Abstract
Type 2 diabetes mellitus (T2DM) is a low-grade chronic inflammatory diseases, which have been implicated in the pathogenesis of cognitive decline. We aim to evaluate associations between inflammatory markers and the risk of mild cognitive impairment (MCI) in T2DM. This study of 140 diabetic patients involved 71 with MCI and 69 controls. Clinical parameters, neuropsychological tests, high sensitivity C reactive protein (hsCRP), interleukin-6 (IL-6), lipoprotein-associated Phospholipase A2 (Lp-PLA2) mass and activity were measured. The results showed significantly higher plasma hsCRP, IL-6, Lp-PLA2 mass and activity in MCI group compared to controls. In T2DM with MCI, the Montreal Cognitive Assessment (MoCA) score was positively correlated with education level and high-density lipoprotein cholesterol (HDL-c), but inversely correlated with age, glycosylated hemoglobin, intima-media thickness (IMT), hsCRP, IL-6, and Lp-PLA2 mass and activity. Correlation analysis showed that both plasma Lp-PLA2 mass and activity were positively correlated with total cholesterol, low-density lipoprotein cholesterol, and IMT but negatively associated with MoCA score. Multivariable logistic regression analysis indicated higher hsCRP, Lp-PLA2 mass, Lp-PLA2 activity, and lower HDL-c to be independent risk factors increasing the possibility of MCI in T2DM. In conclusion, plasma Lp-PLA2 and hsCRP were found to be associated with the risk of MCI among T2DM patients.
Similar content being viewed by others
Introduction
The rapid growth of type 2 diabetes mellitus (T2DM) in the past few decades has aroused world public concern1. T2DM is associated with several complications that threaten human health2 and several studies have suggested that T2DM is an independent risk factor for mild cognitive decline (MCI) and dementia3,4,5. However, the pathogenesis of diabetes-related cognitive dysfunction is complex and involves many factors6. As an important characteristic of T2DM, inflammation is a potential mechanism explaining the association between T2DM and cognitive decline7,8.
Lipoprotein-associated phospholipase A2 (Lp-PLA2) is a circulating enzyme produced by inflammatory cells9. This enzyme belongs to the phospholpase A2 superfamily and may be regarded as an inflammatory marker10. In plasma, Lp-PLA2 hydrolyzes oxidized low-density lipoprotein (LDL) to produce inflammatory molecules such as lysophosphatidylcholine and oxidized nonesterified fatty acids11. Moreover, Lp-PLA2 can hydrolyze platelet-activating factor in platelets, monocytes, and macrophages12. It has been shown that both Lp-PLA2 mass and activity are higher in T2DM than in individuals without diabetes13,14,15 and that a high Lp-PLA2 level is associated with poor control of diabetes16. Moreover, previous studies have indicated that high Lp-PLA2 activity is a risk factor for dementia, independent of cardiovascular disease and inflammatory factors17,18, and a meta-analysis of more than 79,000 subjects showed that higher Lp-PLA2 mass or activity increases the risk of stroke, coronary heart disease, and vascular mortality which are associated with the development of Alzheimer’s disease (AD) and dementia19. Considering these findings together, we hypothesized that Lp-PLA2 might be of vital importance in mediating the role of chronic inflammation in the susceptibility of diabetic patients to cognitive impairment.
Another two potential markers associated with cognitive dysfunction and diabetes are high-sensitivity C-reactive protein (hsCRP) and interleukin-6 (IL-6)20. A longitudinal two-year clinical research observed that individuals within the highest tertile of serum CRP or IL-6 had a 24% higher risk for cognitive decline than those in the lowest tertile21. HsCRP is an acute-phase protein synthesized in the liver and is a sensitive marker of systemic low-grade inflammation22. Studies have suggested that an elevated CRP level is associated with global cognitive impairment21 and high risk for dementia23,24. In the brain of dementia patients, CRP has been found to be upregulated and deposited around amyloid plaques and small-vessel damages25,26. IL-6 is a pro-inflammatory cytokine that participates in inflammatory reactions and immune response and influences the growth and differentiation of cells in the central nervous system. Various studies have indicated increased peripheral IL-6 levels to be associated with cognitive impairment27,28. Furthermore, studies have shown that IL-6 may directly inhibit human hippocampal neurogenesis29.
In the current study, we aimed to explore the plasma levels of inflammatory markers (Lp-PLA2 mass and activity, CRP, and IL-6) in T2DM with and without MCI, and determine potential predictors of MCI among patients with T2DM. Such findings will help to clarify the potential mechanism of inflammation in cognitive decline susceptibility in T2DM and support the development of anti-inflammatory treatments for use in T2DM-associated MCI.
