Abstract
Survivors of childhood brain tumors (SCBT) face a higher risk of cardiometabolic disorders and premature mortality compared to the general population. Excess adiposity is a known risk factor for these comorbidities. However, while SCBT have higher adiposity compared to healthy controls, measuring adiposity in clinical practice involves access to specialized equipment and may impact busy clinical services. Tri-ponderal Mass Index (TMI; kg/m3) may be a superior measure of adiposity when compared to Body Mass Index (BMI; kg/m2). However, its use in determining adiposity in SCBT has not been assessed. This study aims to validate TMI as a clinical measure of adiposity in SCBT. This was a cross-sectional study including 44 SCBT (n = 20 female) and 137 (n = 64 female) non-cancer control children, 5–17 years of age. BMI and TMI were calculated from height and weight measurements. Fat mass percentage was assessed using bioelectrical impedance analysis and waist to hip and waist to height ratios were used to assess central adiposity. Regression analyses were adjusted for age, sex, puberty and treatment. TMI demonstrated strong correlations to measures of total and central adiposity and predicted adiposity in SCBT and non-cancer controls, with stronger trends in the latter group. TMI may serve as a reliable clinical measure of adiposity in both SCBT and healthy children.
Similar content being viewed by others
Introduction
Obesity has contributed to the rise of cardiovascular diseases and type 2 diabetes, making them some of the most significant and costly healthcare challenges of the 21st century1,2,3,4,5,6. One group that is especially impacted by these chronic diseases include childhood cancer survivors7,8,9. Within this population, survivors of childhood brain tumors (SCBT) represent an emerging group that has been recently reported to develop stroke and type 2 diabetes at higher rates than those seen in non-cancer control populations10,11,12. Obesity leads to increased cardiovascular mortality at a relatively young age in SCBT12,13,14,15,16,17,18,19,20,21,22.
Excess adiposity, especially visceral adiposity, has been linked to cardiovascular disease and type 2 diabetes in the general population, and SCBT have more adiposity compared to healthy controls23,24,25,26,27.
While adiposity is a potentially modifiable risk factor for cardiometabolic risk, measuring adiposity in clinical practice can be time consuming in the clinical setting, and requires specialized equipment including bioelectrical impedance scales or Dual-energy X-ray Absorptiometry (DXA) scans28,29,30. The availability of feasible and reliable clinical measures of adiposity will circumvent these limitations and help prioritize SCBT for closer monitoring and targeting them in interventions in an attempt to improve outcomes.
The tri-ponderal mass index, defined as weight divided by height cubed (TMI, kg/m3), is an alternate measure of adiposity in children31. TMI is reported as a more accurate predictor of adiposity compared to Body Mass Index (BMI, kg/m2) and BMI z-score when validated against DXA scans in adolescents31. An important advantage of TMI is that it uses the same height and weight measurements used to calculate BMI. Thus, TMI may offer a feasible clinical measure to assess adiposity. However, TMI has not been validated as a measure of adiposity in SCBT. Our aim is to validate TMI as a clinical measure of adiposity in SCBT and compare this group to non-cancer controls.
Results
Population characteristics
The characteristics of participants are reported in Table 1. We included 44 SCBT (n = 20 female, 45.50%), and 137 non-cancer controls (n = 64 female, 46.70%).
The SCBT and control groups had similar sex (p = 0.88) and ethnic distribution (Caucasian SCBT: n = 34 (77.30%); controls: n = 91 (66.40%), p = 0.18). SCBT were younger than the non-cancer controls (SCBT: 11.16 ± 4.29; controls: 14.03 ± 2.56, p < 0.001), and fewer survivors were pubertal compared to controls (SCBT: n = 23 (52.30%); controls: n = 121 (88.30%), p < 0.001). Survivors had lower weight (p < 0.001) and were shorter (p < 0.001) compared to controls.
In relation to body mass measures, we confirmed previous similar trends in both survivors and controls of BMI z-score (SCBT:0.57 ± 0.94; controls: 0.45 ± 1.12, p = 0.51) and BMI percentile (SCBT: 67.60 ± 26.30%; controls: 62.20 ± 29.30%, p = 0.33).
