was also evidence that maternal smoking was an important factor for the development of a smoking habit in their daughters [aRR 1.43 (95% CI 1.38, 1.47); p < 0.0001].
Discussion
Our study showed that maternal smoking in early pregnancy was associated with increased risk of short stature (+55%) in the adult daughters and a marked dose-dependent relationship with obesity risk. Women whose mothers smoked in early pregnancy were approximately 1 cm shorter, while daughters born to Heavier smokers (≥10 cigarettes per day) were on average 2.9 kg heavier with an adjusted relative risk of obesity that was 61% higher. In addition, consistent with previous research, women in our study whose mothers smoked during early pregnancy were lighter and shorter at birth than offspring of non-smokers.
This is the first study to report the long-term associations between smoking in early pregnancy and adult height, and one of few to investigate associations between maternal smoking at any stage of pregnancy with long-term outcomes. Similarly to our findings for mothers who smoked in early pregnancy, the smaller 1958 National Child Development Study (NCDS) reported an increased risk of obesity in adulthood for men and women (44% for the latter) whose mothers smoked beyond the fourth month of pregnancy, after controlling for maternal and environmental factors31. Previously, Mattsson et al. showed a very similar dose-dependent association between cigarette smoking in early pregnancy and offspring obesity risk in Swedish women32. Our study has strengthened those findings, as we have confirmed that the association between maternal smoking during pregnancy with an increased risk of obesity in the adult offspring not only remains after adjustment for maternal anthropometry, but that the apparent effects on weight and BMI become more pronounced. In addition, we also showed a novel association between maternal smoking during pregnancy and an increased risk of short stature in the offspring, irrespective of smoking levels.
Longitudinal studies suggest that the risk of obesity in children born to mothers who smoked during pregnancy increases as they get older13,15,26. The results of our study confirm previous research reporting that the increased risk of obesity for offspring of women who smoke while pregnant persists into adulthood31,32, although the relationship may not be as strong as in childhood. Children whose mothers smoked during pregnancy are typically estimated to be between 1.7 and 3.4 times more likely to be obese than other children15,21,28,29,30, including studies where smoking status was assessed early in pregnancy15,21. In comparison, maternal overweight and obesity have been estimated to increase the odds of offspring obesity in adulthood more than two-fold39. Due to the complex combination of shared genetic and environmental influences involved in this relationship, little is known about whether interventions focused on maternal weight loss are effective in reducing the obesity risk for offspring39,40. However, there is some evidence that smoking cessation during pregnancy can reduce the risk of low infant birthweight14 and subsequent obesity risk31.
No studies of adult outcomes have compared maternal smoking in early pregnancy vs late in pregnancy, but a German study reported that the risk of childhood obesity may be similar between offspring of women who quit smoking early in pregnancy and those whose mothers continued smoking throughout pregnancy27. In contrast, it seems that the relationship between maternal smoking and lower birthweight appears to be strongest when smoking continues into the third trimester41, the time when most fetal growth occurs. In our study, we were not able to identify the mothers who smoked throughout pregnancy and those who smoked only in early pregnancy. Nonetheless, the similarity of our results to the NCDS suggest that smoking in early pregnancy (irrespective of continuous smoking further into pregnancy) influences the future obesity risk of the offspring.
To our knowledge, the NCDS study is the only other to have examined the association between maternal smoking in pregnancy and adult height25. Consistent with our findings, women in the NCDS whose mothers had smoked during pregnancy were approximately 1 cm shorter than those born to non-smokers25. However, this association was observed only for very heavy smokers (smoking more than 20 cigarettes per day)25. Further, the association was no longer statistically significant after controlling for confounding factors25. Women born to both Light and Heavier smokers in our study had a markedly increased risk of short stature than offspring of non-smokers, and the relationships persisted after adjustment for confounding factors (including maternal anthropometry). Nonetheless, in contrast to our observations, studies on pre-pubertal children and teenagers have suggested a dose-dependent association between maternal smoking and stature, though the height differences between offspring of light smokers and heavy smokers was small (0.1 to 0.2 cm)22,42. Overall, the observed risk of short stature in association with maternal smoking during pregnancy is of similar magnitude (although slightly higher) to that observed in Swedish women born moderately preterm36. Further, we observed that average adult height in women born to Heavier smokers was 1 cm shorter than the offspring of non-smokers, while in comparison, women who were born during the Chinese Famine (1959–1961) were 1.7 cm shorter as adults43.
