Abstract
A novel in-vitro test (T50-test) assesses ex-vivo serum calcification propensity which predicts mortality in HD patients. The association of longitudinal changes of T50 with all-cause and cardiovascular mortality has not been investigated. We assessed T50 in paired sera collected at baseline and at 24 months in 188 prevalent European HD patients from the ISAR cohort, most of whom were Caucasians. Patients were followed for another 19 [interquartile range: 11–37] months. Serum T50 exhibited a significant decline between baseline and 24 months (246 ± 64 to 190 ± 68 minutes; p < 0.001). With serum Δ-phosphate showing the strongest independent association with declining T50 (r = −0.39; p < 0.001) in multivariable linear regression. The rate of decline of T50 over 24 months was a significant predictor of all-cause (HR = 1.51 per 1SD decline, 95% CI: 1.04 to 2.2; p = 0.03) and cardiovascular mortality (HR = 2.15; 95% CI: 1.15 to 3.97; p = 0.02) in Kaplan Meier and multivariable Cox-regression analysis, while cross-sectional T50 at inclusion and 24 months were not. Worsening serum calcification propensity was an independent predictor of mortality in this small cohort of prevalent HD patients. Prospective larger scaled studies are needed to assess the value of calcification propensity as a longitudinal parameter for risk stratification and monitoring of therapeutic interventions.
Similar content being viewed by others
Introduction
Disturbed calcium and phosphate homeostasis, vascular disease progression and excess mortality, largely attributable to cardiovascular (CV) causes, remain unresolved issues in haemodialysis (HD) patients1,2,3. Non-traditional risk factors, e.g. chronic inflammation, malnutrition and aberrant bone turn over gain increasing importance along with declining renal function4. Besides monitoring and targeting calcium and phosphate, the physiological humoral system, which resists the formation of calcium-phosphate-nanocrystal-formation in biological fluids, has largely been neglected.
Recently, Pasch et al. developed an in-vitro test (T50-test), that time-dependently assesses the calcification propensity of human serum in the presence of supersaturating doses of calcium and phosphate5,6. In this process, amorphous primary calciprotein particles (CPP) spontaneously grow into crystallized secondary CPP5. The transformation time T50 is thought to reflect the complex interplay of anti- and pro-calcifying serum components, such as calcium and phosphate on the one and such as magnesium, fetuin-A and albumin on the other hand5,6,7. A shorter T50 time was associated with accelerated vascular stiffness progression and overall mortality in chronic kidney disease stage III-IV7. Lower T50 values were also shown to predict graft failure, CV and all-cause mortality in renal transplant recipients8,9.
A recently published study revealed a moderate, yet independent association of decreased serum T50 with mortality and CV endpoints in patients of the original “Evaluation of Cinacalcet Therapy to Lower Cardiovascular Events” (EVOLVE) trial10,11. These data originate from 2785 HD patients with secondary hyperparathyroidism10,11. The moderate predictive capacity of T50 for all-cause mortality (HR = 1.1 per 1 SD lower T50) in the EVOLVE cohort was somewhat surprising considering that “pro-calcific pressure” should be particularly high in HD patients10,12. Interestingly, individual serum calcification propensity (T50-value) is to a large extent genetically determined13. This finding led us to hypothesize that it might not only be the absolute T50-value at a given time point, which mediated the risk of dialysis patients. Alternatively, changes to the individual’s resilience against CPP formation – a decline in T50 – throughout dialysis dependency might mirror risk more accurately. We therefore assessed T50 from serum samples collected at baseline and after 24 months in 188 HD patients to test if intra-individual changes in T50 precede mortality.
Results
This study was performed in a subgroup of 188 European haemodialysis patients of the ISAR cohort who were still alive and active in the study after the first follow up (FU) period of 24 months with a maximum spread of ± 3.2 months and for whom sera were available at both baseline and FU. Patients for whom timely 24 [23–25] months FU had been missed were excluded a priori (Fig. 1). Most patients were of Caucasian ethnicity with only four black (2%) and two Chinese (1%) participants.