Results
Demographic, clinical, and cognitive characteristics of the study participants
A total of 140 T2DM patients were enrolled in this study: 71 patients with MCI and 69 patients without MCI. The demographic, clinical, and cognitive characteristics of the included patients are presented in Table 1. The MCI and non-MCI groups were well matched in age and gender. There were no significant differences between the two groups in history of smoking, diabetes durations, education levels, glycosylated hemoglobin (HbA1c), fasting blood glucose (FBG), triglyceride (TG), and low-density lipoprotein cholesterol (LDL-c) (false discovery rate[FDR] > 0.05). Compared with the controls, the T2DM patients with MCI had higher total cholesterol (TC) levels, intima-media thickness (IMT), and the percentage of plaque formation, whereas the high-density lipoprotein cholesterol (HDL-c) level was lower in the diabetic patients with MCI (P < 0.05, FDR < 0.05). The neuropsychological test scores of the MCI group were significantly lower than those of the non-MCI group (P < 0.001, FDR < 0.001). Plasma hsCRP, IL-6, Lp-PLA2 mass and activity were significantly higher in the MCI group (P < 0.05, FDR < 0.05). There were no significant differences in drug use between the two groups (Table 2).
Correlations between MoCA scores and other clinical parameters
Table 3 shows the correlations between Montreal Cognitive Assessment (MoCA) scores and clinical indicators in the T2DM patients with MCI. The MoCA score was positively correlated with education level (r = 0.329, P = 0.005) and HDL-c (r = 0.320, P = 0.007) and inversely correlated with age (r = −0.290, P = 0.014), HbA1c (r = −0.276, P = 0.023), IMT (r = −0.396, P = 0.001), hsCRP (r = −0.327, P = 0.005), IL-6 (r = −0.282, P = 0.017), Lp-PLA2 mass (r = −0.612, P < 0.001), and Lp-PLA2 activity (r = −0.263, P = 0.027). No associations between MoCA score and diabetes duration, FBG, TG, TC, or LDL-c were observed.
Correlations between Lp-PLA2 mass, Lp-PLA2 activity and other parameters
Pearson correlation analysis for normally distributed variables and Spearman rank correlation analysis for nonnormally distributed variables were performed to investigate associations between plasma Lp-PLA2 mass, Lp-PLA2 activity and other variables (Table 4). The results suggested plasma Lp-PLA2 mass to be positively associated with TC (r = 0.187, P = 0.027) LDL-c (r = 0.215, P = 0.011), TG (r = 0.184, P = 0.030), and IMT (r = 0.353, P < 0.001) but negatively associated with MoCA score (r = −0.625, P < 0.001). No significant correlations were found between FBG, HbA1c, HDL-c, hsCRP, or IL-6 and Lp-PLA2 level. Lp-PLA2 activity was positively associated with TC (r = 0.182, P = 0.031), LDL-c (r = 0.187, P = 0.027), and IMT (r = 0.181, P = 0.032) but negatively correlated with MoCA score (r = −0.548, P < 0.001). There were no significant correlations of Lp-PLA2 activity with FBG, HbA1c, TG, HDL-c, hsCRP, or IL-6 (P > 0.05 for all).
Logistic regression analysis
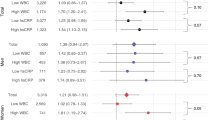
We first conducted univariate logistic regression analysis to select independent factors that increase the selection risk of MCI in T2DM and then used multivariable regression to investigate predictors associated with the presence of MCI. All variables in Table 1 were entered in the univariate logistic regression model at step one. The results showed that T2DM patients with higher TC, IMT, hsCRP, IL-6 levels, Lp-PLA2 mass, Lp-PLA2 activity, percentage of carotid plaque, lower HDL-c levels were more likely to have MCI (Table 5).
In forward stepwise multivariable regression analysis, MCI was used as the dependent variable, whereas TC, HDL-c, IMT, hsCRP, IL-6, Lp-PLA2 mass, Lp-PLA2 activity, and percentage of carotid plaque were entered as independent variables. The results showed that higher hsCRP (P = 0.002, FDR = 0.004), Lp-PLA2 mass (P = 0.016, FDR = 0.016), and Lp-PLA2 activity (P < 0.001, FDR < 0.001) and lower HDL-c (P = 0.012, FDR = 0.016) contributed to the development of MCI in T2DM (Table 6).
Discussion
The major finding of this study is that the investigated diabetic patients with MCI had higher plasma hsCRP, IL-6, Lp-PLA2 mass and Lp-PLA2 activity than those with healthy cognition. MoCA score was inversely correlated with age, HbA1c, IMT, hsCRP, IL-6, Lp-PLA2 mass, and Lp-PLA2 activity and positively correlated with education level and plasma HDL-c. The results also indicated that plasma Lp-PLA2 mass and activity were positively associated with TC, LDL-c, and IMT and negatively associated with MoCA score. In addition, multivariable logistic regression analysis further showed higher hsCRP, Lp-PLA2 mass, and Lp-PLA2 activity and lower HDL-c to be independent risk factors for MCI in T2DM.
