Abstract
Less than 30% of people in Africa received a dose of the COVID-19 vaccine even 18 months after vaccine development1. Here, motivated by the observation that residents of remote, rural areas of Sierra Leone faced severe access difficulties2, we conducted an intervention with last-mile delivery of doses and health professionals to the most inaccessible areas, along with community mobilization. A cluster randomized controlled trial in 150 communities showed that this intervention with mobile vaccination teams increased the immunization rate by about 26 percentage points within 48–72 h. Moreover, auxiliary populations visited our community vaccination points, which more than doubled the number of inoculations administered. The additional people vaccinated per intervention site translated to an implementation cost of US $33 per person vaccinated. Transportation to reach remote villages accounted for a large share of total intervention costs. Therefore, bundling multiple maternal and child health interventions in the same visit would further reduce costs per person treated. Current research on vaccine delivery maintains a large focus on individual behavioural issues such as hesitancy. Our study demonstrates that prioritizing mobile services to overcome access difficulties faced by remote populations in developing countries can generate increased returns in terms of uptake of health services3.
Similar content being viewed by others
Main
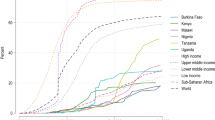
By 10 March 2022, more than a year after COVID-19 vaccines arrived on the market, 80% of the populations living in high-income countries had received at least one dose compared with only 15% of the people in low-income countries. As of 20 November 2023, only 33% of the population in Africa had received at least the first dose of a COVID-19 vaccine1. Low rates of vaccination keep many countries in Africa vulnerable to the threat of disease recurrence and a renewed possibility of costly lockdowns capable of undermining employment, income generation and food security4. Low vaccination coverage also raises the hazard of new subvariants emerging that puts the entire world at risk5.
To understand why vaccination rates remain low, we assembled data on vaccination beliefs, hesitancy and access from several countries in late 2021 (ref. 6). Nationally representative data from Sierra Leone revealed that obtaining access to a COVID-19 vaccine required the average person in Sierra Leone to travel three and a half hours each way to the nearest vaccination centre at a cost that exceeds 1 week of wages2. This finding motivated the design of an intervention we implemented in March–April 2022 in partnership with the Sierra Leone Ministry of Health and Sanitation (MoHS) and the international non-governmental organization (NGO) Concern Worldwide. The primary aim of this intervention was to take vaccine doses and nurses to administer vaccines to remote, rural communities, preceded by seeking permission and community mobilization. A cluster randomized controlled trial (RCT) across 150 communities showed that the vaccination rate in treatment villages increased by about 26 percentage points in response to this intervention. In addition, large numbers of people from neighbouring communities showed up to receive vaccines at our temporary clinics. In villages that received the intervention, the average number of people vaccinated increased from about 9 people pre-intervention to 55 people within the intervention period of about 2–3 days, at a cost of $33 per person vaccinated.
These results suggest that low vaccination rates are related to deficiencies in access and that a cost-effective intervention is capable of overcoming that deficiency. The Sierra Leone MoHS operates a network of peripheral health units (PHUs), but a significant proportion of people in Sierra Leone—particularly those in inaccessible rural areas—live outside the 5-km catchment area of any PHU. As such, interventions such as the one we conducted in communities outside PHU catchment areas are necessary to ease the burden of access.
This result carries broader implications for global public health. The child mortality rate in Sierra Leone was 10.5% in 2021 (ref. 7), as many children die from preventable diseases that immunizations and other simple interventions could address. The situation is almost as acute in neighbouring Guinea and Liberia. By contrast, efforts at community engagement in Bangladesh, including simple acts of taking maternal and child health interventions to rural populations, contributed to increasing the infant vaccination rate from 1% in the early 1980s to more than 70% within 10 years8. Populations in remote areas of West Africa have proven more challenging to reach, but our intervention with COVID-19 vaccination serves as a proof of concept that it may be similarly possible to tackle the high rates of child mortality in West Africa by cost-effectively delivering simple health interventions to rural populations. In fact, bundling multiple health interventions together would further reduce the cost of delivery per person treated given the high fixed transportation costs of reaching each remote community.