Observation schedule, endpoints and selection of the study population; Patients were selected per predefined criteria stated in “methods”. Dotted arrows indicate patients not selected or leaving the study. Sera were collected at inclusion and after 24 [23–25] months of observation. Patients were then followed up for mortality for an average of 19 [11; 37] months.
In comparison with the total cohort, the study population did not significantly differ with regard to demographic parameters, body mass index (BMI) and dialysis modality. Included patients were, by nature of the study design, enriched for survivors (22.9% versus 35.8% all-cause mortality in the total cohort; p < 0.001). Additionally, history of myocardial infarction (14.4% versus 19.8%; p = 0.02) and use of central venous catheters (2.7% versus 7.3%; p = 0.001) at baseline were less frequent among included patients. Median albumin levels were slightly higher in the study population (41 g/l versus 40 g/l, p = 0.04). For details please see supplementary Table 1.
Serum calcification propensity declines in stable haemodialysis patients
Both T50 Baseline and T50 Follow up values were nearly normally distributed in this cohort (Supplementary Figure 1). Mean T50 values were 246 ± 64 minutes at baseline and 190 ± 68 minutes at time of 24 months FU indicating a significantly declining T50 over time (p < 0.001; Fig. 2A). In accordance, the histogram of T50 Change was skewed towards negative values (Fig. 2B). Of 188 patients included 31 (16%) presented with increasing T50 values. 18 (10%) patients showed stable values as defined by T50 Change = 0 ± 5,1% (5,1% was the inter-assay coefficient for T50 standards at 260 min in the EVOLVE cohort)10. Remarkably, a total of 106 (77%) patients presented declining T50 values (T50 Change < −5,1%) during 24 months of FU (Fig. 2B).
Absolute T50 at baseline and FU and percentage decline of T50; (A) Absolute T50 values at baseline (white boxplot) and at 24 months FU (grey boxplot). (B) Histogram stating the frequencies of T50 Change ((=T50 Follow up − T50 Baseline)/(T50 Baseline)) of n = 188 Patients. (C) Individual patients were sorted in descending order per their T50 Change values. Patients displaying a decline in T50 (defined by T50 Change < −5.1%; 5,1% was the inter-assay coefficient for T50 standards at 260 min in the EVOLVE cohort) were stained red. Absolute number of patients and (percent of total) are reported with dashed rectangles. The same colour code was used to stain the histogram in B.
Description of the study cohort and factors associated with declining T50 (low T50 Change)
Table 1 displays the characteristics of the study population stratified by median T50 Change (above or below −22.7%) or by median absolute T50 Follow up (above or below 192.5 min) at time of 24 months FU. Median age of the entire cohort was 71 [57–78] years. Comparing the subgroups generated by medians, no significant associations were detectable for T50 Change with age, pre-existing comorbidities (including the adapted CCI) and intake of phosphate lowering drugs. However, in univariate analysis, increased serum phosphate was higher in those with T50 Change below the median (1.7± 0.5 versus 1.5 ± 0.4 mmol/l, p < 0.001). Interestingly, Δ phosphate (=phosphateFollow up – phosphateBaseline) was also distributed differently among individuals above and below the median of T50 Change (Table 1). Whereas in the total study population absolute phosphate levels tended to decline between baseline (1.7 ± 0.5 mmol/l) and FU (1.6 ± 0.5 mmol/l; p = 0.003), patients with declining T50 values (T50 Change < −5.1%) presented with stable high phosphate levels (1.7 ± 0.5 mmol/l; ppaired t-test = 0.31). Subjects presenting with stable or increasing T50 at baseline and 24 months FU showed declining phosphate levels between baseline and 24 months FU (1.8 versus 1.5 ± 0.4 mmol/l, respectively; p < 0.001). Both groups did not significantly differ in phosphate levels measured at baseline (p = 0.43) but exhibited significantly different phosphate at 24 months FU (Fig. 3A). Δ phosphate was significantly correlated with T50 Change (r = −0.39; p < 0.001; Fig. 3B), suggesting a permanently elevated or increasing phosphate associates with declining T50. Δ phosphate remained the strongest regressor of T50 Change in multivariable linear regression (β = −8.4; 95%CI: −13.1 to−3.6; p = 0.001). R² of the model created was 0.24 - “(enter method)”. Additionally, Kt/V was a significant regressor of T50 Change (β = 5.4; 95% CI: 0.8 to 9.9; p = 0.001; Table 2). Of note, lower absolute T50 at FU was associated with higher parathyroid hormone and IL-6 levels (p = 0.01 and 0.03 respectively, Table 1).
