Abstract
Theta-burst stimulation (TBS) over the dorsolateral prefrontal cortex (DLPFC) may be more effective for modulating cortical excitability compared to standard repetitive transcranial magnetic stimulation. However, the impact of intermittent (iTBS) and continuous TBS (cTBS) on working memory (WM) is poorly studied. The aim of our study was to compare the effects of iTBS and cTBS on WM over the left and right DLPFC. iTBS, cTBS or sham stimulation was administered over the right and left hemisphere of fifty-one healthy human subjects. WM was assessed before and after TBS using the 1-back, 2-back, and 3-back tasks. We found classical practice effects in the iTBS and the sham group: WM performance improved following stimulation as measured by the discriminability index. However, this effect could not be observed in the cTBS group. We did not find any hemisphere-dependent effects, suggesting that the practice effect is not lateralized, and TBS affects WM performance in a comparable manner if administered either over the left or the right hemisphere. We propose that our findings represent a useful addition to the literature of TBS-induced effects on WM. Moreover, these results indicate the possibility of clarifying processes underlying WM performance changes by using non-invasive brain stimulation.
Similar content being viewed by others
Introduction
Non-invasive brain stimulation has become a highly prosperous field of cognitive research in the last few decades. One of the available methods is repetitive transcranial magnetic stimulation (rTMS), that involve the application of rapid, brief magnetic fields to the scalp. These magnetic fields induce a current in the underlying tissues, leading to the depolarization of neurons in the targeted brain area1. Administering high-frequency rTMS (above 5 Hz) over the dorsolateral prefrontal cortex (DLPFC) has been shown to improve working memory (WM). In contrast, applying low-frequency (≤1 Hz) rTMS results in performance disruption2,3,4. A relatively new and seemingly more effective alternative to rTMS is theta-burst stimulation (TBS), which uses gamma frequency trains applied at theta rhythm5. The pattern of TBS was designed to mimic theta-gamma coupling, i.e. the modulation of gamma power by theta phase6. This type of cross-frequency coupling serves as a tool for realizing effective coordination between several cortical areas during cognitive tasks7,8,9. Thus, it might be capable of inducing behavioral effects as theta-gamma coupling is involved in WM and long-term memory processes8,10,11,12. Two main type of TBS can be distinguished: the intermittent TBS (iTBS) is described as facilitating13, while the continuous TBS (cTBS) is expected to be suppressive on cortical excitability14. However, in the motor domain, TBS after-effects have been found to be highly variable across subjects15,16,17,18. Despite the advantages of TBS (its specific pattern, shorter stimulation period and longer-lasting effects, at least in the motor domain)5,19, to date, only a few studies investigated the impact of TBS on WM20. Here we present a study comparing iTBS- and cTBS-induced effects on WM both over the right and left DLPFC.
Previous studies have found different effects of cTBS and iTBS on several cognitive domains. Interestingly, the distinct protocols did not consistently lead to opposite behavioral outcomes20,21. Three recent studies have investigated the effect of iTBS administration over the left DLPFC. Increased theta weighted phase-lag index between frontoparietal regions and increased parietal gamma power has been found following iTBS along with behavioral improvement in the n-back WM task22. Enhanced amplitudes of TMS-evoked event-related potentials23, as well as increased theta and gamma power, have also been detected by Chung et al.24. However, in these studies, consistent behavioral improvement could not be revealed23,24. On the other hand, cTBS over the DLPFC has been reported to impair WM25,26 and also to decrease theta power27. Given these inconsistencies, a systematic investigation of cTBS- and iTBS-related impact on WM and direct comparisons of the effect of the two stimulation protocols with the same stimulation parameters on WM are needed.
A recent study has compared changes in performance on several neurocognitive tests, both following iTBS and cTBS. WM performance decreased following both active stimulation protocols considering reaction times, as reflected by a diminished practice effect. However, only cTBS had a disruptive effect on task accuracy21. This suggests that cTBS does not (only) disrupt WM itself but (also) the capacity to improve in a WM task. Although practice effects have been considered to be a confounding factor in cognitive measurements, practice-related changes - as a tool to measure cognitive plasticity28 – also yield useful information about the underlying mechanism of cognitive performance29,30. It is currently not known whether the mechanism behind the practice-related improvement (i.e. the ability to learn task-specific skills) in a WM task can be interfered by a single session of non-invasive stimulation. This question might also be relevant for the interpretation of TBS effects on brain plasticity, which is a key mechanism for learning and memory16,18.
The above-mentioned TBS-studies have applied stimulation over the left DLPFC only. Thus, effects of TBS administration over the right hemisphere also remain an open question. A recent study has found that left but not right cTBS induces bilateral blood oxygenation changes in the prefrontal area31, and dopamine release is enhanced only following left DLPFC stimulation32. From the behavioral perspective, a direct comparison of TBS effects on WM over the left and right DLPFC is lacking in the current literature. Traditional TMS studies have found that verbal WM appears to be modified by left but not right DLPFC stimulation33,34. Others have reported rTMS to effectively modulate WM both over the left and the right DLPFC3,35,36,37,38. However, in some cases, the effects of rTMS over the right DLPFC have only been prominent for WM tasks containing spatial39,40 or negatively valenced stimuli41,42. Thus, clarifying whether DLPFC stimulation over the left and the right hemisphere is associated with verbal WM changes is warranted.
