Abstract
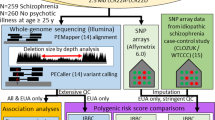
The 22q11.2 deletion syndrome (22q11DS) is associated with a 20–25% risk of schizophrenia. In a cohort of 962 individuals with 22q11DS, we examined the shared genetic basis between schizophrenia and schizophrenia-related early trajectory phenotypes: sub-threshold symptoms of psychosis, low baseline intellectual functioning and cognitive decline. We studied the association of these phenotypes with two polygenic scores, derived for schizophrenia and intelligence, and evaluated their use for individual risk prediction in 22q11DS. Polygenic scores were not only associated with schizophrenia and baseline intelligence quotient (IQ), respectively, but schizophrenia polygenic score was also significantly associated with cognitive (verbal IQ) decline and nominally associated with sub-threshold psychosis. Furthermore, in comparing the tail-end deciles of the schizophrenia and IQ polygenic score distributions, 33% versus 9% of individuals with 22q11DS had schizophrenia, and 63% versus 24% of individuals had intellectual disability. Collectively, these data show a shared genetic basis for schizophrenia and schizophrenia-related phenotypes and also highlight the future potential of polygenic scores for risk stratification among individuals with highly, but incompletely, penetrant genetic variants.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data sets (raw data) generated and/or analyzed during the current study are available through the National Institute of Mental Health Data Archive repository at https://nda.nih.gov/study.html?id=938, accession number 10.15154/1519190.
To construct the polygenic score for schizophrenia, we used results from the Schizophrenia Working Group of the Psychiatric Genomics Consortium24, specifically the ‘Full SNP Results’ file ckqny.scz2snpres.gz with md5 af7b9b521a196ce711d99060426fe01e, which is available after filling out an application as described at https://www.med.unc.edu/pgc/download-results/scz/.
To construct the polygenic score for fluid intelligence, we used results from the Neale lab, which are available at http://www.nealelab.is/blog/2017/7/19/rapid-gwas-of-thousands-of-phenotypes-for-337000-samples-in-the-uk-biobank, specifically the file fluid_intelligence.20016.assoc.tsv.gz with md5 685d4b5e2f35c82fe29d9d9ac6e35db4, which is available through their website, http://www.nealelab.is/uk-biobank, and is additionally mirrored at https://figshare.com/articles/dataset/fluid_intelligence_20016_assoc_tsv_gz_from_2017_Neale_lab_analysis/12746570.
Code availability
Bespoke analysis code for analyses downstream of genotype generation is available.
References
Sommer, I. E. et al. Early interventions in risk groups for schizophrenia: what are we waiting for? NPJ Schizophr. 2, 16003 (2016).
Reichenberg, A. et al. Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: a 30-year study. Am. J. Psychiatry 167, 160–169 (2010).
Bearden, C. E. et al. A prospective cohort study of childhood behavioral deviance and language abnormalities as predictors of adult schizophrenia. Schizophr/ Bull. 26, 395–410 (2000).
Rosso, I. M. et al. Childhood neuromotor dysfunction in schizophrenia patients and their unaffected siblings: a prospective cohort study. Schizophr. Bull. 26, 367–378 (2000).
Walker, E. F., Grimes, K. E., Davis, D. M. & Smith, A. J. Childhood precursors of schizophrenia: facial expressions of emotion. Am. J. Psychiatry 150, 1654–1660 (1993).
Dickson, H., Laurens, K. R., Cullen, A. E. & Hodgins, S. Meta-analyses of cognitive and motor function in youth aged 16 years and younger who subsequently develop schizophrenia. Psychol. Med. 42, 743–755 (2012).
Woodberry, K. A., Giuliano, A. J. & Seidman, L. J. Premorbid IQ in schizophrenia: a meta-analytic review. Am. J. Psychiatry 165, 579–587 (2008).
Mollon, J., David, A. S., Zammit, S., Lewis, G. & Reichenberg, A. Course of cognitive development from infancy to early adulthood in the psychosis spectrum. JAMA Psychiatry 75, 270–279 (2018).
Zammit, S. et al. A longitudinal study of premorbid IQ score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Arch. Gen. Psychiatry 61, 354–360 (2004).
Khandaker, G. M., Barnett, J. H., White, I. R. & Jones, P. B. A quantitative meta-analysis of population-based studies of premorbid intelligence and schizophrenia. Schizophr. Res. 132, 220–227 (2011).
Kahn, R. S. & Keefe, R. S. Schizophrenia is a cognitive illness: time for a change in focus. JAMA Psychiatry 70, 1107–1112 (2013).
MacCabe, J. H. et al. Decline in cognitive performance between ages 13 and 18 years and the risk for psychosis in adulthood: a Swedish longitudinal cohort study in males. JAMA Psychiatry 70, 261–270 (2013).