Numerous studies have indicated the association of diabetes with increased risks for dementia, MCI, and cognitive decline30,31,32. Moreover, people with diabetes in their midlife have a threefold increased risk for developing dementia in 30 years33. MCI is characterized by memory deficiency without loss in daily activity functions34. Diabetes increases the risk for MCI by 40% in both amnestic and non-amnestic35. Furthermore, people on anti-diabetic medications have reduced cognitive impairment36,37. Neuroimaging and neuropathological studies have shown that the brain atrophy rate in T2DM is three times faster than that in normal aging individuals38,39. Although not fully understood, glucose metabolism, insulin signaling, impairment of amyloid clearance capacity, hypercholesterolemia, vascular defect, oxidative stress, and chronic inflammation may account for the association between T2DM and cognitive impairment40. In this study, we mainly investigate the general effect of inflammatory markers on cognitive impairment seen in the T2DM associated MCI patients.
The association of T2DM-associated MCI with the established inflammatory cytokines (Lp-PLA2, hsCRP, and IL-6) identified in this study proposes a novel assumption for its implication in inflammation-related pathogenesis. Results showed that all inflammatory biomarkers are significantly increased in the MCI group and are inversely associated with MoCA scores. Except for plasma IL-6, all cytokines remained significantly associated with MCI in T2DM after correction for multiple testing in multivariable logistic regression analysis. These results suggest a fundamental role of inflammation in the development of cognitive decline. Moreover, recent studies have implicated inflammatory markers in cognitive dysfunction. The Rotterdam Study17 suggested that individuals within the highest quartile of Lp-PLA2 activity exhibit a 70% higher risk for developing dementia than those in the lowest quartile17. The Honolulu-Asia Aging Study found that men in the upper three quartiles of hsCRP had a 3-fold increased risk for dementia irrespective of vascular risk factors23. Other studies have indicated that elevated hsCRP levels are associated with and poor memory41 and non-memory-related performance42. Additionally, IL-6 is also associated with the development of cognitive decline43,44. However, as found in other studies45,46,47, neither serum hsCRP nor IL-6 is correlated with serum Lp-PLA2 mass or activity levels in this study. This finding may be explained by the disparate inflammation pathways of the three inflammatory cytokines. Studies have suggested that Lp-PLA2 is involved in the process of inflammation arteriosclerosis46. Thus, Lp-PLA2 might be a highly specific marker for vascular inflammation. HsCRP is primarily activated by other cytokines in the liver and IL-6 is elevated under the circumstance of insulin resistance and visceral obesity46. Accordingly, hsCRP and IL-6 are mainly systemic inflammatory markers. Our study revealed that T2DM patients with MCI suffer from increased IMT and prevalence of plaque formation related to atherosclerosis. Inflammatory biomarkers Lp-PLA2, hsCRP, and IL-6 have been reported associated with atherosclerosis48,49,50, which is a risk factor for vascular disease. Epidemiologic and experimental studies have shown that both atherosclerosis and vascular disease are associated with cognitive impairments74,75. What’s more, it is suggested that treating vascular risk factors is important to prevent cognitive impairment51. Thus, it can be hypothesized that inflammatory biomarkers may collectively contribute to the vascular pathology and result in cognitive impairment.
Several studies have found potential links between inflammatory biomarkers and cognitive dysfunction, but the mechanisms remain unclear. In T2DM, Lp-PLA2 activates upstream inflammatory pathways and induces insulin resistance (IR)52,53. Consequently, IR leads to glucose, fat, and protein metabolism disorders related to chronic inflammation6. Furthermore, increased levels of inflammatory cytokines stimulate macrophages to express increased Lp-PLA29,54,55,56,57,58, resulting in a vicious cycle. Regarding the generative process of Lp-PLA2, the correlations of LP-PLA2 mass and LP-PLA2 activity with diabetes-associated MCI may be attributable to the accumulation of inflammatory cells during inflammatory processes. Increased Lp-PLA2 can hydrolyze oxidized phospholipids to form lysophosphatidylcholine and oxidized fatty acids (primary arachidonic acid [AA]), which are inflammatory molecules11. In neurons, overproduction of AA can trigger depolarization of neuronal cells through calcium-dependent apoptosis59. AA can also be transferred to prostaglandins, which are inflammation mediators that participate in the etiopathogenesis of neurodegenerative diseases60,61. Additionally, hydrolysis of Lp-PLA2 can promote expression of tumor necrosis factor (TNF-α), which is a key cytokine affecting hippocampal neuroplasticity62. Moreover, Lp-PLA2 is an important contributor to vascular deficit and diabetes itself is a vascular risk factor63. Thus, the elevated Lp-PLA2 level in T2DM may be linked to cognitive decline through the vascular pathology. The specific mechanism that links hsCRP, IL-6, and cognitive deficit is not fully understood. Through activation of the complement system, CRP might contribute to immune cascade reactions that result to neurodegeneration64. In addition, CRP may increase the expression of adhesion molecules in vascular endothelial cells, including endothelial cells in the brain65. In the central nervous system, IL-6 mediates immune response and inflammatory reactions and its overexpression is harmful for cell growth66.