Relation of serum phosphate and T50 Change; (A) Left: Absolute phosphate levels at baseline (broadest white boxplot) and FU (broadest grey box plot) in the total cohort (n = 188). This cohort was split per T50 decliners versus T50 non-decliners Middle: Absolute phosphate levels at baseline (white boxplot) and FU (grey boxplot) in those that declined in T50 between baseline and FU (T50 Change < −5.1%); n = 139. Right: Absolute phosphate levels at baseline (small white boxplot) and FU (small grey boxplot) in those that had stable or increasing T50 (T50 Change ≥ −5.1%); n = 49. Differences among groups regarding absolute phosphate levels were tested using paired and unpaired t-test as appropriate. (B) Dot plot depicting the correlation of T50 Change with ∆ phosphate (=phosphate Follow up−phosphate Baseline). T50 decliners and non-decliners were coloured red and blue, respectively. Pearson correlation was used to quantify the relation.
Declining T50 predicts all-cause and cardiovascular mortality in haemodialysis patients
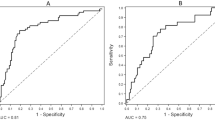
After 24 months of observation, patients were followed up for all-cause (n = 43) and CV mortality (n = 17) for a median of 19 [11–35] months. Three patients underwent renal transplantation and 12 were lost to FU (Fig. 1). In Kaplan Meier analysis, cumulative incidence of all-cause mortality was significantly higher in patients below the median of T50 Change (p = 0.02; Fig. 4A). Regarding CV-mortality a similar trend was visible although median T50 Change did not reach statistical significance (p = 0.05, Fig. 4C and D).
Univariate correlation of T50 Change and absolute T50 Change. (A) Overall cumulative incidence functions stratified by median T50 Change (=−22.7%). (B) Overall cumulative incidence functions stratified by median T50 Follow up (=192.5 min). Patients at risk and total events per group are reported below the graphs. (C) Predicted cardiovascular death incidence functions stratified by median T50 Change. (D) Predicted cardiovascular death incidence functions stratified by median T50 Follow up. Number of lethal cardiovascular events are reported below the graphs. Log-rank statistics was used for comparison of incidence functions. p-values are reported in the upper right corner of each graph.
In contrast, stratification of patients by median of T50 Follow up didn’t significantly predict all-cause mortality in our cohort (Fig. 4B). Likewise, stratification of the study population by T50 Baseline was not significantly associated with all-cause mortality (Supplementary Figure 2), likely due to the preselection described above.
Considering T50 Change on a continuous scale, declining T50 was significantly associated with all-cause mortality in Cox-regression (HR = 1.74 per SD decline; 95%CI: 1,2 to 2,51; p = 0.003). After block-wise adjustment for demographics (age, sex, BMI), comorbidities and basic laboratory parameters, 1SD = 30.5% decline in T50 remained associated with a 51% (95%CI: 4–120%; p = 0.03) increased risk for all-cause mortality. Likewise, declining T50 was associated with CV mortality (HR = 2.14; 95%CI:1.15 to 3.97; Table 3). Exclusion of non-Caucasian study participants (n = 6) did not materially affect the latter results (supplementary Table 4).
By contrast, neither absolute T50 Follow up nor T50 Baseline remained significant predictors of all-cause mortality in the final adjusted model (supplementary Table 2 and supplementary Table 3, respectively) and were relevantly associated with CV mortality in our study (not shown).
Discussion
The main findings of this subgroup analysis in chronic haemodialysis patients, were, firstly, that serum calcification propensity T50 declined between baseline and FU. Secondly, that a decline in T50 was accompanied by increasing phosphate levels at baseline and 24 months FU. Thirdly, that the intra-individual decline of calcification resistance predicts all-cause and cardiovascular mortality in HD patients. These findings suggest that observing change of T50 might add prognostic value to absolute T50 values in HD patients.
