Abtract
Establishing a cure for HIV is hindered by the persistence of latently infected cells which constitute the viral reservoir. Real-time qPCR, used for quantification of this reservoir by measuring HIV DNA, requires external calibration; a common choice of calibrator is the 8E5 cell line, which is assumed to be stable and to contain one HIV provirus per cell. In contrast, digital PCR requires no external calibration and potentially provides ‘absolute’ quantification. We compared the performance of qPCR and dPCR in quantifying HIV DNA in 18 patient samples. HIV DNA was detected in 18 by qPCR and in 15 by dPCR, the difference being due to the smaller sample volume analysed by dPCR. There was good quantitative correlation (R2 = 0.86) between the techniques but on average dPCR values were only 60% of qPCR values. Surprisingly, investigation revealed that this discrepancy was due to loss of HIV DNA from the 8E5 cell calibrant. 8E5 extracts from two other sources were also shown to have significantly less than one HIV DNA copy per cell and progressive loss of HIV from 8E5 cells during culture was demonstrated. We therefore suggest that the copy number of HIV in 8E5 extracts be established by dPCR prior to use as calibrator.
Similar content being viewed by others
Introduction
HIV continues to be a major issue for global health, with approximately 36.7 million people living with HIV at the end of 2014 and about 2 million individuals becoming infected each year (WHO 2015). Despite the advent of effective combination antiretroviral therapy (cART), establishing a cure is hindered by the persistence of latently infected host cells, even in the absence of detectable plasma viraemia1, 2. These cells, usually CD4+ resting T cells, constitute the viral reservoir3 and have the potential to release progeny virions, therefore being responsible for viral rebound after discontinuation of therapy4, 5. With the advent of novel strategies for HIV cure that include latency reversing agents6, 7 accurate and robust methods are required for measurement and monitoring of the latent reservoir8.
A routine method for quantification of HIV RNA viral load, real-time quantitative PCR (qPCR), is also increasingly being used for measuring HIV DNA associated with the viral reservoir9. qPCR requires calibration and for this to be reproducible it is essential that the calibrator must be stable when shared between laboratories. A popular choice of calibrator for quantifying HIV DNA by qPCR is 8E5 (ATCC® CRL-8993)10,11,12,13,14,15,16,17, a lymphoblastic leukaemia cell line which has been reported by several studies to contain one integrated HIV genome per cell12, 18, 19.
Digital PCR (dPCR) is a more recently developed method that offers absolute quantification20. It has been used to value assign a variety of qPCR calibrators, including those for BCR-ABL21 and Mycobacterium tuberculosis22. dPCR has also been used in the direct quantification of HIV DNA from patients in a number of studies23,24,25,26,27 and unlike qPCR has the advantage of not requiring an external calibration standard. However, false positives and issues surrounding threshold determination have been reported to limit the usefulness of dPCR when employed for the most sensitive measurements of HIV DNA28. In this study we investigated the application of dPCR instruments in the context of HIV DNA measurement, both for comparison with qPCR analysis of patient samples and as a method for value assigning 8E5 calibration standards from three different sources.
Methods
Patient samples and 8E5 cell calibration standards
Anonymised peripheral blood mononuclear cell samples (PBMC) were obtained from HIV-positive individuals receiving antiretroviral therapy as part of a recently published clinical trial29 comparing Short Cycle Therapy (SCT) with continuous antiretroviral therapy. The study had received appropriate ethical committee approval.
Aliquots of DNA extracted from the 8E5 cell line19 were obtained from three separate institutions and designated Standard 1, Standard 2 and Standard 3. Standard 1 had been used for clinical research on HIV DNA levels; Standard 2 had been used in research as a source of HIV RNA; Standard 3 was a freshly obtained 8E5 cell culture from the American Type Culture Collection (ATCC® CRL-8993™) distributed by LGC, Teddington, UK. The passage numbers of the 8E5 cells from which Standard 1 and Standard 2 were obtained were unknown.
Culture of 8E5 cells (Standard 3)
Briefly, one vial of 8E5 cells (ATCC® CRL-8993™) was taken from liquid nitrogen and thawed at 37 °C for 1–2 minutes. 500 µL of cells was removed from the vial for culture and the remaining 300 µL (approximately 2.4 × 106 cells) retained for DNA extraction as passage 0 (P0). The full culture methodology is described in Supplementary Information. Following the single initial flask (designated passage 1), successive passages were maintained in triplicate (three separate flasks for passages 2, 3 and 4). During each passage cells were taken, pelleted and stored at −80 °C prior to DNA extraction.