These results are relevant for donors and international pharmaceutical companies who have cited cases of unused vaccines in Africa reaching expiration dates9 to explain why low-income countries did not receive adequate supplies of vaccine doses early in the pandemic10,11. Our implementation efforts taught us that the Sierra Leone MoHS needed to engage in ‘learning by doing’ to develop new distribution systems to reach remote populations with those doses. But it is a catch-22 situation: the required experimentation is only possible once a steady and dependable supply of vaccine doses is made available.
To benchmark our results against other vaccination strategies, we conducted a comprehensive literature review that identified 235 distinct interventions in 144 RCT studies that used information, nudges, community engagement, social signalling and non-financial and financial incentives to increase vaccination rates across many settings around the world. More than one third of these interventions produced null effects. Here our access intervention produced a larger percentage point effect size than 223 (95%) of the treatments reviewed. This result is not surprising because vaccinating the first 50% of the population in remote parts of low-income countries requires solving the fundamental problem of access, which we address. Once access issues are addressed, misinformation and hesitancy may loom large in the effort to vaccinate the last 20% of the population of high-income countries who stubbornly hold out, and this is the target of the bulk of the literature. Even in high-income settings, access constraints were relevant in the earliest phase of COVID-19 vaccine delivery12.
This finding implies that we may need to further emphasize access interventions if we are to increase the global vaccination rate and improve vaccine equity. Guidelines from the Centers for Disease Control and the World Health Organization (WHO) highlight the importance of ‘bringing services closer to the people’, and our RCT is a proof of concept that such approaches can increase vaccination rates rapidly and cost-effectively, even under difficult circumstances in the most remote communities. The mobile delivery concept has produced large effects in HIV testing13. Rigorously demonstrating effectiveness in vaccine delivery is crucial given the persistent low rates of vaccination in low-income countries. Our literature review revealed thousands of studies on vaccine hesitancy and misinformation, but only a handful on vaccine supply and access, with a clear bias in favour of high-income contexts. This imbalance is emblematic of a wider debate on the relative importance of individual-specific behavioural factors versus systemic deficiencies in limiting the diffusion of welfare-improving technologies among low-income populations14. Prominent behavioural scientists have recently acknowledged our excessive focus on individual behavioural peculiarities (‘i-frame’) at the expense of systemic solutions (‘s-frame’)15.
Context and research design
We conducted a pre-registered cluster RCT in 150 rural villages in Sierra Leone. We first mapped all PHUs where the MoHS was offering COVID-19 vaccines together with the catchment areas of a PHU, which is defined by the MoHS as the 5-mile (about 8-km) radius around each PHU. We then compiled a list of all communities situated outside these catchment areas and randomly selected 150 communities from this list. Overall, 100 communities were randomly assigned to receive the intervention and the other 50 were assigned to the control group. During March and April 2022, a research team first visited all communities to conduct a village population listing and a baseline survey. Immediately afterwards, mobile vaccination teams coordinated by the MoHS visited the 100 villages assigned to the intervention for 2–3 days per village (Supplementary Fig. 1).
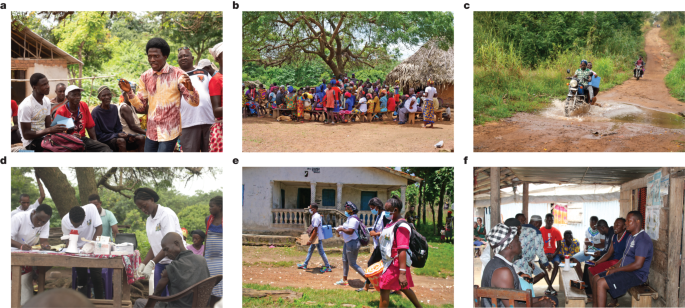
On the first day of the intervention, a social mobilization team—trained and supervised by the MoHS—organized a conversation with all village leaders, including the town chief, mammy queen, town elders, the youth leaders and religious leaders, and any other important stakeholders including the paramount and section chiefs if they were available (step 1; Fig. 1a). Members of the social mobilization team we employed were previously vetted and trained by ministry staff and commonly engaged for short-term projects such as vaccination campaigns. This cadre is referred to as MoHS volunteers because they are paid per-diem against project work and not a regular salary per a civil servant. The mobilization team explained the purpose of the visit, answered questions about the available vaccines and asked leaders for their cooperation in encouraging eligible community members to take the COVID-19 vaccine.
