Abstract
Climate change may be the greatest health threat of the twenty-first century, impacting lives both directly and indirectly, through undermining the environmental and social determinants of health. Rapid action to decarbonize economies and build resilience is justified on health, human rights, environmental and economic grounds. While the necessary health response is wide ranging, it can largely be encapsulated within three grand challenges: (i) promote actions that both reduce carbon emissions and improve health; (ii) build better, more climate-resilient and low-carbon health systems; and (iii) implement public health measures to protect from the range of climate risks to health. The health community can make a unique and powerful contribution, applying its trusted voice to climate leadership and advocacy, providing evidence for action, taking responsibility for climate resilience and decarbonization of healthcare systems, and guiding other sectors whose actions impact substantially on health, carbon emissions and climate resilience.
Similar content being viewed by others
Main
The world is warming at a faster rate than at any time in human history, due mainly to the burning of fossil fuels—with an important additional contribution through land-use changes, mainly for agriculture and forestry. Unless urgent action is taken to cut carbon emissions, global warming will soon exceed the 1.5 °C limit set in the Paris climate agreement, and current trends are likely to result in over 3 °C of warming by the end of the century1.
Climate change has been identified as potentially the greatest health challenge of the twenty-first century2,3. It is bringing more deadly extreme heat and wildfires, increasing noncommunicable diseases and facilitating the emergence and spread of infectious diseases, contributing to health emergencies. It is impacting the health workforce and infrastructure, reducing capacity to provide universal health coverage. More fundamentally, climate shocks and growing stresses such as droughts and rising sea levels are undermining the environmental and social determinants of physical and mental health, from clean air and water, to sustainable food systems, to livelihoods—and threatening the existence of some nations1. Further delay in action will increase the risks, undermine decades of improvements in global health and contravene our collective commitments to ensure the human right to health for all4.
The same development pathways and economic choices that are driving the climate crisis are also directly causing large health impacts. These include polluting energy systems that the World Health Organization (WHO) estimates to cause almost 7 million premature deaths from air pollution each year5; environmentally destructive and unhealthy food systems that are contributing to the global increase in noncommunicable disease; and urban planning and transport systems that result in car dependency—contributing to the burdens of physical inactivity and road traffic injuries. The healthcare sector itself is now also a notable contributor to climate change, responsible for almost 5% of global carbon emissions6,7.
The world is not yet responding to the scale of this challenge. Although the ‘right to health’ is at the core of the United Nations Framework Convention on Climate Change (UNFCCC) and the Paris Agreement, it is largely absent from its operational mechanisms. Less than 0.5% of international climate finance is currently allocated to health projects8, and only 30% of nationally determined contributions to the Paris Agreement take account of the large health gains expected from climate change mitigation9. Similarly, while health is routinely identified as a top priority for climate action, 70% of countries lack adequate finance to implement a national adaptation plan (NAP) for health, and few national or international health actors allocate meaningful resources to climate action10.
As part of their latest annual health monitoring report for the sustainable development goals11, the WHO have identified key objectives for the health response to climate change. In line with this, we outline the main connections between climate change and health and summarize three ‘grand challenges’ to protect and promote health in the face of climate change. In addition, we discuss the specific roles of the health community in responding to these challenges and driving change within and beyond the health sector.
Current status of climate change impacts on health
The Sixth Assessment Report of the Intergovernmental Panel on Climate Change estimates that up to 3.6 billion people are living in conditions that are highly vulnerable to the impacts of climate change12. Low-income and lower-middle-income countries and Small Island Developing States face the greatest health consequences of climate change, despite contributing the least to historical global emissions8,12. It is estimated that over the past decade, the mortality rate from extreme weather events was 15 times higher for populations in highly vulnerable regions than in regions with the lowest vulnerability12. Within-country disparities also exist; those living in poverty, older people, women, children, indigenous peoples, outdoor workers, the socially isolated and individuals with preexisting medical conditions are typically at highest risk12.
The WHO estimates that approximately 2 billion people lack access to safe drinking water13. Furthermore, there are about 600 million global cases of foodborne illnesses each year and children under the age of 5 years carry 30% of the burden of foodborne deaths (or 125,000 child deaths every year)14. Extreme weather events and climate-related environmental stressors degrade water and soil safety, thereby increasing the risks of waterborne and foodborne illnesses.
In 2020, about 770 million people in the world faced hunger, primarily in Africa and Asia—with women and children at particularly high risk15. Higher temperatures, rising sea levels and flooding affect all aspects of food and nutrition security. Consequently, climate-related reductions in agricultural and marine productivity, biodiversity loss, volatility in food prices and disruptions in food imports further impact the quality, quantity and diversity of food consumed, leading to food and nutrition crises.