Meier, M. H. et al. Neuropsychological decline in schizophrenia from the premorbid to the postonset period: evidence from a population-representative longitudinal study. Am. J. Psychiatry 171, 91–101 (2014).
Lin, A. et al. Neurocognitive predictors of functional outcome two to 13 years after identification as ultra-high risk for psychosis. Schizophr. Res. 132, 1–7 (2011).
Kaymaz, N. et al. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol. Med. 42, 2239–2253 (2012).
Poulton, R. et al. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch. Gen. Psychiatry 57, 1053–1058 (2000).
Insel, T. R. Rethinking schizophrenia. Nature 468, 187–193 (2010).
Murphy, K. C., Jones, L. A. & Owen, M. J. High rates of schizophrenia in adults with velo-cardio-facial syndrome. Arch. Gen. Psychiatry 56, 940–945 (1999).
Bassett, A. S. & Chow, E. W. 22q11 deletion syndrome: a genetic subtype of schizophrenia. Biol. Psychiatry 46, 882–891 (1999).
Gur, R. E. et al. A neurogenetic model for the study of schizophrenia spectrum disorders: the International 22q11.2 Deletion Syndrome Brain Behavior Consortium. Mol. Psychiatry 22, 1664–1672 (2017).
Kates, W. R. et al. Trajectories of psychiatric diagnoses and medication usage in youth with 22q11.2 deletion syndrome: a 9-year longitudinal study. Psychol. Med. 49, 1914–1922 (2019).
Vorstman, J. A. et al. Cognitive decline preceding the onset of psychosis in patients with 22q11.2 deletion syndrome. JAMA Psychiatry 72, 377–385 (2015).
Pardinas, A. F. et al. Common schizophrenia alleles are enriched in mutation-intolerant genes and in regions under strong background selection. Nat. Genet. 50, 381–389 (2018).
Schizophrenia Working Group of the Psychiatric Genomics Consortium.Biological insights from 108 schizophrenia-associated genetic loci. Nature 511, 421–427 (2014).
Wray, N. R. et al. Research review: polygenic methods and their application to psychiatric traits. J. Child Psychol. Psychiatry 55, 1068–1087 (2014).
Davies, G. et al. Study of 300,486 individuals identifies 148 independent genetic loci influencing general cognitive function. Nat. Commun. 9, 2098 (2018).
Rietveld, C. A. et al. GWAS of 126,559 individuals identifies genetic variants associated with educational attainment. Science 340, 1467–1471 (2013).
Sugrue, L. P. & Desikan, R. S. What are polygenic scores and why are they important? JAMA 321, 1820–1821 (2019).
Fullerton, J. M. & Nurnberger, J. I. Polygenic risk scores in psychiatry: will they be useful for clinicians? F1000Res 8, F1000 Faculty Rev-1293 (2019).
Torkamani, A., Wineinger, N. E. & Topol, E. J. The personal and clinical utility of polygenic risk scores. Nat. Rev. Genet. 19, 581–590 (2018).
Kuchenbaecker, K. B. et al. Evaluation of polygenic risk scores for breast and ovarian cancer risk prediction in BRCA1 and BRCA2 mutation carriers. J. Natl Cancer Inst. 109, djw302 (2017).
Cleynen, I. et al. Genetic contributors to risk of schizophrenia in the presence of a 22q11.2 deletion. Mol. Psychiatry https://doi.org/10.1038/s41380-020-0654-3 (2020).
Marder, S. R. & Cannon, T. D. Schizophrenia. N. Engl. J. Med. 381, 1753–1761 (2019).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562, 203–209 (2018).
Miller, T. J. et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr. Bull. 29, 703–715 (2003).
Klaassen, P. et al. Explaining the variable penetrance of CNVs: parental intelligence modulates expression of intellectual impairment caused by the 22q11.2 deletion. Am. J. Med. Genet. B Neuropsychiatr. Genet. 171, 790–796 (2016).
Sieradzka, D. et al. Are genetic risk factors for psychosis also associated with dimension-specific psychotic experiences in adolescence? PLoS ONE 9, e94398 (2014).
Jones, H. J. et al. Phenotypic manifestation of genetic risk for schizophrenia during adolescence in the general population. JAMA Psychiatry 73, 221–228 (2016).
Jones, H. J. et al. Investigating the genetic architecture of general and specific psychopathology in adolescence. Transl. Psychiatry 8, 145 (2018).
Fuller, R. et al. Longitudinal assessment of premorbid cognitive functioning in patients with schizophrenia through examination of standardized scholastic test performance. Am. J. Psychiatry 159, 1183–1189 (2002).
van Oel, C. J., Sitskoorn, M. M., Cremer, M. P. & Kahn, R. S. School performance as a premorbid marker for schizophrenia: a twin study. Schizophr. Bull. 28, 401–414 (2002).