Although the mean difference in height between daughters of smokers and non-smokers was small at the individual level in comparison to other determinants of adult height, we reported an increased risk of short stature for daughters whose mothers smoked in early pregnancy. Shorter stature has been related to poorer social outcomes, such as a reduced likelihood of obtaining tertiary educational qualifications and increased suicide risk44,45. Height is also associated with many markers of cardiovascular health, with shorter stature relating to greater non-HDL cholesterol and triglycerides46, higher systolic and diastolic blood pressure46,47, as well as an increased risk of coronary artery disease46,48,49 and stroke49. The relationship between height and cardiovascular risk factors appears to be linear, with the greatest risk among the shortest members of society50. Although some health outcomes (such as lung function) can be directly affected by shorter height due to mechanical constraints46, it is unclear whether short stature itself is disadvantageous for cardiovascular health or is simply a marker of early growth and development.
Smoking during pregnancy has consistently been associated with decreased growth in utero. On average, mothers who smoke have infants with lower birth weight than those born to non-smokers13,14,15,16,17. This relationship seems to be explained in part by a reduction in insulin-like growth factor 1 (IGF-1, a key driver of fetal growth) levels, as observed in cord blood of fetuses exposed to maternal tobacco smoking17. In general, IGF-1 concentrations are influenced by placental nutrient supply, and the nicotine and carbon monoxide exposure associated with smoking during pregnancy reduce both the blood flow to the fetus and its oxygen content51.
Although children born to mothers who smoked during pregnancy are usually smaller13,14,15,16,17, they tend to experience a period of rapid growth post-natally15,16, and are likely to catch up to their peers in height and weight as early as within the first 12 months of life52. Following this catch-up period, children of mothers who smoked during pregnancy continue to grow at a faster rate than their peers, with proportionally higher increases in fat mass15. This pattern of growth is common to other populations of infants with low birthweight53,54. Catch-up growth is thought to provide benefits in the short term, but poses risks to health in the long term54.
By five years of age, children born to smokers are around twice as likely to be obese compared to the offspring of non-smoking mothers21,26,27,28,29,30. This later weight gain is thought to be a result of fetal programming, where the fetus has adapted to poor nutrient supply in utero, resulting in permanent changes to metabolism that are maladaptive later in life55. A high BMI following low birth weight has been associated with more health risks than a high BMI with high birth weight56. Thus, the apparent effects of maternal smoking on fetal and infant growth could be underpinning the adverse long-term associations we and others have observed.
Of note, several recent studies have explored the role of epigenetics as a pathway by which maternal smoking in pregnancy affects the future health of their offspring. A number of studies have compared the offspring of mothers who did or did not smoke during pregnancy, and cord or newborn heel-prick blood revealed differential methylation of genes known to be involved in the response to tobacco-related compounds57,58, embryonic and fetal development58,59, and immune system function58,60. At least one study has reported that differential methylation of specific genes partially mediates the relationship between maternal smoking in pregnancy and their offspring’s birth weight60. However, there is still much to be learnt about how epigenetics may influence the effects of maternal smoking on offspring health. For example, a meta-analysis identified nearly 3000 sites corresponding to genes whose expression in newborns appeared to be affected by maternal smoking during pregnancy57.