The above-mentioned gaps in the literature have raised the following questions for our study: (1) is iTBS improving and cTBS worsening WM performance, (2) are left and right DLPFC stimulation leading to different consequences considering their distinct effect on WM performance? Therefore, we administered iTBS, cTBS or sham stimulation over the left and right DLPFC of healthy participants. The n-back task, a well-established approach for WM assessment, has been administered twice: once before and once after the stimulation. Hoy et al. found behavioral improvement on WM tasks, as well as increased fronto-parietal theta synchronization and parietal gamma band power following iTBS22. Therefore, we expected an increase in performance on the n-back task following iTBS administration. Opposite behavioral and electrophysiological effects using cTBS have been reported by Schicktanz et al.25 and Chung et al.24, respectively. Thus, we hypothesized that cTBS would decrease WM performance. Our third hypothesis was that the effects related to TBS would not be equal over the two hemispheres. Based on previous findings, we expect more pronounced results following left DLPFC stimulation compared to right DLPFC stimulation31,33,34,43.
Results
Overview
A total of fifty-one participants completed the study. Subjects received iTBS, cTBS or sham stimulation over the DLPFC. At two separate occasions, the left and right hemisphere were stimulated, respectively. The n-back working memory task (1-back, 2-back, and 3-back) was completed by the participants both prior to and following the stimulation. Performance was assessed by reaction times and d′ scores.
Pre-stimulation RTs and d’ scores
We did not find pre-stimulation differences between groups regarding both median RTs and d′ scores. This is supported by non-significant GROUP main effects and the lack of interactions including GROUP (all p > 0.05) (for details, see Supplementary Tables S1 and S2). These results indicate an equal pre-stimulation performance of the three groups for all administered levels of the n-back task and for each condition.
Median RTs
The mixed ANOVA for median RTs revealed a significant main effect of TIME (F(1,48) = 8.763, p = 0.005, np2 = 0.154). Post-hoc tests showed slightly shorter overall median RTs following stimulation (mean scores: pre-stimulation 0.618 s ± 0.012 SE; post-stimulation 0.600 s ± 0.011 SE). An additional main effect of LOAD was found (F(2,96) = 115.233, p < 0.001, np2 = 0.706), indicating increasing RTs with higher cognitive demand (mean scores: 0.499 s ± 0.009 SE for 1-back; 0.609 s ± 0.014 SE for 2-back; 0.719 s ± 0.017 SE for 3-back). The interaction of the two main effects was also found to be significant (F(1,96) = 4.947, p = 0.009, np2 = 0.093). Post-hoc comparison revealed that the difference between the two time points was detectable for the 2-back (F(1,48) = 9.137, p = 0.004, np2 = 0.160) and 3-back level (F(1,48) = 6.519 p = 0.014, np2 = 0.120), but not for 1-back (F(1,48) = 0.591, p = 0.446, np2 = 0.012, BF10 = 0.200). The above interaction was not modified by GROUP (F(4,96) = 1.358, p = 0.254, np2 = 0.054), or by SIDE (F(1.689,81.095) = 0.314, p = 0.694, np2 = 0.007). To clarify whether there is truly no difference related to stimulation type, or our data are just not sensitive enough to detect the difference, we calculated Bayes-factor excluding (H0) and including (H1) the effect of GROUP. The Bayes-factor model indicated a strong evidence for H0 (BF10 = 0.050). We applied the similar algorithm for SIDE, indicating strong evidence in favor of H0 (BF10 = 0.064).
d’ scores
The ANOVA of d′ scores revealed a significant main effect of LOAD (F(1,48) = 344.822, p < 0.001, np2 = 0.878), as well as TIME (F(1,48) = 30.297, p < 0.001, np2 = 0.387). Post-hoc tests showed better performance on the 2-back compared to 3-back condition, indicating a higher cognitive demand for the 3-back condition (mean scores: 3.575 ± 0.065 SE for 2-back; 2.125 ± 0.088 SE for 3-back). As for the main effect of TIME, increased performance was found following stimulation, signaling a potential practice effect between the two time points (mean scores: 2.708 ± 0.072 SE for pre-stimulation; 2.992 ± 0.071 SE for post-stimulation). Notably, a significant TIME × GROUP interaction was detected (F(2,48) = 4.252, p = 0.02, np2 = 0.151). To further analyze the source of this interaction, pairwise comparison with estimated marginal means was applied. We found a difference between the two time points in the iTBS (F(1,48) = 12.095, p = 0.001, np2 = 0.201) and the sham group (F(1,47) = 25.113, p < 0.001, np2 = 0.343), but this did not apply for the cTBS group (F(1,48) = 0.999, p = 0.323, np2 = 0.02, BF10 = 0.398) (Fig. 1). The interaction above was not modified by SIDE (F(1,48) = 0.198, p = 0.821, np2 = 0.008). To support the finding that SIDE as a factor has no critical effect on the detected interaction, Bayes-factors were calculated excluding (H0) and including (H1) for the effect of SIDE. In this model, Bayes-factor indicated strong evidence in favor of H0 (BF10 = 0.096).
