Abstract
The oral use of antimicrobial agents embedded in toothpastes and mouth rinses results in an oral microbial massacre with high amounts of dead bacteria in close proximity to few surviving bacteria. It was hypothesized that this provides the surviving pathogenic bacteria a large amount of dead microbial biomass as a nutritional source for growth (necrotrophy). This study demonstrated the necrotrophic growth of periodontal pathogens in the presence of different dead oral species. In addition, the presence of dead bacteria resulted in an outgrowth of several periodontal pathogens in complex multi-species biofilms. Additionally, upon contact with dead oral bacteria, virulence genes of P. intermedia and P. gingivalis were up-regulated (necrovirulence). This resulted in a more pronounced epithelial cytotoxicity (necrotoxicity). These findings indicate that presence of dead bacteria induce necrotrophy, necrovirulence and necrotoxicity in several oral pathogens.
Similar content being viewed by others
Introduction
Dental plaque is a complex poly-microbial biofilm in which more than 700 different microbial species can reside1. These microbial communities develop on all hard surfaces and soft tissues in the oral cavity and are embedded in extracellular polymeric matrix. The biofilm structure confers new properties to planktonic bacteria in terms of adhesion, communication, protection against the environment, the host’s immune response and antimicrobials2. Bacterial-host-environmental interactions determine the structure, composition and metabolic activity of these biofilms. All of these play an important role in the development of some of the most common diseases of mankind: periodontal diseases and caries. Periodontitis is an infectious disease resulting in a destruction of the tooth or implant supporting tissues. A relationship exists between periodontitis as a chronic infection and several systemic diseases3.
Prevention of caries and plaque-induced periodontal diseases consists of regular disruption and removal of accumulating oral biofilms, primarily from teeth4. Mechanical plaque removal by means of tooth and interdental brushing remains the foundation stone of prevention5. However, individuals are often unable to accomplish this due to, among others, motivational issues and technical difficulties5. Consequently, they leave partially disrupted oral biofilms on teeth and soft tissues for days, weeks, up to months.
Adjunctive chemical approaches to control oral biofilms are widespread under the form of toothpastes and mouth rinses, which often contain antiseptic ingredients such as chlorhexidine (CHX), cetylpyridinium chloride (CPC) or triclosan (TC)6. They are considered as adjuncts and normally do not substitute mechanical plaque control by means of brushing6. Moreover, they will not remove oral biofilms but are used to chemically kill oral bacteria. It is well known that bacteria have developed ingenious ways to survive killing by antimicrobials. Especially, the properties associated with a biofilm lifestyle protect them. There is ample of data showing that the antiseptics in toothpastes or mouth rinses only kill bacteria in the outer layer of the biofilm7. Although a 99.9% killing efficiency (2–3 Log reductions) can be reached 30 minutes after a single application of e.g. CHX or stannous fluoride, still 105 bacteria/mL will survive8. Consequently, the daily use of antimicrobial oral hygiene products containing antiseptics, results in a daily oral microbial massacre with high amounts of dead bacteria in close proximity to many surviving bacteria. Although these survivors can recover quickly from an antiseptic assault9, the fate of the bacterial casualties and their impact on survivors is currently unknown and has never been explored.
Recently it was shown that certain bacterial species can use dead microbial cells as a nutritional source for their own survival. Legionella pneumophila, for example, can use the remaining dead bacteria after heat treatment as a nutritional source to persist in water piping10, 11. This feature has been termed “bacterial necrotrophy”11. It is also known that starving Bacillus subtilis cells can produce toxins to kill sibling bacteria for nutrition12. The nutrients released by this behaviour from the killed siblings are being used to feed the surviving bacteria under conditions of nutritional stress13. By this, B. subtilis can prolong its survival and delay or avoid going into sporulation, which is a time and energy consuming process. This behaviour has been termed “cannibalism”14.
The widespread and daily use of antiseptic mouth rinses and toothpastes together with the inability for most people to accomplish a complete dental plaque removal makes that bacterial necrotrophy might be relevant for the oral ecosystem. Therefore, it is crucial to clarify if and how oral microbial ecosystems respond to sudden increases in dead bacteria.
The aim of this study was to determine if periodontopathogens can use dead bacteria as a nutritional substrate and to determine the impact of dead bacteria on bacterial virulence.
Results
Effect of dead bacteria on bacterial growth
In order to evaluate the necrotrophic behaviour of P. intermedia, a culture of P. intermedia was supplemented with dead P. intermedia. As shown in Table 1, after 24 hours, the total number of P. intermedia (CFU/mL) was significantly increased in the culture supplemented with dead P. intermedia when compared to a not-supplemented culture. This increase was dose dependent and resulted in a maximum supplemental outgrowth of P. intermedia of up to 1.46 (±0.01) Log10 CFU/mL in the presence of dead P. intermedia.
The necrotrophic behaviour of P. intermedia was however depending on the dead species. Supplementing a P. intermedia culture with either dead P. gingivalis, F. nucleatum, S. oralis or S. gordonii resulted in a significant increase of P. intermedia growth (Table 1). However, dead S. gordonii only increased the growth of P. intermedia in its highest concentration whereas dead P. gingivalis and dead F. nucleatum significantly increased the growth of P. intermedia in all used concentrations with up to 0.94 (±0.26) Log10 CFU/mL. Also for these dead species, a dose dependent effect was observed.
