Abstract
Smartphone-based fundus photography (SBFP) allows for a cheap and mobile fundus examination with the potential to revolutionize eye care especially in low income settings. The purpose of this study was to assess the impact of pupil dilation on image quality in optic nerve head (ONH) imaging and vertical cup-to-disc ratio (vCDR) evaluation with SBFP. Eyes with glaucoma or suspected to have glaucoma were imaged with conventional digital fundus photography (CFP) and SBFP undilated and following dilation, all monoscopically. SBFP was possible in 74% of eyes without dilation and in 98% following dilation. Better image quality on SBFP was achieved with dilation and complete visualization of the optic disc rim was possible in 46% of images without dilation and on 94% of images with dilation. VCDR measurements on images obtained following dilation highly correlated with measurements on CFP (coefficient of correlation r = 0.91, p < 0.001), whereas vCDR on images obtained without dilation correlated less well with CFP (r = 0.70, p < 0.001). SBFP for ONH evaluation is promising, however dilation appears mandatory to achieve results comparable to optic disc evaluation on CFP. ONH imaging with smartphones without dilation might bear the risk of underestimating the CDR and hence overlooking patients at risk for glaucoma.
Similar content being viewed by others
Introduction
Smartphone-based fundus photography (SBFP) allows for a cheap and mobile fundus examination and documentation with the potential to revolutionize eye care especially in low income countries1,2,3,4. With the advent of SBFP multiple applications in ophthalmology have been accomplished including smartphone-based diabetic retinopathy screening5,6,7,8,9,10. Although optic nerve head (ONH) evaluation would be another natural application of SBFP, there is a dearth of literature on the application of SBFP for glaucoma screening to date11,12. As the vertical cup-to-disc ratio (vCDR) has proved to be a simple, relatively robust index of glaucomatous loss of the neuroretinal rim13,14, ONH evaluation using SBFP may be applicable in glaucoma screening. If the camera’s light beam and the illumination source are adequately coaxial, SBFP can even be performed without pupil dilation, which further simplifies its application15,16.
In the study by Russo et al. undilated SBFP with a D-Eye adapter and an iPhone 5 s was compared to undilated clinical 90D lens biomicroscopy for vCDR evaluation11. Agreement between the two modalities was good (kappa = 0.63) and SBFP was possible in 97% of the eyes (104 out of 107). However only undilated SBFP has been performed. Bastawrous and coworkers compared dilated SBFP with a Peek Retina adapter and a Samsung S3 to dilated conventional digital fundus photography for vCDR evaluation12. Also this study revealed good agreement (kappa = 0.69) and SBFP was possible in 80% of the eyes (2322 out of 2920).
With glaucoma being a major cause for irreversible blindness more studies on the applicability of SBFP for glaucoma screening and the evaluation of glaucomatous optic discs are warranted. The comparison of dilated to undilated SBFP with the latter being more feasible in a low income setting is of particular interest. So far, image quality and agreement in vCDR evaluation have not been compared between undilated and dilated SBFP. Thus we performed this study.
Methods
Subject recruitment
Patients were consecutively recruited from the glaucoma outpatient clinic at the Department of Ophthalmology of the University of Bonn, Germany. Ethical approval was obtained from the ethics committee of the University of Bonn and informed consent was obtained from all study participants prior to study inclusion. The Declaration of Helsinki was followed. Exclusion criteria were any retinal diseases and severe media opacities.