Changing temperature and precipitation patterns also create conditions that facilitate the transmission of mosquito-borne, tick-borne and rodent-borne diseases in many regions12. If prevention methods are not strengthened, this could lead to an increase in deaths from vector-borne diseases (already at over 700,000 each year)16.
The health risks of climate change can have both immediate and long-term consequences. Extreme weather events can lead to acute mental health conditions such as anxiety, depression and post-traumatic stress. The cumulative effect of loss of livelihood, displacement, disrupted social cohesion and uncertainty from climate change can also result in longer-term mental health disorders17.
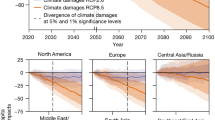
Research is ongoing to quantify the current and projected future health effects of climate change. A recent study of 43 countries estimated that 37% of heat-related deaths are attributable to human-induced climate change18, and the 2022 Lancet Countdown on Climate Change and Health Report found that heat-related mortality of people older than 65 years increased by almost 70% over the past two decades7. The same report estimates 98 million more people reporting moderate-to-severe food insecurity in 2020 than the average in 1981–2010, due to climate change7. Advances in the application of detection and attribution studies to health outcomes are also providing greater insight and confidence regarding the magnitude of climate change-related health impacts of extreme weather events19.
Providing a single estimate of the overall health burden of climate change is challenging. The WHO has published conservative projections estimating the effect of climate change only on malaria, heat exposure in older people, diarrheal disease in children, undernutrition in children and coastal flood mortality, for the 2030s and 2050s. For example, under a medium-to-high emissions scenario, it was estimated that climate change would cause approximately 250,000 additional deaths per year by the 2030s20. While the WHO assessments established that climate change was already having a substantial adverse impact on human health, which was projected to increase into the future, they recognized the inability of existing models to account for major causal pathways for which no reliable quantitative models exist, or that impact a wide range of health outcomes or that may have compounding effects with other health risks. Examples include persistent drought, migration pressures and risk of conflict. Further methodological work is needed to either improve quantitative models or develop alternative assessment approaches to capture these important risks.
The fact that poorer communities tend to have relatively lower carbon emissions, but higher health vulnerabilities to climate change, highlights the need for specific consideration of equity in designing the public health response. A just and equitable response requires that those with both the largest responsibility for carbon emissions, and the greatest means, should bear the largest part of any costs of climate change mitigation and adaptation, and that public measures should be explicitly designed to promote health equity, for example, by prioritizing particularly vulnerable groups.
Three grand challenges for health and climate action
Climate change presents a fundamental threat to human health. It affects the physical environment as well as all aspects of both natural and human systems—including social and economic conditions and the functioning of health systems. It is therefore a ‘threat multiplier’, undermining and potentially reversing decades of health progress.
We identify three ‘grand challenges’ to address the threat of climate change to health.
Promote actions that both reduce carbon emissions and improve health
To stay within the 1.5 °C global warming limit set out in the 2015 Paris Agreement and avoid escalating and intolerable impacts on human health and well-being, the world will need to drastically reduce carbon emissions.
While efforts to achieve this goal are often discussed in terms of paying higher economic costs to protect the global climate, evidence now shows that the global transformation to clean energy would pay for itself through reduced energy costs in as little as 6 years21. This transformation would also bring more and better jobs, and greatly improve health22. Valuing these societal benefits is estimated to bring the payback time to less than 1 year21.
Health has a strong influence on estimates of the benefits of climate action, as the development pathways that are driving climate change also have very large negative effects on human health. Notably, the sectors driving greenhouse gas emissions—including energy, transport, industry, agriculture and waste—are also sources of harmful air pollutants, which increase mortality from cardiovascular disease, respiratory illnesses and cancer23. The air quality improvements that would accompany compliance with the Paris Agreement would therefore avoid millions of premature deaths every year by 2050, bringing economic benefits that would equal or exceed the mitigation costs24,25.
These benefits can also be estimated at the national level, and in relation to specific policies. A 2021 WHO study modeled the health benefits of adjusting Pakistan’s nationally determined contribution to the UNFCCC under the Paris Agreement. The study found that under a high-ambition scenario, Pakistan could reduce greenhouse gas emissions by approximately 27.5% by 2030, compared to a reference case scenario. The accompanying air quality improvements could prevent more than 65,000 annual premature air pollution-related deaths by the same year, with associated annual economic benefits estimated to be about 9 billion USD26.
Solutions exist to cut carbon emissions across all sectors22 and would bring a range of large health gains beyond air quality alone. For example, road transport is estimated to account for almost one-fifth of global CO2 emissions, while the global food system is responsible for between 21% and 37% of greenhouse gas emissions27. Sustainable urban planning that promotes a shift toward safe walking and cycling as well as access to public transport can lead to health benefits from increased physical activity, reduced ambient air pollution and lower noise exposure28. In high-income countries, a transition toward plant-based diets, lower red meat consumption and less food waste could help to mitigate climate change while lowering the health burden of diet-related noncommunicable diseases27. In low-income and middle-income countries, sustainable agriculture and food production can protect local environments, reduce emissions and promote food and nutrition security15.