Necrotrophic behaviour was also observed for F. nucleatum and P. gingivalis in the presence of dead F. nucleatum and dead P. gingivalis respectively (Table 1). However, the magnitude of the growth increase induced by supplementing these species with dead bacteria was clearly lower than for P. intermedia. All concentrations (109, 108 and 107 CFU/mL) of dead P. gingivalis and dead F. nucleatum could increase the growth of P. gingivalis (Table 1).
Since the above described experiments were performed in a nutrient rich medium, it could be hypothesized that the effect of supplementing dead bacteria could be more pronounced in nutrient limited media. This was examined by supplementing P. intermedia with dead P. gingivalis in a nutrient limited medium BHI diluted 1/10 or 1/100 in PBS. After 24 hours of incubation, the concentration of P. intermedia in 1/10 BHI was reduced to 4.65 (±0.77) Log10 CFU/mL, indicating starvation of P. intermedia. However, if P. intermedia in 1/10 BHI was supplemented with dead P. gingivalis, the number of surviving bacteria was 6.42 (±0.13) Log10 CFU/mL (Table 1). The latter was significantly (p < 0.05) more than in the not supplemented condition and points towards a higher survival rate when dead P. gingivalis was present. When the culture media was further depleted from nutrients (1/100 BHI), no surviving bacteria could be detected for both conditions (data not shown).
The fate of dead bacteria
In order to further substantiate the necrotrophic behaviour, the DNA of dead bacteria was monitored over time by qPCR and correlated to the number of consumed cells.
As shown in Table 2, the qPCR data confirmed the dose dependent culturing data showing that when P. intermedia is supplemented with dead P. gingivalis or dead S. oralis, its growth over 24 hours is increased with up to 1.07 (±0.12) Log10 Geq/mL and with up to 0.32 (±0.17) Log10 Geq/mL respectively (p < 0.05). Additionally, the qPCR data showed that the DNA concentrations of dead P. gingivalis and S. oralis decreased significantly after 24 hours of incubation with living P. intermedia. No decrease was seen in control solutions containing only dead P. gingivalis and S. oralis without living P. intermedia. The DNA concentrations of dead P. gingivalis decreased for all concentrations of dead bacteria with up to 0.77 Log10 Geq/mL whereas the DNA concentrations of dead S. oralis, decreased for all concentrations of dead bacteria with up to 1.99 Log10 Geq/mL.
Necrotrophic growth in a multispecies community
Necrotrophic activity in the presence of other bacteria was tested to check for competitive effects. An increase in the concentrations of periodontal pathogens was observed inside of the 14 species planktonic community by the presence of dead P. intermedia and P. gingivalis in BHI-2, saliva or serum (Table 3, Supplementary Table 1, Supplementary Table 2 and Supplementary Table 3). The presence of dead P. intermedia increased the growth of living P. intermedia in BHI-2, saliva and serum (p < 0.05). F. nucleatum and A. actinomycetemcomitans increased also significantly by the addition of dead P. intermedia in BHI-2. Only the presence of dead P. intermedia increased the concentrations of P. gingivalis and F. nucleatum in saliva. Moreover the presence of dead P. gingivalis increased significantly the growth of P. intermedia, P. gingivalis and F. nucleatum in BHI-2, of P. gingivalis and F. nucleatum in saliva, and of P. intermedia, A. actinomycetemcomitans and P. gingivalis in serum.
In complex multi-species biofilms in BHI-2, the presence of dead P. intermedia resulted in an increased growth of P. gingivalis, P. intermedia, A. actinomycetemcomitans and F. nucleatum of up to 0.27 (±0.11), 0.82 (±0.16), 0.68 (±0.11) and 1.26 (±0.25) Log10 CFU/mL. Additionally, the presence of dead P. intermedia increased in serum only the growth of P. intermedia and F. nucleatum with up to 1.09 (±0.21) and 0.67 (±0.10) Log10 CFU/mL. In saliva the growth of P. intermedia, P. gingivalis and F. nucleatum was increased up to 0.32 (±0.03), 0.50 (±0.09) and 0.41(±0.07) Log10 CFU/mL.
Furthermore, the presence of dead P. gingivalis increased the growth of P. gingivalis, P. intermedia and F. nucleatum in complex multi-species biofilms up to 0.59 (±0.02), 0.56 (±0.09) and 0.97 (±0.23) Log10 CFU/mL in BHI, 0.47(±0.09), 0.79 (±0.08) and 1.36(±0.20) Log10 CFU/mL in serum and 0.16 (±0.08), 0.16 (±0.10) and 0.45 (±0.08) Log10 CFU/mL in saliva.
The effect of dead P. intermedia and dead P. gingivalis was also examined on the rest of bacterial species in the 14 species community (Table 3, Supplementary Table 1, Supplementary Table 2 and Supplementary Table 3). The presence of dead P. intermedia decreased the growth of S. sanguinis, S. mitis, S. gordonii, S. oralis, A. viscosus, A. naeslundii, S. mutans in BHI-2 and saliva (p < 0.05). Additionally, the presence of dead P. gingivalis decreased the concentrations of S. sanguinis, S. salivarius, S. gordonii, S. mitis, S. oralis, S. mutans and S. sobrinus in BHI-2 (p < 0.05) and of S. gordonii, S. oralis, A. viscosus, A. naeslundii, S. mitis in saliva (p < 0.05). A significant increase of V. parvula in BHI-2 was only reported by the presence of P. intermedia. Furthermore the presence of dead P. gingivalis in serum increased significantly the growth of S. sanguinis, A. naeslundii, A. viscosus, S. gordonii, S. oralis, V. parvula, S. mutans and S. sobrinus (p < 0.05).
