Abstract
In this randomized phase 2 trial, blockade of cytotoxic T-lymphocyte protein 4 (CTLA-4) with continuation of programmed death protein 1 (PD-1) blockade in patients with metastatic melanoma who had received front-line anti-PD-1 or therapy against programmed cell death 1 ligand 1 and whose tumors progressed was tested in comparison with CTLA-4 blockade alone. Ninety-two eligible patients were randomly assigned in a 3:1 ratio to receive the combination of ipilimumab and nivolumab, or ipilimumab alone. The primary endpoint was progression-free survival. Secondary endpoints included the difference in CD8 T cell infiltrate among responding and nonresponding tumors, objective response rate, overall survival and toxicity. The combination of nivolumab and ipilimumab resulted in a statistically significant improvement in progression-free survival over ipilimumab (hazard ratio = 0.63, 90% confidence interval (CI) = 0.41–0.97, one-sided P = 0.04). Objective response rates were 28% (90% CI = 19–38%) and 9% (90% CI = 2–25%), respectively (one-sided P = 0.05). Grade 3 or higher treatment-related adverse events occurred in 57% and 35% of patients, respectively, which is consistent with the known toxicity profile of these regimens. The change in intratumoral CD8 T cell density observed in the present analysis did not reach statistical significance to support the formal hypothesis tested as a secondary endpoint. In conclusion, primary resistance to PD-1 blockade therapy can be reversed in some patients with the combination of CTLA-4 and PD-1 blockade. Clinicaltrials.gov identifier: NCT03033576.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data and code to reproduce the analyses presented in this article are available upon request from SWOG in accordance with SWOG’s data sharing policy and process: https://www.swog.org/sites/default/files/docs/2019-12/Policy43_0.pdf. The protocol (including the statistical analysis plan in Section 11 of the protocol) and informed consent are found in the Supplementary Information.
References
Robert, C. et al. Nivolumab in previously untreated melanoma without BRAF mutation. N. Engl. J. Med. 372, 320–330 (2015).
Robert, C. et al. Pembrolizumab versus ipilimumab in advanced melanoma. N. Engl. J. Med. 372, 2521–2532 (2015).
Larkin, J. et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N. Engl. J. Med. 373, 23–34 (2015).
Ribas, A. et al. Association of pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA 315, 1600–1609 (2016).
Tumeh, P. C. et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 515, 568–571 (2014).
Ribas, A. & Wolchok, J. D. Cancer immunotherapy using checkpoint blockade. Science 359, 1350–1355 (2018).
Sharma, P. & Allison, J. P. The future of immune checkpoint therapy. Science 348, 56–61 (2015).
Ribas, A. Releasing the brakes on cancer immunotherapy. N. Engl. J. Med. 373, 1490–1492 (2015).
Sharma, P. & Allison, J. P. Immune checkpoint targeting in cancer therapy: toward combination strategies with curative potential. Cell 161, 205–214 (2015).
Wei, S. C. et al. Distinct cellular mechanisms underlie anti-CTLA-4 and anti-PD-1 checkpoint blockade. Cell 170, 1120–1133 (2017).
Wei, S. C. et al. Combination anti-CTLA-4 plus anti-PD-1 checkpoint blockade utilizes cellular mechanisms partially distinct from monotherapies. Proc. Natl Acad. Sci. USA 116, 22699–22709 (2019).
Ribas, A. et al. Imaging of CTLA4 blockade-induced cell replication with 18F-FLT PET in patients with advanced melanoma treated with tremelimumab. J. Nucl. Med. 51, 340–346 (2010).
Cha, E. et al. Improved survival with T cell clonotype stability after anti-CTLA-4 treatment in cancer patients. Sci. Transl. Med. 6, 238ra270 (2014).
Robert, L. et al. Distinct immunological mechanisms of CTLA-4 and PD-1 blockade revealed by analyzing TCR usage in blood lymphocytes. Oncoimmunology 3, e29244 (2014).