In support of this, a study of nine countries with high greenhouse gas emissions found that, if these countries followed a sustainable pathway scenario consistent with the goals of the Paris Agreement, this would be expected to bring a total annual reduction of 1.18 million air pollution-related deaths, 5.86 million diet-related deaths and 1.15 million deaths due to physical inactivity by 2040 (ref. 24).
The fact that many actions that would reduce carbon emissions would also bring large health benefits has two major implications. Firstly, health should be central to policies in all of these sectors, and in national and international climate policy. Under the Paris Agreement, countries set out their mitigation commitments and adaptation priorities through their nationally determined contributions and NAPs. The 2023 WHO Review of Health in the Nationally Determined Contributions report found that over 90% of countries reflect health priorities in this context9. This ensures that health considerations have at least an entry point in national and international climate plans and processes, to be delivered through specific policy measures.
Secondly, health actors should work to identify and accelerate those climate change mitigation actions that bring the greatest health gains, helping to galvanize political and financial support for accelerated climate action, and sustainable development overall. These include a just and inclusive transition to renewable energy, phasing out coal combustion and inefficient fossil fuel subsidies, promoting sustainable and healthy urban transport systems and housing, and sustainable and healthy food systems and diets4.
Build better, more resilient and environmentally sustainable health systems
Building climate-resilient and sustainable health systems involves a systematic and comprehensive approach to strengthening all core functions of a health system so it can respond and adapt to the health risks of climate change29. This coincides with increased political momentum to transform the provision of universal health coverage in the face of increasing demand and rising costs, with a revitalization of primary healthcare, bringing health services closer to people and communities30.
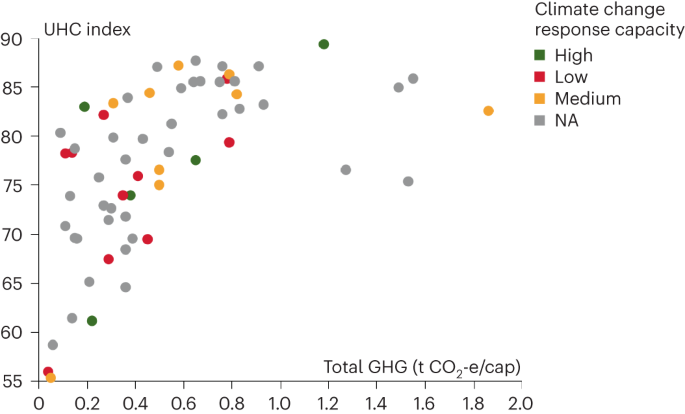
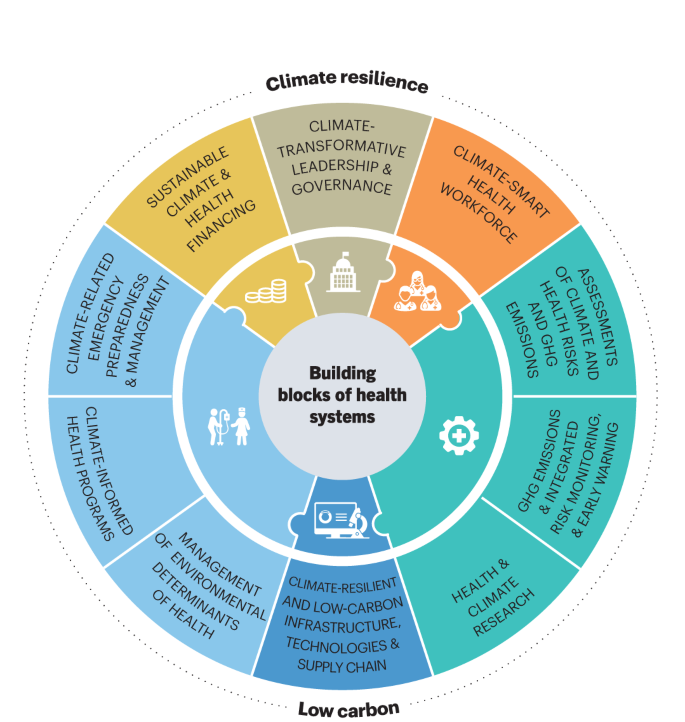
To meet even basic levels of healthcare provision, services including clean energy, water and sanitation, waste management, essential medical equipment and a trained health workforce are essential. To ensure economic and environmental sustainability, this transformation should also support the shift toward a circular economy in health (and in society generally), through rethinking models of care—including optimizing the use of telemedicine, minimizing consumption and wastage and making more sustainable purchasing decisions. All of the above can cut operational costs, reduce losses from climate hazards and increase quality of care—enhancing universal health coverage and primary healthcare. The overall goal for health systems should be to improve delivery of high-quality health services to all, minimize carbon emissions from healthcare, and enhance resilience of health systems to climate and other shocks (Fig. 1).