The current study revealed that plasma Lp-PLA2 mass and activity are positively associated with LDL-c and TC levels. However, in multivariable logistic regression, LDL-c and TC were not risk factors of MCI in T2DM. These results suggested that the association between Lp-PLA2 and MCI was independent of lipid levels to some extent. In this study, we also identified an association of HDL-c with MCI in T2DM. HDL-c can remove excess cholesterol from subendothelian space of cerebral microvessels67. Moreover, low HDL-c level is known as a risk factor of atherosclerotic diseases68, leading to ischemic lesions in the brain and causing cognitive decline69. Notably, MoCA score was positively correlated with education level in this study. It has also been suggested that higher education could increase neocortical synaptic density and delay the progression of dementia70. These are in line with our finding showed that educational attainment is beneficial for cognitive function. On the basis of these findings, we encourage the elderly to exercise their brain, remain active, and participate in more intellectual activities to help delay cognitive impairment.
Several limitations should be noted in the interpretation of our results. First, the results of this case-control study may be misinterpreted because of the influence of farraginous factors, random and systematic recall errors, and selection bias. For instance, the population in this study had uncontrolled diabetes; consequently, the results cannot be generalized to patients with optimal glycemic control. Second, the small sample size and single ethnicity of the surveyed subjects may limit the application of our results to other ethnic groups. Finally, the conclusion of this study should be interpreted carefully as T2DM itself may increase the risk of MCI via different mechanisms. Consequently, the relationship between Lp-PLA2 and MCI in this study may have been confounded by T2DM.
In conclusion, our study indicates that increased levels of Lp-PLA2 mass, Lp-PLA2 activity, and hsCRP are associated with MCI in T2DM patients. These biomarkers are related to inflammation, thereby suggesting potential inflammatory reaction mechanisms underlying T2DM-associated MCI. These findings suggest the need for future investigation of the role of inflammatory cytokines in the etiology of cognitive impairment in T2DM. Thus, in view of the wide availability, safety, and convenience for monitoring plasma hsCRP and Lp-PLA2 mass and activity, both of these markers should be considered for early detection of MCI.
Methods
Ethics
The protocol and informed consent documents were approved by the Research Ethics Committee of the Affiliated Zhongda Hospital of Southeast University. All methods in this study were performed in accordance with approved guidelines and regulations. The study protocol was explained to the participants, and all patients provided written informed consent.
Study subjects
We performed a case-control study at the Endocrinology Division of the Affiliated Zhongda Hospital of Southeast University. We approached T2DM patients who satisfied the 1999 World Health Organization Criteria71 and were aged 40–80 years with a history of diabetes >3 years. We excluded subjects with the following: suffering from hypoglycemia within 3 days of neuropsychological tests and those with hypoglycemic coma, diabetic ketoacidosis, lactic acidosis or hyperosmolar nonketotic diabetic coma; cerebrovascular accidents confirmed by neuroimaging scans; a history of known neurological degenerative diseases, such as AD and Parkinson’s disease; a history of depression, severe visual or hearing loss; a history of drug or alcohol abuse within 2 months of the study; a history of taking anti-Parkinson drugs, benzodiazepines, barbiturates, short-acting anxiolytic or sedative drugs, drugs with significant anticholinergic or antimuscarinic adverse reactions, and antiepileptics within the previous 3 months; major medical illnesses (e.g., cancer, anemia, or serious infection); and thyroid disease. Participants were evaluated using 2006 European Alzheimer’s Disease Consortium criteria72 to assess cognitive status (normal cognition or MCI). Among the diabetic patients recruited, we identified 71 cases of MCI and 69 age-matched controls with healthy cognition.
Clinical parameter collection and carotid intima-media thickness determination
The following patient characteristics were collected: age, gender, level of education, medication history, smoking status, and diabetes duration. Physical characteristics were measured. FBG, HbA1c, TG, TC, LDL-c, and HDL-c levels were determined from blood samples. We used color Doppler ultrasound to measure IMT, which is the distance between the luminal-intimal interface and the medial-adventitial interface. Measurements were taken at the thickest site, at two further upstream sites, and at a site located 1 cm downstream of the left and right carotid arteries. Each site was measured six times, and the average value was calculated.
Neuropsychological tests
Neuropsychological tests, such as the MoCA, Trial Making Test-A, Trial Making Test-B, Clock Drawing Test, Verbal Fluency Test, Digit Span Test, and Word Similarity Test were conducted to evaluate cognitive function, including semantic memory, episodic memory, executive function, psychomotor speed, attention, and visuospatial skill. The Activities of Daily Living Scale, Clinical Dementia Rating Scale, Hamilton Depression Rating Scale, and Hachinski Ischemic Scale were also administered. The MoCA score was selected as the variable to evaluate the relationship between cognitive and clinical indicators based on the ability of this score to assess multiple cognitive domains. All neuropsychological tests were conducted by a skilled neuropsychiatrist from the Department of Neurology, Affiliated Zhongda Hospital of Southeast University.