The development of the T50-test was an important step ahead for a more comprehensive assessment of colloidal chemical interactions within the complex field of “calcification and calcium x phosphate nanocrystal formation”5,10. Elevated serum phosphate, calcium, low magnesium and fetuin-A levels have long been linked to vascular calcification and mortality in ESRD and HD patients14,15,16,17,18,19,20,21,22,23,24,25. The colloidal chemical nature of the crystallization process per se suggests strong interaction effects amongst these players, which is in line with findings from cohort studies16,26,27,28. In fact, mortality is especially high for patients with both excessively high phosphate and calcium serum levels21,28. On the contrary, magnesium appears to dampen the detrimental effects of elevated phosphate levels in HD patients16. The strength of the T50-test is that it takes these interactions into account by assessing the distal tract of the calcification cascade, i.e. the interaction between calcium and phosphate, which takes place in the CPP-forming biological matrix of human serum6. Elevated serum phosphate, calcium and lower serum albumin have already been associated with lower absolute T50 at a single time point in CKD and HD patients7,10. Our data add further plausibility to this concept by indicating, that high or increasing phosphate, parallels declining T50. We did not, however, observe a similar relation for Δ albumin and Δ calcium, which might in part be due to a lower variance of these parameters between baseline and 24 months FU in our cohort. Nevertheless, our data underscore the importance of controlling serum phosphate levels in HD patients, as high or rising phosphate levels may well weaken the natural resistance against the formation of secondary CPP. However, given the moderate fit of our linear regression model, besides Δ phosphate or Kt/V other factors will also relate to declining T50. Magnesium is such a candidate indicated by our data. Unfortunately, we were unable to investigate Δ ionized magnesium levels over time, due to an incomplete magnesium-dataset at baseline.
Given that a short T50 time represents lower resistance to secondary CPP formation5,6, a decline of T50, as observed in our study, implies the loss of anti-calcific capacities of biologic fluids. In our cohort, a decline of T50 occurred over the course of dialysis dependency and was independently associated with all-cause mortality and remained associated with cardiovascular mortality after adjustment for potential confounders. As such, the per cent decline of T50 between baseline and 24-months reassessment showed a considerably stronger association with mortality than absolute T50 Follow up. Since absolute T50 values are to a large extent genetically determined in the general population13, it appears plausible that the dynamics of T50 predict future risk more accurately in HD patient, which face longitudinal weakening of their “natural“ calcification resistance. By analogy, prognosis of e.g. calcific aortic stenosis is not only determined by the absolute reduction of valve area but also the rapidity of stenosis progression which is especially high in HD patients29,30. Based on this reasoning, it is tempting to speculate that preventing a decline of T50 in HD patients or restoring T50 in those who present with declining T50 might favourably affect the future clinical course. Importantly, T50 represented the only modifiable risk factor in our adjusted Cox model for mortality. In fact, first interventional pilot studies suggest that increasing dialysate magnesium and bicarbonate act concordantly to prolong T50 time in HD patients31. Similarly, phosphate binder therapy has the potential to elevate T50 32.
Our study has several limitations. Although this is the first study to assess individual dynamics of serum calcification propensity in HD patients it doesn’t fulfil all criteria for studying change, since T50 was only assessed from sera collected at two not three different time points. In addition, the study design required exclusion of patients who did not survive the first 24 months FU period or who missed timely FU. Therefore, the study population was significantly enriched for survivors, which limits the generalizability of our results and explains the lack of predictive potential of T50 Baseline. Due to the relatively low number of cardiovascular deaths we were unable to fully adjust the Cox model for cardiovascular mortality. The study design and post hoc character of the study preclude conclusions regarding causality and therefore, the pathophysiologic mechanism linking declining T50 to excess mortality remains elusive. We could not consider dietary calcium or phosphorus intake since these parameters were not available in the dataset. Lastly, although these data provide a fascinating new perspective on intra-individual serum calcification resistance and the interpretation of the T50 test, larger scaled studies are needed to replicate and develop these results.
In conclusion, longitudinally monitoring changes in T50-time in HD patients might offer a suitable tool to identify patients at risk for adverse outcome and open the conceptual possibility of basing multimodal and personalized therapeutic interventions on longitudinal changes of T50 5. Larger scaled prospective interventional studies are needed to put this concept to a test.
