Abstract
Serial cervical length (CL) measurement in mid-trimester is recommended in post-conization pregnancy to estimate the risk of spontaneous preterm birth (SPTB). A short mid-trimester cervix (CL < 25 mm) has been considered as a strong predictor for SPTB. However, the low incidence of short cervix limits the utility of mid-trimester CL measurement in prediction of SPTB. A great proportion of women who develop SPTB don’t have a short mid-trimester cervix. Therefore, this study was aimed to investigate the additional value of serial CL measurement in predicting SPTB in addition to detecting short cervix alone. A total of 613 post-conization pregnant women who did not have short mid-trimester cervix between January 2004 and January 2014 were included in this study. Serial CL measurements were taken by transvaginal ultrasound at three timepoints (A: 13 + 0–15 + 6 weeks, B: 16 + 0–18 + 6 weeks, and C: 20 + 0–22 + 6 weeks). Eight parameters were analyzed for predicting SPTB, including CL measurements at different timepoints (CLA, CLB, CLC), the maximum and minimum CL measurements (CLMAX, CLMIN), and the percentage change in CL measurement between different timepoints (%ΔCLAB, %ΔCLBC, %ΔCLAC). After univariate and multivariate analysis, CLMAX and %ΔCLAC were independent variables in predicting SPTB. Lower CLMAX (OR [95%CI]: 0.92 [0.90–0.93]) and higher %ΔCLAC (OR [95%CI]: 1.05 [1.01–1.09]) were related to an increasing risk of SPTB. In conclusion, our study for the first time in literature reported the value of serial CL measurement in prediction of SPTB in post-conization pregnancy without short mid-trimester cervix. In the subpopulation of pregnant women who did not have short mid-trimester cervix, CLMAX and %ΔCLAC were of value in predicting SPTB, which warranted further investigations.
Similar content being viewed by others
Introduction
Conization is a cone biopsy of the uterine cervix that serve as a diagnostic and therapeutic procedure, which is used for conservative treatment of cervical intraepithelial neoplasia (CIN)1. However, this local cervical treatment has been correlated to an increased risk of spontaneous preterm birth (SPTB) in a subsequent pregnancy2. The underlying pathogenesis is poorly understood. Hypotheses include a loss of mechanical support from the cervix, a change in immunologic defense mechanism, and an alteration in cervicovaginal bacterial flora2,3,4.
Currently, transvaginal cervical sonography is commonly utilized in the mid-trimester to assess CL in women at high risk for SPTB, such as post-conization pregnacy5. Detection of a short cervix has been considered to be a surrogate for cervical insufficiency, and therefore, a useful predictor of SPTB3,6. In clinical practice, once a woman has been identified as being at higher risk of SPTB due to short cervix, a decision regarding prophylactic treatment must be made7. A cut-off value of 25 mm is widely used as the threshold8,9.
However, the low incidence of short cervix limits the utility of mid-trimester cervical screening in prediction of SPTB. A great proportion of women who developed SPTB did not have a short mid-trimester cervix10. For example, Boelig et al. reported the majority of women (82%) who developed SPTB did not have a short mid-trimester cervix in a prospective cohort study, which included 2071 singleton pregnant women without a prior history of SPTB undergoing universal CL screening in mid-trimester11.
In fact, little was known about the additional value of mid-trimester cervical screening in prediction of SPTB in addition to detecting short cervix alone. In the subpopulation of pregnant women who did not have short mid-trimester cervix, the predictability of SPTB was of great clinical value, however only limited studies focused on this issue in previous literatures. Therefore, the present study was designed to investigate the value of serial CL measurement in prediction of SPTB in post-conization pregnancy without short mid-trimester cervix.
Results
A total of 613 pregnant women post-conization were included in this retrospective study. The average maternal age was 34.2 ± 5.1 years. Ethnicity information was available in 578 women (94.2%). Of them, 145 (25.1%) were Asian, 117 (20.2%) were Black, and 316 (54.7%) were Caucasian. For pregnancy outcome, despite the absence of short cervix <25 mm in mid-trimester, SPTB < 37 weeks still occurred in 45 women (7.3%).
Predictor selection
A total of eight parameters were taken as the candidates for SPTB predictors, including CL measurements at different timepoints (CLA, CLB, CLC), the maximum and minimum CL measurements (CLMAX, CLMIN), and the percentage change in CL measurement between different timepoints (%ΔCLAB, %ΔCLBC, %ΔCLAC). In univariate analysis, CLC, CLMAX, CLMIN, and %CLAC were significantly different between SPTB group and term birth group (Table 1). In multivariate analysis, CLC and CLMIN were excluded on logistic regression, while CLMAX and %CLAC were finally selected as the predictors for SPTB (Table 1).
