Abstract
Objectives
To compare the performance of a handheld fundus camera with standard 50° visual field to ultra-widefield (UWF) table-top fundus camera in diabetic retinopathy (DR) detection and grading.
Methods
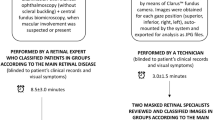
Patients affected by diabetes mellitus and referred to our diabetic retinopathy clinic were enroled and underwent fundus photography in mydriasis. All photos were taken using the ultra-widefield table-top fundus camera Zeiss Clarus™ 500 (four fields per eye) and the Optomed Aurora® handheld fundus camera (3 fields per eye). The following parameters were analysed: the gradability of the images, the grade of DR, and diabetic maculopathy (DM), the presence of hypertensive retinopathy (HR) and the presence of other ocular diseases.
Results
We enroled 759 eyes of 384 diabetic patients and analysed 5313 fundus photos. The handheld fundus camera obtained a sensitivity of 84.2% and specificity of 95.4% for referable cases. Moreover, it obtained, compared to UWF, an almost perfect agreement with linear weighting for DR, DM and HR (k = 0.877, k = 0.854, and k = 0.961, respectively). The lowest sensitivity was achieved for proliferative DR (58.7% sensitivity, 100% specificity).
Conclusions
Optomed Aurora® handheld fundus camera imaging showed a strong agreement compared to UWF in grading DR, considering all DR and DM grades, in mydriasis. However, the use of UWF imaging increases the detection of referable eyes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Silva PS, Cavallerano JD, Sun JK, Soliman AZ, Aiello LM, Aiello LP. Peripheral lesions identified by mydriatic ultrawide field imaging: distribution and potential impact on diabetic retinopathy severity. Ophthalmology. 2013;120:2587–95.
Vujosevic S, Aldington SJ, Silva P, Hernández C, Scanlon P, Peto T, et al. Screening for diabetic retinopathy: new perspectives and challenges. Lancet Diabetes Endocrinol. 2020;8:337–47.
Curran K, Piyasena P, Congdon N, Duke L, Malanda B, Peto T. Inclusion of diabetic retinopathy screening strategies in national-level diabetes care planning in low-income and middle-income settings: protocol for a scoping review. BMJ Open. 2020;10:e038647.
Salongcay RP, Aquino LAC, Salva CMG, Saunar AV, Alog GP, Sun JK. Comparison of handheld retinal imaging with ETDRS 7-standard field photography for diabetic retinopathy and diabetic macular edema. Ophthalmol Retin. 2022. https://doi.org/10.1016/J.ORET.2022.03.002
Midena E, Zennaro L, Lapo C, Torresin T, Midena G, Pilotto E. Handheld fundus camera for diabetic retinopathy screening: a comparison study with table-top fundus camera in real-life setting. J Clin Med. 2022;11:2352.
Davila JR, Sengupta SS, Niziol LM, Sindal MD, Besirli CG, Upadhyaya S. Predictors of photographic quality with a handheld nonmydriatic fundus camera used for screening of vision-threatening diabetic retinopathy. Ophthalmologica. 2017;238:89–99.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013;36(Suppl 1):S67–74.
Vujosevic S, Benetti E, Massignan F, Pilotto E, Varano M, Cavarzeran F, et al. Screening for diabetic retinopathy: 1 and 3 nonmydriatic 45-degree digital fundus photographs vs 7 standard early treatment diabetic retinopathy study fields. Am J Ophthalmol. 2009;148:111–8.
Wilkinson CP, Ferris FL 3rd, Klein RE, Lee PP, Agardh CD, Davis M, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110:1677–82.
Vujosevic S, Pucci P, Casciano M, Daniele A, Bini S, Berton M, et al. A decade-long telemedicine screening program for diabetic retinopathy in the north-east of Italy. J Diabetes Complicat. 2017;31:1348–53.
Cicchetti DV, Allison T. A new procedure for assessing reliability of scoring EEG sleep recordings. Am J EEG Technol. 1971;11:101–10.
Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas 1973;33:613–9.
Yang Z, Zhou M. Weighted kappa statistic for clustered matched-pair ordinal data. Comput Stat Data Anal 2015;82:1–18.
Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33:363–74.
Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis. 2015;2:17.
Avogaro A, Fadini GP. Microvascular complications in diabetes: a growing concern for cardiologists. Int J Cardiol 2019;291:29–35.
DRCR Retina Network—Public Site. https://public.jaeb.org/drcrnet/stdy/239. accessed 2 Jun 2022.
Mead A, Burnett S, Davey C. Diabetic retinal screening in the UK. J R Soc Med. 2001;94:127–9.
Feinstein AR, Cicchetti DV. High agreement but low Kappa: I. the problems of two paradoxes. J Clin Epidemiol 1990;43:543–9.
Marcus DM, Silva PS, Liu D, Aiello LP, Antoszyk A, Elman M, et al. Association of predominantly peripheral lesions on ultra-widefield imaging and the risk of diabetic retinopathy worsening over time. JAMA Ophthalmol. 2022;140:946–54.
Early Treatment Diabetic Retinopathy Study Research Group. Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Ophthalmology. 1991;98:823–33.
Ruan S, Liu Y, Hu WT, Jia HX, Wang SS, Song ML, et al. A new handheld fundus camera combined with visual artificial intelligence facilitates diabetic retinopathy screening. Int J Ophthalmol. 2022;15:620–7.
Kubin AM, Wirkkala J, Keskitalo A, Ohtonen P, Hautala N. Handheld fundus camera performance, image quality and outcomes of diabetic retinopathy grading in a pilot screening study. Acta Ophthalmol. 2021;99:e1415–20.
Khan R, Raman S, Karamcheti SKM, Srinivasan S, Sharma A, Surya J, et al. Comparison of two ultra-widefield cameras with high image resolution and wider view for identifying diabetic retinopathy lesions. Transl Vis Sci Technol. 2021;10:9.
Acknowledgements
The research contribution of the Fondazione Bietti in this paper was supported by the Ministry of Health and Fondazione Roma. The authors thank Fabiano Cavarzeran, Ophthalmology Clinic, Department of Ophthalmology, University of Padova, Padova, Italy, for his support in the statistical analysis.
Author information
Authors and Affiliations
Contributions
EM and LF were responsible for conceptualisation, methodology and validation; LZ and CL were responsible for data curation and formal analysis; GM and TT were responsible for the investigation and data curation; LZ and LF were responsible for the investigation and original draft preparation. All Authors were responsible for review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Midena, E., Zennaro, L., Lapo, C. et al. Comparison of 50° handheld fundus camera versus ultra-widefield table-top fundus camera for diabetic retinopathy detection and grading. Eye 37, 2994–2999 (2023). https://doi.org/10.1038/s41433-023-02458-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02458-3