Duijff, S. N. et al. Cognitive development in children with 22q11.2 deletion syndrome. Br. J. Psychiatry 200, 462–468 (2012).
Chawner, S. et al. Childhood cognitive development in 22q11.2 deletion syndrome: case–control study. Br. J. Psychiatry 211, 223–230 (2017).
Trevethan, R. Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Front. Public Health 5, 307 (2017).
Bergen, S. E. et al. Joint contributions of rare copy number variants and common SNPs to risk for schizophrenia. Am. J. Psychiatry 176, 29–35 (2019).
Tansey, K. E. et al. Common alleles contribute to schizophrenia in CNV carriers. Mol. Psychiatry 21, 1085–1089 (2016).
Lecarpentier, J. et al. Prediction of breast and prostate cancer risks in male BRCA1 and BRCA2 mutation carriers using polygenic risk scores. J. Clin. Oncol. 35, 2240–2250 (2017).
Gibson, G. On the utilization of polygenic risk scores for therapeutic targeting. PLoS Genet. 15, e1008060 (2019).
Damask, A. et al. Patients with high genome-wide polygenic risk scores for coronary artery disease may receive greater clinical benefit from alirocumab treatment in the ODYSSEY OUTCOMES trial. Circulation 141, 624–636 (2020).
Perkins, D. O. et al. Polygenic risk score contribution to psychosis prediction in a target population of persons at clinical high risk. Am. J. Psychiatry 177, 155–163 (2020).
Fiksinski, A. M. et al. Understanding the pediatric psychiatric phenotype of 22q11.2 deletion syndrome. Am. J. Med. Genet. A 176, 2182–2191 (2018).
Martin, A. R. et al. Human demographic history impacts genetic risk prediction across diverse populations. Am. J. Hum. Genet. 100, 635–649 (2017).
Chelune, G. J., Naugle, R. I., Lüders, H., Sedlak, J. & Awad, I. A. Individual change after epilepsy surgery: practice effects and base-rate information. Neuropsychology 7, 41–52 (1993).
Vorstman, J. A. et al. MLPA: a rapid, reliable, and sensitive method for detection and analysis of abnormalities of 22q. Hum. Mutat. 27, 814–821 (2006).
Yung, A. R. et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust. N. Z. J. Psychiatry 39, 964–971 (2005).
Kaufman, J. et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 36, 980–988 (1997).
Purcell, S. et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. 81, 559–575 (2007).
Deary, I. J., Johnson, W. & Houlihan, L. M. Genetic foundations of human intelligence. Hum. Genet. 126, 215–232 (2009).
Spearman, C. ‘General Intelligence,’ objectively determined and measured. Am. J. Psychol. 15, 201–293 (1904).
Euesden, J., Lewis, C. M. & O’Reilly, P. F. PRSice: polygenic risk score software. Bioinformatics 31, 1466–1468 (2015).
Gazal, S. et al. Linkage disequilibrium-dependent architecture of human complex traits shows action of negative selection. Nat. Genet. 49, 1421–1427 (2017).
Acknowledgements
This study was supported by the National Institute of Mental Health (NIMH) International Consortium on Brain and Behavior in 22q11.2 Deletion Syndrome (U01MH101719, U01MH0101720, U01MH0101723, U01MH101722 and EU01MH101724); the Lap-Chee Tsui Fellowship for Research Excellence and the CIHR STAGE Fellowship (to R.W.D.); the Brain and Behavior Research Foundation (to J.A.S.V.; Young Investigator Award); NIMH R01MH085953 and 1U01MH119736-01 (to C.E.B.); NIH RO1 MH064824 (to W.K.); Wellcome Trust grant 102428/Z/13/Z (to N.W. and T.M.); Canadian Institutes of Health Research grants MOP-79518, MOP-89066, MOP-97800 and MOP-111238, a McLaughlin Centre Accelerator grant, the Canada Research Chairs program and Dalglish Chair (to A.S.B); the Academic Scholars Award from the Department of Psychiatry, University of Toronto and the O’Brien Scholars Fund (to E.B.); Fondecyt 1171014 and ACT 192064 (ANID-Chile) (to G.R.); Spanish Ministry of Science and Innovation, Instituto de Salud Carlos III (SAM16PE07CP1, PI16/02012, PI19/024), CIBERSAM, Madrid Regional Government (B2017/BMD-3740 AGES-CM-2), European Union Structural Funds, European Union Seventh Framework Program (FP7-HEALTH-2013-2.2.1-2-603196 Project PSYSCAN) and European Union H2020 Program under the Innovative Medicines Initiative 2 Joint Undertaking (grant agreement 115916, Project PRISM, and grant agreement 777394, Project AIMS-2-TRIALS), Fundación Familia Alonso and Fundación Alicia Koplowitz (to C.A); Innovative Medicines Initiative 2 Joint Undertaking (#777394 for the project AIMS-2-TRIALS), the NIHR Maudsley BRC (to D.M.); and Binational Science Foundation grant 2017369 (to R.E.G. and D.G.).
