Abstract
Alpha-1 antitrypsin (AAT) augmentation therapy involves infusion of plasma-purified AAT to AAT deficient individuals. Whether treatment affects microRNA expression has not been investigated. This study’s objectives were to evaluate the effect of AAT augmentation therapy on altered miRNA expression in monocytes and investigate the mechanism. Monocytes were isolated from non-AAT deficient (MM) and AAT deficient (ZZ) individuals, and ZZs receiving AAT. mRNA (qRT-PCR, microarray), miRNA (miRNA profiling, qRT-PCR), and protein (western blotting) analyses were performed. Twenty one miRNAs were differentially expressed 3-fold between ZZs and MMs. miRNA validation studies demonstrated that in ZZ monocytes receiving AAT levels of miR-199a-5p, miR-598 and miR-320a, which are predicted to be regulated by NFκB, were restored to levels similar to MMs. Validated targets co-regulated by these miRNAs were reciprocally increased in ZZs receiving AAT in vivo and in vitro. Expression of these miRNAs could be increased in ZZ monocytes treated ex vivo with an NFκB agonist and decreased by NFκB inhibition. p50 and p65 mRNA and protein were significantly lower in ZZs receiving AAT than untreated ZZs. AAT augmentation therapy inhibits NFκB and decreases miR-199a-5p, miR-598 and miR-320a in ZZ monocytes. These NFκB-inhibitory properties may contribute to the anti-inflammatory effects of AAT augmentation therapy.
Similar content being viewed by others
Introduction
Alpha-1 antitrypsin (AAT) deficiency is characterised by lower than normal circulating levels of AAT leading to a decreased antiprotease protective screen within the lung1. Although hepatocytes are the major source of circulating AAT, other cell types including monocytes can express AAT and our group has shown that accumulation of misfolded ZAAT within monocytes affects their basal and agonist-induced cytokine expression2. Furthermore other work of ours has demonstrated that monocytes from ZZ homozygous (AAT deficient) individuals show an altered pattern of microRNA (miRNAs) compared to MM (non-AAT deficient) monocytes3; miRNAs are important posttranscriptional negative regulators of gene expression.
AAT augmentation therapy involves infusion of purified human plasma AAT (60 mg per kilogram of body weight per week) and has been associated with both clinical and biochemical effects4,5,6,7,8,9,10,11,12,13. A number of studies have suggested that AAT also exhibits anti-inflammatory properties independent of inhibition of serine proteases in a variety of cell models. For example AAT augmentation therapy has been shown to reduce levels of chemoattractant leukotriene B4 in the airways14. For circulating inflammatory cells such as neutrophils, infused plasma AAT has the ability to bind them and modulate IL-8 or soluble immune complex-induced neutrophil chemotaxis15 and neutrophil degranulation16. In monocytes, AAT augmentation therapy inhibits endotoxin-induced inflammatory responses such as release of TNFα and IL-β17. That group also demonstrated that in vitro AAT inhibition of LPS-stimulated TNFα and IL-10 is mediated by a rise in cAMP and activation of cAMP-dependent protein kinase18. Other anti-inflammatory effects of AAT on murine and human neutrophils and in lung tissues have also been described. These include alterations in surface receptors on macrophages treated exogenously with AAT19and activation of protein phosphatase 2A in human alveolar macrophages, monocytes, neutrophils, airway epithelial cells, and in mouse lungs. It has been proposed that these effects counterbalance inflammatory and proteolytic responses induced by TNF signalling within the lung20.
Studies examining the effects of AAT deficiency and AAT augmentation therapy in circulating immune cells such as monocytes have provided insight into both the pathophysiology of the disease and non-classical anti-inflammatory properties of AAT augmentation therapy.
Whether AAT augmentation therapy affects miRNA expression has not been investigated, nor is it known if some of the anti-inflammatory effects of AAT augmentation therapy may be mediated by changes in miRNA and miRNA target protein expression. Here we identify a set of differentially expressed miRNAs in monocytes from asymptomatic MM and ZZ individuals, and show further changes in the miRNA expression profile of ZZ monocytes isolated from individuals receiving AAT augmentation therapy. We elucidate the molecular mechanisms responsible for the altered expression of a subset of these miRNAs, focussing on NFκB, and link our observations regarding altered miRNA expression to other responses potentially mediated by AAT augmentation therapy.
Results
Global miRNA expression is altered in ZZ monocytes from individuals receiving AAT augmentation therapy
We explored the global miRNA expression pattern in monocytes from asymptomatic MM and ZZ individuals and symptomatic ZZ individuals receiving weekly AAT augmentation therapy at Day 0 and Day 2 (48-hour post-AAT augmentation therapy) (n = 3 per group). The mean ± SE serum AAT concentrations in the MM, ZZ Day 0 and ZZ Day 2 individuals were 26.2 ± 1.7, 8.1 ± 0.8, 30.29 ± 4.7 µM AAT, respectively. For the miRNA profiling studies RNA was also isolated from THP-1 monocytic cells (a human leukaemia monocytic cell line used as a control) and all samples were examined for expression of 731 human miRNAs using the Nanostring Technologies nCounter miRNA Expression Kit. Appreciable target detection occurred for 398 miRNAs across all samples. Fifty nine miRNAs were identified that were expressed at an average difference of greater or less than 1.5 fold in (i) asymptomatic ZZ monocytes compared to MM monocytes or asymptomatic ZZ monocytes compared to ZZ monocytes receiving weekly AAT augmentation therapy at (ii) Day 0 or (iii) Day 2 (Supplementary Dataset File 01).