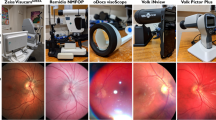
Image acquisition
Eyes were imaged with a Galaxy S4 (Samsung Electronics, Seoul, South Korea) using the D-Eye adapter (Fig. 1, version from 2016, D-EYE S.r.l., Padova, Italy) monoscopically first undilated and then dilated. The D-Eye adapter’s optics consist of a negative lens, a beam splitter, a mirror and polarized filters and allow for smartphone-based direct ophthalmoscopy15. Additionally eyes were imaged with conventional monoscopic fundus photography (CFP) (Visucam 500, Carl Zeiss Meditec, Jena, Germany), also dilated. The Galaxy S4 backside camera is equipped with a 12.8 megapixel CMOS (“complementary metal-oxide-semiconductor”) sensor and the Visucam 500 with a 5.0 megapixel CCD (“charge-coupled device”) sensor. The working distance for image acquisition was 10–30 mm for the Galaxy S4 with the D-Eye adapter and 40 mm for the Visucam 500. SBFP was performed by the same examiner, experienced in direct and indirect SBFP, in all patients (MWMW) in a darkened room. After 5 minutes of unsuccessful imaging attempts examination was aborted.
Image analysis
For analysis only the central circular part of the image was cropped using Image J17 in order to mask for the status of dilation. All images were pseudonymized and analyzed by two masked graders (MWMW and CKB). Image quality was graded using a six-step-scale with exemplary images based on vessel visibility (Fig. 2). Optic disc rim visualization and degree of optic disc pallor were evaluated using a respective three-step-scale with exemplary images (Figs 3 and 4). VCDR was evaluated by measuring the total ONH height and the height of the superior and inferior neuroretinal rim with Image J, entering the results in an Excel table and vCDR was automatically calculated. Statistical analyses were performed with R (R: A Language and Environment for Statistical Computing, R Core Team, R Foundation for Statistical Computing, Vienna, Austria, 2016). Photographic vCDR assessment on CFP was compared with assessment from the medical records based on stereoscopic slit lamp biomicroscopy. Weighted kappa (for image quality, optic disc pallor and degree of optic disc rim visualization) and intraclass correlation (for vCDR) were calculated to assess inter-observer reliability.
Image quality grading. Image quality (IQ) was graded on a 6-step-scale with these exemplary images for 0 = no fundus details visible, 1 = trail of major vessels visible (A), 2 = trail of medium size vessels visible (B), 3 = trail of some small vessels visible (C), 4 = trail of nearly all small vessels visible (D), 5 = even small vessels sharp (E).
Optic disc rim visualization. Degree of optic disc rim visualization was graded on a 3-step-scale with these exemplary images for 1 = less than ¾ of the optic disc rim identifiable (A), 2 = at least ¾ of the optic disc rim identifiable (B, the lower left of the optic disc rim is overlaid by a reflex) and 3 = optic disc rim completely identifiable (C).
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Results
Subject demographics and clinical characteristics
54 eyes (27 participants) were included in the study. All participants were imaged bilaterally. Characteristics of the sample are displayed in Table 1.
Evaluation of image quality and optic disc rim visualization
SBFP was possible in 74% without dilation and in 98% following dilation. Reasons for failure of SBFP were small pupil diameter, media opacity or the combination of both, based on subjective evaluation during examination. Mean image quality ± standard deviation (SD) on CFP and on dilated and undilated SBFP was 4.8 ± 0.36, 3.0 ± 0.50 and 2.4 ± 0.94, respectively (p < 0.001, Fig. 5A, for parametric testing see Table 2). Weighted kappa in between graders for image quality and degree of optic disc rim visualization were 0.73 and 0.83, respectively.
Evaluation of Image quality (A) and degree of optic disc rim visualization (B). Conventional fundus photography (CFP) and dilated (dil.) and undilated (undil.) smartphone-based fundus photography (SBFP) were compared. Error bars indicate standard error of the mean, paired t-test was used for analysis, asterisks indicate significant differences in regards to CFP if not otherwise indicated, *p < 0.05, ***p < 0.001.
Mean degree of optic disc rim visualization ± SD on CFP and on dilated and undilated SBFP was 3.0 ± 0, 2.9 ± 0.33 and 2.0 ± 0.79, respectively (Fig. 5B, for parametric testing see Table 2). Degree of optic disc rim visualization was nearly one step lower in undilated SBFP compared to dilated SBFP and CFP, whereas there was only a small difference between dilated SBFP and CFP.
