Abstract
Aging populations are susceptible to heat-related mortality because of physiological factors and comorbidities. However, the understanding of individual vulnerabilities in the aging population is incomplete. In the Chinese Longitudinal Healthy Longevity Survey, we assessed daily heatwave exposure individually for 13,527 participants (median age = 89 years) and 3,249 summer mortalities during follow-up from 2008 to 2018. The mortality risk during heatwave days according to relative temperature is approximately doubled (hazard ratio (HR) range = 1.78–1.98). We found that heatwave mortality risks were increased for individuals with functional declines in mobility (HR range = 2.32–3.20), dependency in activities of daily living (HR range = 2.22–3.27), cognitive impairment (HR = 2.22) and social isolation reflected by having nobody to ask for help during difficulties (HR range = 2.14–10.21). Contrary to current understanding, older age was not predictive of heatwave mortality risk after accounting for individual functional declines; no statistical differences were detected according to sex. Beyond age as a risk factor, our findings emphasize that functional aging is an underlying factor in enhancing heatwave resilience. Assessment of functional decline and implementing care strategies are crucial for targeted prevention of mortality during heatwaves.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Researchers interested in using the CLHLS data are subject to data use agreement, available from the official repository located at https://doi.org/10.18170/DVN/WBO7LK. The environmental exposure datasets, including ERA5-Land (https://doi.org/10.24381/CDS.E2161BAC), MOD09GA v.061 (https://doi.org/10.5067/MODIS/MOD09GA.061) and ChinaHighPM2.5 (https://doi.org/10.5281/zenodo.6398971)44, are accessible.
Code availability
The code for the environmental assessment and cohort study analysis can be obtained from https://github.com/johnjiresearchlab/CLHLS_heatwave_vulnerability (ref. 46).
References
Ebi, K. L. et al. Hot weather and heat extremes: health risks. Lancet 398, 698–708 (2021).
Vicedo-Cabrera, A. M. et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat. Clim. Change 11, 492–500 (2021).
Bennett, J. E., Blangiardo, M., Fecht, D., Elliott, P. & Ezzati, M. Vulnerability to the mortality effects of warm temperature in the districts of England and Wales. Nat. Clim. Change 4, 269–273 (2014).
Ballester, J., Robine, J.-M., Herrmann, F. R. & Rodó, X. Long-term projections and acclimatization scenarios of temperature-related mortality in Europe. Nat. Commun. 2, 358 (2011).
Yin, Q., Wang, J., Ren, Z., Li, J. & Guo, Y. Mapping the increased minimum mortality temperatures in the context of global climate change. Nat. Commun. 10, 4640 (2019).
Yang, J. et al. Projecting heat-related excess mortality under climate change scenarios in China. Nat. Commun. 12, 1039 (2021).
Kephart, J. L. et al. City-level impact of extreme temperatures and mortality in Latin America. Nat. Med. 28, 1700–1705 (2022).
Ballester, J. et al. Heat-related mortality in Europe during the summer of 2022. Nat. Med. 29, 1857–1866 (2023).
Huang, C., Barnett, A. G., Wang, X. & Tong, S. The impact of temperature on years of life lost in Brisbane, Australia. Nat. Clim. Change 2, 265–270 (2012).
Zhao, Q. et al. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet. Health 5, e415–e425 (2021).
Ma, W., Chen, R. & Kan, H. Temperature-related mortality in 17 large Chinese cities: how heat and cold affect mortality in China. Environ. Res. 134, 127–133 (2014).
Ma, W. et al. The short-term effect of heat waves on mortality and its modifiers in China: an analysis from 66 communities. Environ. Int. 75, 103–109 (2015).
Yang, J. et al. Heatwave and mortality in 31 major Chinese cities: definition, vulnerability and implications. Sci. Total Environ. 649, 695–702 (2019).
Liu, J. et al. Mortality burden attributable to high and low ambient temperatures in China and its provinces: results from the Global Burden of Disease Study 2019. Lancet Reg. Health West. Pac. 24, 100493 (2022).
Balmain, B. N., Sabapathy, S., Louis, M. & Morris, N. R. Aging and thermoregulatory control: the clinical implications of exercising under heat stress in older individuals. BioMed Res. Int. 2018, 8306154 (2018).
Kenney, W. L. & Munce, T. A. Invited review: aging and human temperature regulation. J. Appl. Physiol. 95, 2598–2603 (2003).
Hajat, S., O’Connor, M. & Kosatsky, T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet 375, 856–863 (2010).
Naughton, M. P. Heat-related mortality during a 1999 heat wave in Chicago. Am. J. Prev. Med. 22, 221–227 (2002).
Semenza, J. C. et al. Heat-related deaths during the July 1995 heat wave in Chicago. N. Engl. J. Med. 335, 84–90 (1996).