For each country (circle), the graph shows WHO Universal Health Coverage (UHC) Index score (vertical axis), versus estimated carbon emissions from healthcare (in annual tonnes of carbon dioxide equivalent per capita; horizontal axis). Circles are colored by score on an aggregate index of actions taken to build health system resilience to climate change, as measured by the WHO Health and Climate Change Survey Report10. The pattern that emerges is one of large differences in all dimensions. Some countries with currently very high health sector carbon emissions need to urgently reduce emissions without sacrificing health performance, while others with currently low health sector carbon emissions need to focus on increasing their health systems performance in a way that ensures a low-carbon future with health equity45. Figure adapted from ref. 45. GHG, greenhouse gas; NA, data not available.
While the health sector is responsible for almost 5% of global greenhouse gas emissions, this contribution is as high as 10% in some high-income nations6,7,31. Health systems can decarbonize through measures such as more efficient or renewable energy sources, as well as through optimizing the use of resources, sustainable procurement practices and waste reduction—as over 70% of carbon emissions from healthcare come from the supply chain. Implementing these measures can bring multiple health system benefits by contributing to a higher quality of care, greater accessibility, more reliable services, reduced occupational hazards from air pollution and waste and reduced costs31,32.
In particular, health systems in all countries can benefit from the transition to renewable energy which, over the medium term to long term is now cheaper and more reliable than fossil fuel sources and generally well suited to health facilities—especially in remote, off-grid settings. The greatest opportunities for improvement are likely to be in poorly served populations. For example, over 50% of health facilities in some countries in sub-Saharan Africa lack core environmental services including energy, water and sanitation, and many lack any safe management of healthcare waste33,34. Investments in these settings can allow countries to ‘leapfrog’ directly to better, cheaper, and more resilient services.
In addition, in countries across the entire range of economic development, vulnerabilities in infrastructure, management practices and human resources make health systems vulnerable to climate extremes (such as heatwaves, high winds, dust storms and floods) as well as longer-term threats ranging from persistent droughts and sea level rise, to the spread of infectious diseases to areas that currently lack the public health capacities to address them. This makes it essential to improve the ability to detect, prepare for, respond to and recover from both short-term shocks and long-term stresses.
Increasing climate resilience and controlling carbon emissions in health systems should not result in separate, parallel structures. Instead, it should seek to reinforce and build on existing functions. The 2015 WHO Operational Framework for Building Climate Resilient Health Systems29 builds on the six core building blocks of health systems (leadership, workforce, information systems, technology, service delivery and finance), and describes how specific actions to build climate resilience can be added to each of these. The framework is now being updated to include complementary actions to control carbon emissions (Fig. 2).
The health system response to climate change should build on the core ‘building blocks’ of health systems: leadership, workforce, information systems, infrastructure and technologies, service delivery and finance (inner ring); adding additional functionality and capacity specifically to build resilience to climate shocks and stresses, while minimizing carbon emissions (outer ring)45. Figure adapted from ref. 45.
Implement public health measures to protect from the range of climate risks to health
The diverse risks that climate change presents to health, many acting through long causal pathways, require action not only within healthcare (that is, curative services), but also on public health functions, including on the environmental and social determinants of health.
The essential first step is to understand the scale and nature of health vulnerabilities to climate variability and change, taking account of important determinants including geography and socioeconomic condition, and considering differential impacts on subpopulations—typically in the form of a climate change and health vulnerability and adaptation assessment. This informs the development of evidence-based NAPs and interventions, most commonly in the form of a health national adaptation plan (HNAP) aligned with the whole-of-government NAP.
Many countries have made substantial progress on assessment and planning in recent years. The 2021 WHO Health and Climate Change Global Survey found that approximately half of all countries surveyed (48 out of 95) reported having conducted a climate change and health vulnerability and adaptation assessment, while 52% (49 out of 95) reported having a national climate change and health strategy in place10.