Discussion
In the current study, we aimed to investigate the effects of iTBS and cTBS delivered over the right and left DLPFC on two repeated measurements of WM performance. The n-back task has been administered before and after stimulation. The expected practice effect (i.e. general improvement due to repeated task completion44) occurred in the iTBS and sham stimulation group. This was reflected by the discriminability index. However, cTBS eliminated the practice effect and thus reducing WM performance. Considering RTs, practice-related effects occurred independently of stimulation type. Moreover, we detected a similar impact of TBS on both hemispheres. Bayesian statistics further support our findings obtained with more classical statistical approaches.
TBS has been shown to modulate brain activity by mimicking theta-gamma coupling5 which is a key feature for realizing coordination during cognitive tasks7,8,9. Thus, the effect of TBS is expected to modulate WM based on the theta-gamma neural code11. Previous studies have found a disruptive effect of cTBS on WM measured by behavioral methods25,26. Therefore, our results suggesting reduced WM performance (i.e. lack of improvement) following cTBS are in line with previous findings. We might argue that cTBS affected WM performance by causing long-term depression-like effects or by impairing the dopaminergic transmission in networks involving the DLPFC5,32,45. Besides that, the modulation of theta-gamma oscillations could also play a role in the cTBS-related WM effects. Studies have found cTBS to increase the power of theta-gamma frequency oscillations over the DLPFC, whereas iTBS has been reported to increase it22,23,27.
Contrary to our hypothesis, a lack of iTBS effects was found in the current study. iTBS has been reported to enhance task-related theta-gamma synchronization between frontal and parietal areas22,24, and subtle effects of iTBS on WM have also been shown22. However, some recent studies have also failed to find behavioral enhancement after iTBS accompanied by oscillatory changes23,24. Behavioral modulations are difficult to show after a single session of stimulation of healthy individuals2, and the behavioral consequences of cTBS on cognition might be more stable than iTBS effects46. This assumption could partially explain why we only detected cTBS-related changes on the behavioral level. Studies show that iTBS is more likely to alter electrophysiological markers (i.e. to cause differences in the features of event-related potentials, to change the degree of theta-gamma coupling or power in the crucial frequency ranges) than to cause behavioral changes23,24. Thus, iTBS might have had an effect on the neural level, which was not manifested on the behavioral level. Nevertheless, as WM-related electrophysiological after-effects of cTBS are not revealed yet, further studies should be conducted to clarify the underlying mechanism of the cTBS-induced behavioral changes, also compared to iTBS.
We might also speculate that the revealed disruptive effect of cTBS was not necessarily specific to WM itself, but rather to the consolidation of task-specific skills. Therefore, practice effects might also be interpreted as task-related knowledge which would help participants to improve their performance on the second administration. This might be supported by the lack of practice effect reported in neurocognitive disorders47,48, which are characterized by deficits in memory consolidation and acquiring new information49. Considering that memory processes may be modified by TBS50,51, and theta frequency oscillations are associated with memory consolidation processes12, it might be possible that prefrontal stimulation affected the consolidation of task-related skills. Future studies assessing whether consolidation may also play a role in TBS-related WM performance changes, seem warranted.
We did not find practice effects to occur in the 1-back condition. This supports the assumption that the changes detected here are WM-dependent to some extent and not solely associated with a more general task-related skill learning ability. Practice-related effects have been previously described to be independent of task difficulty52. However, different levels of performance modulation (or the lack of practice-related behavioral changes) following sham TBS have been found on several neuropsychological tasks21. A recent study has also revealed that the practice effect consists of various sub-processes, which are differently affected by the repeated completion of the task53. In the current study, processing speed was not modulated by TBS, thus supporting the notion that the applied stimulation affected only sub-processes defining WM performance. Nevertheless, the question if the measured effects originate from alterations in task-independent model-building processes or from solely WM-related changes remains in the focus of interest for future research. This could be addressed by measuring TBS-induced changes on the practice effect using other executive function tests with less WM demand (for example, Attention Network Task54). Additionally, the longitudinal assessment of practice effects (i.e. through multiple testing sessions) could reveal its dynamics and potential specificities. To sum up, we suggest that the disruption of practice effects related to cTBS might serve as a helpful concept to explain the inhibitory influence of cTBS on cognitive performance, whereas iTBS appears to be less robust than cTBS in this aspect.
Previous rTMS findings have reported bilateral contribution or even right DLPFC superiority for WM tasks using different cognitive targets3,35,36,37,39,40,42. In contrast, an early TMS study has suggested the left DLPFC stimulation leads to verbal WM performance modulation33. Interestingly, neuroimaging data have also suggested left DLPFC superiority for WM43. The n-back task used here was verbally featured, with no spatial or emotional aspects, which could partially explain the equal effects of TBS over the left and right hemisphere. We might argue that the left and right DLPFC play a similar role in the tested WM-related learning ability. Another possible explanation might be that disrupting activity in either hemisphere provokes an imbalance between the hemispheres that results in impaired performance55. This would also mean that enhancing activity using iTBS or high-frequency rTMS on one hemisphere could cause an imbalance that ultimately reduces performance. In studies using facilitatory TMS-methods either increase or a lack of change in performance has been detected2,46. This makes the hemispheric imbalance explanation less plausible. However, future studies specifically addressing this issue are required. Our current results further support the notion that WM-related processes can be equally modulated by TBS over either hemisphere in healthy individuals.