DNA extraction
120 µL of each PBMC sample was lysed in 120 µL ATL buffer and the nucleic acid extracted on the QIAsymphony platform (Qiagen) using the DSP Virus/Pathogen Mini Kit (Qiagen) according to manufacturer’s protocols. Extracts were eluted in 60 µL and stored at −20 °C prior to analysis. DNA was extracted from the 8E5 Standard 3 cell pellets from each culture passage using the QIAamp DNA Blood Mini Kit (Qiagen). Supplemental to the manufacturer’s protocol, extracts were treated with 4 µL of RNase A (Qiagen) prior to the addition of lysis buffer. Final elution volume was 200 µL in buffer AE.
PCR assay design and primer sequences
Sequence information for the primers and probes used in the study is given in Table S1 of Supplementary Information. All PCR assays were performed in duplex format (i.e. two PCRs in the same reaction tube) consisting of one human reference gene assay (either pyruvate dehydrogenase, PDH or RNase P) and one assay specific for HIV-1. The HIV LTR-gag assay was designed to span a highly conserved region of the LTR-gag junction to allow amplification of a single Long Terminal Repeat.
qPCR analysis of clinical samples
qPCR analysis of 18 PBMC sample extracts was performed using an Applied Biosystems® 7500 Real-Time PCR System. Experiments were implemented in accordance with the MIQE guidelines30 (Table S2, Supplementary Information). To prepare a qPCR calibration curve consisting of ~50,000 to ~5 HIV DNA copies per reaction (assuming 1 HIV DNA copy per 8E5 cell), DNA extracted from the 8E5 cell line Standard 1, (DNA concentration initially established by Qubit fluorometric quantitation; ThermoFisher Scientific Inc.), was serially diluted using a tenfold dilution series in 5 µg/mL carrier RNA (Qiagen) dissolved in nuclease-free water. Twenty µL of each clinical sample extract (~1.2 µg DNA, equivalent to approximately 200,000 cells) was added to a total reaction volume of 50 µL. Full details of the PDH/HIV LTR-gag duplex qPCR assay protocol, cycling parameters and primer/probe sequences are given in Supplementary Information.
Digital PCR basic protocol
Duplex format dPCR experiments were implemented in accordance with the dMIQE guidelines (Supplementary Information)31. Two dPCR instruments were employed during the study; the RainDrop® Digital PCR System (RainDance Technologies) was used to measure the clinical samples and 8E5 extracts, and the QX200™ Droplet Digital™ PCR System (BioRad) was used to measure the 8E5 extracts only. Positive and negative partitions were selected for the RainDrop® and QX200™ manually using ellipse and quadrant gating, respectively, as recommended by the manufacturer using the instruments’ software. Full experimental protocols for both dPCR instruments and details of primers and probes used in the duplex assays are given in Supplementary Information. No template controls (NTCs) were included in all experiments.
Digital PCR analysis of clinical samples
5 µL (equivalent to approximately 50,000 cells) of the same 18 clinical sample extracts that had previously been analysed by qPCR were analysed using the RainDrop® dPCR platform as described above. The samples were amplified using the PDH/HIV LTR-gag duplex assay and NTCs of nuclease-free water were included as controls. The extracts were coded and the operator had no prior knowledge of the qPCR results on the same samples.
Digital PCR characterisation of 8E5 cells
The 8E5 DNA extracts from Standards 1, 2 and 3 were assessed using the RainDrop® platform with duplex primer sets to PDH/HIV LTR-gag, PDH/HIV pol and RNase P/HIV LTR-gag (Table S1). For the Standard 3 cells all four culture passage extracts and the initial passage zero (P0) extract were analysed using both RainDrop® and QX200™ instruments with the PDH/HIV LTR-gag duplex assay.
Effect of different 8E5 calibrator sources on qPCR analysis of clinical samples
Analysis of an additional seven HIV-positive clinical sample PBMC extracts was performed using qPCR as above. This experiment utilised the three different 8E5 cell Standards 1, 2 and 3 (passage 2) simultaneously as calibrators in the same run. HIV DNA copies were calculated per million cells using either the published quantity of 1 HIV DNA copy per 8E5 cell12, 18, 19 for all three different 8E5 sources or alternatively, the quantity determined empirically for the respective 8E5 extracts by dPCR during the present study.