HNAPs generally include intervention measures that are shown to protect against current weather and climate hazards, and that can therefore be expected to provide some level of protection against long-term climate change35,36. These vary, but typically include three common features. First, implementation of climate-informed surveillance and response systems for key risks, such as extreme heat, infectious disease, and food and nutrition security to improve lead times and accuracy of health early warning systems, and to project the longer-term effects of climate variability and change. Second, integration of climate risk into key ‘vertical’ health programs, targeting a specific disease or population group35. This includes emergency preparedness and response, infectious disease control, mental health and programs focusing on groups with particular vulnerabilities to climate risks, such as occupational health, maternal, newborn and child health, climate migrant health and healthy aging. Third, supporting resilience and adaptation in ‘health-determining’ sectors, and within communities35. Approximately 25% of the current global burden of disease is attributable to environmental risks—largely determined by decisions outside of health systems23. The greatest health gains, and protection from climate risks, may therefore be achieved through collaboration with other sectors, and some HNAPs also include integration of climate resilience into water and sanitation service provision, the built environment, food and nutrition security programs and through supporting community-based health adaptation.
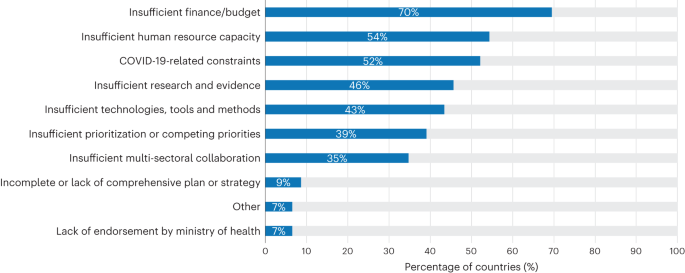
Despite progress on assessment and planning, only a quarter of countries responding in the WHO global survey (11 out of 46) have reached a ‘high’ or ‘very high’ level of implementation. Insufficient finance was a main barrier to implementation of national strategies and plans10 (Fig. 3). In addition to an overall scarcity of resources, action on climate change and health faces an additional financial barrier. While most governments and development agencies identify both health and climate change as top priorities, they generally do so separately, rather than via integrated and mutually reinforcing goals. Meaningful progress on implementation will only come with clear mandates and proportionate resources dedicated specifically to the intersection of climate change and health.
Data from the WHO Climate and Health Country Survey10; 46 country respondents, multiple responses possible.
Ultimately, tackling climate change and protecting health will require effective monitoring and continuous learning and improvement. The interaction between climate change, other environmental and social determinants of health, health interventions and health effects, is constantly evolving. This calls for integrated monitoring systems across these dimensions to improve understanding, track progress and guide health actions.
The unique role of the health community in delivering transformative change
The climate crisis requires transformative action from across society. However, the health community—including frontline health workers, Ministries of Health, intergovernmental and nongovernmental health organizations and health academics—has a unique role to play.
We outline three key functions for the health community in responding to the climate crisis.
Leadership and advocacy
There is increasingly strong evidence from experimental studies from around the world that presenting a positive vision of a healthier, more environmentally sustainable common future, is effective in ensuring public support for climate action, and cutting across political divides37,38,39,40.
Health researchers have assembled a large body of evidence on the health benefits of climate action—and the overwhelmingly negative health consequences of inaction. Health is also central to key regulations and legislation, from air quality and emissions standards, to food standards, to protection of the right to health under national and international law and conventions41. Health institutions should therefore build not only the applied evidence base, but also their own individual and institutional capacity to engage more directly in policymaking.
At the same time, health professionals are increasingly engaged on climate change in a range of roles, from actions to reduce carbon emissions in their professional work, to organized expressions of support for stronger international climate action (https://healthyclimateletter.net/), to a spectrum of public engagement and nonviolent protests to protect their patients from the impacts of climate change and related threats including air pollution. The large number of health professionals, their direct personal connection to individuals and communities, and their position among the most trusted professions in the world42, mean that they have the potential to be among the most powerful advocates for a healthy future through climate action (Box 1).
Evidence and monitoring
Research on climate change and human health is a rapidly growing field, with the number of articles published each year surging more than sixfold over the past decade43. Despite the increase in volume, the research itself remains uneven. Most of the currently available studies are focused on assessing health impacts of climate change, with a particular emphasis on a subset of causal pathways—notably the direct health effects of excessive heat. There is a relative lack of research on other major questions on which health policymakers have expressed demand44—notably the effectiveness of health adaptation measures, the diverse range of potential health co-benefits of both adaptation and mitigation measures, the development of decision-support tools and economic assessments of the benefits and costs of climate and health actions. Research output is also highly unevenly distributed across geographical regions, with many more studies conducted in high-income countries compared to low-income and middle-income countries. Often, data are not available at a level of resolution that corresponds to decision-makers’ needs—that is, for national or subnational levels, or disaggregated by gender, age, ethnicity or socioeconomic status—to assess the differential effects of actions on different population groups. In addition, while much applied research focusses on improving capacity to protect populations from current climate risks, there is also a need for research that takes account of the specific characteristics of long-term climate change, including future projections of changes in various determinants of health, such as aging and urbanizing populations that are particularly vulnerable to extreme heat.