Adiposity levels were similar between groups including fat mass percentage (%FM; SCBT: 24.10 ± 9.30%; controls: 22.20 ± 9.40%, p = 0.16) and waist-to-height ratio (WHtR) (SCBT: 0.46 ± 0.06; controls: 0.45 ± 0.07, p = 0.17). However, waist to hip ratio (WHR) was higher in SCBT when compared to non-cancer controls (SCBT: 0.87 ± 0.07; controls: 0.82 ± 0.07, p < 0.001).
Due to the age and pubertal staging differences noted, we validated the results of the analysis of the full cohort by performing a subgroup analysis that included age- and sex-matched controls. In the latter analysis age, sex, and puberty adjusted analyses revealed identical trends to those reported for the full study cohort. The data for the matched subgroup analyses are reported in Supplementary Tables S1–S3.
Tumor characteristics and treatments
The details of tumor characteristics and treatment methods are reported in Table 2.
The most common tumors in survivors were low-grade gliomas (n = 29 (65.90%)). Brain tumors were equally localized to supratentorial and infratentorial regions. The treatments included surgery (n = 29 (65.90%)), radiotherapy (n = 13 (29.50%)) and chemotherapy (n = 20 (45.50%)). Eight (18.20%) participants were being managed with a wait and see approach at the time of inclusion in the study.
The association of TMI with body mass and adiposity
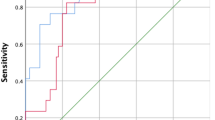
To assess if TMI correlates with body mass measures and adiposity, we used Spearman’s correlation test. We conducted unadjusted and age, sex, and puberty-adjusted analyses (Table 3).
TMI levels were similar between the groups (SCBT: 14.12 ± 2.54 kg/m3; controls: 13.46 ± 2.86 kg/m3, p = 0.10). TMI correlated with BMI z-score in both groups (Unadjusted, SCBT: ρ = 0.87; p < 0.001; controls: ρ = 0.95; p < 0.001; Adjusted, SCBT: r = 0.86; p < 0.001; controls: r = 0.94; p < 0.001).
We next assessed whether TMI correlates with measures of adiposity. TMI correlated significantly with measures of total adiposity including fat mass percentage (%FM) (Unadjusted, SCBT: ρ = 0.73; p < 0.001; controls: ρ = 0.85; p < 0.001; Adjusted, SCBT: r = 0.73; p < 0.001; controls: r = 0.88; p < 0.01). In addition, TMI correlated with measures of central adiposity, including WHR (Unadjusted, SCBT: ρ = 0.56; p < 0.001; controls: ρ = 0.38; p < 0.001; Adjusted, SCBT: r = 0.44; p < 0.01; controls: r = 0.46; p < 0.001), and WHtR correlated more strongly with TMI when compared to WHR (Unadjusted, SCBT: ρ = 0.69; p < 0.001; controls: ρ = 0.83; p < 0.001; Adjusted, SCBT: r = 0.82; p < 0.001; controls: r = 0.87; p < 0.001). There were similar trends of correlations of TMI and BMI z-score with measures of central adiposity (Table 3). Taken together, the above data indicate that TMI is a stronger predictor of total adiposity than BMI z-score and is equivalent to BMI z-score in predicting central adiposity. The correlation between TMI and BMI z-score tended to be stronger in non-cancer controls compared to SCBT.
To assess whether TMI is a predictor of body mass and adiposity in SCBT, multivariable linear regression analyses were conducted adjusting for age, sex and puberty. As radiotherapy was a significant predictor of %FM (p = 0.002) in SCBT, it was also adjusted for in the regression analyses.
We calculated unstandardized (B) and standardized (β) coefficients, and both trended in the same direction. Moving forward, we report on the latter coefficient (Table 4).
TMI was a strong predictor of BMI z-scores in both SCBT and controls, with a stronger trend in the latter (SCBT: β = 0.867; p < 0.001; controls: β = 0.935; p < 0.001). TMI was a strong predictor of total adiposity (%FM) in both SCBT and controls (SCBT: β = 0.604; p < 0.001; controls: β = 0.819; p < 0.001). While it had lower correlation with WHR, TMI was associated strongly with WHtR, and the strength of this association was higher in controls compared to SCBT (SCBT: β = 0.793; p < 0.001; controls: β = 0.880; p < 0.001).