Data Analysis
Data from dPCR and qPCR experiments were subject to threshold and baseline setting in the relevant instrument software, and were exported as .csv files to be analysed in Microsoft Excel 2010. For dPCR experiments the average number of copies per droplet (λ) was calculated as described previously32. dPCR and qPCR analyses of the clinical samples were compared by using a paired t-test on the log transformed HIV DNA copies per million cells. Agreement between methods was investigated using a Bland-Altman analysis and data evaluated for linearity using linear regression.
Results
Analysis of clinical samples by qPCR and dPCR
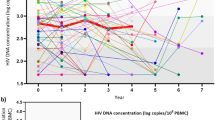
18 PBMC DNA samples from HIV-positive patients were analysed by dPCR and qPCR using the PDH/HIV LTR-gag duplex assays. HIV DNA was detected in all 18 samples by qPCR but in only 15 samples by dPCR. The three dPCR negative samples were near the lower limit of detection by qPCR (Supplementary Information, Table S3) and were probably undetected by dPCR due to the lower volume of template used (RainDrop® dPCR used ~5 µL whereas the qPCR used 20 µL, an approximately 4 fold greater volume of template). When the HIV DNA copies per million cells were calculated the dPCR and qPCR results correlated well (R2 = 0.86), however the dPCR results were on average only ~60% of the qPCR results, a statistically significant difference (p = 0.02) (Fig. 1a). Linear regression on the data generated from Bland-Altman analysis found no evidence of a trend in the observed bias which was independent of HIV DNA concentration (Figure S3). No false positive dPCR results were observed in the NTCs (Supplementary Information, Table S4).
Comparison between dPCR and qPCR results from 18 PBMC samples from HIV-positive patients, expressed as HIV DNA copies per million cells. The three samples in which HIV DNA was not detected by dPCR are not plotted. (a) qPCR quantities calculated assuming one HIV DNA copy per 8E5 cell. (b) qPCR quantities calculated assuming 0.6 HIV DNA copy per 8E5 cell as determined experimentally by dPCR NB. The dashed line represents equivalence.
Discrepancy between qPCR and dPCR due to loss of HIV DNA from 8E5 cells
In order to determine whether the ~60% discrepancy between dPCR and qPCR results might have been due to erroneous calibration of the qPCR, we investigated the calibrator (8E5 Standard 1) that had been used to calibrate the qPCR assay. Surprisingly, RainDrop® dPCR analysis of 8E5 Standard 1 with the PDH/HIV LTR-gag duplex assay revealed a ratio of PDH copies to HIV copies of approximately 3.2:1, whereas according to the literature12, 18, 19 the expected PDH:HIV ratio should have been exactly 2:1. This surprising finding was confirmed by repeating the dPCR analysis of 8E5 Standard 1 with a different dPCR instrument (QX200™) and with a different region of the HIV genome (pol) as PCR target. To exclude the possibility that the unexpected PDH:HIV ratio in 8E5 Standard 1 might have been caused by an increase in the PDH reference gene copy number we repeated the assays using a different human reference gene (RNase P) located on a different chromosome. In all cases the results confirmed that the PDH:HIV ratio in 8E5 Standard 1 was approximately 3.2:1 which is equivalent to approximately 0.6 HIV DNA copies per 8E5 cell. These findings are summarised in Fig. 2a. When the qPCR results on the 18 clinical samples were corrected to take into account the actual HIV DNA content of the 8E5 Standard 1 used as calibrator, the ~60% discrepancy between qPCR and dPCR findings became statistically insignificant (p = 0.41) (Fig. 1b).
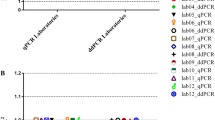
HIV DNA copies per cell calculated for different 8E5 sources. (a) Comparison of 8E5 Standards 1, 2 and 3 analysed by dPCR. (b) Effect of culture passage on HIV DNA content per cell for 8E5 Standard 3 measured using the RainDrop® dPCR platform (c) Effect of culture passage on HIV DNA content per cell for 8E5 Standard 3 measured using the QX200™ dPCR platform. Mean values with standard deviations are plotted.