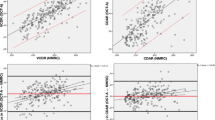
Evaluation of the optic nerve head
Mean vCDR ± SD on CFP and on dilated and undilated SBFP was 0.76 ± 0.14, 0.73 ± 0.13 and 0.68 ± 0.12, respectively. vCDR was underestimated on both dilated and undilated SBFP, however underestimation was greater on undilated SBFP (Fig. 6A, for parametric testing see Table 2). Dilated SBFP correlated better with CFP (Pearson coefficient of correlation r = 0.91, p < 0.001) than undilated SBFP (r = 0.70, p < 0.001) (Fig. 6B). Intraclass correlation for vCDR between graders was 0.81. Photographic vCDR assessment on CFP correlated well with stereoscopic slit lamp biomicroscopy (Pearson coefficient of correlation r = 0.82, p < 0.001).
Evaluation of vertical Cup-to-disc ratio. Conventional fundus photography (CFP) and dilated (dil.) and undilated (undil.) smartphone-based fundus photography (SBFP) were compared. (A) Comparison of the individual devices and (B) correlation of vertical Cup-to-disc ratio (vCDR) measurement on dil. and undil. SBFP with vCDR-measurement on CFP. Error bars indicate standard error of the mean, paired t-test was used for analysis, asterisks indicate significant differences in regards to CFP if not otherwise indicated, ***p < 0.001.
There was no difference in optic disc pallor evaluation in between CFP and dilated SBFP, however there was a bias towards evaluating optic nerve heads as less pale on undilated SBFP (Fig. 7, for parametric testing see Table 2). Mean optic disc pallor ± SD on CFP and on dilated and on undilated SBFP was 1.77 ± 0.63, 1.79 ± 0.64 and 1.97 ± 0.68, respectively. Weighted kappa in between graders for optic disc pallor was 0.38.
Evaluation of optic disc pallor. Conventional fundus photography (CFP) and dilated (dil.) and undilated (undil.) smartphone-based fundus photography (SBFP) were compared. Error bars indicate standard error of the mean, paired t-test was used for analysis, ns = not significant, *p < 0.05, **p < 0.01.
Subgroup analysis phakic vs. pseudophakic eyes
Statistically significant differences concordant to the overall analysis for image quality and degree of optic rim visualization and differences concordant, however not statistically significant, for vCDR evaluation were present (see Table 3). While a concordant, yet not statistically significant difference was evident for optic disc pallor evaluation in phakic eyes, difference was nearly zero for pseudophakic eyes (see Table 3).
Discussion
This is the first study comparing dilated and undilated SBFP. Overall SBFP success rate, image quality and optic disc rim visualization were better following dilation for the tested adapter and vCDR evaluation on dilated SBFP correlates well with vCDR evaluation on CFP, whereas evaluation on undilated SBFP potentially underestimated vCDR. Similarly, disc pallor was underestimated on undilated SBFP. This highlights the need for dilation in order to ascertain good quality ONH evaluation using SBFP. However, CFP still outperformed SBFP.
The findings further support existing data showing that ONH evaluation is possible with SBFP11,12. Possible explanations for reduced image quality and impaired optic disc rim visualization are constrained optics in case of undilated pupils. Only if the illumination’s and the camera’s light beam are perfectly coaxial and centered in the pupil sufficient image quality can be achieved. Especially in very small pupils this is hard to achieve and even if it is achieved the small pupil diameter might lead to backscatter from the pupil margins leading to increased blurring of the image. As a result from this the blurred neuroretinal rim appears wider and kinking of small vessels into the excavation of the disc cannot be recognized clearly anymore or even not at all. Hence, vCDR and vitality of the ONH might be misinterpreted. Additionally, when comparing CFP with SBFP it is important to take into account that the quality of the optics and the optical setup of smartphones equipped with adapters for SBFP is not as good and well adapted to fundus imaging as are professional fundus cameras. This is most likely the reason why image quality is lower in dilated SBFP than in CFP, although the image resolution achieved with the Galaxy S is much higher than with the Visucam 500 (13 vs. 5 megapixels).