a–f, Representative photographs of the steps taken by the vaccination teams in each village for the mobile vaccination clinic. a, Step 1. A social mobilization team from the MoHS organizes a meeting with village leaders. b, Step 2. Social mobilizers convene a community meeting to talk directly with all village residents about vaccine efficacy and safety, the importance of getting vaccinated, address villagers’ questions and concerns, and the location and timing of the mobile vaccination site. c, Step 3. MoHS staff bring vaccine doses and staff to the village. d, Step 4. MoHS staff set up a 48–72 h mobile vaccine clinic in a central location in the village. e, Step 5a. Social mobilizers provide vaccine information to community members in private during door-to-door visits. f, Step 5b. Social mobilizers target social groups at fixed spots in and around the villages. Photographs in a–f reproduced with permission from Concern Worldwide.
Social mobilizers then asked leaders to convene a community meeting that same evening (when people return home from farms) to allow mobilizers to talk directly with all village residents about vaccine efficacy and safety, the importance of getting vaccinated, and to address villagers’ questions and concerns. This process (step 2; Fig. 1b) ended with social mobilizers explaining the location and timing of the mobile vaccination site that they were about to set up.
Vaccine doses, nurses to administer vaccines and MoHS staff who could register the vaccinated were brought into the community either the same evening or early the next morning (step 3; Fig. 1c). The vaccine doses and staff often travelled on motorbikes or on boats given the difficult terrain they had to traverse to reach these remote communities. Once the team was in place, the temporary vaccination site started operating in a central location in the village (step 4; Fig. 1d). Villages in our sample were small, with houses closely clustered; therefore, walking distances to the vaccination site were short. The vaccination site remained operational from sunrise to sunset over the next 2–3 days, which enabled people to visit when convenient. Nurses and registration staff remained stationed at the temporary clinic while the mobilizers continued to provide vaccine information to various community members (step 5).
We randomized the exact nature of these additional step-5 mobilization activities. Half the treatment villages were randomized into an individualized door-to-door campaign (step 5a; Fig. 1e), whereby social mobilizers went to 20 randomly selected structures to privately discuss any concerns about that vaccine that the household residents had and to encourage them to visit the vaccination site. The other 50 treatment communities were randomized into small-group outreach (step 5b; Fig. 1f), whereby mobilizers targeted social groups who gathered at fixed spots in and around the villages (for example, groups of farmers in fields, mosque attendees or women collecting water). Social mobilizers engaged the group to have joint conversations about the vaccines. There was equipoise about whether individualized or small-group outreach would be more successful in persuading people to get vaccinated, so we tested both strategies.
Effects on COVID-19 vaccination rate
Our primary outcome was verified adult vaccine uptake, which was measured using a respondent-level question on whether the person took a COVID-19 vaccine of any type, checked against their vaccination card (if consented). This measure provided us with a site-level count of vaccine doses administered.
To calculate a village-level vaccination rate, we first enumerated the population in all 150 treatment and control villages. Such community census lists typically do not exist in Sierra Leone. Our research team therefore walked to all structures in every village to tally the number of households (39 on average, s.d. = 23), and the number of individuals living in those households (29,588 individuals across the 150 villages, or about 197 people per village).
The population of these villages was on average 22.3 years old, 26.5% of households were headed by women and 64.5% of people lived in a household of 6 or fewer people. Only 20.1% lived in a household where the household head had any form of formal schooling, and about 86.1% lived in a household where the head was primarily engaged in farming. Respondent characteristics were well balanced across the treatment groups (Extended Data Table 2) except for the following: the baseline vaccination rate; the proportion of households employed in agriculture; the proportion of households that own a radio; the proportion of women breastfeeding; and the proportion that owns land. Although an overall F-test did not reject the equality of means across the full set of outcomes, we added these covariates in part of our analysis below.