Zhang, Y. et al. Risk factors for deaths during the 2009 heat wave in Adelaide, Australia: a matched case-control study. Int. J. Biometeorol. 61, 35–47 (2017).
World Population Ageing 2020 Highlights: Living Arrangements of Older Persons (United Nations, 2020); https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/undesa_pd-2020_world_population_ageing_highlights.pdf
Zhang, S. et al. The 2023 China report of the Lancet Countdown on health and climate change: taking stock for a thriving future. Lancet Public Health 8, e978–e995 (2023).
Belmin, J. et al. Level of dependency: a simple marker associated with mortality during the 2003 heatwave among French dependent elderly people living in the community or in institutions. Age Ageing 36, 298–303 (2007).
Vandentorren, S. et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur. J. Public Health 16, 583–591 (2006).
Kim, Y.-O., Lee, W., Kim, H. & Cho, Y. Social isolation and vulnerability to heatwave-related mortality in the urban elderly population: a time-series multi-community study in Korea. Environ. Int. 142, 105868 (2020).
Gasparrini, A. et al. Small-area assessment of temperature-related mortality risks in England and Wales: a case time series analysis. Lancet Planet. Health 6, e557–e564 (2022).
Xu, Z., FitzGerald, G., Guo, Y., Jalaludin, B. & Tong, S. Impact of heatwave on mortality under different heatwave definitions: a systematic review and meta-analysis. Environ. Int. 89–90, 193–203 (2016).
Dai, L. et al. Cognitive function and short-term exposure to residential air temperature: a repeated measures study based on spatiotemporal estimates of temperature. Environ. Res. 150, 446–451 (2016).
Franco-Marina, F. et al. The Mini-mental State Examination revisited: ceiling and floor effects after score adjustment for educational level in an aging Mexican population. Int. Psychogeriatr. 22, 72–81 (2010).
Racinais, S., Gaoua, N. & Grantham, J. Hyperthermia impairs short-term memory and peripheral motor drive transmission: passive hyperthermia alters neuromuscular and cognitive functions. J. Physiol. 586, 4751–4762 (2008).
Heatwaves and Health: Guidance on Warning-System Development (World Meteorological Organization & World Health Organization, 2015); https://library.wmo.int/viewer/54600/download?file=wmo_1142_en.pdf&type=pdf&navigator=1
Center For Healthy Aging And Development Studies. The Chinese Longitudinal Healthy Longevity Survey (CLHLS)—Longitudinal Data (1998–2018) (Peking University Open Research Data Platform, 2020); https://doi.org/10.18170/DVN/WBO7LK
Zeng, Y. Toward deeper research and better policy for healthy aging—using the unique data of Chinese longitudinal healthy longevity survey. China Economic J. 5, 131–149 (2012).
Zeng, Y., Feng, Q., Hesketh, T., Christensen, K. & Vaupel, J. W. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet 389, 1619–1629 (2017).
Copernicus Climate Change Service. ERA5-Land Hourly Data from 2001 to Present (ECMWF, 2019); https://doi.org/10.24381/CDS.E2161BAC
Lawrence, M. G. The relationship between relative humidity and the dewpoint temperature in moist air: a simple conversion and applications. Bull. Am. Meteorol. Soc. 86, 225–234 (2005).
Rothfusz, L. P. The Heat Index Equation (or, More Than You Ever Wanted to Know About Heat Index). Technical Attachment SR/SSD 90-23 (National Weather Service, 1990); https://www.weather.gov/media/ffc/ta_htindx.PDF
Ćwirlej-Sozańska, A., Wiśniowska-Szurlej, A., Wilmowska-Pietruszyńska, A. & Sozański, B. Determinants of ADL and IADL disability in older adults in southeastern Poland. BMC Geriatr. 19, 297 (2019).
Wang, J. et al. Fine particulate matter and poor cognitive function among Chinese older adults: evidence from a community-based, 12-year prospective cohort study. Environ. Health Perspect. 128, 067013 (2020).
Zhu, A. et al. Interaction between plant-based dietary pattern and air pollution on cognitive function: a prospective cohort analysis of Chinese older adults. Lancet Reg. Health West. Pac. 20, 100372 (2022).
Tombaugh, T. N. & McIntyre, N. J. The Mini-Mental State Examination: a comprehensive review. J. Am. Geriatr. Soc. 40, 922–935 (1992).
Lin, N. & Dumin, M. Access to occupations through social ties. Soc. Netw. 8, 365–385 (1986).
Vermote, E. & Wolfe, R. MODIS/Terra Surface Reflectance Daily L2G Global 1 km and 500 m SIN Grid v061 (NASA EOSDIS Land Processes Distributed Active Archive Center, 2021); https://doi.org/10.5067/MODIS/MOD09GA.061
Wei, J. & Li, Z. ChinaHighPM2.5: big data seamless 1 km ground-level PM2.5 dataset for China. Zenodo https://doi.org/10.5281/zenodo.6398971 (2019).