Our study has some limitations. Data about smoking status was not consistently collected when the participants’ mothers were pregnant, so our sample was not randomly selected and cannot be assumed to be the prevalence of smoking during pregnancy at the time. Importantly, smoking data were not collected later in pregnancy beyond the first antenatal visit, so it is not known how many mothers continued to smoke throughout pregnancy, nor can we compare the effects of smoking throughout pregnancy with early pregnancy alone. A Swedish study on women who were pregnant on 1988 (overlapping with the time when mothers of our participants were pregnant) reported that only 18% of smokers quit prior to their first antenatal visit, with 65% of women continuing to smoke throughout pregnancy4. Based on this information and the similarity of our findings to those reported by the NCDS (where smoking status was assessed later in pregnancy), it is likely that the majority of mothers in our study who were smoking at the first antenatal visit continued to smoke throughout pregnancy. Anthropometry of the daughters in our study was also assessed in early pregnancy. While data based on self-reported pre-pregnancy weight indicated that women gained an average of 4 kg in the first 16 weeks of pregnancy61, there is no evidence to suggest that early pregnancy weight gain would differ between women whose mothers smoked during pregnancy and those whose mothers were non-smokers. Therefore, this previously observed weight gain is unlikely to affect the associations between maternal smoking and daughter’s obesity risk described in our study. However, the mean weight and BMI data reported here might have overestimated the obesity risk for some women in both groups. Lastly, we did not have data on maternal second-hand smoking during pregnancy, socioeconomic status, or lifestyle factors (e.g. diet and physical activity) that could have affected our results.
However, our study has important strengths. We studied a large and relatively homogenous cohort of Nordic women. In addition, we have not only accounted for the important confounding effects of maternal anthropometry in our statistical models, but we have also excluded important groups with an increased risk of short stature such as women born preterm36 or those of extremely low birth weight62.
Overall, our results emphasize the importance of early intervention for women who smoke to reduce the long-term health risks to their offspring. We showed that smoking in early pregnancy was associated with an increased risk of obesity and short stature in adult life. Although current rates of maternal smoking have decreased markedly since our participants were born, there remains a high prevalence of smoking amongst teenage mothers (e.g. 1 in 4 in Sweden7 and 1 in 3 in New Zealand8). Furthermore, there is also some evidence that women who smoke during pregnancy underestimate the risk to their fetus from cigarette smoking, particularly if they have fewer years of education63,64. Unplanned or unwanted pregnancies are both associated with a higher likelihood of maternal smoking65, and our findings indicate that the offspring are at risk for adverse health outcomes of maternal smoking at any time during pregnancy. As such, smoking cessation messages should target in particular younger women who may become pregnant, and medical providers should be unequivocal in expressing the risks of smoking during pregnancy for offspring health.
Data Availability
Data used in this study were obtained from the Swedish Medical Birth Register. While these data cannot be made publicly available, they can be accessed upon request to the Swedish National Board of Health and Welfare, pending approval by the appropriate ethics committee. Information on the Birth Register and persons to contact for queries regarding access are available in English from: www.socialstyrelsen.se/register/halsodataregister/medicinskafodelseregistret/inenglish.
References
Hackshaw, A., Rodeck, C. & Boniface, S. Maternal smoking in pregnancy and birth defects: a systematic review based on 173 687 malformed cases and 11.7 million controls. Hum Reprod Update 17, 589–604, https://doi.org/10.1093/humupd/dmr022 (2011).
World Health Organisation. WHO global report on trends in prevalence of tobacco smoking 2015. (World Health Organisation, Geneva, Switzerland, 2015).
Orleans, C. T., Barker, D. C., Kaufman, N. J. & Marx, J. F. Helping pregnant smokers quit: meeting the challenge in the next decade. Tob Control 9(Suppl III), iii6–iii11, https://doi.org/10.1136/tc.9.suppl_3.iii6 (2000).
Cnattingius, S., Lindmark, G. & Meirik, O. Who continues to smoke while pregnant. J Epidemiol Community Health 46, 218–221, https://doi.org/10.1136/jech.46.3.218 (1992).
Gilbert, N. L., Nelson, C. R. M. & Greaves, L. Smoking cessation during pregnancy and relapse after childbirth in Canada. J Obstetr Gynaecol Canada 37, 32–39, https://doi.org/10.1016/S1701-2163(15)30360-1 (2015).
Reitan, T. & Callinan, S. Changes in smoking rates among pregnant women and the general female population in Australia, Finland, Norway and Sweden. Nicotine Tob Res 19, 282–289, https://doi.org/10.1093/ntr/ntw188 (2017).