Virulence gene expression
Gene expression of P. intermedia and P. gingivalis was analysed after supplementing the cultures with dead P. gingivalis and dead P. intermedia respectively. After 24 hours of growth, the P. intermedia virulence genes kpsD, phg, ecf, inpA and adpC were 1.96 to 4.21 fold up-regulated when compared to the control culture (Fig. 1A). P. intermedia heat shock protein genes htpG, dnaJ, dnaK, groeL, groeS, clpB, were also up-regulated with a factor of 4.72 to 11.62 (Fig. 1A). Similarly, supplementing a P. gingivalis culture with dead P. intermedia resulted in a significant 6.02 +/− 3.17 fold increase in prtC gene expression and a 2.94 +/− 1.46 fold increase in fimA expression (Fig. 1B).
Expression of virulence genes from P. intermedia and P. gingivalis in presence of dead oral bacteria. (A) Relative fold change of virulence genes from P. intermedia after exposure to dead P. gingivalis. (B) Relative fold change of virulence genes from P. gingivalis after exposure to dead P. intermedia. *Designates a statistically significant up-regulation of virulence genes respect to house-keeping genes (p < 0.05).
Additionally, the effect of supplementing a P. gingivalis culture with living P. intermedia was compared. Although there were no significant differences found in rgpA, rgpB, prtC and fimA gene expression between both cultures, the P. gingivalis culture supplemented with living P. intermedia showed a 7.29 +/− 4.55 fold higher serB and a 53.37 +/− 36.37 fold higher kgp expression when compared to the P. gingivalis culture supplemented with dead P. intermedia (Supplementary Table 4).
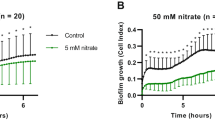
Cell viability assay
In order to verify whether dead bacteria can reduce cell viability on their own or by increasing P. gingivalis and P. intermedia virulence or by the combination of both, a cell viability assay was performed. As shown in Fig. 2, both living and dead P. gingivalis and P. intermedia decreased the epithelial cell viability. However, when the epithelial cells were challenged with a combination of living P. intermedia and dead P. gingivalis, the cell viability further decreased to 36.30% (±2.83) (p < 0.05) (Fig. 2A). Also when the epithelial cells were challenged with a combination of living P. gingivalis and dead P. intermedia, the percentage of cell viability further decreased significantly to 65.87% (±3.44) (Fig. 2B).
Percentages of cell viability after exposure to dead and living bacteria. (A) Percentages of cell viability in presence of living P. intermedia, dead P. gingivalis, living P. gingivalis and the combination living P. intermedia plus dead P. gingivalis. (B) Percentages of cell viability exposed to living P. gingivalis, dead P. intermedia, living P. intermedia and the combination living P. gingivalis plus dead P. intermedia. Control contains only cells without bacteria. *Designates a statistically significant decrease in cell viability respect to control (p < 0.05). #Designates a statistically significant decrease of cell viability respect to all conditions (p < 0.05).
Discussion
The data of this study shows that some oral pathogens can use dead bacteria as a supporting substrate in order to increase their growth in planktonic and biofilm conditions. Such a feature has been named necrotrophy11. Although this behaviour is often mentioned, it has never been shown for oral pathogens. Additionally, we show for the first time that in the presence of dead bacteria, oral pathogens increase their virulence, which we name “necrovirulence”. Both aspects can be of importance since the use of toothpastes and mouth rinses, containing bactericidal agents, is a common daily practice in society. It is very well known that these antimicrobials only kill the bacteria in the superficial layers of biofilms7. The fate of these bacterial casualties after an antiseptic attack is however not known although these layers of dead bacteria disappear within hours15. Therefore it can be hypothesized that these high and dense amounts of dead bacteria could provide multiple nutritional sources, such as C, N, P, Fe, for the surviving bacteria in the same ecosystem. Such behaviour has been shown for B. subtilis and L. pneumophila 11, 16, 17. Starving B. subtilis can produce toxins to kill siblings for nutrition (“cannibalism”) and prolong its survival14. L. pneumophila, on the other hand, can use heath killed dead bacteria as a nutritional source to persist in water piping11.
The necrotrophic behaviour of the tested oral pathogens showed a dose and species dependency. When exposed to different concentrations of dead bacteria, a clear dose dependent effect was observed on the growth of P. intermedia and P. gingivalis. Cultures of P. intermedia and P. gingivalis showed a significant increase in growth when there were at least 10 dead cells available to 1 living cell. The necrotrophic behaviour of these pathogens resulted in a supplemental growth of up to 1.46 Log10 CFU/mL This magnitude and the dose dependency are similar to what was reported for L. pneumophila supplemented with dead Pseudomonas putida 11. The species specificity of the necrotrophy was shown both for the living species as well as for the dead species. In homospecific necrotrophy experiments, the growth increase for P. intermedia was always stronger than for P. gingivalis. F. nucleatum only showed a weak growth increase. These data indicate that the necrotrophic activity specifically depends on the bacterial species. In heterospecific necrotrophy experiments, different dead bacterial species increased the growth of P. intermedia in different magnitudes, depending on the used dead bacterial species. These data indicate a clear dead species preference. A similar species preference has been shown for L. pneumophila. Whereas P. putida, Escherichia coli, Saccharomyces boulardii and Acanthamoeba castellanii increased the necrotrophic growth of L pneumophila, L. plantarum and B. subtilis did not11. Our data showed that the growth of the Gram negative P. intermedia was much less stimulated by the dead Gram positive S. oralis and S. gordonii than by more closely related Gram negative dead P. gingivalis or P. intermedia. This could be explained by the robust cell wall structure of these organisms, which prevents nutrients from becoming readily available, as suggested by Temmerman and coworkers11.