Similar considerations apply in the related fields of monitoring and progress tracking. There has been rapid progress in recent years through initiatives such as the triennial WHO Health and Climate Change Global Survey10 and the annual Lancet countdown on health and climate change7. However, as the integrated field of climate change and health is a relatively new one, there are a range of issues that require further development. These include, among others, standards and indicators for climate-resilient health systems and low-carbon healthcare, and comprehensive and coherent indicator frameworks that connect the high-level sustainable development goals on climate change and health with exposures, vulnerabilities, health effects and progress in implementing climate and health interventions. There is also a need for further strengthening of platforms to make emerging evidence more widely accessible and more directly connected to policy, for example, through regional and national climate change observatories connected to policy institutions.
The urgency and existential threat of climate change calls for greater investment in climate and health research and demonstration projects, and implies that it should pursue a more demand-driven approach to evidence generation, involving decision-makers and affected populations as directly as possible. Such research should be focused on the need to limit global warming, protect and improve health, and ensure universal access to high-quality, climate-resilient, environmentally sustainable health services.
Implementation
Guided by its values and mandates, and informed by the available evidence, the health community can drive the necessary transformation through a range of functions: via direct responsibility for the formal healthcare sector, more broadly through public health functions into the wider community, and also in an advisory role capacity for other sectors that have a strong influence on health and climate change.
The most direct effect that health professionals can exert is through their individual and collective actions within their own work, to deliver improved, climate-resilient and low-carbon health systems. The early experience in this emerging field indicates that success factors include a strong legislative basis (for example, a legally binding climate act mandating emissions reductions across sectors), political leadership from senior management from within the health system, investment in analytical and technical support and networking capacity and, above all, the positive engagement and commitment of the health workforce.
The specific actions to be taken will depend on the professional role and institutional context, and particularly at this relatively early stage of the development of the field, will depend heavily on learning from and sharing experience. This is now being supported from the international level through a range of policy and technical guidance, including the WHO’s Conceptual and Operational Framework for Building Climate Resilient and Low Carbon Health Systems45, guidance on developing roadmaps for low-carbon healthcare31,32, as well as tools for assessing and managing carbon emissions46,47,48. It is also supported by new collaborative initiatives, notably the Alliance for Transformative Action on Climate and Health (Box 1).
Outside healthcare services, public health agencies have a critical role in strengthening and adapting disease prevention to the new challenges presented by climate change. In addition to assessing health vulnerabilities, developing NAPs for health and building capacity, this should also include implementing specific, high-priority interventions for health security. These could include surveillance and early warning systems for climate-sensitive health risks, as well as broader public health and health promotion functions to reduce harmful exposures and enhance the environmental and social determinants of health49.
The third role of the health community in implementation is more indirect but is potentially the most important—to guide policy in sectors other than health, which are driving carbon emissions, and therefore the climate crisis—by providing health analysis, the trusted voice of the health community, and health policy levers. This includes providing health assessments within national climate policies and nationally determined contributions to the UNFCCC, health guidance and impact assessments of policies within key sectors such as energy, transport and food systems, and promoting specific interventions that will bring both climate and health benefits, such as clean energy for households and healthcare facilities. It can also include actions such as behavior change communication around high emission practices, the application of warning labels and marketing restrictions, regulation to control health risks such as air pollution, and pricing mechanisms for products that harm health (which could potentially include fossil fuels).
Cutting across all of the implementation functions above is the issue of finance. While climate change is now recognized as one of the greatest global health threats, there are no dedicated multilateral or bilateral funding mechanisms of the kind that exist for some specific diseases (for example, AIDS, tuberculosis and malaria), health threats (for example, pandemics) or population groups (for example maternal, newborn and child health). There is therefore an important role for the health sector in facilitating simpler, faster and greater access to existing health and climate funding streams, assessing the scale of health impacts which cannot now be avoided and therefore should be supported through any ‘loss and damage’ funds, and proposing improvements in institutional and financial mechanisms for a scale up of investment.
Conclusion
Climate change is already having major negative impacts on public health, and these are increasing rapidly. The societal changes required to stabilize the global climate will entail initial financial cost, but this is outweighed by the health benefits that are projected to result—even before considering the rapid economic payback time—and the fundamental benefit of maintaining the environmental conditions in which humans can survive and thrive.
The range of threats that climate change presents to health is large, diverse and complex, presenting major challenges to health systems, and to the global health architecture, which is largely supported by vertical programs to address individual diseases or health issues. A goal-driven approach to (i) promote actions that both reduce carbon emissions and improve health, (ii) build better, more resilient and environmentally sustainable health systems, and (iii) implement public health measures to protect from the range of climate risks to health, can help to structure and accelerate the health response to climate change.
