Abstract
Studies on serum alkaline phosphatase (ALP) and mortality risk in patients with end-stage renal disease (ESRD) undergoing dialysis have yielded conflicting results. This meta-analysis was designed to assess the association of serum ALP levels with cardiovascular or all-cause mortality risk among patients on dialysis. PubMed and Embase databases were searched until March 2017 for studies evaluating the association of serum ALP levels and cardiovascular or all-cause mortality risk in adult patients with ESRD undergoing maintenance hemodialysis or chronic peritoneal dialysis. Twelve studies enrolling 393,200 patients on dialysis were included. Compared with the reference low serum ALP category, pooled adjusted hazard risk (HR) of all-cause mortality was 1.46 (95% confidence interval [CI] 1.30–1.65) for patients on hemodialysis and 1.93 (95% CI 1.71–2.17) for peritoneal patients on dialysis. In addition, elevated serum ALP significantly increased cardiovascular mortality among patients on peritoneal dialysis (HR 2.39; 95% CI 1.23–4.65) but not in patients on hemodialysis (HR 1.08; 95% CI 0.84–1.40). Elevated serum ALP was an independent risk factor for all-cause mortality among patients on hemodialysis or peritoneal dialysis. Further well-designed prospective studies are needed to investigate the association of high serum ALP levels with cardiovascular mortality among patients on dialysis.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a global public health concern1. End-stage renal disease (ESRD) is a chronic and progressive decline in kidney function. A substantial number of CKD patients progress to ESRD and impose an enormous health and economic burden2. More than two million people suffer from ESRD worldwide3. Renal replacement therapy with maintenance hemodialysis or chronic peritoneal dialysis is increasingly used in the care of patients with ESRD4. Given that patients with ESRD undergoing dialysis have a substantial risk of mortality5,6, the risk factors for mortality in this population should be identified.
Alkaline phosphatase (ALP) is a hydrolase enzyme that catalyzes phosphate from nucleotides and proteins7. ALP usually originates from the liver or bone and concentrates in the bone, liver, placenta, and kidney. Several8,9,10,11,12,13,14,15,16,17,18 but not all19,20 epidemiologic studies reported that elevated serum levels of ALP are associated with increased all-cause mortality among patients on hemodialysis and peritoneal dialysis. Nonetheless, for cardiovascular mortality, studies10,14,15,20 have yielded contradicting results. Meanwhile, the risk estimates of the association vary widely.
Previous meta-analyses did not assess the effect of serum ALP levels on subsequent mortality risk among patients on dialysis. Given the varied and conflicting findings in the published studies, we conducted this meta-analysis to investigate whether baseline serum levels of ALP are an independent predictor of cardiovascular or all-cause mortality in patients with ESRD on hemodialysis or peritoneal dialysis.
Results
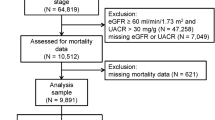
Search results and study characteristics
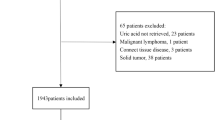
A flowchart of the study selection process is presented in Fig. 1. In brief, 146 articles were retrieved in the initial literature searches after removing duplicates. Subsequently, 134 articles were excluded after applying our predefined inclusion criteria. Thus, 12 studies8,9,10,11,12,13,14,15,16,17,20,21 with 393,200 patients on dialysis were finally included in the meta-analysis. Table 1 presents a summary of the general characteristics of the included studies. These included studies were mainly conducted in the United States8,9,10,12,13, mainland China14, Japan11,15, South Africa17, and Taiwan16,20,21. One study10 was a retrospective analysis of a randomized controlled trial, and others were retrospective cohort designs. Eight studies8,9,10,11,15,16,17,20 enrolled patients on hemodialysis, three studies13,14,21 enrolled patients on peritoneal dialysis, and one study12 comprised both patients on hemodialysis and peritoneal dialysis. Individual study sample sizes varied from 90 to 185,277, and the follow-up duration ranged from 1.0 year to 7.0 years. The mean reported age of patients was between 47.5 and 66 years. Six studies8,9,12,15,16,20 with 7 to 8 Newcastle–Ottawa Scale (NOS) stars were grouped as good quality, and the others10,11,13,14,17,21 achieved 5–6 stars.