In order to verify that the dead bacteria were used as a nutritional source, DNA degradation of the dead bacteria was followed by qPCR as a proxy. This technique showed a decrease in dead bacteria over time concomitant to an increase in living bacteria. Such decrease in dead bacteria was not seen in control experiments without living bacteria. These data suggest that the living bacteria were actively breaking down the dead bacteria. However when the bacterial growth medium (BHI) was diluted, the addition of dead bacteria was insufficient to increase the growth of living bacteria, although their survival was improved. It has already been described that a concentration of 109 CFU/mL of dead bacteria is approximately 1 mg/mL of carbon biomass18. However, bacterial growth medium (BHI) contains about 30 mg/mL of carbon. In terms of nutritional values, the dead bacteria represent only a low proportion of 30:1 of carbon sources compared to the bacterial growth medium (BHI). Although the dead bacteria might provide other essential nutritional sources, their effect on growth cannot be explained only by nutritional aspects. It can be hypothesized that the presence of dead bacteria can also induce a change of the bacterial phenotype in terms of growth and behaviour.
Since a change in phenotype could be induced by the presence of dead bacteria, the virulence profiles of P. intermedia and P. gingivalis were investigated at the gene expression level. Although it is well known that associations of oral pathogenic bacteria can increase their virulence, for instance P. gingivalis can enhance the attachment and invasion of T. forsythia to epithelial cells19, the effect of dead bacteria on bacterial virulence gene expression has never been investigated. Several well-known virulence genes of P. gingivalis and P. intermedia were selected. The data showed that these genes become up-regulated in the presence of dead bacteria. This up-regulation can be explained by the presence of certain specific molecules (inducers) in the solutions of dead bacteria. The gingipain genes rgpA, rgpB, kgp of P. gingivalis were up-regulated in the presence of dead P. intermedia. They are involved in several bacterial functions which contribute to survival and virulence. The gingipain genes of P. gingivalis play an important role in the acquisition of nutrients by degrading peptides from the host or the environment20, 21. Their increased expression can therefore be directly related to the observed necrotrophic behavior of P. gingivalis. Additionally they are also involved in the adhesion, invasion and degradation of host tissues. These genes can also modulate the host immune response by inhibiting IL-2 accumulation in T-cells, by modulating T-cell communication and proliferation22. The long fimbriae gene fimA was also up-regulated. It encodes for the fimbriae structure, necessary for adhesion to and invasion of host tissues23, 24. The up-regulation of fimA can be due to the increase in rgp gingipains, which process the precursor proteins of long fimbriae25. An up-regulation of the collagenase prtC gene was also observed. prtC has a role in collagen and nutritional peptide degradation26, 27. In essence, the virulence genes of P. gingivalis which were upregulated by dead P. intermedia all related to the protein metabolism and to adhesion, invasion and destruction of host tissues. On the other hand, dead P. gingivalis upregulated in P. intermedia the virulence related genes kpsD, ecf, phg, inpA and adpC. The polysialic acid transport protein gene kpsD and the RNA polymerase ECF-type sigma factor ecf gene are involved in the production of a polysaccharide structure which can increase the resistance of P. intermedia against the host defense28. The expression of the hemagglutinin gene phg and the cysteine protease interpainA gene (inpA) were also increased. The pgh gene is involved in the hemolytic degradation of red blood cell to obtain hemoglobin and haem as an exogenous iron source for nutrition29. The inpA gene is also involved in the haem acquisition by breaking down hemoglobin30. It can be hypothesized that these genes are up-regulated in P. intermedia to acquire the iron compounds from inside of the dead P. gingivalis cells. Similar to the upregulated invasion genes in P. gingivalis, the invasin gene adpC, involved in the cell invasion of P. intermedia 31, was also up-regulated. A group of heat shock proteins (htpG, dnaJ, dnaK, groeL, groeS, clpB) were also up-regulated in the presence of dead P. gingivalis. These proteins quickly up-regulate their expression under stressful conditions and can protect the bacterial proteins against external aggression32. In essence, dead P. gingivalis activated genes in P. intermedia which related to nutrition, protection and invasion of host tissues.
In order to verify whether dead bacteria can reduce eukaryotic cell viability on their own or by increasing P. gingivalis and P. intermedia virulence or by the combination of both, a cell viability assay was performed. It is well known that living periodontal pathogens can invade and destroy host tissues33, 34. It also described that bacterial compounds like lipopolysaccharide (LPS), bacterial DNA and certain bacterial proteins can induce an inflammatory reaction35, 36. However, the influence of dead bacteria (necrotoxicity) alone or in combination with living bacteria on the host tissues has never been shown. Our results showed a lower cell viability for cells challenged with living pathogenic bacteria together with dead pathogenic bacteria when compared to living pathogenic bacteria or dead pathogenic bacteria alone. The increase in cell death can be explained by the increased expression of genes involved in the adhesion, invasion and destruction of host tissues like rgpA, rgpB, kgp, fimA and prtC in P. gingivalis and adpC in P. intermedia. However, since dead bacteria alone also reduced cell viability, a combined effect of increase of virulence factors together with toxic compounds of dead bacteria like LPS, bacterial proteins and free bacterial DNA should be considered.
