Abstract
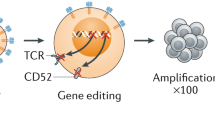
Engineered T cells are effective therapies against a range of malignancies, but current approaches rely on autologous T cells, which are difficult and expensive to manufacture. Efforts to develop potent allogeneic T cells that are not rejected by the recipient’s immune system require abrogating both T- and natural killer (NK)-cell responses, which eliminate foreign cells through various mechanisms. In the present study, we engineered a receptor that mediates deletion of activated host T and NK cells, preventing rejection of allogeneic T cells. Our alloimmune defense receptor (ADR) selectively recognizes 4-1BB, a cell surface receptor temporarily upregulated by activated lymphocytes. ADR-expressing T cells resist cellular rejection by targeting alloreactive lymphocytes in vitro and in vivo, while sparing resting lymphocytes. Cells co-expressing chimeric antigen receptors and ADRs persisted in mice and produced sustained tumor eradication in two mouse models of allogeneic T-cell therapy of hematopoietic and solid cancers. This approach enables generation of rejection-resistant, ‘off-the-shelf’, allogeneic T-cell products to produce long-term therapeutic benefit in immunocompetent recipients.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All data generated for this manuscript will be made available upon reasonable request to the corresponding author. Source data are provided with this paper.
References
June, C. H. & Sadelain, M. Chimeric antigen receptor therapy. N. Engl. J. Med. 379, 64–73 (2018).
Papadopoulou, A. et al. Activity of broad-spectrum T cells as treatment for AdV, EBV, CMV, BKV, and HHV6 infections after HSCT. Sci. Transl. Med. 6, 242ra83 (2014).
Turtle, C. J. et al. Immunotherapy of non-Hodgkin’s lymphoma with a defined ratio of CD8+ and CD4+ CD19-specific chimeric antigen receptor–modified T cells. Sci. Transl. Med. 8, 355ra116–355ra116 (2016).
Graham, C. et al. Allogeneic CAR-T cells: more than ease of access? Cells 7, 155 (2018).
Torikai, H. et al. A foundation for universal T-cell based immunotherapy: T cells engineered to express a CD19-specific chimeric-antigen-receptor and eliminate expression of endogenous TCR. Blood 119, 5697–5705 (2012).
Qasim, W. et al. Molecular remission of infant B-ALL after infusion of universal TALEN gene-edited CAR T cells. Sci. Transl. Med. 9, eaaj2013 (2017).
Ren, J. et al. Multiplex genome editing to generate universal CAR T cells resistant to PD1 inhibition. Clin. Cancer Res. 23, 2255–2266 (2017).
Eyquem, J. et al. Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature 543, 113–117 (2017).
Poirot, L. et al. Multiplex genome-edited T-cell manufacturing platform for ‘off-the-shelf’ adoptive T-cell immunotherapies. Cancer Res. 75, 3853–3864 (2015).
Tzannou, I. et al. Off-the-shelf virus-specific T cells to treat BK virus, human herpesvirus 6, cytomegalovirus, Epstein–Barr virus, and adenovirus infections after allogeneic hematopoietic stem-cell transplantation. J. Clin. Oncol. 35, 3547–3557 (2017).
Leen, A. M. et al. Multicenter study of banked third-party virus-specific T cells to treat severe viral infections after hematopoietic stem cell transplantation. Blood 121, 5113–5123 (2013).
Melenhorst, J. J. et al. Allogeneic virus-specific T cells with HLA alloreactivity do not produce GVHD in human subjects. Blood 116, 4700–4702 (2010).
Watts, T. H. TNF/TNFR family members in costimulation of T cell responses. Annu. Rev. Immunol. 23, 23–68 (2005).
Elliott, T. J. & Eisen, H. N. Allorecognition of purified major histocompatibility complex glycoproteins by cytotoxic T lymphocytes. Proc. Natl Acad. Sci. USA 85, 2728–2732 (1988).
Ciccone, E. et al. Evidence of a natural killer (NK) cell repertoire for (allo) antigen recognition: definition of five distinct NK-determined allospecificities in humans. J. Exp. Med. 175, 709–718 (1992).
Ruggeri, L. et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 295, 2097–2100 (2002).
Colonna, M., Brooks, E., Falco, M., Ferrara, G. & Strominger, J. Generation of allospecific natural killer cells by stimulation across a polymorphism of HLA-C. Science 260, 1121–1124 (1993).