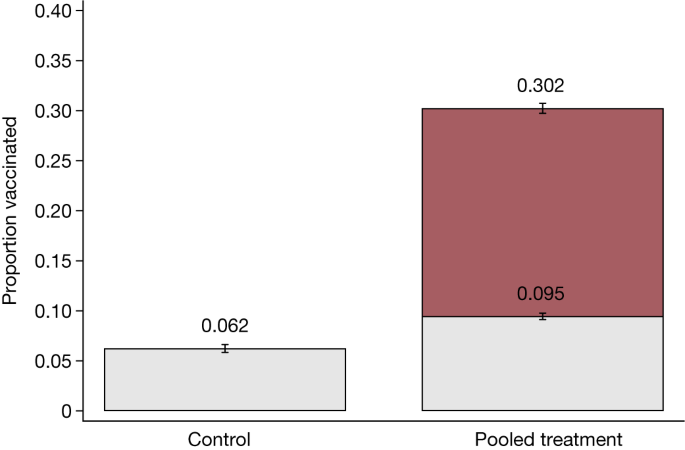
Figure 2 shows that at baseline, the average vaccination rate in villages assigned to the control group (control villages) was 6.2% compared with 9.5% in villages that received treatment (treatment villages) (ordinary least squares (OLS) regression, difference = 0.035, s.e. = 0.014, P = 0.015, n = 12,096). After intervention, the vaccination rate increased to 30.2% in treatment villages. We report effects from linear regression specifications of the intent-to-treat effect with randomization fixed effects and heteroscedasticity-robust standard errors clustered at the village level in Extended Data Table 3 (see the section ‘Statistical analysis’ in the Methods). The intent-to-treat effect was 26 percentage points (OLS regression, s.e. = 0.018, P < 0.001, n = 12,096). The results remained qualitatively similar (OLS regression, 25 percentage points, s.e. = 0.019, P < 0.001, n = 12,096) when covariates for respondent characteristics were added that were imbalanced at baseline (such as vaccination status) or when we aggregated the data up to the village level (OLS regression, 28 percentage points, s.e. = 0.025, P < 0.001, n = 150).
The proportion of vaccinated adults that were enumerated during the census before and at the end of the study in control villages and pooled treatment villages. The analysis includes the 12,096 people (aged >18 years) in 150 villages. Data are presented as the mean ± s.e.m. In the control group, 6% were vaccinated at baseline, whereas 9.5% were vaccinated in treatment groups. At endline, 30% were vaccinated. The intent-to-treat treatment effects estimated using OLS and including randomization block fixed effects and heteroscedasticity-robust standard errors clustered at the village level are provided in Extended Data Table 3.
This increase in the vaccination rate is an underestimate of the total number of vaccines administered over those 2–3 days, as it does not include vaccines given to migrant returnees and others from nearby villages. The average uptake also masks considerable heterogeneity among villages. In 2 out of the 100 treatment villages, there was no increase in vaccination rate because the village authorities either dissuaded villagers from getting vaccinated or refused permission for the intervention to take place, which causing the intervention to essentially fail at step 1 (Fig. 1a). By contrast, the full distribution of vaccination rates displayed in Supplementary Fig. 2 shows that in 5 villages, more than 50% of adults enumerated in the community census were vaccinated during the course of our intervention. A similar large degree of variation was evident from the total count of immunizations set per village (Supplementary Fig. 3).
Effects on total vaccination count
Many of the people who attended our temporary clinics to receive a vaccine were not enumerated during the community census. These additional people fell into one of three categories: residents of other nearby villages (who heard about the clinic and were interested in taking advantage of the easy access to a vaccine); recent migrant returnees who were not present during the village listing; and others—such as high-frequency commuters—not captured in the census. For these auxiliary populations, we do not have a denominator and can therefore not estimate a vaccination rate. We can, however, provide results on vaccination counts.
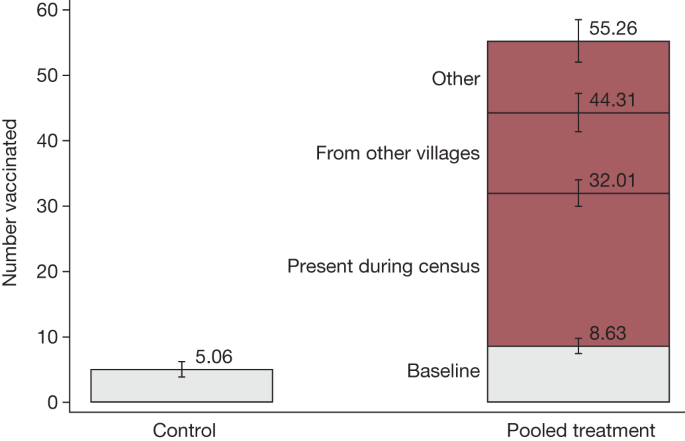
At baseline, there were on average about 5 people vaccinated in control villages and about 9 people in treatment villages (OLS regression, difference = 3.57, s.e. = 1.51, P < 0.021, n = 150). Figure 3 shows that after the intervention was implemented over the subsequent 2–3 days, the number of vaccinated individuals increased to about 55 people on average per treatment site, which is a 6-fold increase. This is the full effect of our mobile vaccination drive. Among individuals vaccinated who were not enumerated in the census, 53% (12–13 people per treatment community) were visitors who came from nearby villages to get vaccinated, whereas the remaining 47% (11–12 people) included short-term, circular commuters or migrant returnees who were not present on the day of the census and could not be matched to our listing records, as well as individuals whose ‘community of origin’ was unknown. The intent-to-treat regression estimates with heteroscedasticity-robust standard errors and additional covariates are included in Extended Data Table 4. In total, the teams vaccinated 4,771 people aged 12 years or above. Of these, 39% received a Johnson & Johnson vaccine, 29% Pfizer, 17% Sinopharm and 16% received AstraZeneca. A variety of vaccine types was administered because there was no steady supply of any specific type of vaccine dose in Sierra Leone when this intervention was conducted. Therefore, we had to make use of the vaccines available in the Ministry of Health stocks in any given week.