Association of serum ALP and all-cause mortality
Nine included studies8,9,10,11,12,15,16,17,20 investigated the association of serum ALP with all-cause mortality among patients on hemodialysis. As shown in Fig. 2, elevated serum ALP levels were associated with increased all-cause mortality (HR 1.46; 95% CI 1.30–1.65) in the random effect model compared with the reference low serum ALP. Substantial heterogeneity (I 2 = 88.9%; p < 0.001) was observed among the included studies. Evidence of publication bias was not found as determined by the Begg’s test (p = 0.754), Egger’s test (p = 0.147), and funnel plot (Fig. 3). Stratified analyses indicated that associations were consistently observed between elevated serum ALP levels and all-cause mortality risk in each predefined subgroup (Table 2).
Four studies12,13,14,21 investigated the association of serum ALP with all-cause mortality among patients on peritoneal dialysis. As shown in Fig. 4, the pooled HR for all-cause mortality was 1.93 (95% CI 1.71–2.17) when the highest was compared with the reference low serum ALP levels in a fixed-effect model, and no heterogeneity was found across studies (I 2 = 0.0%; p = 0.578).
Association of serum ALP and cardiovascular mortality
Three studies10,15,20 assessed the association of serum ALP with cardiovascular mortality among patients on hemodialysis. As shown in Fig. 5, elevated serum ALP levels were not associated with increased cardiovascular mortality (HR 1.08; 95% CI 0.84–1.40) in a random effect model compared with the reference low serum ALP with substantial heterogeneity across studies (I 2 = 52.7%; p = 0.097). Sensitivity analyses by removal of any study at a time did not change the direction of the pooled effect size (data not shown).
Two studies14,21 reported cardiovascular mortality as an outcome among patients on peritoneal dialysis. As shown in Fig. 6, elevated serum ALP levels significantly increased cardiovascular mortality (HR 2.39; 95% CI 1.23–4.65) in a fixed-effect model compared with the reference low serum ALP, and substantial heterogeneity was found across studies (I 2 = 0%; p = 0.956).
Discussion
This study is the first meta-analysis to evaluate the association between serum ALP and risk of cardiovascular and all-cause mortality in patients on dialysis. The main finding of the current meta-analysis showed that elevated serum ALP levels were associated with an increased all-cause mortality risk in patients on dialysis even after adjustment of liver enzymes and bone metabolism parameters. In addition, elevated serum ALP levels appeared to significantly increase cardiovascular mortality among patients on peritoneal dialysis. However, no clear effect was indicated on cardiovascular mortality risk prediction among patients on hemodialysis.
Circulating ALP levels often increase in ESRD. In this study, the observed all-cause mortality risk was more pronounced among patients on peritoneal dialysis than among patients on hemodialysis. Patients on hemodialysis with the highest serum ALP levels significantly increased 46% risk of all-cause mortality. Alternatively, patients on peritoneal dialysis exhibiting the highest serum ALP levels were associated with 93% risk of all-cause mortality. In addition, the association was more pronounced among studies with a short follow up than studies with a long follow-up duration. One-year mortality was 19.8% among 385,074 patients on hemodialysis22. The presence of bone and liver diseases may affect the association of serum ALP with mortality risk. However, the association was still observed in the studies even after adjustment for liver function tests and serum levels of parathyroid hormone, phosphorus, and calcium. Therefore, serum ALP levels should be considered as an independent risk factor for all-cause mortality.
Cardiovascular disease is the main cause of death in patients receiving dialysis23,24. However, the association between serum ALP levels and cardiovascular mortality risk in patients on hemodialysis is unclear. Our meta-analysis indicated that elevated serum ALP levels appeared to significantly increase cardiovascular mortality among patients on peritoneal dialysis but not in patients with hemodialysis. When serum ALP was used as a time-varying exposure variable, high (≥97 IU/l) versus low ALP (<97 IU/l) was associated with a 34% higher risk of cardiovascular mortality10. This finding suggested that the effect of ALP, which leads to increasing cardiovascular death, was time-dependent.