Measurement of Lp-PLA2, hsCRP, and IL-6
Blood samples (2 mL) were collected into anticoagulant-free tubes and centrifuged at 1000 × g for 15 min. The plasma was then stored at −80 °C until analysis. Plasma Lp-PLA2 mass was measured using an enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, Minneapolis, MN, USA), and the Cayman colorimetric assay kit was used to measure plasma LP-PLA2 activity. hsCRP and IL-6 levels were determined by high sensitivity ELISA kits (R&D Systems, Minneapolis, MN, USA). To minimize assay variance, plasma Lp-PLA2 mass and Lp-PLA2 activity were measured on the same day for all individuals.
Statistical analyses
Data are presented as either the mean ± standard deviation (SD), median, or percentage. Normally distributed data were analyzed using Student’s t test and analysis of variance (ANOVA); asymmetrically distributed quantitative variables were analyzed by the nonparametric Mann-Whitney U and Kruskal-Wallis tests. The chi-squared test was used to compare qualitative variables. Relationships between MoCA scores and other parameters were analyzed by Pearson (normally distributed variables) or Spearman rank (non-normally distributed variables) correlation. Correlations between plasma Lp-PLA2 mass, Lp-PLA2 activity and other variables were also analyzed by Pearson or Spearman rank correlation. A simple logistic regression model was used to select so-called independent factors increasing the selection risk of MCI in T2DM. Forward stepwise multivariable regression analysis was then used to explore the “strongest” factors affecting the presence of MCI. We used the Benjamini- Hochberg (BH) method73 which control for false discovery rate (FDR) to adjust for multiple comparisons. A significant value of 0.05 was considered statistically significant.
References
Wild, S., Roglic, G., Green, A., Sicree, R. & King, H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27, 1047–1053 (2004).
Tremblay, J. & Hamet, P. Biomarkers of vascular complications in type 2 diabetes. Metabolism 64, S28–32, https://doi.org/10.1016/j.metabol.2014.10.032 (2015).
Janson, J. et al. Increased risk of type 2 diabetes in Alzheimer disease. Diabetes 53, 474–481 (2004).
Roberts, R. O. et al. Association of diabetes with amnestic and nonamnestic mild cognitive impairment. Alzheimers & Dementia 10, 18–26, https://doi.org/10.1016/j.jalz.2013.01.001 (2014).
Cukierman, T., Gerstein, H. C. & Williamson, J. D. Cognitive decline and dementia in diabetes–systematic overview of prospective observational studies. Diabetologia 48, 2460–2469, https://doi.org/10.1007/s00125-005-0023-4 (2005).
Ahmad, W. Overlapped metabolic and therapeutic links between Alzheimer and diabetes. Mol Neurobiol 47, 399–424, https://doi.org/10.1007/s12035-012-8352-z (2013).
Whitmer, R. A. Type 2 diabetes and risk of cognitive impairment and dementia. Curr Neurol Neurosci Rep 7, 373–380 (2007).
Schuitemaker, A. et al. Inflammatory markers in AD and MCI patients with different biomarker profiles. Neurobiol Aging 30, 1885–1889, https://doi.org/10.1016/j.neurobiolaging.2008.01.014 (2009).
Asano, K. et al. Cellular source(s) of platelet-activating-factor acetylhydrolase activity in plasma. Biochem Biophys Res Commun 261, 511–514, https://doi.org/10.1006/bbrc.1999.1066 (1999).
Rader, D. J. Inflammatory markers of coronary risk. N Engl J Med 343, 1179–1182, https://doi.org/10.1056/NEJM200010193431609 (2000).
MacPhee, C. H. et al. Lipoprotein-associated phospholipase A2, platelet-activating factor acetylhydrolase, generates two bioactive products during the oxidation of low-density lipoprotein: use of a novel inhibitor. Biochem J 338(Pt 2), 479–487 (1999).
Tselepis, A. D. & John Chapman, M. Inflammation, bioactive lipids and atherosclerosis: potential roles of a lipoprotein-associated phospholipase A2, platelet activating factor-acetylhydrolase. Atheroscler Suppl 3, 57–68 (2002).
Serban, M. et al. Significance of platelet-activating factor acetylhydrolase in patients with non-insulin-dependent (type 2) diabetes mellitus. J Cell Mol Med 6, 643–647 (2002).
Kudolo, G. B., Bressler, P. & DeFronzo, R. A. Plasma PAF acetylhydrolase in non-insulin dependent diabetes mellitus and obesity: effect of hyperinsulinemia and lovastatin treatment. J Lipid Mediat Cell Signal 17, 97–113 (1997).
Basu, A. et al. Lack of an effect of pioglitazone or glipizide on lipoprotein-associated phospholipase A2 in type 2 diabetes. Endocr Pract 13, 147–152, https://doi.org/10.4158/EP.13.2.147 (2007).
