Abstract
Background
Maternal smoking (MS) is associated with low birthweight (BW) but adult obesity in offspring, however, it remains unknown whether it modifies offspring’s genetic susceptibility to obesity on BW, adult body weight, and birth-to-adulthood body weight tracking pattern.
Methods
This study included 246,759 UK Biobank participants with information on MS, BW (kg), adult body weight and BMI (kg/m2). Individual polygenetic score (PGS) was created on the basis of 97 BMI-associated genetic loci. We calculated individual birth-to-adulthood percentile change, and body weight tracking patterns that combined BW levels (<2.5, 2.5–4.0, and ≥4.0 as low, normal and high BW [LBW, NBW, and HBW]) and adulthood obesity status (≥30 as obesity [OB] and <30 as non-obesity [NOB]), including LBW-to-OB, LBW-to-NOB, NBW-to-OB, NBW-to-NOB, HBW-to-OB, and HBW-to-NOB.
Results
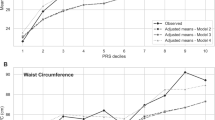
Participants exposed to MS had a 0.108 kg lower BW (95% CI, −0.114 to −0.102), a 1.418 kg higher adult body weight (95% CI, 1.291–1.545), and a 6.91 greater percentile increase of body weight from birth to adulthood (95% CI, 6.62–7.21), compared with those nonexposed (all P < 0.001). In comparison to participants of NBW-to-NOB, MS was associated with an approximately twofold higher risk of LBW-to-OB (odds ratio [OR] 1.98, 95% CI 1.87–2.10), and a reduced likelihood of HBW-to-NOB (0.85, 95% CI 0.82–0.88). The increases in BW, adult body weight, and birth-to-adulthood percentile change per increment of 10 BMI-PGS were 0.021 vs. 0.012, 2.50 vs. 2.11, and 4.03 vs. 3.55, respectively, for participants exposed vs. nonexposed to MS (all Pinteraction < 0.05).
Conclusion
Our results indicate that exposure to MS is associated with an increased risk of transition from low BW-to-adulthood obesity, and reduced likelihood of change from high BW-to-normal adult body weight. MS may modify the relation of genetic susceptibility to obesity and body weight in offspring.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Somm E, Schwitzgebel VM, Vauthay DM, Aubert ML, Hüppi PS. Prenatal nicotine exposure and the programming of metabolic and cardiovascular disorders. Mol Cell Endocrinol. 2009;304:69–77.
Jaddoe VWV, de Jonge LL, van Dam RM, Willett WC, Harris H, Stampfer MJ, et al. Fetal exposure to parental smoking and the risk of type 2 diabetes in adult women. Diabetes Care. 2014;37:2966–73.
Lawlor DA, Najman JM, Sterne J, Williams GM, Ebrahim S, Davey Smith G. Associations of parental, birth, and early life characteristics with systolic blood pressure at 5 years of age: findings from the Mater-University study of pregnancy and its outcomes. Circulation. 2004;110:2417–23.
Power C, Atherton K, Thomas C. Maternal smoking in pregnancy, adult adiposity and other risk factors for cardiovascular disease. Atherosclerosis. 2010;211:643–8.
Pereira PP, da S, Da Mata FAF, Figueiredo ACG, de Andrade KRC, Pereira MG. Maternal active smoking during pregnancy and low birth weight in the americas: a systematic review and meta-analysis. Nicotine Tob Res. 2017;19:497–505.
Salmasi G, Grady R, Jones J, McDonald SD. Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89:423–41.
Leonardi-Bee J, Smyth A, Britton J, Coleman T. Environmental tobacco smoke and fetal health: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2008;93. https://doi.org/10.1136/adc.2007.133553.
Riedel C, Schönberger K, Yang S, Koshy G, Chen YC, Gopinath B. et al. Parental smoking and childhood obesity: Higher effect estimates for maternal smoking in pregnancy compared with paternal smoking-a meta-analysis. Int J Epidemiol. 2014;43:1593–06.