Importantly, 21 miRNAs were altered by more than 3-fold in asymptomatic ZZ compared to MM monocytes (Supplementary Table S1, and previously reported in3). MiRNAs expressed in symptomatic ZZs receiving AAT augmentation therapy at Day 2 were also compared to both symptomatic or asymptomatic ZZ monocytes not receiving AAT augmentation therapy at Day 0. Many of the miRNAs that were increased or decreased > 3-fold in symptomatic ZZ monocytes receiving AAT augmentation therapy at Day 0 (compared to asymptomatic ZZ monocytes not receiving AAT augmentation therapy) were similarly differentially expressed in ZZ monocytes receiving AAT augmentation therapy at Day 2 (italicised in Supplementary Table S2). Eleven miRNAs were altered >3-fold in ZZ monocytes receiving AAT augmentation therapy at Day 2 versus Day 0 (Supplementary Table S3). Of these 7 were decreased, including miR-199a-5p and miR-598.
AAT augmentation therapy alters global gene expression
Microarray analysis was perfomed on pooled samples of (i) ZZ monocytes treated ex vivo with AAT versus control, and (ii) in Day 2 versus Day 0 ZZ monocytes. The microarray contained probes for over 26,000 protein coding transcripts. Of these 334 genes were commonly down regulated by AAT greater than or equal to 2-fold in both datasets. These (and their fold-change in each dataset) are listed in Supplementary Dataset 02 and 03, which includes both the probe name and the gene name to allow for isoforms. A subset of 8 genes was identified (common to both samples with an absolute fold change greater than 10 in both cases). We submitted these genes to Enrichr (gene set enrichment analysis web server)21 and explored the gene ontology and pathway involvement of the genes. The significantly associated gene ontology terms (adjusted p-value < 0.05) were imported to REVIGO22 where they were clustered based on their relatedness and any redundancy was removed. Significantly enriched pathways with adjusted p-value < 0.05 were exported from Enrichr and plotted (Genes uploaded to Enrichr: ABLIM3, CCL11, DNAJC14, FAHD1, IL17RC, LOC100287482, RHD and TPD52L2). This identified numerous processes with altered expression of genes (Supplementary Dataset 04). Terms with significant adjusted P values were only evident in the ‘Biological Processes’ and ‘Molecular Function’ analyses, these are plotted in Supplementary Figure 1. Pathways significantly affected by the altered genes are listed in Supplementary dataset 05 and depicted in Supplementary Figure 2A–E.
Validation of miRNA profiling and identification of NFκB as a potential regulator of altered miRNAs
In order to explore if the effects of AAT on miRNA expression might be mediated by modulation of transcription factors, the regulatory regions of the altered miRNAs were analysed using bioinformatics with DIANA miRGEN 2.0 (http://www.diana.pcbi.upenn.edu). This analysis highlighted that of the 21 altered miRNAs that were increased at least 3-fold in asymptomatic ZZ vs MM cells, a subset were predicted to be regulated by NFκB, namely miR-598, miR-199a and miR-320a (Fig. 1a). miR-30a-5p which contains a putative NFκB binding site in its promoter that is too close to the transcriptional start site to be functional (i.e. it is not regulated by NFκB) is also shown. This miRNA was not increased in ZZ vs. MM monocytes.
MiRNAs predicted to be regulated by NFκB are altered in ZZ individuals receiving AAT augmentation therapy. (a) Schematic diagram showing the location of predicted NFκB binding sites on regulatory regions of miRNA genes (TSS: transcription start site, blue box represent distance from TSS). Relative expression of miR-598, miR-199a-5p, miR-320a and miR-30a was determined using TaqMan miRNA assays and normalized to U6 snRNA using the 2−ΔΔCt method in (b), asymptomatic MM versus ZZ monocytes (n = 4, in triplicate, *p ≤ 0.0167: t-test with Bonferroni correction for 3 test miRNAs) and (C), ZZ monocytes from symptomatic individuals pre and 2 days post AAT augmentation therapy (n = 4, in triplicate, *p ≤ 0.0167; t-test with Bonferroni correction for 3 test miRNAs, $p = 0.05). Data are represented as mean ± SEM.
Supplementary Fig. 3A shows the heat map of these miRNAs in the samples that were profiled. The full heat map and dendogram of all altered miRNAs of interest is provided in Supplementary Fig. 3B. MiR-199a-5p was 40-fold higher in asymptomatic ZZ monocytes compared to MM monocytes. Symptomatic ZZ patients at Day 0 (i.e. 7 days after weekly AAT augmentation therapy) had 8-fold lower miR-199a-5p levels compared to asymptomatic ZZs, whilst ZZs at Day 2 had 50-fold lower levels than ZZs not receiving AAT augmentation therapy. MiR-598 and miR-320a, were also increased in ZZ versus MM monocytes (17- and 12-fold, respectively). Although AAT augmentation therapy did not alter levels of miR-320a at Day 0 and 2, or miR-598 levels at Day 0, there was a 4-fold decrease in miR-598 in ZZ monocytes receiving AAT augmentation therapy at Day 2 compared to ZZs not receiving therapy. miR-30a-5p was included as a negative control. There were no significant differences in miR-30a-5p levels in asymptomatic ZZs, MMs or ZZ monocytes receiving AAT augmentation therapy at Day 0. However, its levels increased 4-fold in ZZs at Day 2 compared to ZZ monocytes not receiving AAT.