Ekblad, M., Gissler, M., Korkeilia, J. & Lehtonen, L. Trends and risk groups for smoking during pregnancy in Finland and other Nordic countries. Eur J Public Health 24, 544–551, https://doi.org/10.1093/eurpub/ckt128 (2014).
Ministry of Health. Report on Maternity 2015. (Ministry of Health, Wellingto, 2017).
Lindqvist, R., Lendahls, L., Tollbom, Ö., ÅBerg, H. & Håkansson, A. Smoking during pregnancy: comparison of self-reports and cotinine levels in 496 women. Acta Obstet Gynaecol Scand 81, 240–244, https://doi.org/10.1034/j.1600-0412.2002.810309.x (2002).
Ford, R. P., Tappin, D. M., Schluter, P. J. & Wild, C. J. Smoking during pregnancy: how reliable are maternal self reports in New Zealand? J Epidemiol Community Health 51, 246–251, https://doi.org/10.1136/jech.51.3.246 (1997).
Castles, A., Adams, E. K., Melvin, C. L., Kelsch, C. & Boulton, M. L. Effects of smoking during pregnancy: five meta-analyses. Am J Prev Med 16, 208–215, https://doi.org/10.1016/S0749-3797(98)00089-0 (1999).
Fleming, P. & Blair, P. S. Sudden infant death syndrome and parental smoking. Early Hum Dev 83, 721–725, https://doi.org/10.1016/j.earlhumdev.2007.07.011 (2007).
Suzuki, K. et al. Gender differences in the association between maternal smoking during pregnancy and childhood growth trajectories: multilevel analysis. Int J Obes 35, 53–59, https://doi.org/10.1038/ijo.2010.198 (2011).
Sexton, M. & Hebel, J. A clinical trial of change in maternal smoking and its effect on birth weight. JAMA 251, 911–915, https://doi.org/10.1001/jama.1984.03340310025013 (1984).
Timmermans, S. H. et al. Maternal smoking during pregnancy and childhood overweight and fat distribution: the KOALA birth cohort study. Pediatr Obes 9, e14–e25, https://doi.org/10.1111/j.2047-6310.2012.00141.x (2014).
Vik, T., Jacobsen, G., Vatten, L. & Bakketeig, L. S. Pre- and post-natal growth in children of women who smoked in pregnancy. Early Hum Dev 45, 245–255, https://doi.org/10.1016/0378-3782(96)01735-5 (1996).
Fleisch, A. F. et al. Associations of maternal prenatal smoking with umbilical cord blood hormones: the Project Viva cohort. Metabolism 72, 18–26, https://doi.org/10.1016/j.metabol.2017.04.001 (2017).
Hanrahan, J. P. et al. The effect of maternal smoking during pregnancy on early infant lung function. Am Rev Respir Dis 145, 1129–1135, https://doi.org/10.1164/ajrccm/145.5.1129 (1992).
Gilliland, F. D., Li, Y.-F. & Peters, J. M. Effects of maternal smoking during pregnancy and environmental tobacco smoke on asthma and wheezing in children. Am J Respir Crit Care Med 163, 429–436, https://doi.org/10.1164/ajrccm.163.2.2006009 (2001).
Howe, L. D. et al. Maternal smoking during pregnancy and offspring trajectories of height and adiposity: comparing maternal and paternal associations. Int J Epidemiol 41, 722–732, https://doi.org/10.1093/ije/dys025 (2012).
Widerøe, M., Torstein, V., Jacobsen, G. W. & Bakketeig, L. S. Does maternal smoking during pregnancy cause childhood overweight? Paediatr Perinat Epidemiol 17, 171–179, https://doi.org/10.1046/j.1365-3016.2003.00481.x (2003).
Leary, S., Smith, G. D. & Ness, A. & Alspac Study Team. Smoking during pregnancy and components of stature in offspring. Am J Hum Biol 18, 502–512, https://doi.org/10.1002/ajhb.20518 (2006).