Cheraghi, A. et al. Comparison of Serum LP-PLA2 Level and some Nutritional Factors between Well-Controlled and Poorly-Controlled Diabetic Patients. Acta Med Iran 53, 690–696 (2015).
van Oijen, M. et al. Lipoprotein-associated phospholipase A2 is associated with risk of dementia. Ann Neurol 59, 139–144, https://doi.org/10.1002/ana.20721 (2006).
Fitzpatrick, A. L. et al. Lipoprotein-associated phospholipase A2 and risk of dementia in the Cardiovascular Health Study. Atherosclerosis 235, 384–391, https://doi.org/10.1016/j.atherosclerosis.2014.04.032 (2014).
Lp, P. L. A. S. C. et al. Lipoprotein-associated phospholipase A(2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet 375, 1536–1544, https://doi.org/10.1016/S0140-6736(10)60319-4 (2010).
Gorska-Ciebiada, M., Saryusz-Wolska, M., Borkowska, A., Ciebiada, M. & Loba, J. Serum levels of inflammatory markers in depressed elderly patients with diabetes and mild cognitive impairment. PLoS One 10, e0120433, https://doi.org/10.1371/journal.pone.0120433 (2015).
Yaffe, K. et al. Inflammatory markers and cognition in well-functioning African-American and white elders. Neurology 61, 76–80 (2003).
Pearson, T. A. et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107, 499–511 (2003).
Schmidt, R. et al. Early inflammation and dementia: a 25-year follow-up of the Honolulu-Asia Aging Study. Ann Neurol 52, 168–174, https://doi.org/10.1002/ana.10265 (2002).
Engelhart, M. J. et al. Inflammatory proteins in plasma and the risk of dementia: the rotterdam study. Arch Neurol 61, 668–672, https://doi.org/10.1001/archneur.61.5.668 (2004).
Lin, H. B. et al. Memory deficits and neurochemical changes induced by C-reactive protein in rats: implication in Alzheimer’s disease. Psychopharmacology (Berl) 204, 705–714, https://doi.org/10.1007/s00213-009-1499-2 (2009).
Marchesi, V. T. Alzheimer’s dementia begins as a disease of small blood vessels, damaged by oxidative-induced inflammation and dysregulated amyloid metabolism: implications for early detection and therapy. FASEB J 25, 5–13, https://doi.org/10.1096/fj.11-0102ufm (2011).
Fraga, V. G. et al. Genetic predisposition to higher production of interleukin-6 through −174 G > C polymorphism predicts global cognitive decline in oldest-old with cognitive impairment no dementia. Arq Neuropsiquiatr. https://doi.org/10.1590/0004-282X20150137 (2015).
Miwa, K., Okazaki, S., Sakaguchi, M., Mochizuki, H. & Kitagawa, K. Interleukin-6, interleukin-6 receptor gene variant, small-vessel disease and incident dementia. Eur J Neurol 23, 656–663, https://doi.org/10.1111/ene.12921 (2016).
Monje, M. L., Toda, H. & Palmer, T. D. Inflammatory blockade restores adult hippocampal neurogenesis. Science 302, 1760–1765, https://doi.org/10.1126/science.1088417 (2003).
Whitmer, R. A., Sidney, S., Selby, J., Johnston, S. C. & Yaffe, K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology 64, 277–281, https://doi.org/10.1212/01.WNL.0000149519.47454.F2 (2005).
Xu, W. L., Qiu, C. X., Wahlin, A., Winblad, B. & Fratiglioni, L. Diabetes mellitus and risk of dementia in the Kungsholmen project: a 6-year follow-up study. Neurology 63, 1181–1186 (2004).
Kravitz, E., Schmeidler, J. & Schnaider Beeri, M. Type 2 diabetes and cognitive compromise: potential roles of diabetes-related therapies. Endocrinol Metab Clin North Am 42, 489–501, https://doi.org/10.1016/j.ecl.2013.05.009 (2013).
Schnaider Beeri, M. et al. Diabetes mellitus in midlife and the risk of dementia three decades later. Neurology 63, 1902–1907 (2004).
Petersen, R. C. et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 56, 303–308 (1999).
Luchsinger, J. A. et al. Relation of diabetes to mild cognitive impairment. Arch Neurol 64, 570–575, https://doi.org/10.1001/archneur.64.4.570 (2007).
Wu, J. H. et al. Impact of antidiabetic medications on physical and cognitive functioning of older Mexican Americans with diabetes mellitus: a population-based cohort study. Ann Epidemiol 13, 369–376 (2003).
Umegaki, H. Therapeutic Potential of Antidiabetic Medications in the Treatment of Cognitive Dysfunction and Dementia. Drugs Aging 33, 399–409, https://doi.org/10.1007/s40266-016-0375-0 (2016).
Kooistra, M. et al. Diabetes mellitus and progression of vascular brain lesions and brain atrophy in patients with symptomatic atherosclerotic disease. The SMART-MR study. J Neurol Sci 332, 69–74, https://doi.org/10.1016/j.jns.2013.06.019 (2013).
van Elderen, S. G. et al. Progression of brain atrophy and cognitive decline in diabetes mellitus: a 3-year follow-up. Neurology 75, 997–1002, https://doi.org/10.1212/WNL.0b013e3181f25f06 (2010).