Methods
Subjects/Study population
This study was undertaken in a subset of patients of the original “rISk strAtification in end stage Renal disease” - (ISAR)-cohort, a multicentre, prospective longitudinal observatory cohort study33. Between 2010 and 2013, 519 stable HD patients from 17 dialysis centres in Munich, Germany and the surrounding area were included. Out of these patients the present study included 188 patients, which were still alive and active in the study after the first FU period of 24 months with a maximum spread of ±3.2 months and for whom sera were available at both baseline and follow-up. Patients for whom timely 24 [23–25] months FU had been missed were excluded a priori (Fig. 1). Patients were ≥18 years of age, had an HD vintage of least 90 days and gave written and informed consent. The ISAR study was approved by the ethics committees of the Klinikum rechts der Isar, Technical University Munich and of the Bavarian State Board of Physicians33. It was carried out in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants. The study was registered under ClinicalTrials.gov identifier: NCT01152892 prior to its start. For the derived study, no additional ethics committee approval was sought. For more details, we refer to the study protocol33.
Clinical data assessment
Patients’ age, comorbidities and medication at FU were assessed using medical records from the contributing dialysis centres. Comorbidities were recorded following an adapted version of the Charlson Comorbidity Index (CCI) for ESRD as introduced by Liu et al.34. BMI at FU was calculated as body weight/height2 [kg/m2]. Access type (fistula or permanent catheter) was determined at time of FU and considered constant for the consecutive observation period. Information on dialysis prescription (Ultrafiltration, session duration, Kt/V as a measure of dialysis efficiency, HD/HDF, anticoagulation) was provided by the contributing centres. All patients underwent regular bicarbonate dialysis with synthetic membranes. For details, we refer to the study protocol33.
Endpoints
The primary outcome parameters for the ISAR-trial and this project were all-cause and CV mortality. Observation for all-cause and cause-specific mortality started the day after the 24 month FU visit. In the absence of a final medical report stating the cause of death, attending physicians and relatives were contacted to confirm death and gather available information, based on which the ISAR-study physician board assigned each case an underlying cause of death. CV mortality (n = 17) was due to sudden cardiac death (n = 6), myocardial infarction (n = 4), heart failure (n = 1), cardiac surgical procedure (n = 2), pulmonary embolism (n = 1), major stroke (n = 2) and rupture of aortic aneurysm (n = 1). Non-CV lethal events (n = 26) comprised infectious events, gastrointestinal bleeding, non-CV related surgery, withdrawal from treatment, chronic pulmonary disease, malignant diseases and unknown causes of death.
Blood specimen collection and Laboratory methods
Serum was collected prior to a midweek dialysis session at time of inclusion and at FU. Serum was centrifuged after 30 min of resting at room temperature, aliquoted and frozen at −20 °C, transferred to our laboratory on dry ice and stored at −80 °C for later analysis. Routine laboratory analysis was performed by ISO certified laboratories. IL-6 was determined using BD Flex-sets on a FACS Canto II and BD Diva software following the manufacturer’s instructions. BD FCAP Array software 3.0 was used for analysis. Ionized magnesium levels were determined from frozen sera using the Nova 8 Analyzer (Nova Biomedical, Waltham, MA, US). T50 was determined at previously described by Pasch et al.6,10. Sera had never been thawed prior to analysis and were sent to Bern on dry ice and analyzed in a blinded manner. Median storage duration was 48 [42–70] or 24 [18–47] months for samples collected at baseline or 24 months follow, respectively.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics 23 and R version 3.3.2 software. We present mean ± standard deviation (SD), median and [interquartile-range] or counts and (% of superset) for normally distributed data, non-normally distributed metric and ordinal variables or nominal data, respectively. IL-6 levels were natural logarithm-(ln)-transformed to adjust for skewness of distribution.