Oken E, Levitan EB, Gillman MW. Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis. Int J Obes. 2008;32:201–10.
Rayfield S, Plugge E. Systematic review and meta-analysis of the association between maternal smoking in pregnancy and childhood overweight and obesity. J Epidemiol Community Health. 2017;71:162–73.
Oken E, Gillman MW. Fetal origins of obesity. Obes Res. 2003;11:496–506.
Inadera H. Developmental origins of obesity and type 2 diabetes: molecular aspects and role of chemicals. Environ Health Prev Med. 2013;18:185–97.
Breier BH, Vickers MH, Ikenasio BA, Chan KY, Wong WPS. Fetal programming of appetite and obesity. Mol Cell Endocrinol. 2001;185:73–9.
Vickers MH, Breier BH, Cutfield WS, Hofman PL, Gluckman PD. Fetal origins of hyperphagia, obesity, and hypertension and postnatal amplification by hypercaloric nutrition. Am J Physiol Endocrinol Metab. 2000;279:E83–7.
Frankel S, Elwood P, Sweetnam P, Yarnell J, Smith GD, Sweetnam P, et al. Birthweight, body-mass index in middle age, and incident coronary heart disease. Lancet (London, England). 1996;348:1478–80.
Osler M, Lund R, Kriegbaum M, Andersen A-MN. The influence of birth weight and body mass in early adulthood on early coronary heart disease risk among Danish men born in 1953. Eur J Epidemiol. 2009;24:57–61.
Bjerregaard LG, Jensen BW, Ängquist L, Osler M, Sørensen TIA, Baker JL. Change in overweight from childhood to early adulthood and risk of type 2 diabetes. N Engl J Med. 2018;378:1302–12.
Wang T, Huang T, Kang JH, Zheng Y, Jensen MK, Wiggs JL, et al. Habitual coffee consumption and genetic predisposition to obesity: gene-diet interaction analyses in three US prospective studies. BMC Med. 2017;15:97.
Wang T, Heianza Y, Sun D, Huang T, Ma W, Rimm EB, et al. Improving adherence to healthy dietary patterns, genetic risk, and long term weight gain: gene-diet interaction analysis in two prospective cohort studies. BMJ. 2018;360:j5644.
Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206.
World Health Organization. ICD-10: International statistical classification of diseases and related health problems: tenth revision. 2nd ed. Geneva: World Health Organization; 2004. http://www.who.int/iris/handle/10665/42980.
International Physical Activity Questionnaire. Guidelines for data processing and analysis of the international physical activity questionnaire (IPAQ)—short and long forms. Int Phys Act Quest. 2005:1–15. http://www.ipaq.ki.se/scoring.pdf.
Li P, Stuart EA, Allison DB. Multiple imputation: a flexible tool for handling missing data. J Am Med Assoc. 2015;314:1966–7.
Howe LD, Matijasevich A, Tilling K, Brion MJ, Leary SD, Smith GD, et al. Maternal smoking during pregnancy and offspring trajectories of height and adiposity: comparing maternal and paternal associations. Int J Epidemiol. 2012;41:722–32.
Harris HR, Willett WC, Michels KB. Parental smoking during pregnancy and risk of overweight and obesity in the daughter. Int J Obes. 2013;37:1356–63.
Power C, Li L, Manor O, Smith GD. Combination of low birth weight and high adult body mass index: at what age is it established and what are its determinants? J Epidemiol Community Heal. 2003;57:969–73.
Zhao Y, Wang S-F, Mu M, Sheng J. Birth weight and overweight/obesity in adults: a meta-analysis. Eur J Pediatr. 2012;171:1737–46.
Schellong K, Schulz S, Harder T, Plagemann A, King D, Mokdad A, et al. Birth weight and long-term overweight risk: systematic review and a meta-analysis including 643,902 persons from 66 studies and 26 countries globally. PLoS ONE. 2012;7:e47776.
Wadhwa PD, Buss C, Entringer S, Swanson JM, Wadhwa PD, Buss C, Entringer S, Swanson JM, Ph D. Developmental origins of health and disease: brief history of the approach and current focus on epigenetic mechanisms. Semin Reprod Med. 2009;27:358–68.