In order to validate the miRNA profiling data, the expression patterns of these miRNAs was independently verified by qRT-PCR using Taqman miRNA assays. Similar to the profiling data, Fig. 1b shows that there was significantly increased expression of miR-199a-5p, miR-598 and miR-320a in asymptomatic ZZ compared to MM monocytes (N = 4 in each group, 22-, 28- and 16-fold increase, respectively); miR-30a was 5-fold higher.
Figure 1c shows that levels of miR-199a-5p and miR-598 were significantly decreased in symptomatic ZZ monocytes receiving AAT augmentation therapy at Day 0 and Day 2; levels of miR-320a were substantially decreased. Expression of miR-30a was not decreased following AAT augmentation therapy.
AAT decreases miR-598, miR-199a-5p, and miR-320a in ex vivo ZZ monocytes
The effect of exogenous AAT (27.5 µM for 4 hours) on asymptomatic ZZ monocytes was explored next. Similar to the in vivo observations, expression of miR-598, miR-199a-5p, and miR-320a, but not miR-30a, was significantly reduced in asymptomatic ZZ monocytes treated ex vivo with physiologically relevant concentrations of AAT reflecting the actual augmentation therapy dose (Fig. 2).
AAT decreases expression of miRNAs predicted to be regulated by NFκB in ZZ monocytes. Relative expression of miR-598, miR-199a-5p, miR-320a and miR-30a was determined using TaqMan miRNA assays and normalized to U6 snRNA using the 2−ΔΔCt method in asymptomatic ZZ monocytes (1 × 105 cells) and ZZ monocytes treated with 27.7 µM AAT for 4 hours. Assays were performed n = 3, in triplicate and data are represented as mean ± SEM (*p ≤ 0.0167 measured by t-test with Bonferroni correction).
Validated targets of miR-598, miR-199a-5p, and miR-320a are increased in ZZ monocytes receiving AAT augmentation therapy
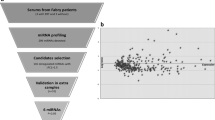
Given that AAT augmentation therapy decreased levels of miRNAs predicted to be regulated by NFκB, targets of these miRNAs are likely to be increased in response to AAT augmentation therapy. Based on this relationship we hypothesised that experimentally validated targets of miR-598, miR-199a and miR-320a, should be reciprocally increased in the same samples. Therefore we cross-compared data for each of these miRNAs alone and together with microarray data specifically focusing on mRNAs that are increased in response to AAT i.e. in ZZ individuals post- versus pre-augmentation therapy, and in ZZ monocytes treated ex vivo with AAT vs untreated cells (Fig. 3). We identified a selection of mRNAs that were increased in both groups known to be individually regulated by the lead miRNAs (Supplementary Tables 4–6). These deregulated mRNAs were also evaluated for possibly belonging to specific pathways and five most relevant ones (although none with significant adjusted P values) are reported in Supplementary Table 7.
Schema to identify miRNA-mediated effects of AAT on gene expression in ZZ monocytes. Eukaryotic translation initiation factor 4 H and heterogeneous ribonuclear protein U were identified by cross-comparing experimentally validated targets of miR-598, miR-199a and miR-320a with two microarray datasets of mRNAs upregulated in response to AAT (i.e. ZZ individuals post versus pre AAT augmentation therapy, and ZZ monocytes treated ex vivo with AAT vs untreated cells).
Only two mRNAs that were known to be co-regulated by two of the lead miRNAs (miR-199a-3p and miR-320a) were increased in both microarray datasets; eukaryotic translation initiation factor 4 H (EIF4H) and heterogeneous nuclear ribonuclear protein U (HNRNPU) which have roles in translation and splicing, respectively. These results suggest that AAT augmentation therapy may enhance these events in monocytes. There were no targets known to be co-regulated by all three miRNAs that were increased by AAT in vivo or in vitro.
miR-598, miR-199a-5p, and miR-320a are regulated by NFκB in ZZ monocytes
Having used bioinformatics to identify NFκB as a possible regulator of the altered miRNAs next we investigated the mechanism by which these altered miRNAs are decreased in response to AAT in monocytes in more detail. In order to determine if NFκB is indeed involved in the regulation of the validated miRNAs (miR-598, miR-199a-5p and miR-320a), inhibition or activation of NFκB was induced in asymptomatic ZZ monocytes by 4 hours treatment with 20 µM BAY-11 7082 or 500 U/ml TNFα, respectively (Fig. 4a–c). Monocytes treated with BAY-11 7082 showed significantly decreased expression of all three miRNAs. Basal expression of miR-30a, which was included as a negative control, was not affected by BAY-11 7082 although it was increased by TNFα (data not shown). Conversely, treatment with TNFα led to significant increases in miR-598, miR-199a-5p and miR-320a levels.
NFκB modulation regulates (a), miR-598, (b), miR-199a-5p, and (c), miR-320a expression. Relative expression of miRNAs normalized to U6 snRNA was determined using Taqman assays in asymptomatic ZZ monocytes (1 × 105 cells, n = 3, separate cultures in triplicate) treated with or without 20uM BAY-11 7082 or 500U/ml TNF-α or both for 4 hours. (d), Relative expression of miR-598, miR-199a-5p, miR-320a and miR-30a was determined using the TaqMan miRNA assays in asymptomatic MM monocytes (1 × 105 cells) and MM monocytes treated with 50 nM of thapsigargin for 1 hour. Assays were performed n = 3, in triplicate and data are represented as mean ± SEM (a and b ***p < 0.0001, c ***p = 0.0007 measured by ANOVA with Bonferroni’s correction for multiple group comparison. d *p ≤ 0.0167 measured by t-test with Bonferroni correction).