Strachan, M. W. R. D Lawrence Lecture 2010. The brain as a target organ in Type 2 diabetes: exploring the links with cognitive impairment and dementia. Diabet Med 28, 141–147, https://doi.org/10.1111/j.1464-5491.2010.03199.x (2011).
Teunissen, C. E. et al. Inflammation markers in relation to cognition in a healthy aging population. J Neuroimmunol 134, 142–150 (2003).
Noble, J. M. et al. Association of C-reactive protein with cognitive impairment. Arch Neurol 67, 87–92, https://doi.org/10.1001/archneurol.2009.308 (2010).
Licastro, F. et al. Increased plasma levels of interleukin-1, interleukin-6 and alpha-1-antichymotrypsin in patients with Alzheimer’s disease: peripheral inflammation or signals from the brain? J Neuroimmunol 103, 97–102 (2000).
Savas, S. et al. No relationship between lipoprotein-associated phospholipase A2, proinflammatory cytokines, and neopterin in Alzheimer’s disease. Exp Gerontol 77, 1–6, https://doi.org/10.1016/j.exger.2016.01.014 (2016).
Liu, C. F. et al. Elevated plasma lipoprotein-associated phospholipase A(2) activity is associated with plaque rupture in patients with coronary artery disease. Chin Med J (Engl) 124, 2469–2473 (2011).
Tektas, A. K. et al. Effects of lipoprotein-associated phospholipase A2 on arginase/nitric oxide pathway in hemodialysis patients. Ren Fail 34, 738–743, https://doi.org/10.3109/0886022X.2012.681535 (2012).
Atik, B., Johnston, S. C. & Dean, D. Association of carotid plaque Lp-PLA(2) with macrophages and Chlamydia pneumoniae infection among patients at risk for stroke. PLoS One 5, e11026, https://doi.org/10.1371/journal.pone.0011026 (2010).
Silva, I. T., Mello, A. P. & Damasceno, N. R. Antioxidant and inflammatory aspects of lipoprotein-associated phospholipase A(2) (Lp-PLA(2)): a review. Lipids Health Dis 10, 170, https://doi.org/10.1186/1476-511X-10-170 (2011).
Jialal, I. & Devaraj, S. Inflammation and atherosclerosis: the value of the high-sensitivity C-reactive protein assay as a risk marker. Am J Clin Pathol 116(Suppl), S108–115 (2001).
Park, S. Y. et al. Predictive value of circulating interleukin-6 and heart-type fatty acid binding protein for three months clinical outcome in acute cerebral infarction: multiple blood markers profiling study. Crit Care 17, R45, https://doi.org/10.1186/cc12564 (2013).
Snowdon, D. A. et al. Brain infarction and the clinical expression of Alzheimer disease. The Nun Study. JAMA 277, 813–817 (1997).
Iwase, M. et al. Lysophosphatidylcholine contents in plasma LDL in patients with type 2 diabetes mellitus: relation with lipoprotein-associated phospholipase A2 and effects of simvastatin treatment. Atherosclerosis 196, 931–936, https://doi.org/10.1016/j.atherosclerosis.2007.02.012 (2008).
Noto, H., Chitkara, P. & Raskin, P. The role of lipoprotein-associated phospholipase A(2) in the metabolic syndrome and diabetes. J Diabetes Complications 20, 343–348, https://doi.org/10.1016/j.jdiacomp.2006.07.004 (2006).
Davidson, J. E. et al. Plasma lipoprotein-associated phospholipase A2 activity in Alzheimer’s disease, amnestic mild cognitive impairment, and cognitively healthy elderly subjects: a cross-sectional study. Alzheimers Res Ther 4, 51, https://doi.org/10.1186/alzrt154 (2012).
Zalewski, A., Macphee, C. & Nelson, J. J. Lipoprotein-associated phospholipase A2: a potential therapeutic target for atherosclerosis. Curr Drug Targets Cardiovasc Haematol Disord 5, 527–532 (2005).
Stafforini, D. M. et al. Molecular basis of the interaction between plasma platelet-activating factor acetylhydrolase and low density lipoprotein. J Biol Chem 274, 7018–7024 (1999).
Hatoum, I. J., Hu, F. B., Nelson, J. J. & Rimm, E. B. Lipoprotein-associated phospholipase A2 activity and incident coronary heart disease among men and women with type 2 diabetes. Diabetes 59, 1239–1243, https://doi.org/10.2337/db09-0730 (2010).
Cao, Y., Stafforini, D. M., Zimmerman, G. A., McIntyre, T. M. & Prescott, S. M. Expression of plasma platelet-activating factor acetylhydrolase is transcriptionally regulated by mediators of inflammation. J Biol Chem 273, 4012–4020 (1998).