In conclusion, the presence of dead bacteria can stimulate the growth of several oral pathogens (necrotrophy), inducing a new phenotype characterized by an up-regulation of bacterial virulence genes (necrovirulence) and an increased cytotoxicity towards host tissues (necrotoxicity). Such behaviour can also be expected from other human pathogenic species present in other microbiological ecologies such as the gut, the skin and the reproductive tract. These data should warn us for the indiscriminant use of broad-spectrum antimicrobials in conditions where there is an unspecific and incomplete eradication of the whole bacterial population. Therefore, the clinical impact of these results should be investigated.
Methods
Bacterial strains and media
Prevotella intermedia ATCC 25611, Porphyromonas gingivalis ATCC 33277, Fusobacterium nucleatum DSM 20482, Streptococcus gordonii ATCC 49818, Streptococcus oralis DSM 20627, Streptococcus sanguinis LM14657, Streptoccocus mitis DSM 12643, Streptococcus salivarius TOVE-R, Streptococcus mutans ATCC 20523, Streptococcus sobrinus ATCC 20742, Actinomyces viscosus DSM 43327, Actinomyces naeslundii ATCC 51655, Aggregatibacter actinomycetemcomitans ATCC 43718 and Veillonella parvula DSM 2008 were maintained on blood agar (Blood agar Base I, Oxoid, Basingstoke, UK) supplemented with hemin (5.0 mg/mL), menadione (1.0 mg/mL) and 5% sterile horse blood. Broth cultures were prepared in Brain Hearth Infusion (BHI) broth (Difco, Sparks, MD). Multi-species biofilm experiments were performed in Brain Hearth Infusion 2 (BHI-2) broth containing BHI supplemented with 2.5 g/L mucin (Sigma-Aldrich, St. Louis, USA), 1.0 g/L yeast extract (Oxoid, Basingstoke, UK), 0.1 g/L cysteine (Calbiochem, San Diego, USA), 2.0 g/L sodium bicarbonate and 0.25% (v/v) glutamic acid (Sigma-Aldrich, St Louis, USA).
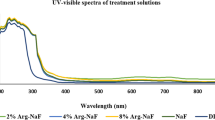
Preparation of dead bacteria
P. intermedia, P. gingivalis, F. nucleatum, S. gordonii and S. oralis were grown on blood agar for 48 hours. These agar plates were exposed to chloroform (Acros organics, Geel, Belgium) vapors for 30 minutes. After exposure, the cultures were removed from the agar plates by a sterile loop and suspended in 3 mL BHI, BHI-2, saliva or serum. This bacterial solution was transferred to an empty Petri dish and exposed to UV light (253 nm) for 30 minutes. The effectiveness of this killing procedure was verified by plating 50 µl of the killed bacterial solutions and control solutions containing living bacteria on a blood agar plate and incubating them for 10 days under aerobic and anaerobic conditions. Absence of bacterial growth confirmed the effectiveness of the killing procedure. Additionally, the killed bacterial solutions and control solutions were subjected to conventional and vitality RT-qPCR. The absence of amplification, when using vitality qPCR on the killed bacterial solutions, additionally confirmed the absence of living bacteria (data not shown). The bacterial concentration was determined by spectrophotometer (OD600, GeneQuant Spectrophotometer, Buckinghamshire, UK) and stock solutions were frozen at −80 °C upon use.
Necrotrophic growth experiments
3 mL of an overnight culture containing 5 × 107/mL P. intermedia was supplemented with 3 mL of dead bacteria at 109, 108, and 107 CFU/mL for 24 hours. A culture without dead bacteria (3 mL fresh BHI-2) was used as a control. After 24 hours of anaerobic growth, the cultures were analyzed by plate counting and qPCR.
For the plating experiments, 100 µL from the different conditions were taken and diluted from 10−1 until 10−6 in physiological water containing 9 g/L of sodium chloride. These dilutions were inoculated on blood agar plates and incubated for 48 hours under anaerobic conditions. Afterwards, P. intermedia colonies were counted to calculate the final number of bacteria CFU/mL in each condition. The same setup was used to test other bacterial combinations.
Quantification of bacteria in broth by qPCR
A conventional qPCR technique was used to quantify the total number of P. intermedia and DNA of dead P. intermedia, P. gingivalis, F. nucleatum and S. oralis. A vitality RT-qPCR was also employed to quantify only the living bacterial species in the planktonic and biofilm experiments using specific primers37, 38. Both were performed with a CFX96 Real-Time System (Bio-Rad, Temse, Belgium). The Taqman 5’ nuclease assay PCR method was used for detection and quantification of bacterial DNA (already developed for the species). Quantification was based on a plasmid standard curve.