Serum ALP is primarily used as an indicator for hepatic and bone disease. Apart from liver and bone diseases, serum ALP levels are elevated in various cancers, chlorpropamide therapy, hormonal contraception, pregnancy, and hyperthyroidism25. Our findings were in line with evidence from a previous meta-analysis26; elevated serum levels of ALP indicated a high all-cause mortality in people with normal or preserved renal function. Moreover, elevated serum bone-specific ALP was also associated with mortality risk in patients on hemodialysis19,27.
The exact mechanisms for the association of alkaline phosphatase with mortality risk remain unclear. A possible explanation for the observed association is that ALP is a marker of high-turnover bone disease28. ALP can promote vascular calcification by hydrolyzing pyrophosphate in the arterial wall29,30,31. In addition, inflammation may be another potential mechanism for the association between high serum ALP levels and increased mortality32.
Several potential limitations should be mentioned in this meta-analysis. First, substantial heterogeneity was observed among studies involving patients on hemodialysis. However, substantial heterogeneity did not obviously disappear in the subgroup analysis. The observed heterogeneity may be correlated with patient characteristics and dialysis regimen. Second, serum ALP levels were determined at a single time, and misclassification in ALP categories was not excluded. Third, a “U”-shaped correlation between all-cause mortality and serum levels of ALP was reported in patients on hemodialysis. Low ALP was associated with a high risk of all-cause mortality12. Thus, selecting the lowest serum ALP as a reference value may have underestimated the actual risk estimate. Finally, all the included studies were retrospective analyses of an existing database, and more prospective cohort studies are needed to confirm this association.
Elevated serum ALP was an independent risk factor for all-cause mortality among patients on hemodialysis or peritoneal dialysis. Our findings revealed that patients on dialysis with elevated serum ALP were candidates at high risk of all-cause mortality, and low ALP levels may reduce all-cause mortality rates in the dialysis population. However, a U-shaped association of serum ALP with mortality risk in patients on dialysis needs to further investigated. Moreover, future well-designed prospective studies are necessary to investigate the association between elevated serum ALP and cardiovascular mortality among patients on dialysis.
Methods
Data sources and search strategy
This meta-analysis was performed and reported following the standard criteria of the Meta-analysis Of Observational Studies in Epidemiology statement33. A comprehensive literature search was conducted using the PubMed and Embase databases from inception to March 2017. Key words used for the search were (alkaline phosphatase) AND (end-stage renal disease OR renal replacement therapy OR hemodialysis OR peritoneal dialysis) AND (death OR mortality) AND (follow-up OR longitudinal). Language restrictions were not applied in the electronic literature searches. To identify additional eligible studies, we manually reviewed the reference lists of relevant articles.
Study selection
Studies were included according to the following inclusion criteria: (1) prospective or retrospective cohort studies; (2) inclusion of patients with ESRD undergoing hemodialysis or peritoneal dialysis; (3) baseline serum ALP levels as exposure; and (4) provided multiple adjusted odds ratio (OR) or hazard ratio (HR) and 95% confidence interval (CI) of cardiovascular or all-cause mortality comparing the highest with the reference lower serum ALP levels. Exclusion criteria were (1) pre-dialysis CKD patients; (2) skeletal ALP as exposure; (3) time-varying serum ALP as exposure; and (4) risk estimates were not reported separately for patients on hemodialysis or peritoneal dialysis.
Data collection and quality assessment
The following items were extracted from the included articles by two independent authors: first author’s surname, publication year, origin of study, study design, sample size, type of dialysis, mean age of patients, male gender proportion, cutoff value of ALP comparison, number of death events, multivariate adjusted risk estimates for all-cause or cardiovascular mortality, follow-up period, and adjustment variables. To assess the quality of the included studies, Newcastle-Ottawa Scale (NOS) for cohort studies34 was used to evaluate the methodological quality. The following three aspects were assessed: selection of study participants, comparability of groups, and ascertainment of outcomes. Using this scale, the maximum score was 9 stars. Studies were graded as good quality if they achieved a score of ≥7 stars. Disagreements in data collection and quality assessment were resolved through consensus.