Robert, L. et al. CTLA4 blockade broadens the peripheral T-cell receptor repertoire. Clin. Cancer Res. 20, 2424–2432 (2014).
Huang, R. R. et al. CTLA4 blockade induces frequent tumor infiltration by activated lymphocytes regardless of clinical responses in Humans. Clin. Cancer Res. 17, 4101–4109 (2011).
Taube, J. M. et al. Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy.Clin. Cancer Res. 20, 5064–5074 (2014).
Pires da Silva, I. et al. Ipilimumab alone or ipilimumab plus anti-PD-1 therapy in patients with metastatic melanoma resistant to anti-PD-(L)1 monotherapy: a multicentre, retrospective, cohort study. Lancet Oncol. 22, 836–847 (2021).
Olson, D. J. et al. Pembrolizumab plus ipilimumab following anti-PD-1/L1 failure in melanoma. J. Clin. Oncol. 39, 2647–2655 (2021).
Friedman, C. F. et al. Ipilimumab alone or in combination with nivolumab in patients with advanced melanoma who have progressed or relapsed on PD-1 blockade: clinical outcomes and translational biomarker analyses. J. Immunother. Cancer 10, e003853 (2022).
Schwartz, L. H. et al. RECIST 1.1—update and clarification: from the RECIST committee. Eur. J. Cancer 62, 132–137 (2016).
Tetzlaff, M. T. et al. Pathological assessment of resection specimens after neoadjuvant therapy for metastatic melanoma. Ann. Oncol. 29, 1861–1868 (2018).
Larkin, J. et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N. Engl. J. Med. 381, 1535–1546 (2019).
Kluger, H. M. et al. Defining tumor resistance to PD-1 pathway blockade: recommendations from the first meeting of the SITC Immunotherapy Resistance Taskforce. J. Immunother. Cancer 8, e000398 (2020).
Tawbi, H. A. et al. Relatlimab and nivolumab versus nivolumab in untreated advanced melanoma. N. Engl. J. Med. 386, 24–34 (2022).
Atkins, M. B. et al. Combination dabrafenib and trametinib versus combination nivolumab and ipilimumab for patients with advanced BRAF-mutant melanoma: the DREAMseq Trial-ECOG-ACRIN EA6134. J. Clin. Oncol. 41, 186–197 (2023).
Luke, J. J., Flaherty, K. T., Ribas, A. & Long, G. V. Targeted agents and immunotherapies: optimizing outcomes in melanoma. Nat. Rev. Clin. Oncol. 14, 463–482 (2017).
Rohaan, M. W. et al. Tumor-infiltrating lymphocyte therapy or ipilimumab in advanced melanoma. N. Engl. J. Med. 387, 2113–2125 (2022).
Sharma, P., Hu-Lieskovan, S., Wargo, J. A. & Ribas, A. Primary, adaptive, and acquired resistance to cancer immunotherapy. Cell 168, 707–723 (2017).