To establish whether this loss of HIV DNA from the 8E5 calibrator was unique to the particular source of 8E5 that had been used, we obtained additional aliquots of 8E5 (designated Standard 2 and Standard 3 for the purposes of this study) from two independent institutions. 8E5 DNA extracts from Standard 2 and Standard 3 were analysed with both RainDrop® and QX200™ dPCR instruments by duplex assays using both regions of the HIV genome as target and both human reference genes. Remarkably, the magnitude of the loss of HIV DNA from 8E5 Standard 2 proved to be even greater (~0.02 HIV DNA copies per cell) than for Standard 1. In contrast, the loss of HIV DNA from 8E5 Standard 3 (~0.8 HIV DNA copies per cell) was less marked. The results of this dPCR characterisation of 8E5 Standards 2 and 3 are shown in Fig. 2a.
For the ATCC stock (8E5 Standard 3) five separate culture passages were analysed starting from baseline (P0) to passage 4. One DNA extract representing each culture flask per passage was analysed on RainDrop® and QX200™ dPCR platforms using the PDH/HIV LTR-gag duplex assay. The HIV DNA copies were observed to decrease relative to PDH copies with successive passages, equating to a fall in HIV DNA copy number from ~0.8 to ~0.6 copies per cell (Fig. 2b and c). Short Tandem Repeat (STR) analysis was performed by the supplier prior to culture, with the unique DNA profile being concordant with the cell line specification, suggesting proliferation of an additional non related clonal population was unlikely to be the source of this HIV DNA copy number change. No false positive results were observed for either instrument during these comparisons (Table S4).
Different sources of 8E5 calibrator may generate significant inaccuracies in HIV DNA quantification of clinical samples
To assess the effect of using different sources of 8E5 calibration material on the qPCR quantification of HIV DNA in clinical samples, three separate standard curves were constructed from 8E5 Standards 1, 2 and 3 in the same experimental run. Seven additional patient PBMC samples were tested in duplicate by qPCR using the PDH/HIV LTR-gag duplex assay and the means (expressed in HIV DNA copies per million cells) calculated for each sample (Fig. 3). When the previously reported one HIV DNA copy per 8E5 cell was assumed for all three Standards, the values calculated using 8E5 Standard 2 as calibrator were approximately 45 times higher than those calculated using the 8E5 Standards 1 and 3 which agreed with each other (Fig. 3a). When the dPCR derived values of HIV DNA copies per 8E5 cell were applied to the respective 8E5 Standard 1, 2 and 3 extracts the results with all three sources of 8E5 calibrator became concordant (Fig. 3b).
Median HIV DNA copies per million cells (boxplots with interquartile and range) of seven clinical samples assayed in duplicate by qPCR using 8E5 Standards 1, 2 and 3 for calibration. (a) Calculated assuming one HIV DNA copy per 8E5 cell for all three Standards. (b) Calculated using the actual number of HIV DNA copies per 8E5 cell as determined by dPCR for each of the three Standards.
Discussion
Detection of total cellular HIV DNA, comprising integrated proviral DNA and unintegrated forms such as LTR circles, offers a means of monitoring the latent viral reservoir in the absence of circulating HIV RNA5. However, it should be noted that HIV DNA assays are unable to differentiate between replication competent and incompetent HIV genomes and therefore do not actually measure the functional viral reservoir, which is most directly assessed by viral outgrowth assays24. Notwithstanding these reservations, HIV DNA assays have been widely used as an alternative to viral outgrowth assays because the latter are disadvantaged by being relatively expensive, labour intensive, technically demanding and requiring large amounts of blood. There is data supporting the use of HIV DNA assays and reports indicating a correlation between HIV DNA levels and clinically important parameters such as disease progression, post-treatment virological control and time to viral rebound on stopping cART5. qPCR is a widely used method for measuring total cellular HIV DNA9 as it is a versatile technique that is already well established for HIV RNA viral load measurement. It is comparatively inexpensive and readily scalable both in terms of reaction volume and throughput.
More recently, digital PCR has also been applied for HIV DNA measurement with some success but concerns have been raised regarding its sensitivity28. In this study we aimed to compare qPCR with dPCR for measuring total cellular HIV DNA in clinical samples and attempted to explain why discrepancies between the techniques may have occurred. We found that the results were broadly comparable, but that dPCR had reduced sensitivity related to the lower sample volume protocol employed. We did not observe the false positive dPCR results reported by others28 with either RainDrop® or QX200™ platforms (Table S4) and so did not have the challenge associated with setting thresholds to omit false positives. This demonstrates that dPCR could be effective as an alternative to qPCR for measurement of HIV DNA in patient samples if adequate sample volumes are used and strict contamination control measures maintained.