Paired t-test was used to compare differences between absolute T50-values at baseline and 24 months FU. Change in T50 (T50 Change) was calculated as (T50 Follow up−T50 Baseline)/T50 Baseline and expressed in percent. Subjects were stratified above and below the median of T50 Change and T50 Follow up, respectively for description of baseline characteristics at time of 24 months FU. Group differences were tested using unpaired t-test, Mann-Whitney-U, χ²-test and paired t-test as appropriate. Additionally, we assessed associations of continuous variables with T50 Change and T50 Follow up using Pearson correlation. Median T50 Follow up and median T50 Change were also used to stratify patients for univariate Kaplan-Meier survival analysis of all-cause and CV mortality. Cumulative incidence functions were estimated for CV and non-CV deaths to account for competing risks. Log-rank tests were performed to compare (cause specific) hazard rates between relevant groups. Patients were censored at time of transplantation or at time of loss to FU.
A multivariable linear regression model was built including age, sex, BMI, coronary heart disease (CHD), peripheral arterial occlusive disease (PAOD), diabetes, hypertension, intake of calcium containing phosphate binders, Vitamin D3 supplementation and laboratory parameter (calcium, magnesium, albumin, phosphate, intra-individual Δ-phosphate (=phosphateFollow up−phosphateBaseline [mmol/l]) and Δ-calcium, Δ-albumin to identify factors that were associated with T50 Change. Coefficients of regression are reported per 1 SD increase of the regressor. Variance of inflation factors were below 2 for all entered variables. Cox proportional hazard models were fit to the data to characterize the association of T50 Change with all-cause mortality. Proportionality of hazard rates was investigated by the use of Schoenfeld residuals and a statistical test for proportional hazard proposed by Grambsch and Therneau35.
The models were adjusted for demographic factors (age, gender, BMI), comorbidities (following the adapted CCI as proposed by Liu et al.34), albumin and ln-transformed IL-6. Hazard ratios (HR) and 95 % confidence interval (95% CI) are reported per 1SD of T50 Change (≈30.5 % change in T50) during the 24 months FU, 2 of 188 cases were censored before the earliest event had occurred. The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E. & Hsu, C.-y. Chronic Kidney Disease and the Risks of Death, Cardiovascular Events, and Hospitalization. N. Engl. J. Med. 351, 1296–1305, https://doi.org/10.1056/NEJMoa041031 (2004).
Foley, R. N., Parfrey, P. S. & Sarnak, M. J. Epidemiology of cardiovascular disease in chronic renal disease. J. Am. Soc. Nephrol. 9, S16–23 (1998).
Stokes, J. B. Consequences of Frequent Hemodialysis: Comparison to Conventional Hemodialysis and Transplantation. Trans. Am. Clin. Climatol. Assoc. 122, 124–136 (2011).
Mizobuchi, M., Towler, D. & Slatopolsky, E. Vascular calcification: the killer of patients with chronic kidney disease. J. Am. Soc. Nephrol. 20, 1453–1464, https://doi.org/10.1681/asn.2008070692 (2009).
Pasch, A. Novel assessments of systemic calcification propensity. Curr. Opin. Nephrol. Hypertens. 25, 278–284, https://doi.org/10.1097/mnh.0000000000000237 (2016).
Pasch, A. et al. Nanoparticle-based test measures overall propensity for calcification in serum. J. Am. Soc. Nephrol. 23, 1744–1752, https://doi.org/10.1681/asn.2012030240 (2012).
Smith, E. R. et al. Serum calcification propensity predicts all-cause mortality in predialysis CKD. J. Am. Soc. Nephrol. 25, 339–348, https://doi.org/10.1681/asn.2013060635 (2014).
Dahle, D. O. et al. Serum Calcification Propensity Is a Strong and Independent Determinant of Cardiac and All-Cause Mortality in Kidney Transplant Recipients. Am. J. Transplant. 16, 204–212, https://doi.org/10.1111/ajt.13443 (2016).
Keyzer, C. A. et al. Calcification Propensity and Survival among Renal Transplant Recipients. J. Am. Soc. Nephrol. 27, 239–248, https://doi.org/10.1681/asn.2014070670 (2016).
Pasch, A. et al. Blood Calcification Propensity, Cardiovascular Events, and Survival in Patients Receiving Hemodialysis in the EVOLVE Trial. Clin. J. Am. Soc. Nephrol. 12, 315–322, https://doi.org/10.2215/cjn.04720416 (2017).