Data synthesis and analysis
All the meta-analyses were performed using STATA software (version 12.0). The pooled multivariable-adjusted HR and 95% CI of cardiovascular or all-cause mortality was computed for the highest versus the reference low category of serum ALP levels. Statistical heterogeneity across studies was assessed using the Cochrane Q test and I 2 statistic. The significance of the statistical heterogeneity was set at the I 2 statistic ≥50% and/or Cochrane Q test p < 0.10. We selected a random effect model for pooling risk estimates if significant statistical heterogeneity was present; otherwise, a fixed-effect model was utilized. Subgroup analyses were planned for patient types (hemodialysis versus peritoneal dialysis), region (Asia versus no-Asia), sample size (≥2000 versus <2000), mean age (≥60 versus <60), comparison of ALP levels (single cutoff versus ≥3 category analysis), follow-up duration (≥3 years versus <3 years), and NOS stars (≥7 versus <7). Publication bias was assessed using the Begg’s test, Egger’s test, and a funnel plot.
References
Hill, N. R. et al. Global Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-Analysis. PLoS One 11, e0158765 (2016).
Wang, V., Vilme, H., Maciejewski, M. L. & Boulware, L. E. The Economic Burden of Chronic Kidney Disease and End-Stage Renal Disease. Semin Nephrol 36, 319–30 (2016).
Robinson, B. M. et al. Factors affecting outcomes in patients reaching end-stage kidney disease worldwide: differences in access to renal replacement therapy, modality use, and haemodialysis practices. Lancet 388, 294–306 (2016).
Thomas, B. et al. Maintenance Dialysis throughout the World in Years 1990 and 2010. J Am Soc Nephrol 26, 2621–33 (2015).
Cheung, A. K. et al. Atherosclerotic cardiovascular disease risks in chronic hemodialysis patients. Kidney Int 58, 353–62 (2000).
Herzog, C. A. et al. Cardiovascular disease in chronic kidney disease. A clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 80, 572–86 (2011).
Sharma, U., Pal, D. & Prasad, R. Alkaline phosphatase: an overview. Indian J Clin Biochem 29, 269–78 (2014).
Regidor, D. L. et al. Serum alkaline phosphatase predicts mortality among maintenance hemodialysis patients. J Am Soc Nephrol 19, 2193–203 (2008).
Abramowitz, M. et al. Serum alkaline phosphatase and phosphate and risk of mortality and hospitalization. Clin J Am Soc Nephrol 5, 1064–71 (2010).
Beddhu, S., Baird, B., Ma, X., Cheung, A. K. & Greene, T. Serum alkaline phosphatase and mortality in hemodialysis patients. Clin Nephrol 74, 91–6 (2010).
Yamashita, T., Shizuku, J., Ohba, T., Kabaya, T. & Nitta, K. Serum alkaline phosphatase levels and mortality of chronic hemodialysis patients. Int J Clin Med 2, 388–93 (2011).
Rhee, C. M. et al. Comparative mortality-predictability using alkaline phosphatase and parathyroid hormone in patients on peritoneal dialysis and hemodialysis. Perit Dial Int 34, 732–48 (2014).
Fein, P. A. et al. Relationship between alkaline phosphatase and all-cause mortality in peritoneal dialysis patients. Adv Perit Dial 29, 61–3 (2013).
Liu, X. et al. Alkaline phosphatase and mortality in patients on peritoneal dialysis. Clin J Am Soc Nephrol 9, 771–8 (2014).
Maruyama, Y. et al. A higher serum alkaline phosphatase is associated with the incidence of hip fracture and mortality among patients receiving hemodialysis in Japan. Nephrol Dial Transplant 29, 1532–8 (2014).
Chang, J. F. et al. Combined alkaline phosphatase and phosphorus levels as a predictor of mortality in maintenance hemodialysis patients. Medicine (Baltimore) 93, e106 (2014).
Waziri, B., Duarte, R. & Naicker, S. High Serum Alkaline Phosphatase, Hypercalcaemia, Race, and Mortality in South African Maintenance Haemodialysis Patients. Int J Nephrol 2017, 2795432 (2017).