Fried, P. A., James, D. S. & Watkinson, B. Growth and pubertal milestones during adolescence in offspring prenatally exposed to cigarettes and marihuana. Neurotoxicol Teratol 23, 431–436, https://doi.org/10.1016/S0892-0362(01)00161-1 (2001).
Oken, E., Huh, S. Y., Taveras, E. M., Rich-Edwards, J. W. & Gillman, M. W. Associations of maternal prenatal smoking with child adiposity and blood pressure. Obes Res 13, 2021–2028, https://doi.org/10.1038/oby.2005.248 (2005).
Fogelman, K. R. & Manor, O. Smoking in pregnancy and development into early adulthood. BMJ 297, 1233–1236, https://doi.org/10.1136/bmj.297.6658.1233 (1988).
Riedel, C. et al. Differences in BMI z-scores between offspring of smoking and nonsmoking mothers: A longitudinal study of German children from birth through 14 years of age. Environ Health Perspect 122, 761–767, https://doi.org/10.1289/ehp.1307139 (2014).
Toschke, A. M., Montgomery, S. M., Pfeiffer, U. & von Kries, R. Early intrauterine exposure to tobacco-inhaled products and obesity. Am J Epidemiol 158, 1068–1074, https://doi.org/10.1093/aje/kwg258 (2003).
Toschke, A. M., Koletzko, B., Slikker, W. Jr., Hermann, M. & von Kries, R. Childhood obesity is associated with maternal smoking in pregnancy. Eur J Pediatr 161, 445–448, https://doi.org/10.1007/s00431-002-0983-z (2002).
Aucott, L., Bhattacharya, S., McNeill, G. & Turner, S. Differences in body mass index between siblings who are discordant for exposure to antenatal maternal smoking. Paediatr Perinat Epidemiol 31, 402–408, https://doi.org/10.1111/ppe.12386 (2017).
Mizutani, T., Suzuki, K., Kondo, N. & Yamagata, Z. Association of maternal lifestyles including smoking during pregnancy with childhood obesity. Obesity 15, 3133–3139, https://doi.org/10.1038/oby.2007.373 (2007).
Power, C. & Jefferis, B. J. Fetal environment and subsequent obesity: a study of maternal smoking. Int J Epidemiol 31, 413–419, https://doi.org/10.1093/ije/31.2.413 (2001).
Mattsson, K., Källén, K., Longnecker, M. P., Rignell-Hydbom, A. & Rylander, L. Maternal smoking during pregnancy and daughters’ risk of gestational diabetes and obesity. Diabetologia 56, 1689–1695, https://doi.org/10.1007/s00125-013-2936-7 (2013).
Pomeroy, E., Wells, J. C. K., Cole, T. J., O’Callaghan, M. & Stock, J. T. Relationships of maternal and paternal anthropometry with neonatal body size, proportions and adiposity in an Australian cohort. Am J Phys Anthropol 156, 625–636, https://doi.org/10.1002/ajpa.22680 (2015).
Tequeanes, A. L., Gigante, D. P., Assunção, M. C., Chica, D. A. & Horta, B. L. Maternal anthropometry is associated with the body mass index and waist:height ratio of offspring at 23 years of age. J Nutr 139, 750–754, https://doi.org/10.3945/jn.108.100669 (2009).
Cnattingius, S., Ericson, A., Gunnarskog, J. & Källén, B. A quality study of a medical birth registry. Scand J Soc Med 18, 143–148, https://doi.org/10.1177/140349489001800209 (1990).
Derraik, J. G. B., Lundgren, M., Cutfield, W. S. & Ahlsson, F. Association between preterm birth and lower adult height in women. Am J Epidemiol 185, 48–53, https://doi.org/10.1093/aje/kww116 (2017).
Derraik, J. G. B., Lundgren, M., Cutfield, W. S. & Ahlsson, F. Body mass index, overweight, and obesity in Swedish women born post-term. Paediatr Perinat Epidemiol 30, 320–324, https://doi.org/10.1111/ppe.12292 (2016).
Niklasson, A. et al. An update of the Swedish reference standards for weight, length and head circumference at birth for given gestational age (1977–1981). Acta Paediatr Scand 80, 756–762, https://doi.org/10.1111/j.1651-2227.1991.tb11945.x (1991).