Necrotrophic growth in multispecies communities
An overnight culture of a bioreactor derived complex multi-species co-culture of 14 species was centrifuged (1438 × g, 10 minutes) and re-suspended in BHI-2, serum or saliva (1 × 108 CFU/mL). 1 mL of this bacterial multi-species solution was inoculated together with 500 µl of 1 × 109 CFU/mL dead or living bacteria in BHI-2, saliva or serum. After 24 hours of anaerobic incubation, 1 mL was taken from each well and analysed via vitality qPCR or/and conventional qPCR. Afterwards, the remaining supernatant was removed and the biofilms at the bottom of the wells were washed with phosphate buffered saline (PBS). The biofilms were detached with 500 µL 0,05% Trypsin-EDTA (Gibco, Paisley, UK) for 15 minutes at 37 °C, transferred to Eppendorf tubes, centrifuged (6010 × g, 10 minutes) and after discarding the trypsin, the biofilm pellets were re-suspended in 1 mL of PBS and analysed by conventional and vitality qPCR.
Saliva and serum preparation
Unstimulated saliva was obtained for 1 hour per day from a single male volunteer during several days at least 1.5 hours after eating, drinking, or tooth-cleaning. Saliva samples, collected in sterile 50-mL polypropylene tubes, were centrifuged (30 min, 4 °C, 27,000 × g), and the supernatant was pasteurized (60 °C, 30 min) and re-centrifuged in sterile Eppendorf tubes. The resulting supernatants were dispensed into sterile 1.5 mL Eppendorf tubes and stored at −20 °C. The efficacy of pasteurization was tested by plating processed saliva samples onto blood agar (Blood agar Base I, Oxoid, Basingstoke, UK) supplemented with hemin (5 mg/mL), menadione (1 mg/mL) and 5% sterile horse blood. After 72 hours at 37 °C, no CFUs were observed on either aerobically or anaerobically incubated plates. Human serum was obtained by venepuncture of a single, systemically healthy, male volunteer with no oral disease and who had not taken any antibiotics for 1 year. Peripheral venous blood was immediately centrifuged at 264 × g for 30 min at room temperature. The serum was removed and frozen at −20 °C after aliquotation.
Ethics Statement
The use of human serum and saliva was approved by the ethical committee of the KU Leuven and registered with identifier B322201628215. The procedures were executed according to the Helsinki Declaration and the regulations of the University Hospital, which are approved by the ethical committee. The adult subject provided a written and oral consent after having explained to him the purpose of the study. The subject is aware that the results will be used in a scientific study.
Bioreactor derived multi-species community
A multi-species community was established in a BIOSTAT B TWIN (Sartorius, Germany) bioreactor. 750 mL of BHI-2 broth was added to the vessel together with 5.0 mg/mL hemin, 1.0 mg/mL menadione and 200 µl/L Antifoam Y-30 (Sigma, St. Louis, USA). The medium was pre-reduced over 24 hours at 37 °C by bubbling 100% N2 and 5% CO2 in the medium under continuous stirring at 300 rpm. pH was set at 6.7 +/−0.1. After 24 hours, overnight cultures of S. sanguinis, S. gordonii, S. salivarius, S. mitis, S. oralis, S. mutans, S. sobrinus, A. viscosus, A. naeslundii, P. intermedia, P. gingivalis, F. nucleatum, A. actinomycetemcomitans and V. parvula were adjusted to an OD of 1.4 and added to the bioreactor. During the first 48 hours, the medium was not replaced. After that, the medium was replaced at a rate of 200 mL/24 hours.
Virulence gene expression
RNA samples were extracted from the combinations living periodontal pathogen supplemented with 109 dead bacteria and from the periodontal pathogen without dead bacteria after 24 hours using RNeasy Mini Kit (Qiagen, Hilden, Germany). RNA quality was analyzed by nanodrop (Thermo Fisher Scientific, Doornveld, Belgium) and the samples were adjusted to the same concentration before transforming RNA to cDNA through PrimeScript 1st strand cDNA Synthesis Kit (Takara, Shiga, Japan). The expression of virulence genes in the periodontal pathogens was analyzed by qPCR in respect to the house-keeping genes. The primers were extracted from previous publications31, 37, 39, 40 or designed based on the genome of P. intermedia and P. gingivalis available in the National Center for Biotechnology Information (http://www.ncbi.nlm.nih.gov/) (Table 4).
Cell culture of human oral keratinocytes
Human oral keratinocyte cell line (HOK-18A)38 was grown in tissue culture flasks with keratinocyte growth medium (KSFM) supplemented as indicated by the manufacturer (Gibco, Life Technologies Ltd., Paisley, Scotland). Cell culture media were refreshed 3 times a week. After trypsinization, cells were maintained in culture bottles at 37 °C humidified atmosphere containing 5% CO2.
Cell viability assay
Cell viability was evaluated using the XTT cell proliferation assay. XTT powder (Sigma-Aldrich, Diegem, Belgium) was dissolved in RPMI 1640 medium (Life Technologies, Gent, Belgium) at a concentration of 1 mg/mL. Phenazine methyl sulphate (PMS) powder (AppliChem, Darmstadt, Germany) was also dissolved in PBS with a concentration of 0.383 mg/mL PMS. A mixture 50 µl XTT together with 1 µl PMS was added to each well. In brief, HOK-18A41 were seeded in 96-well plates (Grenier Bio-One, Frickenhausen, Germany) at a density of 2 × 104 cells per well. The cells were exposed to 5 × 107 CFU/mL of P. intermedia, 5 × 107 CFU/mL P. intermedia together with 108 CFU/mL of dead P. gingivalis, 108 CFU/mL dead of P. gingivalis and 108 CFU/mL living P. gingivalis for 20 h at 37 °C. The same combinations were used for P. gingivalis except for the concentrations of dead and living P. intermedia which were 107 CFU/mL because dead P. intermedia killed the cells in higher concentrations. After being exposed, 50 µl of XTT solution was added on the cells in each well for 4 hours. Afterwards, the formazan released by HOK-18A was measured at 450 nm using a micro-plate reader (Multiskan, Thermo Electron Corporation, Vanta, Finland). Cell viabilities are expressed as the percentages in respect to the control without treatment.