Penzo, D. et al. Arachidonic acid released by phospholipase A(2) activation triggers Ca(2+)-dependent apoptosis through the mitochondrial pathway. J Biol Chem 279, 25219–25225, https://doi.org/10.1074/jbc.M310381200 (2004).
Fattahi, M. J. & Mirshafiey, A. Positive and negative effects of prostaglandins in Alzheimer’s disease. Psychiatry Clin Neurosci 68, 50–60, https://doi.org/10.1111/pcn.12092 (2014).
Johansson, J. U. et al. Prostaglandin signaling suppresses beneficial microglial function in Alzheimer’s disease models. J Clin Invest 125, 350–364, https://doi.org/10.1172/JCI77487 (2015).
Stellwagen, D. & Malenka, R. C. Synaptic scaling mediated by glial TNF-alpha. Nature 440, 1054–1059, https://doi.org/10.1038/nature04671 (2006).
Dearborn, J. L. et al. Intracranial atherosclerosis and dementia: The Atherosclerosis Risk in Communities (ARIC) Study. Neurology 88, 1556–1563, https://doi.org/10.1212/WNL.0000000000003837 (2017).
Eagan, D. E. et al. Elevated serum C-reactive protein relates to increased cerebral myoinositol levels in middle-aged adults. Cardiovasc Psychiatry Neurol 2012, 120540, https://doi.org/10.1155/2012/120540 (2012).
Uchikado, H. et al. Activation of vascular endothelial cells and perivascular cells by systemic inflammation-an immunohistochemical study of postmortem human brain tissues. Acta Neuropathol 107, 341–351, https://doi.org/10.1007/s00401-003-0815-x (2004).
Hermida, A. P., McDonald, W. M., Steenland, K. & Levey, A. The association between late-life depression, mild cognitive impairment and dementia: is inflammation the missing link? Expert Rev Neurother 12, 1339–1350, https://doi.org/10.1586/ern.12.127 (2012).
Zuliani, G. et al. Lipoprotein profile in older patients with vascular dementia and Alzheimer’s disease. BMC Geriatr 1, 5 (2001).
Sharrett, A. R. et al. Associations of lipoprotein cholesterols, apolipoproteins A-I and B, and triglycerides with carotid atherosclerosis and coronary heart disease. The Atherosclerosis Risk in Communities (ARIC) Study. Arterioscler Thromb 14, 1098–1104 (1994).
Breteler, M. M., Claus, J. J., Grobbee, D. E. & Hofman, A. Cardiovascular disease and distribution of cognitive function in elderly people: the Rotterdam Study. BMJ 308, 1604–1608 (1994).
Katzman, R. Education and the prevalence of dementia and Alzheimer’s disease. Neurology 43, 13–20 (1993).
Alberti, K. G. & Zimmet, P. Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15, 539–553, https://doi.org/10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S (1998).
Portet, F. et al. Mild cognitive impairment (MCI) in medical practice: a critical review of the concept and new diagnostic procedure. Report of the MCI Working Group of the European Consortium on Alzheimer’s Disease. Journal of neurology, neurosurgery, and psychiatry 77, 714–718, https://doi.org/10.1136/jnnp.2005.085332 (2006).
Benjamini, Y. & Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society 57, 289–300 (1995).
Gorelick, P. B. et al. Vascular Contributions to Cognitive Impairment and Dementia: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 42(9), 2672–2713 (2011).
Jellinger, K. A. & Attems, J. Neuropathological evaluation of mixed dementia. Journal of the Neurological Sciences 257(1–2), 80–87 (2007).
Acknowledgements
We would like to express our heartfelt gratitude to the staff of the department of Endocrinology, Affiliated Zhongda Hospital of Southeast University, especially Prof. Hui Jin for her selfless help and valuable assistance. This work was partially supported by the National Natural Science Foundation of China (No. 81570732, Wang SH).
Author information
Authors and Affiliations
Contributions
S.W. contributed to the idea and revised the manuscript. R.C. carried out the design, conduct of the study and wrote the manuscript. R.H., J.H., H.S. carried out the data collection. J.S. and W.X. participated in the data analysis. S.T., X.D. and Y.S. helped data interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cai, R., Huang, R., Han, J. et al. Lipoprotein-associated Phospholipase A2 Is Associated with Risk of Mild Cognitive Impairment in Chinese Patients with Type 2 Diabetes. Sci Rep 7, 12311 (2017). https://doi.org/10.1038/s41598-017-12515-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12515-z
This article is cited by
-
Effect of probiotic supplementation on lipoprotein-associated phospholipase A2 in type 2 diabetic patients: a randomized double blind clinical controlled trial
Nutrition & Metabolism (2024)
-
Research Advance of Chinese Medicine in Treating Atherosclerosis: Focus on Lipoprotein-Associated Phospholipase A2
Chinese Journal of Integrative Medicine (2024)
-
Relationship between inflammatory markers and mild cognitive impairment in Chinese patients with type 2 diabetes: a case-control study
BMC Endocrine Disorders (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.