Acknowledgements
We thank the patients and their caregivers, the support of the patient advocates S. Guild and V. Guild, and the support of Bristol Myers Squibb in providing investigational agents for the study. The study was funded by Southwest Oncology Group (SWOG) National Institutes of Health (NIH) and NCI grant nos. LS1616_R01LDRGAPP01, U10CA180888, U10CA180819, U10CA180821 and U10CA18068. Biopsies and their analyses were supported by the Stand Up to Cancer (SU2C) Catalyst-Bristol Myers Squibb-American Association for Cancer Research grant no. CT06-17. A.R. is funded by NIH and NCI grant nos. P01 CA244118 and R35 CA197633, and the Parker Institute for Cancer Immunotherapy, the Ressler Family Fund and support from K. and D. Schultz, T. and D. Jones, K. and J. Witemyre, T. Stutz and J. Isaacson. K.M.C. was supported by the Cancer Research Institute Postdoctoral Fellowship Program, the V Foundation Gil Nickel Melanoma Research Fellowship and the Parker Institute for Cancer Immunotherapy and V Foundation Bridge Fellowship. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
A.V., S.L.B., E.S., S.P.P., K.F.G., J.M., M.C.W. and A.R. designed, initiated and oversaw the conduct of the clinical trial. A.V., K.L.K., N.I.K., F.C., J.A.S., A.I., A.I.V., T-G.T., B.C., D.C.P., Y.C., K.M., C.B., C.A.D., D.B.J., Z.E., S.C., S.H-L., S.P.P. and A.R. enrolled, treated and cared for the patients on the clinical study protocol. A.V., S.L.B., J.M., M.C.W. and A.R. conducted the clinical data analyses. K.M.C., E.M., C.R.G., I.B-C., A.V-C. and I.P.G. processed, banked and analyzed the biopsies. P.O.S. and L.F.K. performed the dermatopathological analyses of biopsies. K.M.C., P.O.S., L.F.K. and M.C.W. interpreted the biopsy analyses. A.V., S.L.B., K.M.C., M.C.W. and A.R. wrote the first draft of the manuscript. All authors proofread and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
A.V. declares employment by Caris Life Sciences and consults with the George Clinical, West Clinic; he sits on the advisory boards and steering committees of Bristol Myers Squibb, Genentech and Mirati Therapeutics. He has received research funding from SWOG, Stand Up 2 Cancer, Bristol Myers Squibb and American Association for Cancer Research. K.L.K. reports clinical trial funding through the institution from Merck. N.I.K. sits on the advisory board for Bristol Myers Squibb, Regeneron, Merck, Iovance Biotherapeutics, Genzyme, Novartis, Nektar, Castle Biosciences, Instil Bio and the National Comprehensive Cancer Network (via Pfizer); he is a member of the study steering committees of Bristol Myers Squibb, Nektar, Regeneron and Replimune; he is a member of the data safety monitoring boards of Astra-Zeneca and Incyte; he holds common stock stock in Bellicum Pharmaceuticals, Asensus Surgical and Amarin Corporation; and he has received research funding (to the institute) from Bristol Myers Squibb, Merck, Novartis, GSK, HUYA Bioscience International, Amgen, Regeneron, Celgene, Replimmune and Modulation Therapeutics. K.M.C. reports being a shareholder in Geneoscopy and has received consulting fees from Geneoscopy, PACT Pharma, Tango Therapeutics, Flagship Labs 81 and the Rare Cancer Research Foundation. P.S. received research funding, consulted for and served on the advisory board for Castle Biosciences. F.C. reports that his institution receives research funding for clinical trials. A portion of that funding comes from trials sponsored by Amgen and Replimune and helps cover her salary. J.A.S. reports consultation for Apixagen Consultation, Iovance and Necktor and up-to-date royalties. A.I. discloses research funding to her institution from Checkmate Pharmaceuticals, Dynavax Technologies, GSK/S. Cannon, Immunocore, Merck and Neon Therapeutics/S. Cannon. A.I.V. had an investigator-initiated study supported by Bristol Myers Squibb, but it closed 2 years ago and understands that it does not qualify as a competing interest. T.