As a corollary to these investigations in ZZ monocytes, MM monocytes were treated ex vivo with 50 nM thapsigargin, an ER stress agonist and known activator of NFκB. Figure 4d shows that unlike the miR-30a negative control, miR-598, miR-199a-5p, and miR-328 were significantly increased in MM monocytes treated with thapsigargin compared to non-treated MM monocytes.
NFκB p50 and p65 are down regulated in ZZ monocytes receiving AAT augmentation therapy
To further support the observation that AAT inhibits NFκB in ZZ monocytes we analysed the set of genes that were decreased in both ZZ individuals post-augmentation therapy, and in ZZ monocytes treated ex vivo with AAT. Of the 334 genes in this subset 294 were predicted to be regulated by NFκB (Supplementary Dataset File 06) – thus AAT appears to have a strong inhibitory effect on NFκB-regulated gene expression at least in ZZ monocytes. A Gene Set Enrichment Analysis (GSEA) on downregulated genes after augmentation therapy or AAT treatment in vitro using an NFκB gene signature was performed to support NFκB involvement. The full set of genes down-regulated in Day 2 vs. Day 0 (n = 3173) and down-regulated in ZZ + AAT vs. Control (n = 1760) were screened for NFκB enrichment against the hallmark gene set, which is one of the 8 major collections of gene sets in the Molecular Signatures Database (MSigDB), and is comprised of 50 gene sets. (http://software.broadinstitute.org/gsea/msigdb/genesets.jsp?collection = H). The HALLMARK_TNFA_SIGNALING_VIA_NFKB (Genes regulated by NFκB in response to TNF) gene set was the second and fifth most enriched of 50 Hallmark gene sets in “Day 2 vs. Day 0 (Normalized Enrichment Score (NES) = −1.60; FDR q < 0.17) and “ZZ + AAT vs. Control (NES = −1.34; FDR q < 0.70), respectively.
Finally, in order to functionally link the observations regarding NFκB-regulated miRNAs and AAT augmentation therapy, the effect of intravenous AAT augmentation therapy on NFκB was determined. Expression of p50 and p65 mRNA and protein was measured using qRT-PCR and western blot analyses, respectively (Fig. 5). When compared to Day 0 ZZ monocytes, p50 and p65 mRNA levels were significantly lower in ZZ monocytes receiving AAT augmentation therapy at Day 2 (Fig. 5a). A similar observation was evident for p50 and p65 protein expression (Fig. 5b).
NFκB mRNA and protein expression is decreased in symptomatic ZZ monocytes receiving AAT augmentation therapy. Relative expression of p50 and p65 (a), mRNA and (b), protein in ZZ monocytes pre-AAT therapy and 2 days post AAT augmentation therapy (N = 5 in each group). mRNA and protein relative expression were analysed in triplicate by qRT-PCR and western blot respectively and normalized to GAPDH. aA representative cropped western blot in shown in b, the full-length blots are provided in the Supplementary Information File as Supplementary Fig. 4. Data are represented as mean ± SEM, **p and *** < 0.025 measured via t-test with Bonferroni correction for 2 factors).
Discussion
Monocyte studies in AAT deficiency have revealed the importance of circulating immune cells as effectors contributing to the inflammatory milieu in the AATD lung. Here, using an in vivo model of human monocytes, we report significant alterations in miRNA expression profiles following AAT augmentation therapy. Our analysis revealed that miR-199a-5p, miR-598 and miR-320a are microRNAs which are increased in ZZ vs. MM monocytes in vivo. All three miRNAs were also increased in MM monocytes treated with the ER stress agonist thapsigargin suggesting that these miRNAs may be ER stress-inducible miRNAs independent of ZAAT. miR-199a-5p, miR-598 and miR-320a were decreased in response to AAT augmentation therapy. Validated targets co-regulated by these miRNAs are involved in translation and splicing and their transcripts are reciprocally increased in ZZ monocytes receiving AAT. We show that NFκB regulates miR-199a-5p, miR-598 and miR-320a, and that in addition to these miRNAs, almost 300 other NFκB-regulated genes are decreased in ZZ monocytes receiving AAT. We also show that p50 and p65 mRNA and protein are lower in ZZ monocytes receiving AAT, and conclude that AAT augmentation therapy decreases expression of miR-199a-5p, miR-598 and miR-320a in ZZ monocytes via inhibiting NFκB. These events may contribute to the therapeutic effects of AAT augmentation therapy.
AAT is the most important serpin in the lung where it is responsible for the inhibition of neutrophil elastase and other serine proteinases. People with AAT deficiency, and especially those with severe AATD that are homozygous for the Z allele (Glu342Lys), have lower than normal intrapulmonary and circulating levels of AAT due to accumulation of the misfolded Z protein in the endoplasmic reticulum of hepatocytes, the principal source of AAT. The misfolding defect characteristic of ZAAT leads to the formation of polymers of ZAAT23. AAT augmentation therapy with purified human plasma AAT is the only established and approved therapy for AAT deficiency and is now widely used in Europe and North America. In 2015 the findings from a 2-year, placebo-controlled clinical trial (RAPID-RCT) were published demonstrating clinical efficacy of AAT augmentation therapy wherein progression of emphysema was slowed by 34%12. Subsequently the same patients entered a 2-year open-label extension trial (RAPID-OLE), in which all patients received AAT augmentation therapy13. That study confirmed the continued efficacy of AAT augmentation therapy over 4 years for the prevention of emphysema, showed that the therapy can slow lung density loss, and hence disease progression.