Statistical analysis
All experiments were repeated on 3 different days. A linear mixed model was fitted with run as random factor and growing condition as fixed factor. When residual analysis by means of a normal quantile plot showed that a Log-transformation was recommended, data were Log10-transformed. Comparisons between growing conditions and the control were corrected for simultaneous hypothesis testing according to Dunnett. Data were analysed with S-Plus 8.0 for Linux (Tibco, Palo Alto, CA, USA).
References
Dewhirst, F. E. et al. The human oral microbiome. J. Bacteriol. 192, 5002–5017 (2010).
Marsh, P. D., Moter, A. & Devine, D. A. Dental plaque biofilms: communities, conflict and control. Periodontol 2000 55, 16–35 (2011).
Cullinan, M. P. & Seymour, G. J. Periodontal disease and systemic illness: will the evidence ever be enough? Periodontol 2000 62, 271–286 (2013).
Tonetti, M. S., Chapple, I. L., Jepsen, S. & Sanz, M. Primary and secondary prevention of periodontal and peri-implant diseases: Introduction to, and objectives of the 11th European Workshop on Periodontology consensus conference. J Clin Periodontol 42, 1–4 (2015).
Tonetti, M. S. et al. Principles in prevention of periodontal diseases: Consensus report of group 1 of the 11th European Workshop on Periodontology on effective prevention of periodontal and peri-implant diseases. J Clin Periodontol 42, 5–11 (2015).
Serrano, J., Escribano, M., Roldan, S., Martin, C. & Herrera, D. Efficacy of adjunctive anti-plaque chemical agents in managing gingivitis: a systematic review and meta-analysis. J Clin Periodontol 42, 106–138 (2015).
Zaura-Arite, E., van Marle, J. & ten Cate, J. M. Confocal microscopy study of undisturbed and chlorhexidine-treated dental biofilm. J Dent Res 80, 1436–1440 (2001).
Oosterwaal, P. J., Mikx, F. H., van ‘t Hof, M. A. & Renggli, H. H. Short-term bactericidal activity of chlorhexidine gel, stannous fluoride gel and amine fluoride gel tested in periodontal pockets. J Clin Periodontol 18, 97–100 (1991).
Quintas, V., Prada-Lopez, I., Donos, N., Suarez-Quintanilla, D. & Tomas, I. In situ neutralisation of the antibacterial effect of 0.2% Chlorhexidine on salivary microbiota: Quantification of substantivity. Arch Oral Biol 60, 1109–1116 (2015).
Solimini, A. G., Cottarelli, A., Marinelli, L. & De Giusti, M. Factors influencing persistence of Legionella pneumophila serogroup 1 in laboratory cocultures. BMC Microbiol. 14, 249 (2014).
Temmerman, R., Vervaeren, H., Noseda, B., Boon, N. & Verstraete, W. Necrotrophic growth of Legionella pneumophila. Appl Environ Microbiol 72, 4323–4348 (2006).
Engelberg-Kulka, H. & Hazan, R. Cannibals defy starvation and avoid sporulation. Science. 301, 467–468 (2003).
Nandy, S. K., Bapat, P. M. & Venkatesh, K. V. Sporulating bacteria prefers predation to cannibalism in mixed cultures. FEBS Lett 581, 151–156 (2007).
Gonzalez-Pastor, J. E., Hobbs, E. C. & Losick, R. Cannibalism by sporulating bacteria. Science. 301, 510–513 (2003).
Netuschil, L., Reich, E., Unteregger, G., Sculean, A. & Brecx, M. A pilot study of confocal laser scanning microscopy for the assessment of undisturbed dental plaque vitality and topography. Arch Oral Biol 43, 277–285 (1998).
Gonzalez-Pastor, J. E. Cannibalism: a social behavior in sporulating Bacillus subtilis. FEMS Microbiol Rev 35, 415–424 (2011).
Lopez, D., Vlamakis, H., Losick, R. & Kolter, R. Cannibalism enhances biofilm development in Bacillus subtilis. Mol. Microbiol 74, 609–18 (2009).
Kim, D., Chung, S., Lee, S. & Choi, J. Relation of microbial biomass to counting units for Pseudomonas aeruginosa. Afr J Microbiol Res 6, 4620–4622 (2012).
Inagaki, S., Onishi, S., Kuramitsu, H. K. & Sharma, A. Porphyromonas gingivalis vesicles enhance attachment, and the leucine-rich repeat BspA protein is required for invasion of epithelial cells by “Tannerella forsythia”. Infect Immun. 74, 5023–5028 (2006).
Sheets, S. M., Robles-Price, A. G., McKenzie, R. M., Casiano, C. A. & Fletcher, H. M. Gingipain-dependent interactions with the host are important for survival of Porphyromonas gingivalis. Front. Biosci. 13, 3215–3238 (2008).