-G.T. reports institutional funding from Bristol Myears Squibb, Merck, Roche, Pfizer, Novartis, Regeneron and Astra-Zeneca. B.C. reports clinical trial support paid to his institution from SWOG, Bristol Myers Squibb, Macrogenics, Merck, Karyopharm, Infinity, Advenchen, Idera, Xencor, Compugen, Iovance, PACT Pharma, RAPT Therapeutics, Immunocore, IDEAYA, Ascentage, Novartis, Atreca, Replimmune, Instil Bio, Adagene, TriSalus and Xilio; he reports payment for lectures for Sanofi Genzyme and sits on the advisory boards of Instil Bio, Nektar, Delcath, Novartis, Genentech, IDEAYA, OncoSec, Iovance and Deciphera. Y.C. reports research funding from BMS RELATIVITY-098 to his institution, personal financial interest in Bristol Myers Squibb as speaker on melanoma and is a member of the advisory board; he has spoken about melanoma on behalf of Pfizer. D.B.J. has served on the advisory boards or as a consultant for Bristol Myears Squibb, Catalyst Biopharma, Iovance, Jansen, Mallinckrodt, Merck, Mosaic ImmunoEngineering, Novartis, Oncosec, Pfizer, Targovax and Teiko, and has received research funding from Bristol Myears Squibb and Incyte. Z.E. reports serving on the advisory boards of Array BioPharma, Pfizer, OncoSec, Regeneron, Genentech, Novartis and Natera; she has received research funding from Novartis, Pfizer and Boehringer Ingelheim. S.C. reports serving on the advisory boards of Bristol Myers Squibb, Novartis, Pfizer and Regeneron. S.H-L. reports consulting for Amgen, Genmab, Xencor, Regeneron, Nektar, Astellas, Bristol Myers Squibb and Merck; she reports support from Amgen and Merck, and has undertaken contracted research for Pfizer, Plexxikon, Genentech, Neon Therapeutics, Nektar, Astellas, F Star, Xencor, Merck, Vedanta, Kite Pharma, Boehringer Ingelheim, OncoC4, Dragonfly, Bristol Myers Squibb and BioAlta. S.P.P. reports the following relevant competing interests: clinical trial support to her institution from Bristol Myers Squibb; advisory board membership of Cardinal Health, Castle Biosciences and Delcath; serving as a consultant for Foghorn Therapeutics (clinical trial support to her institution); providing clinical trial support for Ideaya (via her institution); sitting on the data safety monitoring board of Immunocore; sitting on the advisory board of Immatics; providing clinical trial support via her institution to InxMed, Lyvgen Biopharma and Novartis; serving as consultant on the advisory board of Pfizer; providing clinical trial support to Provectus Biopharmaceuticals; providing clinical trial support via her institution to Reata Pharmaceuticals and sitting on the data safety monitoring board; she has sat on the advisory board of Replimmune and the scientific advisory board of TriSalus Life Sciences; and she has provided clinical trial support (via her institution) to Seagen and Syntrix Bio, and has consulted for Advance Knowledge in Healthcare. K.F.G. is an employee and stockholder of Merck Sharp & Dohme, a subsidiary of Merck & Co. A.R. has received honoraria from consulting with Amgen, Bristol Myers Squibb and Merck; is or has been a member of the scientific advisory board and holds stock in Advaxis, Appia, Apricity, Arcus, Compugen, CytomX, Highlight, ImaginAb, ImmPact, ImmuneSensor, Inspirna, Isoplexis, Kite-Gilead, Lutris, MapKure, Merus, PACT, Pluto, RAPT Therapeutics, Synthekine and Tango; and has received research funding from Agilent and from Bristol Myers Squibb through SU2C, and patent royalties from Arsenal Bio. J.M., L.F.K., D.C.P., K.M., C.L.B., C.A.D., E.M., C.R.G., I.B.C., A.V-C., I.P.G., E.S., S.L.B. and M.C.W. declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Reinhard Dummer, Michael Postow and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Ulrike Harjes, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Kaplan-Meier plot of overall survival.
The 12-month OS estimates were 63% (90% CI: 52%–72%) and 57% (38%–71%) for the combination therapy versus ipilimumab alone groups, respectively.
Extended Data Fig. 2 Disposition of tumour biopsies assessed for CD8-positive cell quantitation.
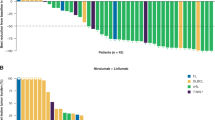
a) CONSORT diagram of tumour biopsies assessed for CD8-positive cell quantitation. b) Alluvial plot depicting the patient demographics (x-axis) for each patient (alluvium) that was included in the final analysis for CD8 T-cell quantitation. Demographics include trial arm, best overall response (BOR, also shown by fill colour), whether pathologic features consistent with melanoma regression were observed on-therapy, and which sample timepoints were included in analysis (either screening or on-therapy biopsy only, or paired). c) Alluvial plot depicting patient demographics and pathologic annotation (x-axis) for each biopsy (alluvium) that was annotated by the dermatopathologists. Fill colour indicates whether the biopsy was included in the final analysis for CD8 T cell quantitation. Biopsies are annotated for the trial arm, BOR, and whether features consistent with pathologic regression of melanoma were noted in the on-therapy biopsies for the corresponding patient, as well as the timepoint the biopsy was taken, and the manual notes for the biopsy from the dermatopathologists.