Ino T. Maternal smoking during pregnancy and offspring obesity: meta-analysis. Pediatr Int. 2010;52:94–9.
Huang JS, Lee TA, Lu MC. Prenatal programming of childhood overweight and obesity. Matern Child Health J. 2007;11:461–73.
Joubert BRR, Felix JFF, Yousefi P, Bakulski KMM, Just ACC, Breton C, et al. DNA methylation in newborns and maternal smoking in pregnancy: genome-wide consortium meta-analysis. Am J Hum Genet. 2016;98:680–96.
Richmond RC, Suderman M, Langdon R, Relton CL, Davey Smith G. DNA methylation as a marker for prenatal smoke exposure in adults. Int J Epidemiol. 2018;47:1120–1130.
Ong KKL, Ahmed ML, Emmett PM, Preece MA, Dunger DB. The avon longitudinal study of pregnancy and childhood study team. Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ. 2000;320:967–71.
Huang R-C, Burrows S, Mori TA, Oddy WH, Beilin LJ. Lifecourse adiposity and blood pressure between birth and 17 years old. Am J Hypertens. 2015;28:1056–63.
Lei X, Zhao D, Huang L, Luo Z, Zhang J, Yu X, et al. Childhood health outcomes in term, large-for-gestational-age babies with different postnatal growth patterns. Am J Epidemiol. 2018;187:507–14.
Gao YJ, Holloway AC, Zeng ZH, Lim GE, Petrik JJ, Foster WG, et al. Prenatal exposure to nicotine causes postnatal obesity and altered perivascular adipose tissue function. Obes Res. 2005;13:687–92.
Holloway AC, Lim GE, Petrik JJ, Foster WG, Morrison KM, Gerstein HC. Fetal and neonatal exposure to nicotine in Wistar rats results in increased beta cell apoptosis at birth and postnatal endocrine and metabolic changes associated with type 2 diabetes. Diabetologia. 2005;48:2661–6.
Somm E, Schwitzgebel VM, Vauthay DM, Camm EJ, Chen CY, Giacobino J-PP, et al. Prenatal nicotine exposure alters early pancreatic islet and adipose tissue development with consequences on the control of body weight and glucose metabolism later in life. Endocrinology. 2008;149:6289–99.
Wehby GL, Prater K, McCarthy AM, Castilla EE, Murray JC. The impact of maternal smoking during pregnancy on early child neurodevelopment. J Hum Cap. 2011;5:207–54.
Landau LI. Tobacco smoke exposure and tracking of lung function into adult life. Paediatr Respir Rev. 2008;9:39–44.
Lehn H, Derks EM, Hudziak JJ, Heutink P, Van Beijsterveldt TCEM, Boomsma DI. Attention problems and attention-deficit/hyperactivity disorder in discordant and concordant monozygotic twins: evidence of environmental mediators. J Am Acad Child Adolesc Psychiatry. 2007;46:83–91.
Berghuis SA, Van Braeckel KNJA, Sauer PJJ, Bos AF. Prenatal exposure to persistent organic pollutants and cognition and motor performance in adolescence. Environ Int. 2018;121:13–22.
Song M, Zheng Y, Qi L, Hu FB, Chan AT, Giovannucci EL. Longitudinal analysis of genetic susceptibility and BMI throughout adult life. Diabetes. 2018;67:248–55.
Walter S, Mejía-Guevara I, Estrada K, Liu SY, Glymour MM. Association of a genetic risk score with body mass index across different birth cohorts. J Am Med Assoc. 2016;316:63.
Godfrey KM. The role of the placenta in fetal programming—a review. Placenta. 2002;23:20–7.
Joubert BR, Håberg SE, Nilsen RM, Wang X, Vollset SE, Murphy SK, et al. 450K epigenome-wide scan identifies differential DNA methylation in newborns related to maternal smoking during pregnancy. Environ Health Perspect. 2012;120:1425–31.