The above threads of data indicate that TMI is a strong predictor of total adiposity and WHtR. The association between TMI and adiposity appears to be stronger in controls compared to SCBT for BMI z-score, %FM and WHtR.
Discussion
Survivors of childhood brain tumors are facing multiple comorbidities including cardiovascular disease and type 2 diabetes, which can impact their quality of life and lifespan13,14,15,27,32,33,34,35,36. The identification of predictors and markers of cardiometabolic risk may offer a path to stratify those in need of close observation and early intervention. In this study, we identified TMI as one such measure. TMI was an equally strong predictor as BMI z-score, total adiposity and WHtR, the latter being a stronger predictor of cardiometabolic risk compared to WHR37,38,39. As central adiposity is associated with adverse cardiometabolic outcomes37,38,39,40, this is of great clinical significance, as it allows the stratification of children with higher central adiposity to a care stream with closer cardiometabolic health monitoring and early more aggressive interventions.
TMI has been validated against DXA scan-measured adiposity in the general pediatric population31. Our data adds to the value of TMI in the general pediatric population and in a population with chronic health needs that has not been studied previously. TMI is a promising marker of adiposity that is clinically feasible and informative. The most widely used clinical measure of body mass, BMI, is a useful population-based measure to report the presence of obesity, and is used interchangeably to report adiposity41. However, one of the limitations of BMI is that it may not be adequate to diagnose obesity in certain populations, including adolescents42,43, hence the use of BMI z-score and percentile data to assess overweight and obesity in children. In addition, BMI misclassifies muscular individuals as being overweight or obese, which does not necessarily reflect their future risk of cardiometabolic disorders44. Furthermore, BMI has a weaker association with cardiovascular risk when compared to measures of adiposity including waist circumference and WHtR37,45,46.
Children require special consideration in using BMI to classify obesity and adiposity. Ratios of weight over height to various powers of rho, ρ, (weight/heightρ) have been explored to account for the effects of children’s growth during puberty, and the adjustment for ρ is critical because incorrect values misclassify tall or physically advanced children as overweight47,48. A ρ value equal to two as used in BMI is sufficient when height is constant, however during puberty changes in height increase the ρ value48.
In pre-school children, weight over height squared is adequate for assessing adiposity47. Adiposity generally declines between the ages 5–7 years before it begins to rise again, the adiposity rebound phase49. An earlier adiposity rebound than expected is associated with an increased risk of obesity and type 2 diabetes in adults49,50,51.
As children approach the peripubertal phase of growth and development, their body composition changes with increased adiposity, especially in girls52,53. The value of ρ gradually rises from two to three; children who have undergone a growth spurt due to puberty tend to be heavier when compared to less mature children at the same height47. The increase in weight accompanying growth spurts results in higher BMI values, therefore greater values of ρ are required to offset the weight gain experienced in physically advanced children.
However, body composition changes in children become more constant as they get older and ρ decreases back to two47,48. Therefore, during puberty, TMI may be a more accurate measure of adiposity in children47. For this reason, the use of TMI is more relevant to assess body fat mass in children and, when evaluated in adults, TMI is less reliable compared to BMI when correlated with skinfold thickness41.
Measures of adiposity in children have relied on technologies that may not be readily available in the clinical setting but have demonstrated accuracy in estimating the fat mass. DXA estimates of trunk and abdominal fat have demonstrated a strong association to total abdominal fat28,29,30, while Bioelectrical impedance analysis (BIA) has been validated as a measure of adiposity against DXA54,55,56. Our results demonstrate that TMI is a strong predictor of adiposity measured using BIA, which is congruent with adiposity assessments using DXA. This is another strength of this study, as it validates TMI against BIA, a common measure of adiposity that is more easily accessible than DXA.
Our results indicate that TMI may offer a better estimate of fat mass and is a potential tool for predicting adiposity in children compared to BMI z-score. While some studies have found TMI to be an appropriate measure of adiposity in children, others have suggested BMI may still be an equivalent measure31,57. However, these studies often include children as young as two years of age, and weight scales over height squared in this age group that makes validating TMI as a measure of adiposity in this group a future goal of research47,57.
There are several strengths of our study. The inclusion of non-cancer controls for comparison to the SCBT group offers validation of this measure in the general pediatric population as well as SCBT. The description of the association of TMI with measures of central adiposity is another strength, as central adiposity is not routinely assessed in clinical practice. Furthermore, the inclusion of an age and sex matched subgroup analysis validates our findings.