Diagnostic performance
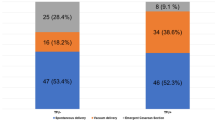
Using CLMAX and %ΔCLAC as the predictors of SPTB, their area under curve (AUC) of receiver operating characteristic (ROC) curve were 0.611 and 0.600, respectively. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios (LR) of CLMAX and %ΔCLAC in predicting SPTB were shown in Table 2 with different cut-off values. According to the ROC curve, the cut-off values with the optimum balance between sensitivity and specificity were ≥10% for %ΔCLAC (Sensitivity = 42.9%, Specificity = 71.2%, PPV = 9.7%, NPV = 94.5% and LR = 1.49) and <30 mm for CLMAX (Sensitivity = 26.7%, Specificity = 90.8%, PPV = 18.8%, NPV = 94.0% and LR = 2.91), respectively.
Discussion
The value of mid-trimester cervical screening in predicting the risk of SPTB has been widely studied. A mid-trimester CL < 25 mm is considered “short,” as 25 mm corresponds to the 10th percentile for this gestational age12. A short mid-trimester cervix has been considered as one of the strongest risk factors for SPTB10.
However, the low incidence of short cervix limits the utility of mid-trimester CL measurement in prediction of SPTB. Esplin et al. reported a multicenter, prospective observational cohort study that included 9410 nulliparous singleton pregnancies. Of them, 474 (5.0%) had SPTB, 335 (3.6%) had medically indicated preterm births, and 8601 (91.4%) had term births. Among women with SPTB < 37 weeks, short CL < 25 mm occurred in only 23.3% cases in the mid-trimester13. Furthermore, even in high-risk population, a great proportion (31–81%) of women who developed SPTB did not have a short CL < 25 mm during mid-trimester cervical screening12.
Unfortunately, in addition to detecting short cervix, little was known about the additional value of mid-trimester cervical screening in predicting SPTB. In the subpopulation of pregnant women who did not have short mid-trimester cervix, the predictability of SPTB was of great clinical value, however only limited studies focused on this issue in previous literatures. Therefore, the present study was aimed to investigate the value of serial CL measurement in prediction of SPTB in women without short mid-trimester cervix. This study was a secondary analysis of open data from a previous research, which was the largest research in literature on serial mid-trimester CL measurement in post-conization pregnancy14.
A total of eight parameters derived from serial CL measurement in the mid-trimester were analyzed in our study, including CLA, CLB, CLC, CLMAX, CLMIN, %ΔCLAB, %ΔCLBC, and %ΔCLAC. After univariate and multivariate analysis, only CLMAX and %ΔCLAC were proven to be independent variables in predicting subsequent SPTB. Lower CLMAX (OR [95%CI]: 0.92 [0.90–0.93]) and higher %ΔCLAC (OR [95% CI]: 1.05 [1.01–1.09]) were related to an increasing risk of SPTB.
For parameters as CL measurement at single timepoint, CLC, CLMIN and CLMAX were significantly different between SPTB group and term birth group. Whereas only CLMAX was selected as an independent variable in predicting subsequent SPTB on logistic regression analysis. To our knowledge, this finding is the first evidence in literature for the predictive value of CLMAX in SPTB. Using ROC curve method, the AUC was 0.611 and the optimum cut-off value was <30 mm for CLMAX (Sensitivity = 26.7%, Specificity = 90.8%, PPV = 18.8%, NPV = 94.0% and LR = 2.91).
In contrast, the value of CLMIN has already been studied in previous researches. Owen et al. reported that CLMIN in serial measurements significantly improved the prediction of SPTB compared with a single CL measurement12. However, our results indicated the superiority of CLMAX to CLMIN in predicting subsequent SPTB, which may be attributable to the exclusion of cases with short cervix <25 mm in our study. CLMIN was a parameter aimed to improve the detection of short cervix in serial screening compared to single measurement in the mid-trimester. Therefore, the predictive value of CLMIN may be dependent on the presence of short cervix <25 mm. Whereas CLMAX was a parameter reflecting the upper limit, but not lower limit, of CL in mid-trimester, which may be independent on the presence of short cervix <25 mm. Thus, it seems to be reasonable that CLMAX is of value in predicting subsequent SPTB in the subpopulation of pregnant women who did not have short mid-trimester cervix.