Yousefi M, Karmaus W, Zhang H, Ewart S, Arshad H, Holloway JW. The methylation of the LEPR/LEPROT genotype at the promoter and body regions influence concentrations of leptin in girls and BMI at age 18 years if their mother smoked during pregnancy. Int J Mol Epidemiol Genet. 2013;4:86–100.
Bagot RC, Meaney MJ. Epigenetics and the biological basis of gene × environment interactions. J Am Acad Child Adolesc Psychiatry. 2010;49:752–771.
Simard JF, Rosner BA, Michels KB. Exposure to cigarette smoke in utero comparison of reports from mother and daughter. Epidemiology. 2008;19:628–33.
Lange S, Probst C, Rehm J, Popova S. National, regional, and global prevalence of smoking during pregnancy in the general population: a systematic review and meta-analysis. Lancet Glob Health. 2018;6:e769–76.
Cooper S, Orton S, Leonardi-Bee J, Brotherton E, Vanderbloemen L, Bowker K, et al. Smoking and quit attempts during pregnancy and postpartum: a longitudinal UK cohort. BMJ Open. 2017;7:1–12.
Scheffers-Van Schayck T, Tuithof M, Otten R, Engels R, Kleinjan M. Smoking behavior of women before, during, and after pregnancy: indicators of smoking, quitting, and relapse. Eur Addict Res. 2019;25:132–44.
Troy LM, Hunter DJ, Manson JE, Colditz GA, Stampfer MJ, Willett WC, et al. Self-reported birthweight and history of having been breastfed among younger women: an assessment of validity. Int J Epidemiol. 1996;25:122–7.
Nilsen TS, Kutschke J, Brandt I, Harris JR. Validity of self-reported birth weight: results from a Norwegian twin sample. Twin Res Hum Genet. 2017;20:406–13.
Horikoshi M, Beaumont RN, Day FR, Warrington NM, Kooijman MN, Fernandez-Tajes J, et al. Genome-wide associations for birth weight and correlations with adult disease. Nature. 2016;538:248–52.
Wang Y, Min J, Khuri J, Li M. A systematic examination of the association between parental and child obesity across countries. Adv Nutr An Int Rev J. 2017;8:436–48.
Lieb DC, Snow RE, DeBoer MD. Socioeconomic factors in the development of childhood obesity and diabetes. Clin Sports Med. 2009;28:349–78.
Parsons TJ, Manor O, Power C. Physical activity and change in body mass index from adolescence to mid-adulthood in the 1958 British cohort. Int J Epidemiol. 2006;35:197–204.
Agostoni C, Braegger C, Decsi T, Kolacek S, Koletzko B, Mihatsch W, et al. Role of dietary factors and food habits in the development of childhood obesity: a commentary by the espghan committee on nutrition. J Pediatr Gastroenterol Nutr. 2011;52:662–9.
Acknowledgements
The authors thank the participants, the members, the project development and management teams in the present study in the UK Biobank. This research has been conducted using the UK Biobank Resource, approved project number 29256.
Funding
This study is supported by grants from the National Heart, Lung, and Blood Institute (HL071981, HL034594, HL126024), the National Institute of Diabetes and Digestive and Kidney Diseases (DK091718, DK100383, DK078616), the Boston Obesity Nutrition Research Center (DK46200), and United States–Israel Binational Science Foundation Grant 2011036 (LQ). The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author contributions
DS and LQ conceptualized and designed the study, coordinated and supervised the project, drafted the initial manuscript, and approved the final manuscript as submitted. DS, TZ, and XL contributed to data cleaning and the statistical analysis. SHL, YH, and LQ contributed to critical revision of the manuscript. All authors actively contributed to the final manuscript and agree to be accountable for all aspects of the work. DS and LQ have full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis; they are the guarantors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sun, D., Zhou, T., Li, X. et al. Maternal smoking, genetic susceptibility, and birth-to-adulthood body weight. Int J Obes 44, 1330–1340 (2020). https://doi.org/10.1038/s41366-019-0509-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0509-7