The number of the people vaccinated before and by the end of the study. Data are presented as the mean ± s.e.m. The analysis includes 150 villages. In the control group, on average five people were vaccinated, whereas in treatment villages, this was nine people. Treatment increased the count to 55 people, including 22–23 individuals who were enumerated during the census group, 12–13 people from nearby villages and 11–12 short-term, circular commuters or migrant returnees who were not present on the day of the census and could not be matched to our listing records, as well as individuals whose community of origin was unknown. The intent-to-treat treatment effects estimated using OLS and including randomization block fixed effects and heteroscedasticity-robust standard errors are provided in Extended Data Table 4.
Effects of home visits
Both types of mobilization activities implemented in step 5 had similar effects on the vaccination rate. The evidence on whether the door-to-door or small-group activities were more effective was mixed. When we compared across communities, the door-to-door programme increased the adult vaccination rate by about 29 percentage points compared with 23 percentage points in villages assigned to the small-group mobilization activities (t-test, difference = 6 percentage points, P = 0.014, n = 12,096; see column 1 in Extended Data Table 1). However, when we studied individual households randomly assigned to a visit against those who are not within door-to-door villages, we did not detect any differential uptake. In these 50 villages, up to 20 randomly selected structures were visited for a private or semi-private conversation with residents about the vaccine and to encourage them to visit the temporary clinic. The random selection of structures enabled us to report experimental results on the effects of receiving this extra nudge on the propensity to receive a vaccine. We interpret this activity as a ‘demand-side treatment’, in that the visit and conversation provides that resident an opportunity to discuss their concerns or questions about vaccines in private, which could be useful to overcome potential hesitancy. Column 3 in Extended Data Table 1 shows that this extra effort did not generate additional demand beyond the effect of our ‘supply side’ activities to enhance vaccine access. The adult vaccination rate at the end of the vaccination programme among those who received the home visit by mobilizers was not different from those who did not receive the extra nudge points (OLS regression, difference = –0.01, s.e. = 0.019, P = 0.543, n = 3,760). Social mobilizers received extensive training and close supervision, but the lack of impact from this additional demand-generating activity on vaccine uptake may reflect low effort by social mobilizers. Within-village spillovers may also dampen these individual treatment effects. Unfortunately, we lack data on distances and other channels of interactions among households to formally test this measure. However, this type of spillover may be small owing to the relatively short time interval between the home visits and the vaccine drive.
We do not have an equivalent analysis of the individual effect of the small-group treatment because that was not randomized within villages. Moreover, the enumerators were not able to exactly track which households participated in the small-group sessions.
Mechanisms
Although our vaccine access intervention significantly raised the vaccination rate, it was also clear that we remained far short of reaching the WHO goal of near-universal uptake. We collected individual-level data in all treatment villages after the intervention from both vaccine takers and non-takers. These data can shed some light on why and how our access intervention was more or less successful for certain types of people.
Meeting attendance
Step 2 of our intervention (Fig. 1b) was to organize a community-wide meeting to inform all village residents about the vaccine clinic. The field team registered which community members attended that meeting, and 41% of households participated in these meetings. Overall, 44% of those who chose to attend the meeting subsequently chose to get vaccinated. One cannot impose any causal interpretation to this correlation because people who were already interested in getting vaccinated may have been the ones who chose to attend the meeting.