While dPCR may offer a powerful alternative ‘absolute’ method to qPCR for research use, the fact that the latter technique is so well established means it is likely to remain the method of choice for most clinical analyses of HIV DNA in the short term at least. However, this study has demonstrated that dPCR has an important role in improving qPCR accuracy and reproducibility by characterising and value assigning the calibration materials used for qPCR quantitation; we identified that qPCR overestimated the amount of HIV DNA per million cells due to unexpected instability of the 8E5 cell calibrator. The 8E5 cell line has been repeatedly reported and assumed to contain one HIV DNA proviral genome per cell12, 18, 19 but our findings suggest that this assumption is unsafe and that different batches of 8E5 may contain different amounts of HIV DNA per cell (varying in this study from ~0.02 to ~0.8 copies per cell).
To determine the HIV DNA copy number in the master stock and investigate the effect of culture on HIV DNA copies, a fresh culture was obtained from ATCC and serially passaged four times. This experiment demonstrated that HIV DNA copies were being lost in culture with serial passage (Fig. 2b and c). Coincidentally, during the preparation of the present manuscript, a study by Wilburn and colleagues was published, also raising concerns over the use of 8E5 for calibrating HIV DNA assays33. Wilburn’s study, based on fluorescent in situ hybridisation (FISH) and flow cytometry also concluded that, contrary to expectation, deletion of the HIV proviral genome could occur during culture of 8E5 cells and that different batches of 8E5 cells could contain dramatically varying numbers of cells lacking viral genomes. The mechanism of HIV DNA loss is unclear but it may be relevant that the provirus in 8E5 cells is inserted at 13q14-q21 which contains common fragile sites18 and could therefore render 8E5 susceptible to proviral loss through genomic instability.
Although qPCR is applied routinely in clinical virology, for the method to be reproducible it is widely recognised that reference materials are needed34 from which calibration standards can be derived. Reference materials do not currently exist for HIV DNA measurement, however the 8E5 cell line, with a reported single HIV DNA copy per cell, has been widely used as a calibrator over many years10,11,12,13,14,15,16,17. We demonstrate here that using the 8E5 cell line and assuming one HIV DNA copy per cell could lead to inaccuracies which could in turn result in misleading quantitative estimates of the HIV reservoir. Although 8E5 is commonly employed for calibration of HIV DNA qPCR assays, alternative calibrators such as the U1 cell line and HIV plasmids have been used in some studies23, 27. Bias of the type described here with 8E5 calibration has not to our knowledge been reported in studies that have utilised these alternatives, however the dPCR approach that we describe can also be used to determine the HIV content of different calibrators.
While we have identified this potential problem and demonstrated the significant bias that may ensue (Fig. 3a) we have also demonstrated how dPCR can be used to rectify any bias and harmonise the quantitative findings from 8E5 sources containing different quantities of HIV DNA (Fig. 3b). It would seem prudent to recommend that laboratories embarking on new quantitative studies into HIV DNA using qPCR obtain a fresh stock of 8E5 or other chosen calibrator and establish its actual HIV DNA content empirically using dPCR. Previous studies that may have used 8E5 with potentially varying HIV DNA quantities can apply the dPCR methods described here to determine the HIV DNA content of the batch used and, if necessary, recalculate their findings based on the new value assignment.
References
Churchill, M. J., Deeks, S. G., Margolis, D. M., Siliciano, R. F. & Swanstrom, R. HIV reservoirs: what, where and how to target them. Nature reviews. Microbiology 14, 55–60, doi:10.1038/nrmicro.2015.5 (2016).
Richman, D. et al. The Challenge of Finding a Cure for HIV Infection. Science 323, 1304–1307, doi:10.1126/science.1165706 (2009).
Siliciano, J. M. & Siliciano, R. F. The Remarkable Stability of the Latent Reservoir for HIV-1 in Resting Memory CD4+ T Cells. The Journal of infectious diseases 212, 1345–1347, doi:10.1093/infdis/jiv219 (2015).
Bruner, K. M. et al. Defective proviruses rapidly accumulate during acute HIV-1 infection. Nature medicine, doi:10.1038/nm.4156 (2016).
Williams, J. P. et al. HIV-1 DNA predicts disease progression and post-treatment virological control. eLife 3, e03821, doi:10.7554/eLife.03821 (2014).