Zalbahar, N., Najman, J., McIntrye, H. D. & Mamun, A. Parental pre-pregnancy BMI influences on offspring BMI and waist circumference at 21 years. Aust NZ J Public Health 40, 572–578, https://doi.org/10.1111/1753-6405.12574 (2016).
Williams, C. B., Mackenzie, K. C. & Gahagan, S. The effect of maternal obesity on the offspring. Clin Obstet Gynecol 57, 508–515, https://doi.org/10.1097/grf.0000000000000043 (2014).
Yan, J. & Groothuis, P. A. Timing of prenatal smoking cessation or reduction and infant birth weight: evidence from the United Kingdom Millennium Cohort Study. Matern Child Health J 19, 447–458, https://doi.org/10.1007/s10995-014-1516-x (2015).
Rantakallio, P. A follow-up study to the age of 14 of children whose mothers smoked during pregnancy. Acta Pediatr Scand 72, 747–753, https://doi.org/10.1111/j.1651-2227.1983.tb09805.x (1983).
Huang, C., Li, Z., Wang, M. & Martorell, R. Early life exposure to the 1959–1961 Chinese famine has long-term health consequences. J Nutr 140, 1874–1878, https://doi.org/10.3945/jn.110.121293 (2010).
Magnusson, P. K., Gunnell, D., Tynelius, P., Davey Smith, G. & Rasmussen, F. Strong inverse association between height and suicide in a large cohort of Swedish men: evidence of early life origins of suicidal behavior? Am J Psychiatry 162, 1373–1375, https://doi.org/10.1176/appi.ajp.162.7.1373 (2005).
Magnusson, P. K., Rasmussen, F. & Gyllensten, U. B. Height at age 18 years is a strong predictor of attained education later in life: cohort study of over 950,000 Swedish men. Int J Epidemiol 35, 658–663, https://doi.org/10.1093/ije/dyl011 (2006).
Nüesch, E. et al. Adult height, coronary heart disease and stroke: a multi-locus Mendelian randomization meta-analysis. Int J Epidemiol 45, 1927–1937, https://doi.org/10.1093/ije/dyv074 (2016).
Bourgeois, B. et al. Associations between height and blood pressure in the United States population. Medicine 96, e9233, https://doi.org/10.1097/md.0000000000009233 (2017).
Lawlor, D. A., Taylor, M., Davey Smith, G., Gunnell, D. & Ebrahim, S. Associations of components of adult height with coronary heart disease in postmenopausal women: the British women’s heart and health study. Heart 90, 745–749, https://doi.org/10.1136/hrt.2003.019950 (2004).
Silventoinen, K., Magnusson, P. K., Tynelius, P., Batty, G. D. & Rasmussen, F. Association of body size and muscle strength with incidence of coronary heart disease and cerebrovascular diseases: a population-based cohort study of one million Swedish men. Int J Epidemiol 38, 110–118, https://doi.org/10.1093/ije/dyn231 (2009).
Wannamethee, S. G., Shaper, A. G., Whincup, P. H. & Walker, M. Adult height, stroke, and coronary heart disease. Am J Epidemiol 148, 1069–1076, https://doi.org/10.1093/oxfordjournals.aje.a009584 (1998).
Lambers, D. S. & Clark, K. E. The maternal and fetal physiologic effects of nicotine. Semin Perinatol 20, 115–126, https://doi.org/10.1016/S0146-0005(96)80079-6 (1996).
Ong, K. K., Preece, M. A., Emmett, P. M., Ahmed, M. L. & Dunger, D. B. Size at birth and early childhood growth in relation to maternal smoking, parity and infant breast-feeding: longitudinal birth cohort study and analysis. Pediatr Res 52, 863–867, https://doi.org/10.1203/01.PDR.0000036602.81878.6D (2002).
Jain, V. & Singhal, A. Catch up growth in low birth weight infants: striking a healthy balance. Rev Endocr Metab Disord 13, 141–147, https://doi.org/10.1007/s11154-012-9216-6 (2012).