Chertow, G. M. et al. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N. Engl. J. Med. 367, 2482–2494, https://doi.org/10.1056/NEJMoa1205624 (2012).
Shroff, R. C. et al. Dialysis accelerates medial vascular calcification in part by triggering smooth muscle cell apoptosis. Circulation 118, 1748–1757, https://doi.org/10.1161/circulationaha.108.783738 (2008).
Edward Pivin, M. B., Devuyst, O., Huynh-Do, U. & Bochud, M. Andreas Pasch Serum Calcification Propensity Is Largely Genetically Determined in the General Population [abstract]. ASN Kidney Week 2016 FR-PO423 (2016).
Yu, L., Li, H. & Wang, S. X. Serum Magnesium and Mortality in Maintenance Hemodialysis Patients. Blood Purif. 43, 31–36, https://doi.org/10.1159/000451052 (2017).
Hermans, M. M. et al. Association of serum fetuin-A levels with mortality in dialysis patients. Kidney Int. 72, 202–207, https://doi.org/10.1038/sj.ki.5002178 (2007).
Sakaguchi, Y., Hamano, T. & Isaka, Y. Effects of Magnesium on the Phosphate Toxicity in Chronic Kidney Disease: Time for Intervention Studies. Nutrients 9, 112, https://doi.org/10.3390/nu9020112 (2017).
Tentori, F. et al. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am. J. Kidney Dis. 52, 519–530, https://doi.org/10.1053/j.ajkd.2008.03.020 (2008).
Westenfeld, R. et al. Fetuin-A Protects against Atherosclerotic Calcification in CKD. Journal of the American Society of Nephrology: JASN 20, 1264–1274, https://doi.org/10.1681/ASN.2008060572 (2009).
Zhang, K. et al. Malnutrition, a new inducer for arterial calcification in hemodialysis patients? J. Transl. Med. 11, 66, https://doi.org/10.1186/1479-5876-11-66 (2013).
Posadas-Sanchez, R. et al. Serum magnesium is inversely associated with coronary artery calcification in the Genetics of Atherosclerotic Disease (GEA) study. Nutr. J. 15, 22, https://doi.org/10.1186/s12937-016-0143-3 (2016).
Melamed, M. L. et al. Changes in serum calcium, phosphate, and PTH and the risk of death in incident dialysis patients: a longitudinal study. Kidney Int. 70, 351–357, https://doi.org/10.1038/sj.ki.5001542 (2006).
Dautova, Y. et al. Fetuin-A and Albumin Alter Cytotoxic Effects of Calcium Phosphate Nanoparticles on Human Vascular Smooth Muscle Cells. PLoS One 9, e97565, https://doi.org/10.1371/journal.pone.0097565 (2014).
Ishimura, E. et al. Significant association between the presence of peripheral vascular calcification and lower serum magnesium in hemodialysis patients. Clin. Nephrol. 68, 222–227 (2007).
Meema, H. E., Oreopoulos, D. G. & Rapoport, A. Serum magnesium level and arterial calcification in end-stage renal disease. Kidney Int. 32, 388–394 (1987).
Isakova, T. et al. Phosphorus Binders and Survival on Hemodialysis. Journal of the American Society of Nephrology: JASN 20, 388–396, https://doi.org/10.1681/ASN.2008060609 (2009).
Sakaguchi, Y. et al. Association between Density of Coronary Artery Calcification and Serum Magnesium Levels among Patients with Chronic Kidney Disease. PLoS One 11, e0163673, https://doi.org/10.1371/journal.pone.0163673 (2016).
Jahromi, M. T., Yao, G. & Cerruti, M. The importance of amino acid interactions in the crystallization of hydroxyapatite. Journal of the Royal Society Interface 10, 20120906, https://doi.org/10.1098/rsif.2012.0906 (2013).
Stevens, L. A., Djurdjev, O., Cardew, S., Cameron, E. C. & Levin, A. Calcium, phosphate, and parathyroid hormone levels in combination and as a function of dialysis duration predict mortality: evidence for the complexity of the association between mineral metabolism and outcomes. J. Am. Soc. Nephrol. 15, 770–779 (2004).