A larger sample size of SCBT is required to validate these results further, and to define their associations. In addition, TMI needs to be validated as a predictor of cardiometabolic outcomes which should be part of longitudinal studies.
In conclusion, TMI represents a clinically feasible measure that uses the same variables measuring BMI but demonstrate higher correlation with adiposity.
The availability of TMI as a clinical measure of adiposity will allow the stratification of patients at risk of excess adiposity to be prioritized for targeted interventions. This is critical, as these survivors are facing cardiometabolic diseases that are important emergent determinants of outcomes.
Methods
Participants
Participants were consecutively recruited from McMaster Children’s Hospital (Hamilton), Ontario, Canada from November 2012 to November 2017 to partake in the Canadian Study of Determinants of Endometabolic Health in Children (CanDECIDE study)58,59.
Children between 5–17 years of age were included. Parental informed consent was obtained for participants less than 7 years of age, and parental consent and participant assent were obtained for those 7–15 years of age. Participants provided written informed consent if they were 16 years or older. This is a secondary analysis of the CanDECIDE cohort study data and this analysis has been approved by the Hamilton Integrated Research Ethics Board. Study procedures were performed in accordance with the relevant guidelines and legal regulations.
Anthropometric and clinical measurements
Standardized questionnaires were used to collect data on age, sex, puberty, and ethnicity58,59. Medical records were consulted to verify and collect data regarding tumor type, location, sidedness and treatment modalities for SCBT.
Anthropometric measurements included weight measured to the nearest 0.1 kg using an electronic weighing scale (Seca, USA) and height using a stadiometer measured to the nearest 0.1 cm. BMI (kg/m2) and TMI (kg/m3) were determined using height and weight measurements from all participants. BMI percentile was determined from the Children’s BMI Tool for Schools60. BMI z-scores were determined from the Centers for Disease Control and Prevention (CDC) growth chart61.
Fat mass percentage (%FM) was used to determine adiposity in the participants that was measured with the Tanita body fat monitor (Tanita Corporation, Illinois, USA)62.
Statistical Analysis
Statistical analyses were performed using PASW version 18 statistical package63. Data are presented as counts with percentages for categorical variables and means with standard deviation for continuous variables. Only participants with complete datasets were included. Box plots and visual inspection were used to identify any outliers for removal from the analysis. Normality of the data distribution was assessed using the Shapiro-Wilk test64. In the case that variables had non-normal distributions, data were log-transformed. Sample size was calculated using the method proposed by Norman and Streiner. We calculated that we need eight subjects per variable to detect significant differences between groups65.
Spearman’s correlations were used to assess the relationship between TMI, BMI z-score, %FM, WHR and WHtR. To assess this relationship adjusted for age, sex and puberty, we ran a Partial Correlations test. Multivariable linear regression analyses were performed to determine the association between TMI with BMI z-score and adiposity measures (%FM, WHR and WHtR), in SCBT and controls. The dependent variable was set as %FM, WHtR, WHR or BMI z-score and the independent variables included TMI, age, sex, puberty and treatment. Results were reported as standardized β coefficients and associated p-values, with statistical significance set to alpha of 0.05. A model summary, including the adjusted R Square and the Standard Error of the Estimate, were also reported.
In order to validate that age and puberty differences did not affect the results, analyses were also repeated using an age- and sex-matched control group. Control participants were matched in terms of sex distribution to SCBT participants on a one-to-one ratio and age was matched to closest value, within three years of the SCBT participants.
Data Availability
The data for the current study used for statistical analysis are available from the corresponding author upon reasonable justification.
References
Zimmet, P., Alberti, K. & Shaw, J. Global and societal implications of the diabetes epidemic. Nature 414, 782–787 (2001).
Zimmet, P. Z., Magliano, D. J., Herman, W. H. & Shaw, J. E. Diabetes: a 21st century challenge. The lancet Diabetes & endocrinology 2, 56–64 (2014).
Murray, C. J. L. & Lopez, A. D. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. The lancet 349, 1436–1442 (1997).
Danaei, G. et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2· 7 million participants. The Lancet 378, 31–40 (2011).