The stimulation intensity is crucial for the interpretation of our results considering that it differed remarkably from the intensity levels applied by previous studies testing the effects of TBS on WM. Nevertheless, cognitive changes have been described previously with comparable or even lower intensities56,57,58. The average MT of our participants was approximately 60% of the MSO. Thus, the stimulation intensity level was at nearly 50% of MT, compared to 80% of MT typically used in similar studies22,25. Consequently, we might speculate that cTBS exerts its effect on WM at low intensity, whereas iTBS might require higher intensities to have a more prominent or longer-lasting effect on WM performance. Additionally, iTBS and cTBS are characterized by distinct electrophysiological parameters, with the ideal stimulation intensity also differing if applied over motor cortical areas5. Similar to our findings, a diminished practice effect on n-back performance following cTBS has been previously found when comparing it to iTBS and sham stimulation21. The stimulation intensity applied by Viejo-Sobera et al.21 was 80% of the active motor threshold. This value is lower compared to motor threshold measured without voluntary contraction, typically by 5–20% of the MSO59. Thus, the level of intensity was comparable to our administration but lower than in studies reporting an increase in WM performance following iTBS22. Additionally, a recent study aimed to identify the ideal stimulation intensity for iTBS to modulate WM. This revealed an inverse U-shaped pattern of the different stimulation intensity effects, with nearly 75% of resting MT resulting in the largest neurophysiological changes. Nevertheless, 50% of resting MT also influenced neurophysiological functioning - but not at the behavioral level24. Exact data on the ideally recommended stimulation intensity of cTBS to affect WM is not yet available, therefore, future studies should address this issue. We strongly believe that our current results shed further light on potentially distinct but optimal stimulation intensities of different TBS protocols. This is supported by the disruptive effect of cTBS at the applied intensity, whereas iTBS remained ineffective at the same intensity.
In the present study, we found cTBS to have an inhibitory influence on the practice effect during the n-back task, while iTBS did not exert this fundamental effect. Our findings suggest that (1) the two distinct stimulation protocols presumably exert different effects on measured cognitive abilities, and (2) stimulation of the left or right DLFPC might have equivalent effects on WM at the behavioral level. Furthermore, in the light of previously reported neurophysiological changes related to WM following TBS administration22,24,25, future studies should examine post-TBS neuronal responses if stimulating both hemispheres. The role of practice underlying WM performance alterations and its interaction with TBS should be systematically explored in the future. The current results also emphasize the importance of investigating effects of low-intensity TBS on cognitive function and the potential differences of the ideal stimulation intensity for iTBS and cTBS to modulate WM. Above this, the assumption that iTBS and cTBS are defined by distinct ideal stimulation intensity levels could well influence the design of TBS-based treatment protocols. We strongly believe that the current findings represent a useful addition to the process of developing effective ways to reveal the influence of iTBS and cTBS on WM and to clarify the sub-processes behind WM changes by using non-invasive brain stimulation.
Methods
Participants
The selected sample size was based on an a priori sample size estimation. We calculated the required sample size with a medium estimated effect size, as TBS-induced effect sizes were found to be larger than in rTMS studies5,22. To find group differences between the three groups and within two repeated measurements with a power of 0.85, and assuming a medium effect size of 0.5, the required sample size was 48. Fifty-two healthy volunteers were recruited to participate in the study (see Table 1 for demographic data). None of the subjects had a history of any psychiatric or neurological disorder at the time of the participation. All participants had normal or corrected-to-normal vision. Participants were randomly assigned to one of the three groups and were naïve to the stimulation type. Informed consent was signed by all participants prior to the first session, and none of them withdrew from the experiment because of TBS discomfort. We had to exclude one participant due to administration failure in the first session. Thus, final analysis was carried out including fifty-one participants. The study was conducted in accordance with the Declaration of Helsinki, and the experimental protocol was approved by the Regional Scientific and Research Ethics Committee, Albert Szent-Györgyi Health Center, University of Szeged (Ref. no.: 165/2014).
Experimental design
The examination was performed in two separate sessions. At least two weeks of washout period was kept between the two occasions. During both sessions, all participants completed three levels of the n-back task before and after stimulation. Either the right or the left DLPFC was stimulated during the first examination, with the other hemisphere on the second occasion, respectively. The order of stimulation side was counterbalanced across participants. Three groups were formed: eighteen out of the fifty-one participants were given iTBS, seventeen of them received cTBS, and sixteen participants were assigned to the sham stimulation group. The experimental protocol was identical in each group, except for the type of stimulation.
N-back task
The 1-back, 2-back, and 3-back version of the n-back task was administered consecutively60 using PsychoPy (version: v1.82.01)61. During the n-back tasks, random capital letter stimuli (A, C, E, I, K, L, S, O, R, T, U) were presented serially on the screen for 1500 ms with an interstimulus interval of 500 ms. Participants had to respond by pressing the space bar if the letter on the screen was the same as the letter presented one (1-back task), two (2-back task) or three (3-back task) trials earlier (Fig. 2). A total of 100 trials was completed at each level meaning a total of 300 trials per measurement. The frequency of target stimuli was set at 20% of all presented stimuli. The total duration of the tasks was about 15 minutes. We assumed that post-stimulation effects lasted during the entire examination, based on previous studies using TBS to modulate cognitive performance22,25. Reaction times (RT), number of hits, correct rejections, false alarms and misses were recorded.
