Abstract
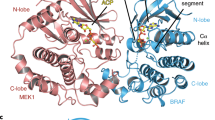
Activating BRAF mutants and fusions signal as RAS-independent constitutively active dimers with the exception of BRAF V600 mutant alleles which can function as active monomers1. Current RAF inhibitors are monomer selective, they potently inhibit BRAF V600 monomers but their inhibition of RAF dimers is limited by induction of negative cooperativity when bound to one site in the dimer1,2,3. Moreover, acquired resistance to these drugs is usually due to molecular lesions that cause V600 mutants to dimerize4,5,6,7,8. We show here that PLX8394, a new RAF inhibitor9, inhibits ERK signaling by specifically disrupting BRAF-containing dimers, including BRAF homodimers and BRAF–CRAF heterodimers, but not CRAF homodimers or ARAF-containing dimers. Differences in the amino acid residues in the amino (N)-terminal portion of the kinase domain of RAF isoforms are responsible for this differential vulnerability. As a BRAF-specific dimer breaker, PLX8394 selectively inhibits ERK signaling in tumors driven by dimeric BRAF mutants, including BRAF fusions and splice variants as well as BRAF V600 monomers, but spares RAF function in normal cells in which CRAF homodimers can drive signaling. Our work suggests that drugs with these properties will be safe and useful for treating tumors driven by activating BRAF mutants or fusions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Yao, Z. et al. BRAF mutants evade ERK-dependent feedback by different mechanisms that determine their sensitivity to pharmacologic inhibition. Cancer Cell 28, 370–383 (2015).
Karoulia, Z. et al. An integrated model of RAF inhibitor action predicts inhibitor activity against oncogenic BRAF signaling. Cancer Cell 30, 485–498 (2016).
Yang, H. et al. RG7204 (PLX4032), a selective BRAFV600E inhibitor, displays potent antitumor activity in preclinical melanoma models. Cancer Res. 70, 5518–5527 (2010).
Nazarian, R. et al. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature 468, 973–977 (2010).
Poulikakos, P. I. et al. RAF inhibitor resistance is mediated by dimerization of aberrantly spliced BRAF(V600E). Nature 480, 387–390 (2011).
Poulikakos, P. I., Zhang, C., Bollag, G., Shokat, K. M. & Rosen, N. RAF inhibitors transactivate RAF dimers and ERK signalling in cells with wild-type BRAF. Nature 464, 427–430 (2010).
Shi, H. et al. Melanoma whole-exome sequencing identifies (V600E)B-RAF amplification-mediated acquired B-RAF inhibitor resistance. Nat. Commun. 3, 724 (2012).
Yaeger, R. et al. Mechanisms of acquired resistance to BRAF V600E inhibition in colon cancers converge on RAF dimerization and are sensitive to its inhibition. Cancer Res. 77, 6513–6523 (2017).
Zhang, C. et al. RAF inhibitors that evade paradoxical MAPK pathway activation. Nature 526, 583–586 (2015).
Basile, K. J., Le, K., Hartsough, E. J. & Aplin, A. E. Inhibition of mutant BRAF splice variant signaling by next-generation, selective RAF inhibitors. Pigment Cell Melanoma Res. 27, 479–484 (2014).
Jain, P. et al. CRAF gene fusions in pediatric low-grade gliomas define a distinct drug response based on dimerization profiles. Oncogene 36, 6348–6358 (2017).
Okimoto, R. A. et al. Preclinical efficacy of a RAF inhibitor that evades paradoxical MAPK pathway activation in protein kinase BRAF-mutant lung cancer. Proc. Natl Acad. Sci. USA 113, 13456–13461 (2016).
Sievert, A. J. et al. Paradoxical activation and RAF inhibitor resistance of BRAF protein kinase fusions characterizing pediatric astrocytomas. Proc. Natl Acad. Sci. USA 110, 5957–5962 (2013).
Nakamura, A. et al. Antitumor activity of the selective pan-RAF inhibitor TAK-632 in BRAF inhibitor-resistant melanoma. Cancer Res. 73, 7043–7055 (2013).
Peng, S. B. et al. Inhibition of RAF isoforms and active dimers by LY3009120 leads to anti-tumor activities in RAS or BRAF mutant cancers. Cancer Cell. 28, 384–398 (2015).
Fabian, J. R., Daar, I. O. & Morrison, D. K. Critical tyrosine residues regulate the enzymatic and biological activity of Raf-1 kinase. Mol. Cell. Biol. 13, 7170–7179 (1993).
Stokoe, D. & McCormick, F. Activation of c-Raf-1 by Ras and Src through different mechanisms: activation in vivo and in vitro. EMBO J. 16, 2384–2396 (1997).
Takahashi, M., Li, Y., Dillon, T. J., Kariya, Y. & Stork, P. J. S. Phosphorylation of the C-Raf N-region promotes Raf dimerization. Mol. Cell. Biol. 37, e00132-17 (2017).
Chong, H., Lee, J. & Guan, K. L. Positive and negative regulation of Raf kinase activity and function by phosphorylation. EMBO J. 20, 3716–3727 (2001).