In addition to its serine antiprotease property AAT also has anti-inflammatory properties that can affect inflammatory cells including monocytes and neutrophils. Short-term AAT augmentation therapy not only restores airway concentrations of AAT to normal, but also reduces levels of LTB4, a major mediator of neutrophil recruitment and activation14. Infused AAT can bind to circulating neutrophils and modulate neutrophil migration to the airways by preventing release of CD16b from the cell membrane15. In monocytes, exogenous AAT can strongly inhibit LPS-induced human monocyte activation and production of IL-1017,18. The mechanisms responsible for these additional properties of AAT have not been fully elucidated although roles for cAMP and protein phosphatase 2 A have been clearly demonstrated18,20. We speculated that AAT-mediated alterations in microRNA expression may underpin some of these effects, and designed this study to address that question.
The major function of miRNAs is to negatively regulate target protein expression. Depending on the degree of complementarity been a miRNA’s seed region and its cognate miRNA recognition element within a target mRNA, mRNA degradation can be induced – this has been reported to occur for over 80% of miRNA targets24. Based on this fact we interrogated gene array data from two AAT-treated sample sets (compared to their non-AAT treated controls) in order to find whether experimentally validated targets of the lead miRNAs that were decreased in response to treatment with AAT demonstrated reciprocal up regulation. Whilst the mRNA of a number of validated targets known to be co-regulated by 2 or all of the lead miRNAs were increased in either sample set (data now shown), only 2 mRNAs were increased in response to AAT in both sample sets. These transcripts EIF4H and HNRNPU encode proteins that are components of a cell’s translation and splicing machinery, respectively. Ideally EIF4H and HNRNPU protein levels would have been measured here however this was not possible due to limitation of sample availablity. The HNRNPU protein is 90.5 kDa and forms part of the spliceosome C complex. It addition to forming complexes with various proteins it also contains RNA- and DNA-binding domains. The protein is essential for efficient pre-mRNA splicing in some organs and can stabilise certain cytokine mRNA transcripts25,26. EIF4H is a 27.4 kDa protein translation factor that was increased 3- to 30-fold in response to AAT27. Some studies have suggested that it can play a role in tumorigenesis in lung and other organs28,29. This undesirable attribute should be explored further in the context of AAT augmentation therapy.
We also explored the potential effects that AAT augmentation therapy may have via modulation of the individual lead miRNAs. miR-199a-5p and miR-598 are normally expressed at low levels in both THP-1 cells30 and primary human monocytes31 however, we have shown that they are present in greater abundance in ZZ versus MM monocytes. AAT augmentation therapy decreases their levels to within the normal range (decreases of 50- and 5 fold, respectively). miR-320a is more abundant than miR-199a-5p and miR-598, and has been more intensively studied and therefore more of its validated targets are known. We observed a number of novel pathways can be affected by these miRNAs with the most interesting regarding what is known about AAT deficiency being ER protein processing due to altered expression of MAN1A2, HSP90AA1 and EDEM1, validated targets of miR-598, miR-199a-5p and miR-320a, respectively.
We observed some interesting gene expression changes overall in response to AAT in vivo and in vitro which may or may not be related to alterations in miRNA expression. Significantly altered GO terms included such processes as leucocyte chemotaxis, responses to cytokines, ion transport and actin filament polymerisation. Pathways affected by these changes include IL-4 and IL-17 cytokine signalling pathways and various G-protein coupled receptor pathways including CXCR3.
Here, we also demonstrated for the first time that AAT augmentation therapy reduces the expression of both the mRNA and protein of the canonical heterodimer of NFκB in ZZ monocytes. NFκB activation in AAT deficiency and in the context of ER accumulation of misfolded ZAAT have been reported in a variety of cell types including monocytes, 16HBE14o- human bronchial epithelial cell lines, Chinese hamster ovary (CHO) cells, liver cell lines and liver cells from transgenic mice with liver-specific inducible expression of ZAAT2,32,33. Our data indicates that augmentation therapy can reverse this effect in ZZ monocytes. A strong inhibitory effect of AAT augmentation therapy on NFκB was evident in ZZ monocytes in vivo and we further confirmed this observation in vitro. However the mechanism by which exogenous, infused AAT may directly influence NFκB expression remains unanswered and is beyond the scope of this study. Interestingly the NFκB subunits p50 and p65 are validated targets of miR-199a-5p3. The present study demonstrates that NFκB is a transcription factor for miR-199a-5p suggesting that an autoregulatory loop exists between NFκB and miR-199a-5p.
The gene array studies and GSEA indicated that up to 300 genes predicted to be regulated by NFκB showed decreased expression in ZZ monocytes from individuals receiving AAT augmentation therapy on Day 2 after infusion and also in ZZ monocytes treated ex vivo with therapeutically relevant levels of AAT compared to matched controls. Future independent validation and functional analysis of the roles of these altered genes can shed light on unexplored biological effects of AAT augmentation therapy. Furthermore, this information coupled with extended studies to determine the consequences of AAT augmentation therapy on altered miRNA expression (via mechanisms other than inhibition of NFκB) will generate further insight into the properties and effects of AAT augmentation therapy. In conclusion the data presented here provides new mechanistic evidence regarding the potential biological effects of AAT augmentation therapy mediated by NFκB inhibition and/or altered miRNA expression that has implications for AAT deficiency and other diseases where AAT augmentation therapy may have relevance.