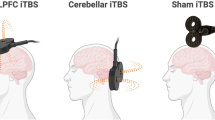
Theta-burst stimulation protocol
TBS was generated by a Magstim Rapid2 stimulator with a D702 70 mm figure-of-eight coil (The Magstim Company Ltd, Whitland, Wales, UK). Prior to the experiment, each participant in the iTBS and cTBS group went through an anatomical T1-weighted MRI-scan using a 1.5T GE Signa Excite HDxt scanner (Milwaukee, WI, USA): 3D IR-FSPGR: TR/TE/TI: 10.3/4.2/450 ms; flip angle: 15; ASSET: 2, FOC: 25 × 25 cm; matrix: 256 × 256; slice thickness: 1 mm. A TMS Neuronavigator (Brain Innovation, Maastricht, the Netherlands) with ultrasound CMS20 Measuring System (Zebris GmbH, Tübingen, Germany) was used to localize the target position on the scalp of each participant. Prior to this, 3D-brain models were created using participants’ MRI scans for accurate and individual targeting. Right and left DLPFC has been marked as the target area located on the 3D surface rendering of the brain, based on each participants’ gyral morphology (the anterior third of the middle frontal gyrus, Brodmann 9/46). We positioned the center of the coil over the target area, tangentially to the skull, with the handle pointing backward. During sham stimulation, the coil was rotated 45° away from the skull, with one wing of the coil being in contact with the scalp. Within the sham group, we administered the iTBS protocol for half of the participants, and cTBS pattern for the other half of the participants.
The cTBS and iTBS administration protocols in the current study was based on the original TBS stimulation pattern described by Huang et al.5. The cTBS pattern consisted of 3 pulses given at 50 Hz (gamma frequency) in every 200 ms (theta frequency intervals of 5 Hz) for 40 s. Thus, a total of 600 pulses of uninterrupted TBS was administered to each participant in the cTBS group. As for iTBS, a 2 s train was repeated every 10 s for 190 s in total. In one train, 3 pulses were given at 50 Hz, which resulted in 600 pulses for each subject in the iTBS group. The stimulation intensity was kept at 30% of the maximal stimulator output (MSO) of the Magstim Rapid2 stimulator, due to limitations in the maximal TBS intensity of the stimulator. We chose to administer equal intensity for all participants. This was based on evidence claiming that the individual adaptation of TMS intensity to the measured motor threshold does not necessarily lead to more prominent effects62. To make sure that the potential effects are not due to differences in the motor thresholds, we measured visible motor threshold (MT) without voluntary contraction prior to the two TBS sessions, at a separate occasion. It was defined as the lowest stimulation intensity applied over the right primary motor cortex (M1) required to elicit visible contraction of the left abductor pollicis brevis muscle in 3 out of 5 probes. If 80% of the individual MT did not reach 30% of MSO so that the intensity does not exceed the 80% of MT, the applied intensity was reduced by 20% of the MT. This occurred in one case in the cTBS group (27% of MSO) and in one case in the sham group (29% of MSO). The mean rMTs and ranges are given in Table 2. There was no difference between groups in terms of the mean rMT (F(2,48) = 1.325, p = 0.275, np2 = 0.52, BF10 = 0.385).
Statistical analysis
For statistical analysis with the frequentist approach, IBM SPSS Statistics 24.0 software package was used. N-back performance was evaluated by two scores: median reaction times (RT) and discriminability index (d′) used in the framework of signal detection theory63. We chose to use median RTs over mean scores to avoid the confounding effect of invalid (i.e. extremely short or extremely long) RTs64. For calculating d′ scores, we distinguished four types of answers: hits (correctly identified targets), misses (incorrectly identified targets as non-targets), false alarms (incorrectly identified non-targets as targets), and correct rejections (correctly identified non-targets). The d′ value is a highly sensitive statistical index involving both the ability to maximize hits and the efficiency of minimizing false alarms. It is calculated from the standard deviation of the signal and the noise distribution, with higher scores representing more readily detected signals (therefore greater discriminability)65. d′ scores were calculated individually as:
We analyzed RTs by a 3 × 2 × 2 × 2 mixed ANOVA with the cognitive load (LOAD: 1. 1-back; 2. 2-back; 3. 3-back), the time of administration (TIME: 1. pre-stimulation; 2. post-stimulation) and the side of the stimulation (SIDE: 1. right DLPFC; 2. left DLPFC) as within-subject factors, and stimulation type (GROUP: 1. iTBS; 2. cTBS; 3. sham) as between-subject factor. Considering that participants completed the 1-back task with an extremely high accuracy (99.53% in total), d′ scores were not calculated for this task. Thus, d′ scores have been analyzed by a 2 × 2 × 2 × 2 mixed ANOVA with the same parameters as for the RTs, excluding the 1-back condition. Pairwise comparisons of estimated marginal means (with Bonferroni correction for multiple testing) was used for follow-up on the significant main effects and interactions. Prior to analyzing TBS-induced effects, an additional mixed ANOVA with LOAD and SIDE as within-subject factors, and with GROUP as a between-subject factor was carried out, to test whether the three groups differed in terms of their pre-stimulation performance (factor levels were the same as previously defined).