Martin, A., Connelly, A., Bland, R. M. & Reilly, J. R. Health impact of catch-up growth in low-birth weight infants: systematic review, evidence appraisal, and meta-analysis. Matern Child Nutr 13, https://doi.org/10.1111/mcn.12297 (2017).
Godfrey, K. M. & Barker, D. J. P. Fetal programming and adult health. Public Health Nutr 4, 611–624, https://doi.org/10.1079/PHN2001145 (2001).
Kensara, O. A. et al. Fetal programming of body composition: relation between birth weight and body composition measured with dual-energy X-ray absorptiometry and anthropometric methods in older Englishmen. Am J Clin Nutr 82, 980–987, https://doi.org/10.1093/ajcn/82.5.980 (2005).
Joubert, B. R. et al. DNA methylation in newborns and maternal smoking in pregnancy: Genome-wide consortium meta-analysis. Am J Hum Genet 98, 680–696, https://doi.org/10.1016/j.ajhg.2016.02.019 (2016).
Joubert, B. R. et al. 450 K epigenome-wide scan identifies differential DNA methylation in newborns related to maternal smoking during pregnancy. Environ Health Perspect 120, 1425–1431, https://doi.org/10.1289/ehp.1205412 (2012).
Markunas, C. A. et al. Identification of DNA methylation changes in newborns related to maternal smoking during pregnancy. Environ Health Perspect 122, 1147–1153, https://doi.org/10.1289/ehp.1307892 (2014).
Küpers, L. K. et al. DNA methylation mediates the effect of maternal smoking during pregnancy on birthweight of the offspring. Int J Epidemiol 44, 1224–1237, https://doi.org/10.1093/ije/dyv048 (2015).
de Jersey, S. J., Nicholson, J. M., Callaway, L. K. & Daniels, L. A. A prospective study of pregnancy weight gain in Australian women. Aust NZ J Obstet Gynaecol 52, 545–551, https://doi.org/10.1111/ajo.12013 (2012).
Lundgren, E. M., Cnattingius, S., Jonsson, B. & Tuvemo, T. Prediction of adult height and risk of overweight in females born small-for-gestational-age. Paediatr Perinat Epidemiol 17, 156–163, https://doi.org/10.1046/j.1365-3016.2003.00489.x (2003).
Fingerhut, L. A., Kleinman, J. C. & Kendrick, J. S. Smoking before, during, and after pregnancy. Am J Public Health 80, 541–544, https://doi.org/10.2105/AJPH.80.5.541 (1990).
Cui, Y., Shooshtari, S., Forget, E. L., Clara, I. & Cheung, K. F. Smoking during pregnancy: findings from the 2009–2010 Canadian Community Health Survey. PLoS ONE 9, e84640, https://doi.org/10.1371/journal.pone.0084640 (2014).
Flower, A., Shawe, J., Stephenson, J. & Doyle, P. Pregnancy planning, smoking behaviour during pregnancy, and neonatal outcome: UK millennium cohort study. BMC Pregnancy Childbirth 13, 238, https://doi.org/10.1186/1471-2393-13-238 (2013).
Author information
Authors and Affiliations
Contributions
J.G.B.D., F.A., M.L., W.S.C. and conceived and designed the study. J.G.B.D. analyzed the data; S.M. and J.G.B.D. wrote the paper with critical input from M.L., F.A. and W.S.C.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maessen, S.E., Ahlsson, F., Lundgren, M. et al. Maternal smoking early in pregnancy is associated with increased risk of short stature and obesity in adult daughters. Sci Rep 9, 4290 (2019). https://doi.org/10.1038/s41598-019-39006-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39006-7
This article is cited by
-
Trends and burden of diabetes in pregnancy among Aboriginal and non-Aboriginal mothers in Western Australia, 1998–2015
BMC Public Health (2022)
-
Cardio-Obstetrics: the Next Frontier in Cardiovascular Disease Prevention
Current Atherosclerosis Reports (2022)
-
Large-for-gestational-age phenotypes and obesity risk in adulthood: a study of 195,936 women
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.