Murray, C. J. L. & Lopez, A. D. Mortality by cause for eight regions of the world: Global Burden of Disease Study. The lancet 349, 1269–1276 (1997).
Dobbs, R. et al. Overcoming obesity: An initial economic analysis. 2014. McKinsey & Company: www. mckinsey. com/mgi, 1–106 (2014).
Oeffinger, K. C. et al. Chronic health conditions in adult survivors of childhood cancer. New England Journal of Medicine 355, 1572–1582 (2006).
Meacham, L. R. et al. Cardiovascular risk factors in adult survivors of pediatric cancer—a report from the childhood cancer survivor study. Cancer Epidemiology and Prevention Biomarkers 19, 170–181 (2010).
Sasaki, K., Srikanthan, A., Baxter, N. & Lega, I. Diabetes Mellitus in Childhood Cancer Survivors: A Systematic Review. Canadian Journal of Diabetes 41, S27 (2017).
Bowers, D. C. et al. Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: a report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology 24, 5277–5282 (2006).
Gurney, J. G. et al. Endocrine and cardiovascular late effects among adult survivors of childhood brain tumors. Cancer 97, 663–673 (2003).
Meacham, L. R. et al. Diabetes mellitus in long-term survivors of childhood cancer: increased risk associated with radiation therapy: a report for the childhood cancer survivor study. Archives of internal medicine 169, 1381–1388 (2009).
Mertens, A. C. et al. Late mortality experience in five-year survivors of childhood and adolescent cancer: the Childhood Cancer Survivor Study. Journal of Clinical Oncology 19, 3163–3172 (2001).
Prasad, P. K., Signorello, L. B., Friedman, D. L., Boice, J. D. & Pukkala, E. Long‐term non‐cancer mortality in pediatric and young adult cancer survivors in Finland. Pediatric blood & cancer 58, 421–427 (2012).
Samaan, M. C. & Akhtar-Danesh, N. The impact of age and race on longevity in pediatric astrocytic tumors: A population-based study. Pediatric blood & cancer, https://doi.org/10.1002/pbc.25522 (2015).
Ward, E., DeSantis, C., Robbins, A., Kohler, B. & Jemal, A. Childhood and adolescent cancer statistics, 2014. CA: a cancer journal for clinicians 64, 83–103 (2014).
Poirier, P. et al. Obesity and cardiovascular disease. Arteriosclerosis, thrombosis, and vascular biology 26, 968–976 (2006).
Nayga, R. M. Jr. Obesity and heart disease awareness: a note on the impact of consumer characteristics using qualitative choice analysis. Applied Economics Letters 4, 229–231 (1997).
Wheelock, V. Healthy eating: the food issue of the 1990s. British food journal 94, 3–8 (1992).
Romero-Corral, A. et al. Normal weight obesity: a risk factor for cardiometabolic dysregulation and cardiovascular mortality. European heart journal 31, 737–746 (2009).
Vatten, L. J., Nilsen, T. I. L., Romundstad, P. R., Drøyvold, W. B. & Holmen, J. Adiposity and physical activity as predictors of cardiovascular mortality. European Journal of Cardiovascular Prevention & Rehabilitation 13, 909–915 (2006).
Wajchenberg, B. L. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocrine reviews 21, 697–738 (2000).
Poirier, P. et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss. Circulation 113, 898–918 (2006).
Juonala, M. et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. New England Journal of Medicine 365, 1876–1885 (2011).
Haffner, S. M. Abdominal adiposity and cardiometabolic risk: do we have all the answers? The American journal of medicine 120, S10–S16 (2007).
Wang, K. W. et al. PS1-176 Where Have All the Fat Cells Gone? A Comparative Analysis of Adiposity Patterns in Childhood Brain Tumor Survivors and Non-Cancer Controls. Canadian Journal of Neurological Sciences 43, S11–S11 (2016).
Wang, K. W. et al. Overweight, obesity and adiposity in survivors of childhood brain tumours: a systematic review and meta‐analysis. Clinical Obesity (2017).
Clasey, J. L. et al. The use of anthropometric and dual‐energy X‐ray absorptiometry (DXA) measures to estimate total abdominal and abdominal visceral fat in men and women. Obesity 7, 256–264 (1999).