In addition to the more conventional frequentist statistical approach, we also calculated Bayes-factors (BF) for the underpinning of our non-significant, but relevant results. Although the classical null-hypothesis testing mainly relies on the p-value, it is important to keep in mind that a non-significant result could mean at least two different things: (1) the null hypothesis is true; or (2) the collected data are not sensitive enough to distinguish between the null and an alternative hypothesis66. BF could be considered as the weight of evidence provided by the collected data, helping to differentiate between these two options67. Therefore, to compare the likelihood of our models favoring the H0 versus the H1 hypothesis, we performed Bayesian ANOVAs using JASP 0.8.03.0168 carried out by default prior. Here we report BF10 values that should be interpreted as follows: BF10 values between 1 and 0.33 indicate anecdotal, values between 0.33 and 0.1 substantial, and values below 0.1 strong evidence for H0. Reversely, values between 1 and 3 indicate anecdotal, values between 3 and 10 substantial, and values above 10 strong evidence in favor of H167.
References
Hallett, M. Transcranial magnetic stimulation: a primer. Neuron 55, 187–199 (2007).
Brunoni, A. R. & Vanderhasselt, M.-A. Working memory improvement with non-invasive brain stimulation of the dorsolateral prefrontal cortex: A systematic review and meta-analysis. Brain Cogn. 86, 1–9 (2014).
Mottaghy, F. M., Döring, T., Müller-Gärtner, H. W., Töpper, R. & Krause, B. J. Bilateral parieto-frontal network for verbal working memory: An interference approach using repetitive transcranial magnetic stimulation (rTMS). Eur. J. Neurosci. 16, 1627–1632 (2002).
Lage, C., Wiles, K., Shergill, S. S. & Tracy, D. K. A systematic review of the effects of low-frequency repetitive transcranial magnetic stimulation on cognition. J. Neural Transm. 123, 1479–1490 (2016).
Huang, Y. Z., Edwards, M. J., Rounis, E., Bhatia, K. P. & Rothwell, J. C. Theta burst stimulation of the human motor cortex. Neuron 45, 201–206 (2005).
Lisman, J. & Buzsáki, G. A neural coding scheme formed by the combined function of gamma and theta oscillations. Schizophr. Bull. 34, 974–980 (2008).
Niessing, J. et al. Neuroscience: Hemodynamic signals correlate tightly with synchronized gamma oscillations. Science (80-.). 309, 948–951 (2005).
Axmacher, N. et al. Cross-frequency coupling supports multi-item working memory in the human hippocampus. Proc. Natl. Acad. Sci. 107, 3228–3233 (2010).
Canolty, R. T. et al. High gamma power is phase-locked to theta oscillations in human neocortex. Science (80-.). 313, 1626–1628 (2006).
Lisman, J. Working memory: The importance of theta and gamma oscillations. Curr. Biol. 20, R490–R492 (2010).
Lisman, J. E. & Jensen, O. The theta-gamma neural code. Neuron 77, 1002–1016 (2013).
Düzel, E., Penny, W. D. & Burgess, N. Brain oscillations and memory. Curr. Opin. Neurobiol. 20, 245–257 (2010).
Di Lazzaro, V. et al. The physiological basis of the effects of intermittent theta burst stimulation of the human motor cortex. J. Physiol. 586, 3871–3879 (2008).
Di Lazzaro, V. et al. Theta-burst repetitive transcranial magnetic stimulation suppresses specific excitatory circuits in the human motor cortex. J. Physiol. 565, 945–50 (2005).
Hamada, M., Murase, N., Hasan, A., Balaratnam, M. & Rothwell, J. C. The role of interneuron networks in driving human motor cortical plasticity. Cereb. Cortex 23, 1593–1605 (2013).
Vallence, A. M. et al. Inter- and intra-subject variability of motor cortex plasticity following continuous theta-burst stimulation. Neuroscience 304, 266–278 (2015).
Jannati, A., Block, G., Oberman, L. M., Rotenberg, A. & Pascual-Leone, A. Interindividual variability in response to continuous theta-burst stimulation in healthy adults. Clin. Neurophysiol. 128, 2268–2278 (2017).
Tse, N. Y. et al. The effect of stimulation interval on plasticity following repeated blocks of intermittent theta burst stimulation. Sci. Rep. 8, 8526 (2018).
Suppa, A. et al. Ten years of theta burst stimulation in humans: established knowledge, unknowns and prospects. Brain Stimul. 9, 323–335 (2016).
Demeter, E. Enhancing cognition with theta burst stimulation. Curr. Behav. Neurosci. Reports 3, 87–94 (2016).
Viejo-Sobera, R. et al. Impact of prefrontal theta burst stimulation on clinical neuropsychological tasks. Front. Neurosci. 11, 462 (2017).
Hoy, K. E. et al. Enhancement of working memory and task-related oscillatory activity following intermittent theta burst stimulation in healthy controls. Cereb. Cortex 1–11, https://doi.org/10.1093/cercor/bhv193 (2016).
Chung, S. W., Rogasch, N. C., Hoy, K. E. & Fitzgerald, P. B. The effect of single and repeated prefrontal intermittent theta burst stimulation on cortical reactivity and working memory. Brain Stimul. 11, 566–574 (2018).
Chung, S. W. et al. Impact of different intensities of intermittent theta burst stimulation on the cortical properties during TMS-EEG and working memory performance. Hum. Brain Mapp. https://doi.org/10.1002/hbm.23882 (2017).