Grenier, D. et al. Role of gingipains in growth of Porphyromonas gingivalis in the presence of human serum albumin. Infect. Immun. 69, 5166–5172 (2001).
Khalaf, H. & Bengtsson, T. Altered T-cell responses by the periodontal pathogen Porphyromonas gingivalis. PLoS One. 7, e45192 (2012).
Lin, X., Wu, J. & Xie, H. Porphyromonas gingivalis minor fimbriae are required for cell-cell interactions. Infect. Immun 74, 6011–6015 (2006).
Kuboniwa, M. et al. P. gingivalis accelerates gingival epithelial cell progression through the cell cycle. Microbes Infect. 10, 122–128 (2008).
Furuta, N., Takeuchi, H. & Amano, A. Entry of Porphyromonas gingivalis outer membrane vesicles into epithelial cells causes cellular functional impairment. Infect. Immun. 77, 4761–4770 (2009).
Odell, L. J., Baumgartner, J. C., Xia, T. & David, L. L. Survey for collagenase gene prtC in Porphyromonas gingivalis and Porphyromonas endodontalis isolated from endodontic infections. J Endod 25, 555–558 (1999).
Kato, T., Takahashi, N. & Kuramitsu, H. K. Sequence analysis and characterization of the Porphyromonas gingivalis prtC gene, which expresses a novel collagenase activity. J Bacteriol. 174, 3889–3895 (1992).
Yamanaka, T. et al. Gene expression profile and pathogenicity of biofilm-forming Prevotella intermedia strain 17. BMC Microbiol 9, 11 (2009).
Okamoto, M., Maeda, N., Kondo, K. & Leung, K. P. Hemolytic and hemagglutinating activities of Prevotella intermedia and Prevotella nigrescens. FEMS Microbiol Lett 178, 299–304 (1999).
Byrne, D. P. et al. Role of the cysteine protease interpain A of Prevotella intermedia in breakdown and release of haem from haemoglobin. Biochem J. 425, 257–264 (2010).
Iyer, D. et al. AdpC is a Prevotella intermedia 17 leucine-rich repeat internalin-like protein. Infect. Immun. 78, 2385–2396 (2010).
Goulhen, F., Grenier, D. & Mayrand, D. Oral microbial heat-shock proteins and their potential contributions to infections. Crit Rev Oral Biol Med 14, 399–412 (2003).
Lamont, R. J. et al. Porphyromonas gingivalis invasion of gingival epithelial cells. Infect. Immun. 63, 3878–3885 (1995).
Dierickx, K. et al. Viability of cultured periodontal pocket epithelium cells and Porphyromonas gingivalis association. J. Clin. Periodontol. 29, 987–996 (2002).
Amoureux, M. C., Rajapakse, N., Stipkovits, L. & Szathmary, S. Peptidoglycan and bacterial DNA induce inflammation and coagulation markers in synergy. Mediators Inflamm. 2, 118–20 (2005).
Sliepen, I. et al. Microbial interactions influence inflammatory host cell responses. J Dent Res 88, 1026–30 (2009).
Loozen, G., Boon, N., Pauwels, M., Quirynen, M. & Teughels, W. Live/dead real-time polymerase chain reaction to assess new therapies against dental plaque-related pathologies. Mol. OralMicrobiol 26, 253–261 (2011).
Herrero, E. R. et al. Dysbiosis by neutralizing commensal mediated inhibition of pathobionts. Sci. Rep. 6, 38179 (2016).
Potempa, M. et al. Interpain A, a cysteine proteinase from Prevotella intermedia, inhibits complement by degrading complement factor C3. PLoS. Pathog. 5, e1000316 (2009).
Boutaga, K., van Winkelhoff, A. J., Vandenbroucke-Grauls, C. M. & Savelkoul, P. H. Comparison of real-time PCR and culture for detection of Porphyromonas gingivalis in subgingival plaque samples. J. Clin. Microbiol. 41, 4950–4954 (2003).
Huang, G. T., Haake, S. K., Kim, J. W. & Park, N. H. Differential expression of interleukin-8 and intercellular adhesion molecule-1 by human gingival epithelial cells in response to Actinobacillus actinomycetemcomitans or Porphyromonas gingivalis infection. Oral. Microbiol. Immunol. 13, 301–309 (1998).
Acknowledgements
This study was supported by grants of the KU Leuven (OT/12/101) and the Fund for Scientific Research Belgium (FWO G.0584.13).
Author information
Authors and Affiliations
Contributions
Conceptualization, E.R.H., K.B., N.B. and W.T.; Methodology, E.R.H., V.S. N.B. and W.T.; Analysis, E.R.H. and W.T.; Investigation, E.R.H. and M.P.; Writing—Original Draft, E.R.H.; Writing—Review & Editing N.B., K.B. and W.T.; Funding Acquisition, W.T. and M.Q.; Resources, W.T., M.Q. and N.B.; Supervision, W.T., N.B. and K.B.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rodriguez Herrero, E., Boon, N., Pauwels, M. et al. Necrotrophic growth of periodontopathogens is a novel virulence factor in oral biofilms. Sci Rep 7, 1107 (2017). https://doi.org/10.1038/s41598-017-01239-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-01239-9
This article is cited by
-
Development of antiseptic adaptation and cross-adapatation in selected oral pathogens in vitro
Scientific Reports (2019)
-
Drinking water bacterial communities exhibit specific and selective necrotrophic growth
npj Clean Water (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.