Barton, K. M. et al. Selective HDAC inhibition for the disruption of latent HIV-1 infection. PloS one 9, e102684, doi:10.1371/journal.pone.0102684 (2014).
Margolis, D. M., Garcia, J. V., Hazuda, D. J. & Haynes, B. F. Latency reversal and viral clearance to cure HIV-1. Science 353, aaf6517, doi:10.1126/science.aaf6517 (2016).
Bruner, K. M., Hosmane, N. N. & Siliciano, R. F. Towards an HIV-1 cure: measuring the latent reservoir. Trends in microbiology 23, 192–203, doi:10.1016/j.tim.2015.01.013 (2015).
Sedlak, R. H. & Jerome, K. R. Viral diagnostics in the era of digital polymerase chain reaction. Diagnostic microbiology and infectious disease 75, 1–4, doi:10.1016/j.diagmicrobio.2012.10.009 (2013).
Avettand-Fenoel, V. et al. LTR real-time PCR for HIV-1 DNA quantitation in blood cells for early diagnosis in infants born to seropositive mothers treated in HAART area (ANRS CO 01). Journal of medical virology 81, 217–223, doi:10.1002/jmv.21390 (2009).
Beck, I. A. et al. Simple, sensitive, and specific detection of human immunodeficiency virus type 1 subtype B DNA in dried blood samples for diagnosis in infants in the field. Journal of clinical microbiology 39, 29–33, doi:10.1128/JCM.39.1.29-33.2001 (2001).
Desire, N. et al. Quantification of human immunodeficiency virus type 1 proviral load by a TaqMan real-time PCR assay. Journal of clinical microbiology 39, 1303–1310, doi:10.1128/JCM.39.4.1303-1310.2001 (2001).
Ghosh, M. K. et al. Quantitation of human immunodeficiency virus type 1 in breast milk. Journal of clinical microbiology 41, 2465–2470, doi:10.1128/JCM.41.6.2465-2470.2003 (2003).
Jaafoura, S. et al. Progressive contraction of the latent HIV reservoir around a core of less-differentiated CD4(+) memory T Cells. Nature communications 5, 5407, doi:10.1038/ncomms6407 (2014).
Kabamba-Mukadi, B. et al. Human immunodeficiency virus type 1 (HIV-1) proviral DNA load in purified CD4+ cells by LightCycler real-time PCR. BMC infectious diseases 5, 15, doi:10.1186/1471-2334-5-15 (2005).
McFall, S. M. et al. A simple and rapid DNA extraction method from whole blood for highly sensitive detection and quantitation of HIV-1 proviral DNA by real-time PCR. J Virol Methods 214, 37–42, doi:10.1016/j.jviromet.2015.01.005 (2015).
Shiramizu, B. et al. Circulating proviral HIV DNA and HIV-associated dementia. Aids 19, 45–52, doi:10.1097/00002030-200501030-00005 (2005).
Deichmann, M., Bentz, M. & Haasa, R. Ultra-sensitive FISH is a useful tool for studying chronic HIV-l infection. Journal of Virological Methods 65, 19–25, doi:10.1016/S0166-0934(96)02164-7 (1997).
Folks, T. et al. Biological and Biochemical Characterization of a Cloned Leu-3- Cell Surviving Infection with the Acquired Immune Deficiency Syndrome Retrovirus. The Journal of Experimental Medicine 164, 280–290, doi:10.1084/jem.164.1.280 (1986).
Day, E., Dear, P. H. & McCaughan, F. Digital PCR strategies in the development and analysis of molecular biomarkers for personalized medicine. Methods 59, 101–107, doi:10.1016/j.ymeth.2012.08.001 (2013).
Cross, N. C., White, H. E., Muller, M. C., Saglio, G. & Hochhaus, A. Standardized definitions of molecular response in chronic myeloid leukemia. Leukemia 26, 2172–2175, doi:10.1038/leu.2012.104 (2012).
Devonshire, A. S. et al. The use of digital PCR to improve the application of quantitative molecular diagnostic methods for tuberculosis. BMC infectious diseases 16, 366, doi:10.1186/s12879-016-1696-7 (2016).
Bosman, K. J. et al. Comparison of digital PCR platforms and semi-nested qPCR as a tool to determine the size of the HIV reservoir. Scientific reports 5, 13811, doi:10.1038/srep13811 (2015).
Eriksson, S. et al. Comparative analysis of measures of viral reservoirs in HIV-1 eradication studies. PLoS pathogens 9, e1003174, doi:10.1371/journal.ppat.1003174 (2013).