For parameters as CL change between two timepoints, %ΔCLAC was an independent variable in predicting subsequent SPTB by univariate and multivariate analysis. Using ROC curve method, the AUC was 0.600 and the optimum cut-off value was ≥10% for %ΔCLAC (Sensitivity = 42.9%, Specificity = 71.2%, PPV = 9.7%, NPV = 94.5% and LR = 1.49). This finding was consistent with previous studies9,15,16,17. Moroz et al. reported that the rate of change in CL was associated with the occurrence of subsequent SPTB17. For every 1 mm of cervical shortening between measurements, there was a 3% increase in odds of SPTB. However, in their research this association between change in CL and risk for SPTB was only present for women with short cervix <25 mm, but not for women with CL >25 mm. In contrast, in our study, %ΔCLAC was still associated with an increasing risk of SPTB in the absence of short cervix (OR [95%CI]: 1.05 [1.01–1.09]). This difference may be attributable to the different duration of cervical screening in the mid-trimester. In the study of Moroz et al., CL measurements were performed between 24 weeks (range: 21–28 weeks) and 28 weeks (range: 25–33 weeks) of gestation. Whereas in our study, %ΔCLAC represented the change of CL between timepoint A (range: 13–16 weeks) and timepoint C (range: 20–23 weeks). By including the early-stage of mid-trimester, the time interval between measurements in our study was much longer than that in Moroz et al.’s study (7 weeks vs 4 weeks on average interval). In support of this explanation, the change of CL during a short duration in our study, represented by %ΔCLAB and %ΔCLBC, was also not associated with an increasing risk of SPTB.
Several limitations need to be acknowledged in our study. First, the study was a secondary analysis of a previous clinical research, which was subject to inherent limitations of the post hoc analysis. Secondly, another important limitation of the study was related to its retrospective design. Particularly in the earlier years of the study, when the association between conization and preterm birth was not well-established, preterm clinic referrals were unlikely to reflect all women post-conization within the population.
In conclusion, our study for the first time in literature reported the value of serial cervical length measurement in prediction of SPTB in post-conization pregnancy without short mid-trimester cervix. In the subpopulation of pregnant women who did not have short mid-trimester cervix, CLMAX and %ΔCLAC were of value in predicting SPTB, which warranted further investigations.
Methods
Study population
The study was a secondary analysis of the open data from a previous study, which was the largest research in literature on serial mid-trimester CL measurement in post-conization pregnancy14,18. The secondary analysis utilized de-identified patient information and was approved by the institutional review board of Peking Union Medical College Hospital.
The original database included a total of 725 pregnant women post-conization from the preterm surveillance clinics at three London University maternity units (Queen Charlottes Hospital, St Marys Hospital, Chelsea Westminster Hospital) between January 2004 and January 2014. Women were only eligible if they had their first singleton pregnancy after excisional cervical treatment for CIN of depth ≥12 mm (including Cone biopsy, LLETZ and LEEP). Any women with a prior preterm delivery (<37 weeks), mid-trimester miscarriage (>13 weeks), uterine anomaly or a multi-fetal pregnancy were excluded.
According to the aim of our study, women who had treatment for short mid-trimester cervix (n = 98) and short mid-trimester cervix without relevant treatment were excluded (n = 14). Finally, a total of 613 pregnant women post-conization were included in present study.
A pre-specified surveillance protocol including serial mid-trimester CL measurements was applied to all women attending prematurity clinics across sites for the duration of the study. CL measurements were taken at transvaginal ultrasound with an empty bladder, avoiding undue pressure on the cervix, and fundal pressure applied to illicit any further cervical shortening. The serial CL measurements were available for at least one of three screening timepoints; A: 13 + 0–15 + 6 weeks, B: 16 + 0–18 + 6 weeks, and C: 20 + 0–22 + 6 weeks.
Statistical analysis
Predictor selection
CL measurements at different timepoints (CLA, CLB, CLC), the maximum and minimum CL measurements (CLMAX, CLMIN), and the percentage change in CL measurement between different timepoints (%ΔCLAB, %ΔCLBC, %ΔCLAC) were taken as the candidates for SPTB predictors.
First, in univariate analysis all above parameters were analyzed by Mann Whitney tests to identify the variables with a significant difference between SPTB group and term birth group. Subsequently, logistic regression with the backward elimination method for a multivariate analysis was performed to exclude the variables that were not independently significant for predicting the outcome. After the 2-step selection, the remaining predictors were used to assess the value of mid-trimester serial CL measurement in prediction of SPTB.
Diagnostic performance
For each above-selected predictor, the diagnostic test was used to calculate test characteristics such as sensitivity, specificity, PPV, NPV and LR from a 2 × 2 table. Finally, the ROC curve was plotted and its AUC was calculated.
All statistical analyses were performed using SPSS version 16.0. Two-tailed P values less than 0.05 were considered statistically significant.
References
Rafaeli-Yehudai, T. et al. The effect of cervical cerclage on pregnancy outcomes in women following conization. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet 27, 1594–1597, https://doi.org/10.3109/14767058.2013.871254 (2014).
Kyrgiou, M. et al. Adverse obstetric outcomes after local treatment for cervical preinvasive and early invasive disease according to cone depth: systematic review and meta-analysis. BMJ (Clinical research ed.) 354, i3633, https://doi.org/10.1136/bmj.i3633 (2016).