Torikai, H. et al. Toward eliminating HLA class I expression to generate universal cells from allogeneic donors. Blood 122, 1341–1349 (2013).
Storkus, W. J., Howell, D. N., Salter, R. D., Dawson, J. R. & Cresswell, P. NK susceptibility varies inversely with target cell class I HLA antigen expression. J. Immunol. 138, 1657–1659 (1987).
Brehm, M. A. et al. Lack of acute xenogeneic graft-versus-host disease, but retention of T-cell function following engraftment of human peripheral blood mononuclear cells in NSG mice deficient in MHC class I and II expression. FASEB J. 33, 3137–3151 (2019).
Tian, G. et al. CD62L+ NKT cells have prolonged persistence and antitumor activity in vivo. J. Clin. Invest. 126, 2341–2355 (2016).
Lamers, C. H. J. et al. Immune responses to transgene and retroviral vector in patients treated with ex vivo-engineered T cells. Blood 117, 72–82 (2011).
Maus, M. V. et al. T cells expressing chimeric antigen receptors can cause anaphylaxis in humans. Cancer Immunol. Res. 1, 26–31 (2013).
Sommermeyer, D. et al. Fully human CD19-specific chimeric antigen receptors for T-cell therapy. Leukemia 31, 2191–2199 (2017).
Gornalusse, G. G. et al. HLA-E-expressing pluripotent stem cells escape allogeneic responses and lysis by NK cells. Nat. Biotechnol. 35, 765–772 (2017).
Braud, V. M. et al. HLA-E binds to natural killer cell receptors CD94/NKG2A, B and C. Nature 391, 795–799 (1998).
Lee, N. et al. HLA-E is a major ligand for the natural killer inhibitory receptor CD94/NKG2A. Proc. Natl Acad. Sci. USA 95, 5199–5204 (1998).
Lieto, L. D., Maasho, K., West, D., Borrego, F. & Coligan, J. E. The human CD94 gene encodes multiple, expressible transcripts including a new partner of NKG2A/B. Genes Immun. 7, 36–43 (2006).
Schwarz, H., Valbracht, J., Tuckwell, J., von Kempis, J. & Lotz, M. ILA, the human 4-1BB homologue, is inducible in lymphoid and other cell lineages. Blood 85, 1043–1052 (1995).
Zhang, X. et al. CD137 promotes proliferation and survival of human B cells. J. Immunol. 184, 787–795 (2010).
Pauly, S., Broll, K., Wittmann, M., Giegerich, G. & Schwarz, H. CD137 is expressed by follicular dendritic cells and costimulates B lymphocyte activation in germinal centers. J. Leukoc. Biol. 72, 35–42 (2002).
Alfaro, C. et al. Functional expression of CD137 (4-1BB) on T helper follicular cells. Oncoimmunology 4, e1054597 (2015).
Heinisch, I. V. W. M., Bizer, C., Volgger, W. & Simon, H.-U. Functional CD137 receptors are expressed by eosinophils from patients with IgE-mediated allergic responses but not by eosinophils from patients with non–IgE-mediated eosinophilic disorders☆. J. Allergy Clin. Immunol. 108, 21–28 (2001).
Nakajima, T. et al. Marked increase in CC chemokine gene expression in both human and mouse mast cell transcriptomes following Fcepsilon receptor I cross-linking: an interspecies comparison. Blood 100, 3861–3868 (2002).
Sallusto, F., Lenig, D., Förster, R., Lipp, M. & Lanzavecchia, A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature 401, 708–712 (1999).
Cheuk, S. et al. CD49a expression defines tissue-resident CD8+ T cells poised for cytotoxic function in human skin. Immunity 46, 287–300 (2017).
Casey, K. A. et al. Antigen-independent differentiation and maintenance of effector-like resident memory T cells in tissues. J. Immunol. 188, 4866–4875 (2012).
Ramos, C. A. et al. Clinical and immunological responses after CD30-specific chimeric antigen receptor-redirected lymphocytes. J. Clin. Invest. 127, 3462–3471 (2017).
Ruella, M. et al. Induction of resistance to chimeric antigen receptor T cell therapy by transduction of a single leukemic B cell. Nat. Med. 24, 1499–1503 (2018).
Zhao, Z. et al. Structural design of engineered costimulation determines tumor rejection kinetics and persistence of CAR T Cells. Cancer Cell 28, 415–428 (2015).
Menk, A. V. et al. 4-1BB costimulation induces T cell mitochondrial function and biogenesis enabling cancer immunotherapeutic responses. J. Exp. Med. 215, 1091–1100 (2018).