Henrich, T. J., Gallien, S., Li, J. Z., Pereyra, F. & Kuritzkes, D. R. Low-level detection and quantitation of cellular HIV-1 DNA and 2-LTR circles using droplet digital PCR. J Virol Methods 186, 68–72, doi:10.1016/j.jviromet.2012.08.019 (2012).
Jones, M. et al. Low copy target detection by Droplet Digital PCR through application of a novel open access bioinformatic pipeline, ‘definetherain’. J Virol Methods 202, 46–53, doi:10.1016/j.jviromet.2014.02.020 (2014).
Strain, M. C. et al. Highly precise measurement of HIV DNA by droplet digital PCR. PloS One 8, e55943, doi:10.1371/journal.pone.0055943 (2013).
Trypsteen, W., Kiselinova, M., Vandekerckhove, L. & De Spiegelaere, W. Diagnostic utility of droplet digital PCR for HIV reservoir quantification. Journal of Virus Eradication 2, 1–8 (2016).
BREATHER (PENTA 16) Trial Group. Weekends-off efavirenz-based antiretroviral therapy in HIV-infected children, adolescents, and young adults (BREATHER): a randomised, open-label, non-inferiority, phase 2/3 trial. The lancet. HIV 3, e421–430, doi:10.1016/S2352-3018(16)30054-6 (2016).
Bustin, S. A. et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clinical chemistry 55, 611–622, doi:10.1373/clinchem.2008.112797 (2009).
Huggett, J. F. et al. The digital MIQE guidelines: Minimum Information for Publication of Quantitative Digital PCR Experiments. Clinical chemistry 59, 892–902, doi:10.1373/clinchem.2013.206375 (2013).
Whale, A. S. et al. Detection of Rare Drug Resistance Mutations by Digital PCR in a Human Influenza A Virus Model System and Clinical Samples. Journal of clinical microbiology 54, 392–400, doi:10.1128/JCM.02611-15 (2016).
Wilburn, K. M. et al. Heterogeneous loss of HIV transcription and proviral DNA from 8E5/LAV lymphoblastic leukemia cells revealed by RNA FISH:FLOW analyses. Retrovirology 13, 55, doi:10.1186/s12977-016-0289-2 (2016).
Fryer, J. F. et al. Development of working reference materials for clinical virology. J Clin Virol 43, 367–371, doi: S1386-6532(08)00298-9 [pii] 10.1016/j.jcv.2008.08.011 (2008).
Acknowledgements
The work described in this paper was funded by the UK government Department for Business, Energy & Industrial Strategy (BEIS). RBF received funding from the NIHR Biomedical Research Centre and the UCLH/UCL BRC funded NIHR Health Informatics Collaborative Study. We also acknowledge the contributions of Karina Butler, Dianne Gibb, Deenan Pillay (PENTA BREATHER Clinical Trial), Sarah Watters (UCL), Simon Carne and David Bibby (Virus Reference Department, Public Health England, London, UK). Finally, we are grateful to Simon Cowen (LGC) for his assistance with the statistical analysis.
Author information
Authors and Affiliations
Contributions
J.A.G. and J.F.H. jointly designed the study and interpreted the data E.B., A.S.W., R.B.F. and G.M. performed laboratory assays and interpreted data. P.G. contributed to assay design and development, and E.N., J.J.C. and C.A.F. contributed to design of the study and sample procurement. E.B., J.F.H. and J.A.G. prepared the manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Busby, E., Whale, A.S., Ferns, R.B. et al. Instability of 8E5 calibration standard revealed by digital PCR risks inaccurate quantification of HIV DNA in clinical samples by qPCR. Sci Rep 7, 1209 (2017). https://doi.org/10.1038/s41598-017-01221-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-01221-5
This article is cited by
-
Accuracy of real-time PCR and digital PCR for the monitoring of total HIV DNA under prolonged antiretroviral therapy
Scientific Reports (2022)
-
Heterogeneity in HIV and cellular transcription profiles in cell line models of latent and productive infection: implications for HIV latency
Retrovirology (2019)
-
The role of integration and clonal expansion in HIV infection: live long and prosper
Retrovirology (2018)
-
Digital PCR as a tool to measure HIV persistence
Retrovirology (2018)
-
In-depth validation of total HIV-1 DNA assays for quantification of various HIV-1 subtypes
Scientific Reports (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.