Extended Data Fig. 3 Semi-automated workflow for CD8-positive cell quantitation in tumour biopsies.
a) Representative images for manual annotation of tumour and tumour periphery regions. b) Screenshot of cell segmentation, identifying CD8-positive cells (red) and CD8-negative cells (blue), for CD8 cell quantitation. Scale bars in each panel are 100um. c) Density of CD8 positive cells detected within the annotated tumour periphery. Paired baseline and on-treatment biopsies are indicated by points connected by lines. Dotted lines indicate patients with pathological features of regressed melanoma in the on-treatment biopsy. The number of patients shown in each group is indicated by the number along the x-axis (Ipilimumab arm, N = 2 partial response [PR], N = 3 stable disease [SD], N = 13 progressive disease [PD]; nivolumab and ipilimumab arm, N = 7 complete response [CR], N = 8 PR, N = 7SD, N = 25 PD). Box plots indicate the median (middle line), 25th and 75th percentiles (box) and 5th and 95th percentiles (whiskers).
Extended Data Fig. 4 Modeling of the timing of CD8 infiltration and the pathological assessment of areas of melanoma regression.
a) Proposed model for the timing of the anti-tumour CD8 T-cell response (numbers are not based upon real data), captured by on-therapy tumour biopsies collected day 28–35 following the start of combination therapy. The red line indicates the changes of CD8 T cell density with respect to the change in tumour cell density (blue line). The grey regions demonstrate the timing captured across on-therapy biopsies from patients who respond to nivolumab plus ipilimumab, where some biopsies captured the peak or maximum CD8 T cell density. Others were collected following the regression of the majority of the tumour, where few CD8 T cells and few melanoma cells remaining, consistent with pathological features of melanoma regression (for example tumour necrosis, fibrosis, presence of melanophages). b) Example of patient-matched screening and on-therapy biopsies. Biopsies collected from a patient who had a complete response to nivolumab plus ipilimumab were stained for CD8 T cells using immunohistochemistry (IHC). The on-therapy biopsy contained residual tumour cells in addition to very high CD8 T cell infiltration. c) Example of patient-matched screening and on-therapy biopsies, stained for CD8 T-cells using IHC, where the biopsies of a patient with complete response to nivolumab plus ipilimumab showed pathological features consistent with melanoma regression. Indicated are areas of tumour necrosis and fibrosis (blue) and tumour regression with residual CD8 T cell infiltration (red).
Extended Data Fig. 5 Model for the mechanism of reversal of tumour resistance to anti-PD-1 with the addition of anti-CTLA-4.
a) Response to PD-1 blockade therapy is mediated by the intratumour pre-existence of tumour-specific CD8 T cells that are negatively regulated by the reactive expression of PD-L1 by cancer cells. Administering an anti-PD-1/L1 therapy results in tumour regression. b) Tumours that are resistant to PD-1 blockade therapy are enriched for low intratumour infiltration by CD8 T cells. c) Releasing the CTLA-4 checkpoint promotes and the trafficking of T cells to the tumour. d) To obtain the maximum density of CD8 T cells in the tumour, and corresponding clinical responses, it requires concurrent release of both the CTLA-4 and PD-1 checkpoints.
Supplementary information
Supplementary Information
Supplementary Tables 1–3, CONSORT checklist and study protocol.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
VanderWalde, A., Bellasea, S.L., Kendra, K.L. et al. Ipilimumab with or without nivolumab in PD-1 or PD-L1 blockade refractory metastatic melanoma: a randomized phase 2 trial. Nat Med 29, 2278–2285 (2023). https://doi.org/10.1038/s41591-023-02498-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-023-02498-y