Methods
Study populations
Asymptomatic non-AAT deficient MM (n = 5, 3 males, 2 females) and AAT-deficient ZZ (n = 6, 3 males, 3 females) individuals, and ZZ individuals receiving AAT augmentation therapy (Zemaira from CSL Behring, n = 5, 3 males, 2 females) were recruited in this study. Asymptomatic MM individuals were control individuals with no evidence of any disease, respiratory symptoms and not on any medication. All controls had an MM phenotype, with serum AAT concentration within the normal range (25 to 50 µM) (mean age 29.82 ± 4.26). Asymptomatic ZZ individuals (mean age 32.18 ± 2.98) and symptomatic ZZ individuals receiving AAT augmentation therapy (mean age 49.91 ± 3.87) were recruited from the Irish AAT deficiency registry. The term ‘symptomatic’ indicates evidence of symptoms and signs of COPD with pulmonary function tests showing an obstructive pattern i.e. FEV1/FVC < 70%. Asymptomatic ZZ individuals were clinically stable, with no evidence of COPD symptoms or exacerbations in the previous 6 months. Mean forced expiratory volume in 1 second (FEV1) were were 74.13% ± 12.45 and 96.12% ± 6.15% predicted for symptomatic and non-symptomatic ZZ individuals respectively. ZZ individuals receiving AAT augmentation therapy were receiving plasma-purified AAT from CSL Behring (Zemaira), administered intravenously at a dosage of 60 mg/kg body weight weekly. Thus, in this study the term Day 0 refers to ‘pre-AAT augmentation therapy’ but also implies ‘Day 7’ whilst Day 2 refers to ‘48 hours post-AAT augmentation therapy’. Patients were free from exacerbations at least 4 weeks prior to obtaining blood samples. All ZZ individuals had a ZZ phenotype determined by isoelectric focussing, with serum concentrations of AAT less than 11 µM and confirmed with allele-specific PCR. All methods were carried out in accordance with relevant guidelines and regulations of the research ethics committee of Beaumont Hospital Dublin who approved this study. Full informed consent was obtained from all subjects.
Isolation, culture and treatment of peripheral blood monocytes
Mononuclear cells were isolated using heparinized venous peripheral blood and treated with Lymphoprep (Axis Shield) for density gradient centrifugation. The mononuclear cell band was aspirated, washed with HBSS (Invitrogen) and monocytes were purified using the EasySep Human CD14 Selection Cocktail (StemCell Technologies). Cells were maintained in RPMI 1640, 10% (v/v) fetal calf serum (Life Technologies) and 1% penicillin/streptomycin (Invitrogen) at 37 °C in a 5% CO2 atmosphere. To induce endoplasmic reticulum (ER) stress, MM monocytes were treated with DMSO (vehicle control) or thapsigargin at 50 nM for 1 hour. For NFκB agonist and antagonist experiments, MM monocytes were treated with 500 U/ml TNFα or 20 µM BAY-11 7082 for 4 hours respectively. Treatment with exogenous AAT (Athens Research & Technology) at 27.5 µM for 4 hours was performed to validate the effects of AAT replacement ex vivo.
miRNA and mRNA expression profiling
miRNA (40 ng) was prepared using the nCounter miRNA Sample Preparation Kit (Nanostring Technologies) according to manufacturer’s instructions (n = 3 in each group) and profiled commercially with the nCounter miRNA Expression Assay. Raw data was normalized based on the relative number of positive and negative control counts and adjusted for probe and background corrections for each miRNA as instructed in the nCounter Data Analysis Guidelines. Significance was calcuated using non-parametric permutation tests with a p-value of permutation < 0.003 considered statistically significant.
mRNA expression profiling was performed by Arraystar, Inc. (Rockville, MD, USA) on RNA from THP-1 cells or monocytes isolated from MMs, asymptomatic ZZs, symptomatic ZZs on Day 0 or Day 2, and asymptomatic ZZ monocytes treasted and not treated with 27 µM AAT for 4 hours (pooled n = 3 each). For microarray analysis an Agilent Array platform was employed and analysed as described in McKiernan et al.34. Approximately 26,109 coding transcripts collected from RefSeq (release 55), UCSC Human (GRCh37/hg19) and GENCODE 13 were detected. Differentially expressed (DE) mRNAs between two groups were identified through volcano plot filtering, and hierarchical clustering was performed to show distinguishable mRNA expression patterns among samples.
Quantitative assessment of mRNA and miRNA levels
TRI reagent was used to isolate RNA according to the manufacturer’s instructions and 500 ng was reverse transcribed into cDNA using the Quantitect Reverse Transcription Kit (Qiagen). Oligonucleotide primers were synthesized (MWG Operon) and quantitative PCR reactions were performed in 20 µl containing 2 µl of template cDNA, SYBR Green MasterMix (Roche) and 10 pmol of each primer. For miRNA expression 100 ng of RNA was used in Taqman miRNA assays (Applied Biosystems) according to manufacturer’s instructions. A Roche LC 480 Lightcycler was used for amplification of both mRNA and miRNA in triplicate. Relative expression of mRNA and miRNA relative to GAPDH and U6 snRNA respectively was determined using the 2−ΔΔCt method.