Our subgroup analysis comparing phakic vs. pseudophakic eyes indicated that the difference in optic disc pallor evaluation between dilated and undilated SBFP might be greater in phakic eyes. However this assumption cannot be validated, as we did not compare the same eyes before and after cataract surgery.
As an implication of the results reported herein ONH evaluation with SBFP should be performed following pupil dilation. Nevertheless in cases where dilation might not be possible, e.g. in an outreach screening camp with very limited or no ophthalmic resources, ONH evaluation with SBFP adapters like the D-Eye, which allow for undilated ONH evaluation, represent a possible alternative. Further technical improvements and developments such as utilization of higher quality optical systems are warranted.
The D-Eye is not the only adapter allowing for SBFP. Both the PEEK vision12 and the Welch Allyn iExaminer16 are two possible alternatives, with only the latter allowing for undilated SBFP. As no comparison between the different adapters has been done so far further studies are needed to evaluate and compare the available smartphone adapters. Additionally experience levels of different examiners should be taken into account, as this can affect image quality18.
The strengths of our study are a direct comparison within the same patient, a patient sample with a wide range of age and vCDR, two masked graders and a comprehensive evaluation of imaging quality factors (image quality and degree of optic disc rim visualization) and ONH evaluation (vCDR and optic disc pallor). The limitations of our study are the small sample size, no comparison between different smartphone adapters, the high number of advanced glaucoma cases and that we did not assess the pupil size, intra-patient repeatability and intra-observer reliability of the examination. Furthermore the use of monoscopic imaging bears the risk of a bias towards lower vCDR measurements and reduced inter-observer agreement19.
Smartphone-based fundus photography for ONH evaluation is promising and dilation further increases its quality. It may become a feasible alternative to conventional cameras in the future, allowing for a novel approach to tele-ophthalmology. However, conventional CFP following dilation still outperforms SBFP and further development of smartphone adapters for fundus photography is warranted.
References
Bolster, N. M., Giardini, M. E., Livingstone, I. A. & Bastawrous, A. How the smartphone is driving the eye-health imaging revolution. Expert Review of Ophthalmology 9, 475–485 (2014).
Garg, S. J. Applicability of Smartphone-Based Screening Programs. JAMA ophthalmology 134, 158–159, https://doi.org/10.1001/jamaophthalmol.2015.4823 (2016).
Hong, S. C. 3D printable retinal imaging adapter for smartphones could go global. Graefes Archive for Clinical and Experimental Ophthalmology 253, 1831–1833, https://doi.org/10.1007/s00417-015-3017-z (2015).
Furdova, A., Furdova, A. & Krcmery, V. Our experience with smartphone and spherical lens for the eye fundus examination during humanitarian project in Africa. Int J Ophthalmol 10, 157–160, https://doi.org/10.18240/ijo.2017.01.25 (2017).
Russo, A., Morescalch, F., Costagliola, C., Delcassi, L. & Semeraro, F. Comparison of Smartphone Ophthalmoscopy With Slit-Lamp Biomicroscopy for Grading Diabetic Retinopathy. American journal of ophthalmology 159, 360–364, https://doi.org/10.1016/j.ajo.2014.11.008 (2015).
Bolster, N. M., Giardini, M. E. & Bastawrous, A. The Diabetic Retinopathy Screening Workflow: Potential for Smartphone Imaging. Journal of diabetes science and technology 10, 318–324, https://doi.org/10.1177/1932296815617969 (2016).
Rajalakshmi, R. et al. Validation of Smartphone Based Retinal Photography for Diabetic Retinopathy Screening. PloS one 10, https://doi.org/10.1371/journal.pone.0138285 (2015).
Micheletti, J. M., Hendrick, A. M., Khan, F. N., Ziemer, D. C. & Pasquel, F. J. Current and Next Generation Portable Screening Devices for Diabetic Retinopathy. Journal of diabetes science and technology 10, 295–300, https://doi.org/10.1177/1932296816629158 (2016).