Mukadam, N., Sommerlad, A., Huntley, J. & Livingston, G. Population attributable fractions for risk factors for dementia in low-income and middle-income countries: an analysis using cross-sectional survey data. Lancet Glob. Health 7, e596–e603 (2019).
johnjiresearchlab/CLHLS_heatwave_vulnerability. GitHub https://github.com/johnjiresearchlab/CLHLS_heatwave_vulnerability (2024).
Acknowledgements
The CLHLS data collection was jointly supported by the National Key R&D Program of China (no. 2018YFC2000400), the National Natural Sciences Foundation of China (no. 72061137004) and the U.S. National Institute of Aging and National Institutes of Health (no. P01AG031719) to Y.Z. We thank all scholars, survey supervisors, staff members, local medical personnel and interviewers who contributed to the longitudinal follow-up of the survey. We thank the interviewees and their families for their voluntary participation in this study. J.S.J. was supported by the National Natural Science Foundation of China (no. 82250610230), Natural Science Foundation of Beijing (no. IS23105) and Tsinghua University Vanke School of Public Health Research Fund (no. 2021PY001).
Author information
Authors and Affiliations
Contributions
J.S.J. conceived the research hypothesis that focused on the heatwave vulnerability analysis; he designed the study, secured the necessary resources, applied the statistical models, interpreted the results and took the lead role in writing and revising the manuscript. D.X. was responsible for all data management, data cleaning and analysis. She set up the computing resources, leveraged the appropriate software for the analyses, oversaw the statistical evaluations and carried out the exposure assessments using remote sensing satellite techniques. In addition, she was the lead author and drafted and revised the manuscript, and also oversaw all aspects of the research. L.L. was responsible for ensuring data integrity, conducted rigorous cross-checking on data use and evaluated the exposure–outcome relationships. K.G.B., K.E. and C.H. interpreted the results, provided insights on climate change risk and outcome relationships, and actively participated in revising the manuscript. M.Z. provided specialized statistical input on the Cox proportional hazards model and semiparametric modeling, interpreted the results, met the statistical assumptions and ensured the robustness of the model specification. Y.Z. oversaw the creation of the CLHLS, ensuring the follow-up and comprehensive data collection pertaining to health and mortality. All authors reviewed the manuscript and gave their approval for its final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Agustin Ibanez, Josiah Kephart and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Ming Yang, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
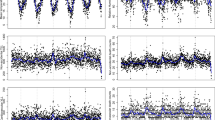
Extended Data Fig. 1 Distribution of study population and annual peak temperature in 2008 and 2018.
a. Geographical spread of the study participants (N = 13,527) in 23 provinces in China. b. Annual peak daily air temperatures in China for the year 2008. c. Annual peak daily air temperatures in China for the year 2018.
Extended Data Fig. 2 Selection procedure of the study population.
Out of 16,954 individuals, we excluded 379 individuals under 65 years of age and 105 individuals due to missing data on key variables such as education (50), occupation (22), marital status (46), and ADL status (1), with some individuals having multiple missing values. Additionally, 2,931 individuals were lost to follow-up after the first survey, contributing person-time to the study. The final analysis included 13,527 participants, of whom 2,341 were still alive at the end of follow up. A total of 1,806 participants were lost in subsequent surveys but had contributed person-time until their loss. There were 3,249 deaths during the summer months (May to September) and 6,131 deaths outside of the summer season.
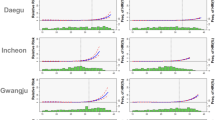
Extended Data Fig. 3 Population attributable fractions (PAF) of heatwave using CMA, WMO, and NOAA definitions.
Note: The bar plots indicate the weighted PAF of heatwave days among the overall study population (N = 13,527). Communality of environmental covariates (relative humidity, PM2.5, NDVI), basic demographic factors (age, sex) and physical and cognitive health status (ADL, IADL, MMSE) was considered and included as the adjustment. The error bars indicate the lower and upper boundaries of 95%CI.
Extended Data Fig. 4 Heatwave vulnerability analysis stratified by age group and sex.
Note: Stratification analysis by age group was adjusted for sex, while stratification analysis by sex was adjusted for age. The stratified Cox model allowed for separate baseline hazard functions for residential provinces. The correlation of the daily observations within each individual is properly accounted for by specifying their unique IDs.
Supplementary information
Supplementary Information
Supplementary Discussion, Methods Questionnaire Figs. 1–6, and Fig. 1.
Supplementary Tables
Supplementary Tables 1–16.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xi, D., Liu, L., Zhang, M. et al. Risk factors associated with heatwave mortality in Chinese adults over 65 years. Nat Med (2024). https://doi.org/10.1038/s41591-024-02880-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41591-024-02880-4
This article is cited by
-
Tackling heat-related mortality in aging populations
Nature Medicine (2024)