The scale and scope of the health sector response needs to be commensurate with the size of the health threat. While much progress has been made, much more is still needed. The challenges to delivering this transformation are largely political rather than technical, and require both leadership and public support. The health community has a critical role to play—directly within the health sector by delivering improved services while reducing carbon emissions, as well as through their public health functions to safeguard and improve the environmental and social determinants of health, but also, crucially, through influencing other sectors. The most important role, however, is likely to be as leaders and advocates, changing the narrative from the threat of the climate crisis, to a positive and healthy future through climate action.
References
Intergovernmental Panel on Climate Change. in Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (eds. Masson-Delmotte, V. et al.) (Cambridge Univ. Press, 2021).
Chan, M. Climate change and health: preparing for unprecedented challenges. David E. Barmes Global Health Lecture. https://www.who.int/director-general/speeches/detail/climate-change-and-health-preparing-for-unprecedented-challenges (2007).
Costello, A. et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 373, 1693–1733 (2009).
World Health Organization. COP26 Special Report on Climate Change and Health: the Health Argument for Climate Action. https://apps.who.int/iris/handle/10665/346168 (2021).
Global Health Observatory. Air pollution data portal. https://www.who.int/data/gho/data/themes/air-pollution?lang=en
Health Care Without Harm & ARUP. Health Care Climate Footprint Report https://noharm-global.org/documents/health-care-climate-footprint-report (2019).
Romanello, M. et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet 400, 1619–1654 (2022).
World Health Organization. COP24 Special Report: Health and Climate Change. https://apps.who.int/iris/handle/10665/276405 (2018).
World Health Organization. WHO Review of Health in the Nationally Determined contributions (NDCs) (in the press).
World Health Organization. 2021 WHO Health and Climate Change Survey Report. https://apps.who.int/iris/handle/10665/348068 (2021).
World Health Organization. World Health Statistics 2023: Monitoring Health for the SDGs, Sustainable Development Goals. https://apps.who.int/iris/handle/10665/367912 (2023).
Intergovernmental Panel on Climate Change. Summary for Policymakers. in Climate Change 2022: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (eds. Pörtner, H.-O. et al.) 3–33 (Cambridge Univ. Press, 2022).
WHO, UNICEF & World Bank. State of the World’s Drinking Water: an Urgent Call to Action to Accelerate Progress on Ensuring Safe Drinking Water for All. https://apps.who.int/iris/handle/10665/363704 (2022).
World Health Organization. Estimating the burden of foodborne diseases. https://www.who.int/activities/estimating-the-burden-of-foodborne-diseases
FAO, IFAD, UNICEF, WFP & WHO. The State of Food Security and Nutrition in the World 2021: Transforming Food Systems for Food Security, Improved Nutrition and Affordable Healthy Diets for All. https://www.fao.org/documents/card/en/c/cb4474en. https://doi.org/10.4060/cb4474en (2021).
World Health Organization. Vector-borne diseases. https://www.who.int/news-room/fact-sheets/detail/vector-borne-diseases (2020).
Corvalan, C. et al. Mental health and the global climate crisis. Epidemiol. Psychiatr. Sci. 31, e86 (2022).
Vicedo-Cabrera, A. M. et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat. Clim. Chang. 11, 492–500 (2021).
Ebi, K. L. et al. Using detection and attribution to quantify how climate change is affecting health. Health Affairs 39, 2168–2174 (2020).
World Health Organization. Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s. https://apps.who.int/iris/handle/10665/134014 (2014).
Jacobson, M. Z. et al. Low-cost solutions to global warming, air pollution, and energy insecurity for 145 countries. Energy Environ. Sci. 15, 3343–3359 (2022).
Intergovernmental Panel on Climate Change. in Climate Change 2022: Mitigation of Climate Change. Contribution of Working Group III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (eds. Shukla, P. R. et al.) (Cambridge Univ.Press, 2022).
Prüss-Üstün, A., Wolf, J., Corvalán, C. F., Bos, R. & Neira, M. P. Preventing Disease through Healthy Environments: a Global Assessment of the Burden of Disease from Environmental Risks. https://apps.who.int/iris/handle/10665/204585 (2016).
Hamilton, I. et al. The public health implications of the Paris Agreement: a modelling study. Lancet Planet. Health 5, e74–e83 (2021).
Markandya, A. et al. Health co-benefits from air pollution and mitigation costs of the Paris Agreement: a modelling study. Lancet Planet. Health 2, e126–e133 (2018).
World Health Organization. Health Benefits of Raising Ambition in Pakistan’s Nationally Determined Contribution: WHO Technical Report. https://apps.who.int/iris/handle/10665/347767 (2021).
Romanello, M. et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet 398, 1619–1662 (2021).