Scialla, J. J. et al. Race, Mineral Homeostasis and Mortality in Patients with End-Stage Renal Disease on Dialysis. Am J Nephrol 42, 25–34 (2015).
Drechsler, C. et al. Bone alkaline phosphatase and mortality in dialysis patients. Clin J Am Soc Nephrol 6, 1752–9 (2011).
Zhu, J. G. et al. Serum Alkaline Phosphatase Levels are Not Associated with Increased Death Risk in Prevalent Hemodialysis Patients: 5-Year Experience in a Single Hemodialysis Center. Kidney Blood Press Res 41, 498–506 (2016).
Liu, Y. et al. An association between time-varying serum alkaline phosphatase concentrations and mortality rate in patients undergoing peritoneal dialysis: a five-year cohort study. Sci Rep 7, 43314 (2017).
Yan, G. et al. Facility size, race and ethnicity, and mortality for in-center hemodialysis. J Am Soc Nephrol 24, 2062–70 (2013).
Wakasugi, M., Kazama, J. J. & Narita, I. Mortality trends among Japanese dialysis patients, 1988–2013: a joinpoint regression analysis. Nephrol Dial Transplant 31, 1501–7 (2016).
Allon, M. Evidence-based cardiology in hemodialysis patients. J Am Soc Nephrol 24, 1934–43 (2013).
Fernandez, N. J. & Kidney, B. A. Alkaline phosphatase: beyond the liver. Vet Clin Pathol 36, 223–33 (2007).
Li, J. W., Xu, C., Fan, Y., Wang, Y. & Xiao, Y. B. Can serum levels of alkaline phosphatase and phosphate predict cardiovascular diseases and total mortality in individuals with preserved renal function? A systemic review and meta-analysis. PLoS One 9, e102276 (2014).
Kobayashi, I. et al. Higher serum bone alkaline phosphatase as a predictor of mortality in male hemodialysis patients. Life Sci 90, 212–8 (2012).
Kalantar-Zadeh, K. et al. Survival predictability of time-varying indicators of bone disease in maintenance hemodialysis patients. Kidney Int 70, 771–80 (2006).
Lomashvili, K. A., Garg, P., Narisawa, S., Millan, J. L. & O’Neill, W. C. Upregulation of alkaline phosphatase and pyrophosphate hydrolysis: potential mechanism for uremic vascular calcification. Kidney Int 73, 1024–30 (2008).
Schoppet, M. & Shanahan, C. M. Role for alkaline phosphatase as an inducer of vascular calcification in renal failure? Kidney Int 73, 989–91 (2008).
Shantouf, R. et al. Association of serum alkaline phosphatase with coronary artery calcification in maintenance hemodialysis patients. Clin J Am Soc Nephrol 4, 1106–14 (2009).
Beddhu, S., Ma, X., Baird, B., Cheung, A. K. & Greene, T. Serum alkaline phosphatase and mortality in African Americans with chronic kidney disease. Clin J Am Soc Nephrol 4, 1805–10 (2009).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–12 (2000).
Wells, G. et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (assessed August 20, 2016).
Acknowledgements
This work was supported by Jiangsu Provincial Key&D special Fund (BE2015666).
Author information
Authors and Affiliations
Contributions
Yu Fan and Xin Jin made the literature research, extracted data, and evaluated the quality. Menglin Jiang drafted the manuscript and performed the statistical analysis. Na Fang designed the study, interpreted the results, and revised the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fan, Y., Jin, X., Jiang, M. et al. Elevated serum alkaline phosphatase and cardiovascular or all-cause mortality risk in dialysis patients: A meta-analysis. Sci Rep 7, 13224 (2017). https://doi.org/10.1038/s41598-017-13387-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-13387-z
This article is cited by
-
Data-driven, two-stage machine learning algorithm-based prediction scheme for assessing 1-year and 3-year mortality risk in chronic hemodialysis patients
Scientific Reports (2023)
-
Intestinal alkaline phosphatase modulation by food components: predictive, preventive, and personalized strategies for novel treatment options in chronic kidney disease
EPMA Journal (2020)
-
Factors associated with low trabecular bone scores in patients with end-stage kidney disease
Journal of Bone and Mineral Metabolism (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.