Glickman, S. G., Marn, C. S., Supiano, M. A. & Dengel, D. R. Validity and reliability of dual-energy X-ray absorptiometry for the assessment of abdominal adiposity. Journal of Applied Physiology 97, 509–514 (2004).
Huang, T. T. K., Watkins, M. P. & Goran, M. I. Predicting total body fat from anthropometry in Latino children. Obesity 11, 1192–1199 (2003).
Peterson, C. M. et al. Tri-Ponderal Mass Index vs Body Mass Index in Estimating Body Fat During Adolescence. JAMA pediatrics (2017).
Chambless, L. B., Parker, S. L., Hassam-Malani, L., McGirt, M. J. & Thompson, R. C. Type 2 diabetes mellitus and obesity are independent risk factors for poor outcome in patients with high-grade glioma. Journal of neuro-oncology 106, 383–389 (2012).
Nader, P. R. et al. Identifying risk for obesity in early childhood. Pediatrics 118, e594–e601 (2006).
Lustig, R. H. et al. Risk factors for the development of obesity in children surviving brain tumors. The Journal of Clinical Endocrinology & Metabolism 88, 611–616 (2003).
Pui, C. H. et al. Treatment outcomes in black and white children with cancer: results from the SEER database and St Jude Children’s Research Hospital, 1992 through 2007. J Clin Oncol 30, 2005–2012, https://doi.org/10.1200/JCO.2011.40.8617 (2012).
Wang, K.-W. et al. Adiposity in childhood brain tumors: a report from the Canadian Study of Determinants of Endometabolic Health in Children (CanDECIDE Study). Scientific reports 7, 45078 (2017).
Savva, S. C. et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. International journal of obesity 24, 1453 (2000).
Savva, S. C., Lamnisos, D. & Kafatos, A. G. Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes, metabolic syndrome and obesity: targets and therapy 6, 403 (2013).
Sayeed, M. A. et al. Waist-to-height ratio is a better obesity index than body mass index and waist-to-hip ratio for predicting diabetes, hypertension and lipidemia. Bangladesh Medical Research Council Bulletin 29, 1–10 (2003).
Ali, O. et al. Obesity, central adiposity and cardiometabolic risk factors in children and adolescents: a family‐based study. Pediatric obesity 9 (2014).
Keys, A., Fidanza, F., Karvonen, M. J., Kimura, N. & Taylor, H. L. Indices of relative weight and obesity. Journal of chronic diseases 25, 329–343 (1972).
Maynard, L. M. et al. Childhood Body Composition in Relation to Body Mass Index. Pediatrics 107, 344–350 (2001).
Quetelet, A. Physique sociale, ou essai sur le développement des facultés de l’homme. Vol. 2 (C. Muquardt, 1869).
Witt, K. A. & Bush, E. A. College athletes with an elevated body mass index often have a high upper arm muscle area, but not elevated triceps and subscapular skinfolds. Journal of the American Dietetic Association 105, 599–602 (2005).
Yusuf, S. et al. Obesity and the risk of myocardial infarction in 27 000 participants from 52 countries: a case-control study. The Lancet 366, 1640–1649 (2005).
Wells, J. C. K. Commentary: the paradox of body mass index in obesity assessment: not a good index of adiposity, but not a bad index of cardio-metabolic risk. International journal of epidemiology 43, 672 (2014).
Cole, T. J. Weight/heightp compared to weight/height2 for assessing adiposity in childhood: influence of age and bone age on p during puberty. Annals of human biology 13, 433–451 (1986).
Franklin, M. F. Comparison of weight and height relations in boys from 4 countries. The American journal of clinical nutrition 70, 157S–162S (1999).
Whitaker, R. C., Pepe, M. S., Wright, J. A., Seidel, K. D. & Dietz, W. H. Early adiposity rebound and the risk of adult obesity. Pediatric0s 101, e5–e5 (1998).
Rolland-Cachera, M.-F. et al. Adiposity rebound in children: a simple indicator for predicting obesity. The American journal of clinical nutrition 39, 129–135 (1984).
Eriksson, J. G., Forsen, T., Tuomilehto, J., Osmond, C. & Barker, D. J. P. Early adiposity rebound in childhood and risk of Type 2 diabetes in adult life. Diabetologia 46, 190–194 (2003).
Kaplowitz, P. B. Link between body fat and the timing of puberty. Pediatrics 121, S208–S217 (2008).