We can make a slightly stronger inference by examining the subset of people who stated in our baseline survey that they were unwilling to receive a vaccine (Extended Data Table 5). Within this subgroup, 53.8% of those who attended meetings ultimately took the vaccine, whereas the vaccination rate was only 14.4% among those who did not attend. Even within the converse subgroup (those who stated at baseline that they were willing to take the vaccine), meeting attendance was strongly predictive of subsequent vaccine uptake: 64.6% vaccination rate among attendees and 39.4% among non-attendees.
These are not causal estimates, but the size and direction of these correlations suggest that the information shared in the meeting, and the answers that were provided to the community’s questions, are unlikely to have dissuaded people from getting vaccinated. These correlations—combined with our team’s on-field experience—suggest that holding these meetings was helpful and form a necessary part of any access intervention. Encouraging greater attendance in meetings in any future replications would probably be a good idea.
Vaccination knowledge and trust
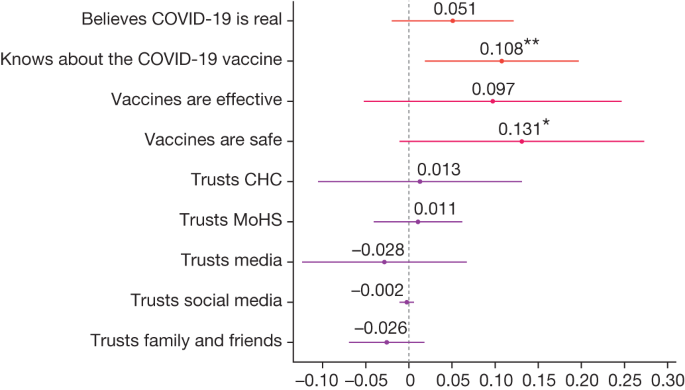
We also collected data on another intermediate outcome in a subset of villages: people’s knowledge and attitudes regarding the COVID-19 vaccine. Figure 4 shows that the treatment improved people’s knowledge about vaccines (OLS regression, difference = 0.11 points, s.e. = 0.044, P = 0.019, n = 817). The change in knowledge implies that our intervention was not solely about improving access. That is, the community interactions and the information we shared were also relevant parts of the intervention package. However, there was no significant change in people’s beliefs about vaccine efficacy (OLS regression, difference = 0.097, s.e. = 0.074, P = 0.197, n = 686). Using a 95% confidence interval (CI), we can reject that our treatment increased beliefs about vaccine efficacy by more than 12 percentage points. The effect on beliefs about the safety of vaccines is not statistically precise (OLS regression, difference = 0.131 points, s.e. = 0.070, P = 0.069, n = 686)—we can neither rule out a null effect nor a 27 percentage point effect. The null effects in OLS regressions on the sources that people trust the most for receiving health information were more precisely estimated: community health clinics (OLS regression, difference = 0.013, s.e. = 0.059, P = 0.828, n = 817, 95% CI upper bound = 0.13); the MoHS (difference = 0.011, s.e. = 0.025, P = 0.682, n = 817, 95% CI upper bound = 0.06); media (OLS regression, difference = –0.028, s.e. = 0.047, P = 0.553, n = 817, 95% CI upper bound = 0.07); social media (OLS regression, difference = –0.002, s.e. = 0.004, P = 0.555, n = 817, 95% CI upper bound = 0.006); or family and friends (OLS regression, difference = –0.026, s.e. = 0.022, P = 0.242, n = 817, 95% CI upper bound = 0.018). Extended Data Tables 6 and 7 provide the associated regression estimates. Note that because this is an exploratory exercise in which we test treatment effects across several outcomes, the tables report the false discovery rate (FDR)-adjusted q values to adjust for multiple hypothesis testing.