Western blot analyses
Equal volumes of cell lysates were separated by NuPage ® Novex 4–12% Bis-Tris Gels (Life Technologies) in MOPS SDS running buffer (Life Technologies) and transferred onto nitrocellulose membranes (Sigma-Aldrich). Membranes were probed with primary antibodies (rabbit anti-p50, Santa Cruz, 1:1000 dilution or mouse anti-p65, Santa Cruz, 1:1000 dilution) and signal detection was determined using the Immobilon® Western HRP Substrate (Milipore) on the Syngene G:Box chemi XL gel documentation system. Densitometry was analysed using GeneTools software on the same system.
Bioinformatic analyses
Diana-miRGen 2.0 was used to analyse miRNA genomic information for predicted transcription factors binding sites in miRNA genes. NFκB binding sites in genes commonly downregulated in vivo on Day 2 vs Day 0, and in ZZ monocytes treated ex vivo with AAT vs. untreated ZZ monocytes were identified using the Genomatix Common Transcription Factor Binding Site software. TarBase was employed to identify the genes, among those commonly upregulated in vivo on Day 2 vs Day 0, and in ZZ monocytes treated ex vivo with AAT vs. untreated ZZ monocytes, that were reported to be targeted by the NFκB-regulated miRNAs. This list of genes was used as an input to perform overrepresentation analysis with WebGestalt (WEB-based Gene SeT Analysis Toolkit; http://www.webgestalt.org/option.php) using the whole human genome as the reference gene list.
The downregulated genes identified common to both Day 2 vs. Day 0 and ZZ + AAT vs. Control with an absolute fold change greater than 10 (n = 8) were uploaded to Enrichr (gene set enrichment analysis web server)21 and the gene ontology biological processes, molecular function and pathway involvement of the genes was explored. The significantly associated gene ontology terms (adjusted p-value < 0.05) were imported to REVIGO22 where they were clustered based on their relatedness and any redundancy was removed. Significantly enriched BioCarta, KEGG, NCI-Nature, Reactome and WikiPathways pathways, with adjusted p-value < 0.05 were exported from Enrichr and plotted.
A Gene Set Enrichment Analysis35 on downregulated genes after AAT augmentation therapy or following in vitro treatment with AAT using a NFκB gene signature was performed to support NFκB involvement.
Statistical analysis
All analyses were performed using GraphPad PRISM 4.0 (San Diego, CA). Results are expressed as the mean ± SEM and were compared by Student t test or ANOVA with Bonferroni correction for multiple testing, as appropriate. Differences were considered significant at p ≤ 0.05 for individual comparisons.
Data availability
Data generated or analysed during this study are included in this published article and its Supplementary Information files.
References
Greene, C. M. et al. alpha1-Antitrypsin deficiency. Nat Rev Dis Primers 2, 16051 (2016).
Carroll, T. P. et al. Evidence for unfolded protein response activation in monocytes from individuals with alpha-1 antitrypsin deficiency. J Immunol 184, 4538–46 (2010).
Hassan, T. et al. miR-199a-5p silencing regulates the unfolded protein response in chronic obstructive pulmonary disease and alpha1-antitrypsin deficiency. Am J Respir Crit Care Med 189, 263–73 (2014).
Survival and FEV1 decline in individuals with severe deficiency of alpha1-antitrypsin. The Alpha-1-Antitrypsin Deficiency Registry Study Group. Am J Respir Crit Care Med 158, 49–59 (1998).
Lieberman, J. Augmentation therapy reduces frequency of lung infections in antitrypsin deficiency: a new hypothesis with supporting data. Chest 118, 1480–5 (2000).
Wencker, M., Fuhrmann, B., Banik, N. & Konietzko, N. & Wissenschaftliche Arbeitsgemeinschaft zur Therapie von, L. Longitudinal follow-up of patients with alpha(1)-protease inhibitor deficiency before and during therapy with IV alpha(1)-protease inhibitor. Chest 119, 737–44 (2001).
Tonelli, A. R., Rouhani, F., Li, N., Schreck, P. & Brantly, M. L. Alpha-1-antitrypsin augmentation therapy in deficient individuals enrolled in the Alpha-1 Foundation DNA and Tissue Bank. Int J Chron Obstruct Pulmon Dis 4, 443–52 (2009).
Seersholm, N. et al. Does alpha1-antitrypsin augmentation therapy slow the annual decline in FEV1 in patients with severe hereditary alpha1-antitrypsin deficiency? Wissenschaftliche Arbeitsgemeinschaft zur Therapie von Lungenerkrankungen (WATL) alpha1-AT study group. Eur Respir J 10, 2260–3 (1997).
Dirksen, A. et al. A randomized clinical trial of alpha(1)-antitrypsin augmentation therapy. Am J Respir Crit Care Med 160, 1468–72 (1999).
Dirksen, A. et al. Exploring the role of CT densitometry: a randomised study of augmentation therapy in alpha1-antitrypsin deficiency. Eur Respir J 33, 1345–53 (2009).
Stockley, R. A. et al. Therapeutic efficacy of alpha-1 antitrypsin augmentation therapy on the loss of lung tissue: an integrated analysis of 2 randomised clinical trials using computed tomography densitometry. Respir Res 11, 136 (2010).
Chapman, K. R. et al. Intravenous augmentation treatment and lung density in severe alpha1 antitrypsin deficiency (RAPID): a randomised, double-blind, placebo-controlled trial. Lancet 386, 360–8 (2015).
McElvaney, N. G. et al. Long-term efficacy and safety of alpha1 proteinase inhibitor treatment for emphysema caused by severe alpha1 antitrypsin deficiency: an open-label extension trial (RAPID-OLE). Lancet Respir Med 5, 51–60 (2017).