Author information
Authors and Affiliations
Consortia
Contributions
J.A.S.V., R.W.D., A.M.F. and C.E.B. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. R.W.D. and A.M.F. contributed equally to the study. Study concept and design: AIM II writing group: R.W.D., A.M.F., E.J.B., T.M., N.M.W., S.R.H., C.E.B. and J.A.S.V. Acquisition of data: M.J.O., M.v.d.B., D.G.M., C.A., J.A.S.V., A.M.F., S.N.D., S.E., M.S., M.J., M.A., S.V., V.S., S.R.H., E.W.C.C., D.M.M.-M., A.V., D.G., R.W., T.v.A., W.K., K.M.A., T.S., O.Y.O., A.S., R.E.G., C.E.B. and A.S.B. Analysis and interpretation of data: AIM II writing group: R.W.D., A.M.F., E.J.B., T.M., N.M.W., S.R.H., C.E.B. and J.A.S.V. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: R.W.D., E.J.B., T.M., N.M.W. and J.A.S.V.
Corresponding author
Ethics declarations
Competing interests
M.J.O. and M.v.d.B. report grants from Takeda Pharmaceuticals outside of the submitted work. C.A. has been a consultant to or has received honoraria or grants from Acadia, Ambrosseti, Gedeon Richter, Janssen Cilag, Lundbeck, Otsuka, Roche, Sage, Servier, Shire, Schering Plough, Sumitomo Dainippon Pharma, Sunovion and Takeda. D.G.M. has provided consultation to Roche. S.R.H. has provided consultation to Novartis. O.Y.O. is a collaborator in a Biomarin Pharmaceutical study. None of the other authors has financial disclosures.
Additional information
Peer review information Kate Gao and Joao Monteiro were the primary editors on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Relationship between polygenic scores and previously studied phenotypes.
Results for the binary SSD phenotype show per-individual values as well as summaries per group, where minimum and maximum values are directly observable from the plot, the box-plot centre is the median, the boxplot edges represent the 25th and 75th percentiles, and the whiskers represent the lesser of the distance to the minimum or maximum value, or 1.5 times the inter-quartile range. Results are shown for logistic regression of SSD on controls (N = 802) and linear regression for FSIQ (N = 720), for both PS_SZ (left panel) and PS_IQ (right panel). P-values are reported from regression analyses and are two sided and are not corrected for multiple testing.
Extended Data Fig. 2 Inferred contribution of controls and future SSD cases given PS SZ.
Shown on the y-axis are group means of PS_SZ, on the x-axis the fraction of controls. For SDD and controls the fractions of controls were taken as 0 and 1, respectively (open circles). For subthreshold psychosis and putative controls they were inferred through the observed PS-SZ values for each group, using linear interpolation based on fitting a straight line between SSD and control values (red circles). Confidence intervals are shown for the group mean values for subthreshold psychosis and putative controls, as the mean plus or minus 1.96 times the standard error, and above and below these confidence intervals are the inferred fraction of controls this would represent. The observed PS_SZ in the subthreshold group is consistent with a scenario in which 86% (95% CI 56 - 100%) of individuals who had subthreshold psychotic symptoms at the time of the assessment for this study would subsequently transition to SSD, a proportion inconsistent with known rates of SSD in 22q11DS.
Supplementary information
Supplementary Information
Supplementary Tables 1–6 and Supplementary Figs. 1–8.
Rights and permissions
About this article
Cite this article
Davies, R.W., Fiksinski, A.M., Breetvelt, E.J. et al. Using common genetic variation to examine phenotypic expression and risk prediction in 22q11.2 deletion syndrome. Nat Med 26, 1912–1918 (2020). https://doi.org/10.1038/s41591-020-1103-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-1103-1
This article is cited by
-
Genetic modifiers of rare variants in monogenic developmental disorder loci
Nature Genetics (2024)
-
Polygenic risk for triglyceride levels in the presence of a high impact rare variant
BMC Medical Genomics (2023)
-
A genetics-first approach to understanding autism and schizophrenia spectrum disorders: the 22q11.2 deletion syndrome
Molecular Psychiatry (2023)
-
The contribution of copy number variants to psychiatric symptoms and cognitive ability
Molecular Psychiatry (2023)
-
The molecular pathology of schizophrenia: an overview of existing knowledge and new directions for future research
Molecular Psychiatry (2023)