Toy, B. C. et al. Smartphone-Based Dilated Fundus Photography and Near Visual Acuity Testing as Inexpensive Screening Tools to Detect Referral Warranted Diabetic Eye Disease. Retina-the Journal of Retinal and Vitreous Diseases 36, 1000–1008 (2016).
Bhat, S. et al. Fully-automated Diabetic Retinopathy Screening Using Cellphone-based Cameras. Investigative ophthalmology & visual science 56, 1428–1428 (2015).
Russo, A. et al. Comparison of Smartphone Ophthalmoscopy With Slit-Lamp Biomicroscopy for Grading Vertical Cup-to-Disc Ratio. Journal of glaucoma 25, e777–781, https://doi.org/10.1097/ijg.0000000000000499 (2016).
Bastawrous, A. et al. Clinical Validation of a Smartphone-Based Adapter for Optic Disc Imaging in Kenya. JAMA ophthalmology 134, 151–158, https://doi.org/10.1001/jamaophthalmol.2015.4625 (2016).
Foster, P. J., Buhrmann, R., Quigley, H. A. & Johnson, G. J. The definition and classification of glaucoma in prevalence surveys. The British journal of ophthalmology 86, 238–242 (2002).
Greslechner, R. & Spiegel, D. Clinical evaluation of the optic disc in glaucoma. Der Ophthalmologe: Zeitschrift der Deutschen Ophthalmologischen Gesellschaft 113, 816–823, https://doi.org/10.1007/s00347-016-0331-8 (2016).
Russo, A., Morescalchi, F., Costagliola, C., Delcassi, L. & Semeraro, F. A Novel Device to Exploit the Smartphone Camera for Fundus Photography. Journal of ophthalmology 2015, 823139–823139, https://doi.org/10.1155/2015/823139 (2015).
Day, L. M., Wang, S. X. & Huang, C. J. Nonmydriatic Fundoscopic Imaging Using the Pan Optic iExaminer System in the Pediatric Emergency Department. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine 24, 587–594, https://doi.org/10.1111/acem.13128 (2017).
Schneider, C. A., Rasband, W. S. & Eliceiri, K. W. NIH Image to ImageJ: 25 years of image analysis. Nat Meth 9, 671–675 (2012).
Adam, M. K. et al. Quality and Diagnostic Utility of Mydriatic Smartphone Photography: The Smartphone Ophthalmoscopy Reliability Trial. Ophthalmic Surgery Lasers & Imaging Retina 46, 631–637, https://doi.org/10.3928/23258160-20150610-06 (2015).
Morgan, J. E., Sheen, N. J., North, R. V., Choong, Y. & Ansari, E. Digital imaging of the optic nerve head: monoscopic and stereoscopic analysis. The British journal of ophthalmology 89, 879–884, https://doi.org/10.1136/bjo.2004.046169 (2005).
Acknowledgements
We thank the Else Kroehner Fresenius Stiftung/German Scholars Organization (EKFS/GSO 16) for their support.
Author information
Authors and Affiliations
Contributions
M.W.M.W. and C.K.B. analyzed the data, wrote the manuscript and prepared the figures. All authors reviewed the manuscript. R.P.F. supervised this research project.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wintergerst, M.W.M., Brinkmann, C.K., Holz, F.G. et al. Undilated versus dilated monoscopic smartphone-based fundus photography for optic nerve head evaluation. Sci Rep 8, 10228 (2018). https://doi.org/10.1038/s41598-018-28585-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-28585-6
This article is cited by
-
Technische und optische Aspekte der Fundusfotographie
Der Ophthalmologe (2022)
-
Smartphone-basierte Fundusfotografie: Anwendungen und Adapter
Der Ophthalmologe (2022)
-
Comparison of vertical cup-to-disc ratio estimates using stereoscopic and monoscopic cameras
Eye (2021)
-
Learning curve evaluation upskilling retinal imaging using smartphones
Scientific Reports (2021)
-
Review of retinal cameras for global coverage of diabetic retinopathy screening
Eye (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.