O’Dwyer, C. A. et al. The BLT1 Inhibitory Function of alpha-1 Antitrypsin Augmentation Therapy Disrupts Leukotriene B4 Neutrophil Signaling. J Immunol 195, 3628–41 (2015).
Bergin, D. A. et al. alpha-1 Antitrypsin regulates human neutrophil chemotaxis induced by soluble immune complexes and IL-8. J Clin Invest 120, 4236–50 (2010).
Bergin, D. A. et al. The circulating proteinase inhibitor alpha-1 antitrypsin regulates neutrophil degranulation and autoimmunity. Sci Transl Med 6, 217ra1 (2014).
Subramaniyam, D. et al. Effects of alpha 1-antitrypsin on endotoxin-induced lung inflammation in vivo. Inflamm Res 59, 571–8 (2010).
Janciauskiene, S. M., Nita, I. M. & Stevens, T. Alpha1-antitrypsin, old dog, new tricks. Alpha1-antitrypsin exerts in vitro anti-inflammatory activity in human monocytes by elevating cAMP. J Biol Chem 282, 8573–82 (2007).
Jonigk, D. et al. Anti-inflammatory and immunomodulatory properties of α1-antitrypsin without inhibition of elastase. Proc Natl Acad Sci USA 110, 15007–12 (2013).
Geraghty, P. et al. α1-Antitrypsin activates protein phosphatase 2A to counter lung inflammatory responses. Am J Respir Crit Care Med. 190, 1229–42 (2014).
Kuleshov, M. V. et al. Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res 44, W90–7 (2016).
Supek., F., Bošnjak., M., Škunca., N. & Šmuc, T. REVIGO summarizes and visualizes long lists of gene ontology terms. PLoS One. 6, e21800 (2011).
Lomas, D. A., Evans, D. L., Finch, J. T. & Carrell, R. W. The mechanism of Z alpha1-antitrypsin accumulation in the liver. Nature 357, 605–7 (1992).
Guo, H., Ingolia, N. T., Weissman, J. S. & Bartel, D. P. Mammalian microRNAs predominantly act to decrease target mRNA levels. Nature 466, 835–40 (2010).
Ye, J. et al. hnRNP U protein is required for normal pre-mRNA splicing and postnatal heart development and function. Proc Natl Acad Sci USA 112, E3020–9 (2015).
Zhao, W. et al. Nuclear to cytoplasmic translocation of heterogeneous nuclear ribonucleoprotein U enhances TLR-induced proinflammatory cytokine production by stabilizing mRNAs in macrophages. J Immunol 188, 3179–87 (2012).
Richter-Cook, N. J., Dever, T. E., Hensold, J. O. & Merrick, W. C. Purification and characterization of a new eukaryotic protein translation factor. Eukaryotic initiation factor 4H. J Biol Chem 273, 7579–87 (1998).
Bai, Y. et al. Overexpression of miR-519d in lung adenocarcinoma inhibits cell proliferation and invasion via the association of eIF4H. Tumour Biol 39, 1010428317694566 (2017).
Wu, D., Matsushita, K., Matsubara, H., Nomura, F. & Tomonaga, T. An alternative splicing isoform of eukaryotic initiation factor 4H promotes tumorigenesis in vivo and is a potential therapeutic target for human cancer. Int J Cancer 128, 1018–30 (2011).
Boele, J. et al. PAPD5-mediated 3′ adenylation and subsequent degradation of miR-21 is disrupted in proliferative disease. Proc Natl Acad Sci USA 111, 11467–72 (2014).
Ou, M. et al. Identification of potential microRNA-target pairs associated with osteopetrosis by deep sequencing, iTRAQ proteomics and bioinformatics. Eur J Hum Genet 22, 625–32 (2014).
Lawless, M. W. et al. Activation of endoplasmic reticulum-specific stress responses associated with the conformational disease Z alpha 1-antitrypsin deficiency. J Immunol 172, 5722–6 (2004).
Hidvegi, T., Schmidt, B. Z., Hale, P. & Perlmutter, D. H. Accumulation of mutant alpha1-antitrypsin Z in the endoplasmic reticulum activates caspases-4 and -12, NFkappaB, and BAP31 but not the unfolded protein response. J Biol Chem 280, 39002–15 (2005).
McKiernan, P. J., Molloy, K., Cryan, S. A., McElvaney, N. G. & Greene, C. M. Long noncoding RNA are aberrantly expressed in vivo in the cystic fibrosis bronchial epithelium. Int J Biochem Cell Biol 52, 184–91 (2014).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci USA 102, 15545–50 (2005).
Acknowledgements
Funding for this work is gratefully acknowledged from the Alpha One Foundation. The authors would like to thank Hans-Georg Koenig and Paul McKiernan, RCSI for advice and technical assistance.
Author information
Authors and Affiliations
Contributions
T.H. concept, experimental design, clinical sample collection, experiments, writing of the manuscript; C.D.S. and C.M. bioinformatics, writing of the manuscript; N.M. concept, patient cohorts; C.M.G. concept, experimental design, microarray, bioinformatics, writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hassan, T., de Santi, C., Mooney, C. et al. Alpha-1 antitrypsin augmentation therapy decreases miR-199a-5p, miR-598 and miR-320a expression in monocytes via inhibition of NFκB. Sci Rep 7, 13803 (2017). https://doi.org/10.1038/s41598-017-14310-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-14310-2
This article is cited by
-
MicroRNA-598 inhibition ameliorates LPS-induced acute lung injury in mice through upregulating Ebf1 expression
Histochemistry and Cell Biology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.