Kaplowitz, P. B., Slora, E. J., Wasserman, R. C., Pedlow, S. E. & Herman-Giddens, M. E. Earlier onset of puberty in girls: relation to increased body mass index and race. Pediatrics 108, 347–353 (2001).
Kabiri, L. S., Hernandez, D. C. & Mitchell, K. Reliability, validity, and diagnostic value of a pediatric bioelectrical impedance analysis scale. Childhood Obesity 11, 650–655 (2015).
Tyrrell, V. J. et al. Foot-to-foot bioelectrical impedance analysis: a valuable tool for the measurement of body composition in children. International Journal of Obesity & Related Metabolic Disorders 25 (2001).
Beeson, W. L. et al. Comparison of body composition by bioelectrical impedance analysis and dual-energy X-ray absorptiometry in Hispanic diabetics. International journal of body composition research 8, 45 (2010).
Mei, Z. et al. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. The American journal of clinical nutrition 75, 978–985 (2002).
Samaan, M. C., Thabane, L., Burrow, S., Dillenburg, R. F. & Scheinemann, K. Canadian Study of Determinants of Endometabolic Health in ChIlDrEn (CanDECIDE study): a cohort study protocol examining the mechanisms of obesity in survivors of childhood brain tumours. BMJ open 3, e002869, https://doi.org/10.1136/bmjopen-2013-002869 (2013).
Samaan, M. C. et al. Recruitment feasibility to a cohort study of endocrine and metabolic health among survivors of childhood brain tumours: a report from the Canadian study of Determinants of Endometabolic Health in ChIlDrEn (CanDECIDE). BMJ Open 4, e005295, https://doi.org/10.1136/bmjopen-2014-005295 (2014).
Nihiser, A. J. et al. Body mass index measurement in schools. J Sch Health 77, 651–671; quiz 722-654, https://doi.org/10.1111/j.1746-1561.2007.00249.x (2007).
Kuczmarski, R. J. et al. 2000 CDC Growth Charts for the UnitedStates: methods and development. Vital Health Stat 11, 1–190 (2002).
Wang, K. W. et al. Adiposity in childhood brain tumors: A report from the Canadian Study of Determinants of Endometabolic Health inChildren (CanDECIDE Study). Scientific reports 7, 45078, https://doi.org/10.1038/srep45078 (2017).
SPSS Inc. PASW Statistics for Windows, Version 18.0. Chicago: SPSS Inc. (2009).
Ghasemi, A. & Zahediasl, S. Normality tests for statistical analysis: a guide for non-statisticians. International journal of endocrinology and metabolism 10, 486 (2012).
Norman, G. R. & Streiner, D. L. PDQ Statistics. 3rd Edition (2003).
Acknowledgements
We would like to thank the participants as well as their families for participating in the study. We would also like to thank the staff for assisting in the recruitment of participants.
Author information
Authors and Affiliations
Contributions
M.C.S. is the guarantor of this study. E.D.S., K.W.W., A.F., D.L.J., S.M.Z., S.R.R., S.B., L.T. and M.C.S. were involved in defining the research question and study design. K.W.W. and E.D.S. were responsible for participant recruitment and data collection and were supported by A.F., S.B., D.L.J. and S.M.Z. Support in research methods and statistical analyses were provided by M.C.S. and L.T. The interpretation of the data was completed by E.D.S., K.W.W., A.F., D.L.J., S.M.Z., S.R.R., S.B., L.T. and M.C.S. E.D.S. and M.C.S. drafted the manuscript which was reviewed by all authors, who agreed with its contents.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sims, E.D., Wang, KW., Fleming, A. et al. Tri-ponderal mass index in survivors of childhood brain tumors: A cross-sectional study. Sci Rep 8, 16336 (2018). https://doi.org/10.1038/s41598-018-34602-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-34602-5
Keywords
This article is cited by
-
The triponderal mass index as a measure of adiposity in pediatric survivors of acute lymphoblastic leukemia: a cross-sectional study
Scientific Reports (2022)
-
Metabolic risk assessment in children and adolescents using the tri-ponderal mass index
Scientific Reports (2022)
-
The Tri-ponderal Mass Index is associated with adiposity in adolescent type 2 diabetes mellitus: a cross-sectional analysis
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.