Yao, Z. et al. Tumours with class 3 BRAF mutants are sensitive to the inhibition of activated RAS. Nature 548, 234–238 (2017).
Nieto, P. et al. A Braf kinase-inactive mutant induces lung adenocarcinoma. Nature 548, 239–243 (2017).
Heidorn, S. J. et al. Kinase-dead BRAF and oncogenic RAS cooperate to drive tumor progression through CRAF. Cell 140, 209–221 (2010).
Karoulia, Z., Gavathiotis, E. & Poulikakos, P. I. New perspectives for targeting RAF kinase in human cancer. Nat. Rev. Cancer 17, 676–691 (2017).
Cheng, D. T. et al. Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT): a hybridization capture-based next-generation sequencing clinical assay for solid tumor molecular oncology. J. Mol. Diagn. 17, 251–264 (2015).
Acknowledgements
We are grateful to L.M. Desrochers, I. Mellinghoff, and A. Ventura for useful discussions. We thank S. Lowe for the vectors of the retrovirus-based inducible expression system. This research was supported by grants (to N.R.) from the National Institutes of Health (NIH) (P01 CA129243; R35 CA210085); the Melanoma Research Alliance (237059 and 348724); the Commonwealth Foundation for Cancer Research and the Center for Experimental Therapeutics at Memorial Sloan Kettering Cancer Center; and the Stand Up To Cancer – American Cancer Society Lung Cancer Dream Team Translational Research Grant (SU2C-AACR-DT17-15). Support was also received from the NIH MSKCC Cancer Center Support Grant P30 CA008748 and T32 CA009207 (to J.T.). Additional funding was provided by a Conquer Cancer Foundation of the American Society of Clinical Oncology Young Investigator Award (to J.T.) and Career Development Award (to R.Y.). We would like to acknowledge the support of the Arlene and Joseph Taub Foundation and of P. and T. McInerney, without whom this work would not have been possible. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was also supported by grants from the Spanish Ministry of Economy and Competitiveness (SAF2011-30173 and SAF2014-59864-R) (to M.B.). M.B. is the recipient of an endowed chair from the AXA Research Fund.
Author information
Authors and Affiliations
Contributions
Z.Y. and N.R. conceived the project and designed the experiments. Z.Y. and N.R. wrote the manuscript. Y.G., W.S., R.Y., C.Z., M.B., D.M.H., and G.B. provided critical revisions of the manuscript. Z.Y., Y.G., W.S., R.Y., J.T., N.N., Y.Z., C.Z., A.R., A.T., N.M.T., R.M., N.A.O., H.Z., Q.C., B.Q., E.d.S., and D.M.H. established the in vitro and in vivo experimental systems, performed the laboratory experiments, and analyzed the results.
Corresponding author
Ethics declarations
Competing interests
N.R. is on the scientific advisory board (SAB) and receives research funding from Chugai, on the SAB and owns equity in Beigene, and Fortress. N.R. is also on the SAB of Daiichi-Sankyo, Astra-Zeneca-MedImmune, and F-Prime, and is a past SAB member of Millenium-Takeda, Kadmon, Kura, and Araxes. N.R. is a consultant to Novartis, Boehringer Ingelheim, Tarveda, and Foresight and consulted in the last three years with Eli Lilly, Merrimack, Kura Oncology, Araxes, and Kadman. N.R. owns equity in ZaiLab, Kura Oncology, Araxes, and Kadman. N.R. collaborates with Plexxikon. R.Y. has received research support from Array BioPharma, Genentech, GlaxoSmithKline, and Norvatis; received travel expenses from Array BioPharma; and served on the advisory board for GlaxoSmithKline. D.M.H. has consulted for Atara Biotherapeutics, Chugai Pharma, CytomX Therapeutics, Boehringer Ingelheim, AstraZeneca, Pfizer, Bayer, Debiopharm Group, and Genetech and has received research funding from AstraZeneca, Puma Biotechnology, and Loxo Oncology. Y.Z., C.Z., A.R., and G.B. are employees of Plexxikon Inc.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–15 and Supplementary Table 1–4
Rights and permissions
About this article
Cite this article
Yao, Z., Gao, Y., Su, W. et al. RAF inhibitor PLX8394 selectively disrupts BRAF dimers and RAS-independent BRAF-mutant-driven signaling. Nat Med 25, 284–291 (2019). https://doi.org/10.1038/s41591-018-0274-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-018-0274-5
This article is cited by
-
BRAF — a tumour-agnostic drug target with lineage-specific dependencies
Nature Reviews Clinical Oncology (2024)
-
Combinatorial strategies to target RAS-driven cancers
Nature Reviews Cancer (2024)
-
Disruption of the pro-oncogenic c-RAF–PDE8A complex represents a differentiated approach to treating KRAS–c-RAF dependent PDAC
Scientific Reports (2024)
-
Mcl-1 mediates intrinsic resistance to RAF inhibitors in mutant BRAF papillary thyroid carcinoma
Cell Death Discovery (2024)
-
BRAFV600E-mutant metastatic NSCLC: disease overview and treatment landscape
npj Precision Oncology (2024)