Schicktanz, N. et al. Continuous theta burst stimulation over the left dorsolateral prefrontal cortex decreases medium load working memory performance in healthy humans. PLoS One 10, e0120640 (2015).
Lee, T. G. & D’Esposito, M. The dynamic nature of top-down signals originating from prefrontal cortex: a combined fMRI-TMS study. J. Neurosci. 32, 15458–15466 (2012).
Chung, S. W. et al. Demonstration of short-term plasticity in the dorsolateral prefrontal cortex with theta burst stimulation: A TMS-EEG study. Clin. Neurophysiol. 128, 1117–1126 (2017).
Calero, M. D. & Navarro, E. Relationship between plasticity, mild cognitive impairment and cognitive decline. Arch. Clin. Neuropsychol. 19, 653–660 (2004).
Duff, K. et al. Practice effects in the prediction of long-term cognitive outcome in three patient samples: A novel prognostic index. Arch. Clin. Neuropsychol. 22, 15–24 (2007).
Duff, K., Callister, C., Dennett, K. & Tometich, D. Practice effects: A unique cognitive variable. Clin. Neuropsychol. 26, 1117–1127 (2012).
Tupak, S. V. et al. Inhibitory transcranial magnetic theta burst stimulation attenuates prefrontal cortex oxygenation. Hum. Brain Mapp. 34, 150–157 (2013).
Ko, J. H. et al. Theta burst stimulation-induced inhibition of dorsolateral prefrontal cortex reveals hemispheric asymmetry in striatal dopamine release during a set-shifting task - A TMS-[11C]raclopride PET study. Eur. J. Neurosci. 28, 2147–2155 (2008).
Mull, B. R. & Seyal, M. Transcranial magnetic stimulation of left prefrontal cortex impairs working memory. Clin. Neurophysiol. 112, 1672–1675 (2001).
Shields, J., Mock, J., Devier, D. & Foundas, A. Unilateral repetitive transcranial magnetic stimulation differentially affects younger and older adults completing a verbal working memory task. J. Neurol. Sci. 384, 15–20 (2017).
Mottaghy, F. M. et al. Modulation of the neuronal circuitry subserving working memory in healthy human subjects by repetitive transcranial magnetic stimulation. Neurosci. Lett. 280, 167–170 (2000).
Preston, G., Anderson, E., Silva, C., Goldberg, T. & Wassermann, E. M. Effects of 10 Hz rTMS on the neural efficiency of working memory. J. Cogn. Neurosci. 22, 447–456 (2010).
Hamidi, M., Tononi, G. & Postle, B. R. Evaluating the role of prefrontal and parietal cortices in memory-guided response with repetitive transcranial magnetic stimulation. Neuropsychologia 47, 295–302 (2009).
Hulst, H. E. et al. RTMS affects working memory performance, brain activation and functional connectivity in patients with multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 88, 386–394 (2017).
Sandrini, M., Rossini, P. M. & Miniussi, C. Lateralized contribution of prefrontal cortex in controlling task-irrelevant information during verbal and spatial working memory tasks: rTMS evidence. Neuropsychologia 46, 2056–2063 (2008).
Fried, P. J., Rushmore, R. J., Moss, M. B., Valero-Cabré, A. & Pascual-Leone, A. Causal evidence supporting functional dissociation of verbal and spatial working memory in the human dorsolateral prefrontal cortex. Eur. J. Neurosci. 39, 1973–1981 (2014).
Weigand, A. et al. State-dependent effects of prefrontal repetitive transcranial magnetic stimulation on emotional working memory. Brain Stimul. 6, 905–912 (2013).
Weigand, A. et al. Lateralized effects of prefrontal repetitive transcranial magnetic stimulation on emotional working memory. Exp. Brain Res. 227, 43–52 (2013).
Wager, T. D. & Smith, E. E. Neuroimaging studies of working memory: A meta-analysis. Cogn. Affect. Behav. Neurosci. 3, 255–274 (2003).
Calamia, M., Markon, K. & Tranel, D. Scoring higher the second time around: Meta-analyses of practice effects in neuropsychological assessment. Clin. Neuropsychol. 26, 543–570 (2012).
Rossini, P. M. et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: Basic principles and procedures for routine clinical and research application: An updated report from an I.F.C.N. Committee. Clin. Neurophysiol. 126, 1071–1107 (2015).
Lowe, C. J., Manocchio, F., Safati, A. B. & Hall, P. A. The effects of theta burst stimulation (TBS) targeting the prefrontal cortex on executive functioning: A systematic review and meta-analysis. Neuropsychologia 111, 344–359 (2018).
Duff, K. et al. Practice effects predict cognitive outcome in amnestic mild cognitive impairment. Am. J. Geriatr. Psychiatry 19, 932–939 (2011).
Ivnik, R. J. et al. Diagnostic accuracy of four approaches to interpreting neuropsychological test data. Neuropsychology 14, 163–177 (2000).
Weintraub, S., Wicklund, A. H. & Salmon, D. P. The neuropsychological profile of Alzheimer disease. Cold Spring Harb. Perspect.Med. 2, a006171 (2012).