Stephan, M. T. et al. T cell-encoded CD80 and 4-1BBL induce auto- and transcostimulation, resulting in potent tumor rejection. Nat. Med. 13, 1440–1449 (2007).
Mamonkin, M. et al. Reversible transgene expression reduces fratricide and permits 4-1BB costimulation of CAR T cells directed to T-cell malignancies. Cancer Immunol. Res. 6, 47–58 (2018).
Mamonkin, M., Rouce, R. H., Tashiro, H. & Brenner, M. K. A T-cell-directed chimeric antigen receptor for the selective treatment of T-cell malignancies. Blood 126, 983–992 (2015).
Gomes-Silva, D. et al. CD7-edited T cells expressing a CD7-specific CAR for the therapy of T-cell malignancies. Blood 130, 285–296 (2017).
Acknowledgements
The authors thank the Metelitsa lab for providing the CHLA255-GFP.FFluc cell line; T. Sauer, S. Sharma, N. Mehta in the C. Rooney lab for the K562-CS cell line, LCLs, β2m-specific sgRNA and GD2.BBz CAR construct; P. Castro and the Baylor College of Medicine Pathology & Histology Core for immunohistochemistry and H&E staining of tissue microarray slides; and C. Gillespie for editing the manuscript. This project was supported by the Leukemia and Lymphoma Society Translational Research Award no. 6566, NIH NCI SPORE in Lymphoma 5P50CA126752, SU2C/AACR 604817 Meg Vosburg T cell Lymphoma Dream Team, Gloria Levin Fund and CPRIT Award nos. RP180810 and RP150611. Stand Up To Cancer is a program of the Entertainment Industry Foundation administered by the American Association for Cancer Research. We also thank the Dan L. Duncan Comprehensive Cancer Center for the support of their shared resources (P30 CA125123).
Author information
Authors and Affiliations
Contributions
F.M. designed and performed experiments, analyzed and interpreted the data, and wrote the manuscript. N.W. and M.K.M. designed and performed experiments and analyzed the data. M.J.H. evaluated the tissue microarray slides. M.S. contributed to vector cloning and in vivo experiments. D.S. established the CD3 gene editing platform. T.S., E.A., P.A.A. and R.M. performed experiments and collected data. D.Q. gave advice on the MLR assay design. H.E.H. advised on the study and edited the manuscript. M.K.B. provided feedback, designed experiments and edited teh manuscript. M.M. conceptualized, directed and funded the study, designed ADR constructs, designed experiments, analyzed and interpreted the data, and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
H.E.H. is co-founder with equity: Allovir, Marker Therapeutics; advisory boards: Gilead, Tessa Therapeutics, Novartis, PACT Pharma, Kiadis Pharma; research funding: Tessa Therapeutics, Cell Medica. M.K.B. is co-founder with equity: Allovir, Marker Therapeutics, Tessa Therapeutics; advisory boards: Tessa Therapeutics, Unum, Allogene. D.Q.’s research funding: Tessa Therapeutics. M.M., F.M. and M.K.B. are co-inventors on a patent related to ADRs and methods of their use, licensed to Fate Therapeutics. All other authors report no relevant financial/nonfinancial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information
Supplementary Figs. 1-13.
Source data
Source Data Fig. 2
Statistical source data for selected panels.
Source Data Fig. 3
Statistical source data for selected panels.
Source Data Fig. 4
Statistical source data for selected panels.
Rights and permissions
About this article
Cite this article
Mo, F., Watanabe, N., McKenna, M.K. et al. Engineered off-the-shelf therapeutic T cells resist host immune rejection. Nat Biotechnol 39, 56–63 (2021). https://doi.org/10.1038/s41587-020-0601-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41587-020-0601-5
This article is cited by
-
New cell sources for CAR-based immunotherapy
Biomarker Research (2023)
-
Cyclosporine A-resistant CAR-T cells mediate antitumour immunity in the presence of allogeneic cells
Nature Communications (2023)
-
Double-edged sword: γδ T cells in mucosal homeostasis and disease
Experimental & Molecular Medicine (2023)
-
Mechanisms of resistance to chimeric antigen receptor-T cells in haematological malignancies
Nature Reviews Drug Discovery (2023)
-
Synthetic Biology Technologies And Genetically Engineering Strategies For Enhanced Cell Therapeutics
Stem Cell Reviews and Reports (2023)