World Health Organization. Walking and Cycling: Latest Evidence to Support Policy-making and Practice. https://apps.who.int/iris/handle/10665/354589 (2022).
World Health Organization. Operational Framework for Building Climate Resilient Health Systems. https://apps.who.int/iris/handle/10665/189951 (2015).
World Health Organization. Declaration of Astana: Global Conference on Primary Health Care: Astana, Kazakhstan, 25 and 26 October 2018. https://apps.who.int/iris/handle/10665/328123 (2019).
Health Care Without Harm. Global Road Map for Health Care Decarbonization: a navigational tool for achieving zero emissions with climate resilience and health equity. Health Care Climate Action https://healthcareclimateaction.org/roadmap (2020).
World Health Organization. WHO Guidance for Climate Resilient and Environmentally Sustainable Health Care Facilities. https://apps.who.int/iris/handle/10665/335909 (2020).
World Health Organization & United Nations Children’s Fund (UNICEF). Progress on WASH in Health Care Facilities 2000–2021: Special Focus on WASH and Infection Prevention and Control https://apps.who.int/iris/handle/10665/366657 (2023).
World Health Organization. Energizing Health: Accelerating Electricity Access in Health-care Facilities. https://apps.who.int/iris/handle/10665/365588 (2023).
World Health Organization. Quality Criteria for Health National Adaptation Plans. https://apps.who.int/iris/handle/10665/339454 (2021).
World Health Organization. WHO Guidance to Protect Health from Climate Change through Health Adaptation Planning. https://apps.who.int/iris/handle/10665/137383 (2014).
Kotcher, J., Maibach, E., Montoro, M. & Hassol, S. J. How Americans respond to information about global warming’s health impacts: evidence from a national survey experiment. GeoHealth 2, 262–275 (2018).
Rossa-Roccor, V., Giang, A. & Kershaw, P. Framing climate change as a human health issue: enough to tip the scale in climate policy? Lancet Planet. Health 5, e553–e559 (2021).
Dasandi, N. et al. Positive, global, and health or environment framing bolsters public support for climate policies. Commun. Earth Environ. 3, 239 (2022).
Badullovich, N., Grant, W. J. & Colvin, R. M. Framing climate change for effective communication: a systematic map. Environ. Res. Lett. 15, 123002 (2020).
United Nations General Assembly. The Human Right to a Clean, Healthy and Sustainable Environment. https://digitallibrary.un.org/record/3983329?ln=en (2022).
Clemence, M. & Boyon, N. Doctors and Scientists are seen as the World’s most Trustworthy Professions. https://www.ipsos.com/en/global-trustworthiness-index-2022 (2022).
World Health Organization. Climate Change and Health Research: Current Trends, Gaps and Perspectives for the Future. https://apps.who.int/iris/handle/10665/353062 (2021).
World Health Organization. World Health Assembly, 61. Climate Change and Health. https://apps.who.int/iris/handle/10665/23547 (2008).
World Health Organization. Conceptual and Operational Framework for Building Climate Resilient and Low Carbon Health Systems (in the press).
World Health Organization. Climate Change Mitigation, Air Quality and Health (CLIMAQ-H). https://www.who.int/europe/tools-and-toolkits/climate-change-mitigation--air-quality-and-health-(climaq-h)
World Health Organization. Health Economic Assessment Tool (HEAT) for Walking and Cycling. https://www.who.int/tools/heat-for-walking-and-cycling
World Health Organization. Benefits of Action to Reduce Household Air Pollution Tool (BAR-HAP). https://www.who.int/tools/benefits-of-action-to-reduce-household-air-pollution-tool
International Association of National Public Health Institutes. Roadmap for Action on Health and Climate Change: Engaging and supporting national public health institutes as key climate actors. https://ianphi.org/news/2021/roadmap-climate-change.html (2022).
Acknowledgements
The authors thank C. Corvalan, A. Sena, E. V. Prats and A. Savage for contributing graphics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Kristie Ebi, Matthew Chersich and Sarah Whitmee for their contribution to the peer review of this work. Primary Handling Editor: Karen O’Leary, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Campbell-Lendrum, D., Neville, T., Schweizer, C. et al. Climate change and health: three grand challenges. Nat Med 29, 1631–1638 (2023). https://doi.org/10.1038/s41591-023-02438-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-023-02438-w
This article is cited by
-
A WHO-led global strategy to control greenhouse gas emissions: a call for action
Globalization and Health (2024)
-
Impact of extreme weather events on healthcare utilization and mortality in the United States
Nature Medicine (2024)
-
Building healthy populations
Nature Medicine (2023)
-
Spatiotemporal change of climate extremes under the projection of CMIP6 model analysis over Awash Basin, Ethiopia
Sustainable Water Resources Management (2023)