Demeter, E., Mirdamadi, J. L., Meehan, S. K. & Taylor, S. F. Short theta burst stimulation to left frontal cortex prior to encoding enhances subsequent recognition memory. Cogn. Affect. Behav. Neurosci. 16, 724–735 (2016).
Blumenfeld, R. S., Lee, T. G. & D’Esposito, M. The effects of lateral prefrontal transcranial magnetic stimulation on item memory encoding. Neuropsychologia 53, 197–202 (2014).
Reeve, C. L. & Lam, H. The relation between practice effects, test-taker characteristics and degree of g-saturation. Int. J. Test. 7, 225–242 (2007).
Dutilh, G., Krypotos, A. M. & Wagenmakers, E. J. Task-related versus stimulus-specific practice: A diffusion model account. Exp. Psychol. 58, 434–442 (2011).
Fan, J., McCandliss, B. D., Sommer, T., Raz, A. & Posner, M. I. Testing the efficiency and independence of attentional networks. J. Cogn. Neurosci. https://doi.org/10.1162/089892902317361886 (2002).
Grimm, S. et al. Imbalance between left and right dorsolateral prefrontal cortex in major depression is linked to negative emotional judgment: an fMRI study in severe major depressive disorder. Biol. Psychiatry 63, 369–376 (2008).
Verbruggen, F., Aron, A. R., Stevens, M. A. & Chambers, C. D. Theta burst stimulation dissociates attention and action updating in human inferior frontal cortex. Proc. Natl. Acad. Sci. 107, 13966–13971 (2010).
Dambacher, F. et al. The role of right prefrontal and medial cortex in response inhibition: interfering with action restraint and action cancellation using transcranial magnetic brain stimulation. J. Cogn. Neurosci. 26, 1775–1784 (2014).
Drummond, N. M., Cressman, E. K. & Carlsen, A. N. Offline continuous theta burst stimulation over right inferior frontal gyrus and pre-supplementary motor area impairs inhibition during a go/no-go task. Neuropsychologia 99, 360–367 (2017).
Chen, R. et al. Intracortical inhibition and facilitation in different representations of the human motor cortex. J. Neurophysiol. 80, 2870–81 (1998).
Gevins, A. & Cutillo, B. Spatiotemporal dynamics of component processes in human working memory. Electroencephalogr. Clin. Neurophysiol. 87, 128–143 (1993).
Peirce, J. W. PsychoPy-Psychophysics software in Python. J. Neurosci. Methods 162, 8–13 (2007).
Kaminski, J. A., Korb, F. M., Villringer, A. & Ott, D. V. M. Transcranial magnetic stimulation intensities in cognitive paradigms. PLoS One 6, e24836 (2011).
Stanislaw, H. & Todorov, N. Calculation of signal detection theory measures. Behav. Res. Methods, Instruments, {&} Comput. 31, 137–149 (1999).
Ulrich, R. & Miller, J. Effects of outlier exclusion on reaction time analysis. J. Exp. Psychol. Gen., https://doi.org/10.1037//0096-3445.123.1.34 (1991).
Haatveit, B. C. et al. The validity of d prime as a working memory index: results from the ‘Bergen n-back task’. J. Clin. Exp. Neuropsychol. 32, 871–880 (2010).
Dienes, Z. Using Bayes to get the most out of non-significant results. Front. Psychol. 5, 781 (2014).
Wagenmakers, E., Wetzels, R., Borsboom, D. & van der Maas, H. L. J. Why psychologists must change the way they analyze their data: The case of psi: Comment on Bem (2011). J. Pers. Soc. Psychol. 100, 426–432 (2011).
JASP Team. JASP (Version 0.8.3.1) [Computer software] (2017).
Acknowledgements
The study was supported by the National Brain Research Program (Grant No. KTIA_13_NAP-A-II/20) and by the Human Resource Development Operational Programme (Grant No. EFOP-3.6.1-16-2016-00008) providing support for study equipment and conduction. A.M. received support from the Bolyai Scholarship Program of the Hungarian Academy of Sciences. A.M. was supported by the UNKP-17-4 and T.V. by the UNKP-17-3 New National Excellence Program of the Ministry of Human Capacities during study conduction and manuscript preparation. We are grateful to D.N. for his incredibly useful comments on the drafts of the manuscript.
Author information
Authors and Affiliations
Contributions
T.V. participated in data acquisition, data management, analyzed data and wrote the manusript; V.L.N. designed the study and participated in data acquisiton; A.H. participated in data acquisition, K.K. participated in data acquisition, Zs.T.K. designed the study; L.V. designed the study, A.M. designed the study and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vékony, T., Németh, V.L., Holczer, A. et al. Continuous theta-burst stimulation over the dorsolateral prefrontal cortex inhibits improvement on a working memory task. Sci Rep 8, 14835 (2018). https://doi.org/10.1038/s41598-018-33187-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33187-3
Keywords
This article is cited by
-
Cognitive Effects Following Offline High-Frequency Repetitive Transcranial Magnetic Stimulation (HF-rTMS) in Healthy Populations: A Systematic Review and Meta-Analysis
Neuropsychology Review (2024)
-
Lack of effects of eight-week left dorsolateral prefrontal theta burst stimulation on white matter macro/microstructure and connection in autism
Brain Imaging and Behavior (2024)
-
Synaptic plasticity and mental health: methods, challenges and opportunities
Neuropsychopharmacology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.