Fischer, R. L., Sveinbjornsson, G. & Hansen, C. Cervical sonography in pregnant women with a prior cone biopsy or loop electrosurgical excision procedure. Ultrasound in obstetrics & gynecology: the official journal of the International Society of Ultrasound in Obstetrics and Gynecology 36, 613–617, https://doi.org/10.1002/uog.7682 (2010).
Nam, K. H., Kwon, J. Y., Kim, Y. H. & Park, Y. W. Pregnancy outcome after cervical conization: risk factors for preterm delivery and the efficacy of prophylactic cerclage. Journal of gynecologic oncology 21, 225–229, https://doi.org/10.3802/jgo.2010.21.4.225 (2010).
Sentilhes, L. et al. Prevention of spontaneous preterm birth: Guidelines for clinical practice from the French College of Gynaecologists and Obstetricians (CNGOF). European journal of obstetrics, gynecology, and reproductive biology 210, 217–224, https://doi.org/10.1016/j.ejogrb.2016.12.035 (2017).
Alfirevic, Z. et al. Vaginal progesterone, cerclage or cervical pessary for preventing preterm birth in asymptomatic singleton pregnant women with a history of preterm birth and a sonographic short cervix. Ultrasound in obstetrics & gynecology: the official journal of the International Society of Ultrasound in Obstetrics and Gynecology 41, 146–151, https://doi.org/10.1002/uog.12300 (2013).
Hezelgrave, N. L. et al. Rationale and design of SuPPoRT: a multi-centre randomised controlled trial to compare three treatments: cervical cerclage, cervical pessary and vaginal progesterone, for the prevention of preterm birth in women who develop a short cervix. BMC pregnancy and childbirth 16, 358, https://doi.org/10.1186/s12884-016-1148-9 (2016).
Conde-Agudelo, A. et al. Vaginal progesterone vs. cervical cerclage for the prevention of preterm birth in women with a sonographic short cervix, previous preterm birth, and singleton gestation: a systematic review and indirect comparison metaanalysis. American journal of obstetrics and gynecology 208, 42.e41–42.e18, https://doi.org/10.1016/j.ajog.2012.10.877 (2013).
Melamed, N. et al. Do serial measurements of cervical length improve the prediction of preterm birth in asymptomatic women with twin gestations? American journal of obstetrics and gynecology 215, 616.e611–616.e614, https://doi.org/10.1016/j.ajog.2016.06.034 (2016).
Glover, A. V. & Manuck, T. A. Screening for spontaneous preterm birth and resultant therapies to reduce neonatal morbidity and mortality: A review. Seminars in fetal & neonatal medicine 23, 126–132, https://doi.org/10.1016/j.siny.2017.11.007 (2018).
Boelig, R. C., Orzechowski, K. M. & Berghella, V. Cervical length, risk factors, and delivery outcomes among women with spontaneous preterm birth. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet 29, 2840–2844, https://doi.org/10.3109/14767058.2015.1105957 (2016).
Owen, J. et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. Jama 286, 1340–1348 (2001).
Esplin, M. S. et al. Predictive Accuracy of Serial Transvaginal Cervical Lengths and Quantitative Vaginal Fetal Fibronectin Levels for Spontaneous Preterm Birth Among Nulliparous Women. Jama 317, 1047–1056, https://doi.org/10.1001/jama.2017.1373 (2017).
Kindinger, L. M. et al. Preterm Birth Prevention Post-Conization: A Model of Cervical Length Screening with Targeted Cerclage. PloS one 11, e0163793, https://doi.org/10.1371/journal.pone.0163793 (2016).
Moroz, L. A. et al. Association between change in cervical length and spontaneous preterm birth in twin pregnancies. American journal of obstetrics and gynecology 216, 159.e151–159.e157, https://doi.org/10.1016/j.ajog.2016.10.002 (2017).
Melamed, N. et al. Serial cervical length determination in twin pregnancies reveals 4 distinct patterns with prognostic significance for preterm birth. American journal of obstetrics and gynecology 215, 476.e471–476.e411, https://doi.org/10.1016/j.ajog.2016.05.018 (2016).
Moroz, L. A. & Simhan, H. N. Rate of sonographic cervical shortening and the risk of spontaneous preterm birth. American journal of obstetrics and gynecology 206, 234.e231–235, https://doi.org/10.1016/j.ajog.2011.11.017 (2012).
Kindinger, L. M. (Dryad Digital Repository, 2016).
Author information
Authors and Affiliations
Contributions
L.W. contributed to all parts of the study as the only author of the article.
Corresponding author
Ethics declarations
Competing Interests
The author declares no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, L. Value of serial cervical length measurement in prediction of spontaneous preterm birth in post-conization pregnancy without short mid-trimester cervix. Sci Rep 8, 15305 (2018). https://doi.org/10.1038/s41598-018-33537-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33537-1
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.