Perkovic, V., Hunt, D., Griffin, S. V., du Plessis, M. & Becker, G. J. Accelerated progression of calcific aortic stenosis in dialysis patients. Nephron Clin. Pract. 94, c40–45, doi:71280 (2003).
Kamath, A. R. & Pai, R. G. Risk factors for progression of calcific aortic stenosis and potential therapeutic targets. The International Journal of Angiology: Official Publication of the International College of Angiology, Inc 17, 63–70 (2008).
Andreas Pasch, M. B., Edward, R. S., Benackova, K. & Uehlinger, D. E. Serum Calcification Propensity Is Improved by Increased Dialysate Bicarbonate and Dialysate Magnesium: The BicMag Pilot Study [abstract]. ASN Kindey Week 2016 FR-PO401 (2016).
Pasch Andreas, D. F. A. L. M., Adrian, C., Barbara, M., Arens Hans, J. & Passlick-Deetjen Jutta, J-D. W. Serum calcification propensity of HD patients is therapeutically improved by a calcium acetate/magnesium carbonate containing phosphate binder [abstract]. 51st Congress of the European-Renal-Association(ERA)/European-Dialysis-and-Transplant-Association (EDTA), May 31-Jun 03, 2014, Amsterdam, Netherlands (2014).
Schmaderer, C. et al. Rationale and study design of the prospective, longitudinal, observational cohort study "rISk strAtification in end-stage renal disease" (ISAR) study. BMC Nephrol. 17, 161, https://doi.org/10.1186/s12882-016-0374-8 (2016).
Liu, J., Huang, Z., Gilbertson, D. T., Foley, R. N. & Collins, A. J. An improved comorbidity index for outcome analyses among dialysis patients. Kidney Int. 77, 141–151, https://doi.org/10.1038/ki.2009.413 (2010).
Grambsch, P. M. & Therneau, T. M. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81, 515–526, https://doi.org/10.1093/biomet/81.3.515 (1994).
Acknowledgements
Special thanks are to be given to the 17 contributing dialysis centres and the hospitals in and around Munich for making this study possible. Isabelle Gsponer, Sandra Haderer and Alina Schmidt must be thanked for technical support.
Author information
Authors and Affiliations
Contributions
All listed authors have contributed sufficiently to the project to be included as authors. All contributors have been listed when they qualified as authors. G.L. and D.S. contributed equally. G.L. and C.S. were responsible for the study design. G.L., D.S., B.H., W.K.S., C.M. and S.W. were responsible for statistical analysis. G.L. drafted the manuscript which was reviewed and approved by all authors. C.S., U.H. and A.B. were responsible for the ISAR study and the database. G.L., D.S., S.K., S.A. and P.M. were responsible for data and serum sample collection and contributed significantly to this version of the manuscript. AP evaluated T50 in a blinded fashion contributed significantly to this version of the manuscript. G.L., Q.B., M.L. and D.P. performed additional lab-work. W.K.S. did data verification for the revision. All authors contributed to interpretation of findings and take responsibility for all aspects of the reliability and freedom of bias of the data presented.
Corresponding authors
Ethics declarations
Competing Interests
A.P. is an employee and stock holder of Calciscon. G.L., D.S. and C.S. receive Investigator-Initiated Research grant support from Baxter completely unrelated to this project. G.L. was supported by a research scholarship of the Else Kröner-Fresenius-Stiftung for physician scientists.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lorenz, G., Steubl, D., Kemmner, S. et al. Worsening calcification propensity precedes all-cause and cardiovascular mortality in haemodialyzed patients. Sci Rep 7, 13368 (2017). https://doi.org/10.1038/s41598-017-12859-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12859-6
This article is cited by
-
Assessment of a serum calcification propensity test for the prediction of all-cause mortality among hemodialysis patients
BMC Nephrology (2023)
-
Reversal Of Arterial Disease by modulating Magnesium and Phosphate (ROADMAP-study): rationale and design of a randomized controlled trial assessing the effects of magnesium citrate supplementation and phosphate-binding therapy on arterial stiffness in moderate chronic kidney disease
Trials (2022)
-
Signaling pathways involved in vascular smooth muscle cell calcification during hyperphosphatemia
Cellular and Molecular Life Sciences (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.