Intent-to-treat estimates of community treatment assignment for each outcome listed on the y axis. Treatment effects were estimated using OLS and included randomization block fixed effects and heteroscedasticity-robust standard errors clustered at the village level. Each dot is labelled with the exact coefficient (to three decimal places) and significance at the ***1,**5 and *10 per cent critical level. Bars represent 95% CIs of treatment estimates. The analysis includes 45 villages and 817 households surveyed at endline for which we observed complete randomization blocks. Associated regression results are provided in Extended Data Tables 6 and 7, including corresponding sample sizes. Reported estimates do not correct for multiple hypothesis testing. The Extended Data tables report the associated FDR-adjusted q values. The survey measures for the ‘Believes COVID-19 is real’ comes from the survey question: “Do you believe that COVID-19 exists in the world?” (yes or no). ‘Knows about the COVID-19 vaccine’ comes from the survey question: “Do you know about the COVID-19 vaccine/marklate?” (yes or no). ‘Vaccines are effective’ is 1 if respondents completely agree with the statement: “Vaccines are effective.” ‘Vaccines are safe’ is 1 if respondents completely agree with the statement “How much do you agree with this statement: vaccines are safe.” Trust in sources of information are from a multiple-select question: “Who do you most trust getting information about COVID-19?” (community health clinic (CHC), MoHS, media (news, TV), social media (Facebook, among others), family and friends, among others).
Heterogeneity across demographic groups
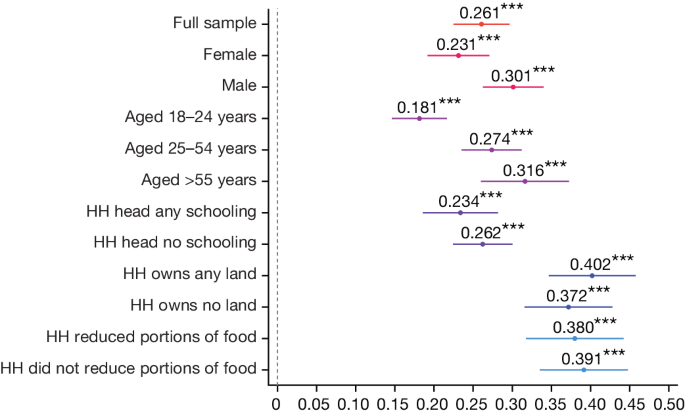
Figure 5 shows the differences in treatment effect for specific demographic subgroups. Extended Data Table 8 and Supplementary Table 1 provide associated regression results. The treatment effect was 7 percentage points larger for men than for women (OLS regression, difference = –0.067, s.e. = 0.016, P < 0.001, n = 12,096), and 12 percentage points larger for the >55 years age group compared with the 18–24 years age group (OLS regression, difference = –0.122, s.e. = 0.028, P < 0.001, n = 12,096). We cannot reject the null hypothesis that there is no difference in treatment effects across education (OLS regression, difference = –0.003, s.e. = 0.018, P = 0.864, n = 12,096, 95% CI upper bound = 0.032), land ownership (OLS regression, difference = 0.038, s.e. = 0.035, P = 0.268, n = 2,674, 95% CI upper bound = 0.11) or food security status (OLS regression, difference = –0.006, s.e. = 0.032, P = 0.865, n = 2,674, 95% CI upper bound = 0.06), and can rule out large effect sizes.
Intent-to-treat estimates of the vaccination rate of the pooled treatment groups for each subgroup listed on the y axis. Treatment effects were estimated using OLS and included randomization block fixed effects and heteroscedasticity-robust standard errors clustered at the village level. Each dot is labelled with the exact coefficient (to three decimal places) and significance at the ***1, **5 and *10 per cent critical level. Bars represent 95% CIs of treatment estimates. The dependent variable is the vaccination status of adults at the end of the study enumerated during the census. Sex, age and schooling data are from the census. Land ownership and food insecurity are from the baseline sample. Associated treatment estimates and associated sample size for each subgroup are provided in Extended Data Table 8. The indicator for ‘HH head any schooling’ indicates whether the household (HH) head had schooling above the primary level. The ‘HH owns any land’ indicates whether the household owns land. The ‘reduced portions of food’ statements indicate whether any household member had reduced food portions during the previous week.
Comparison with other vaccination efforts
As shown in Extended Data Table 3, the intervention increased vaccination rates by about 26 percentage points. Although such an increase seems substantial, this is the gain off a very low base rate: just 6–9.5% were vaccinated at baseline. Another relevant benchmark is our percentage point effect size and how that compares with other vaccination campaigns evaluated in the literature.
We conducted a literature review of vaccination strategies that have been evaluated using RCTs (see the section ‘Literature review of vaccination uptake RCT studies’ in the Methods). The Methods provides inclusion criteria for this review. We identified 144 different published RCT studies that report the results of 235 distinct interventions.
These interventions varied across multiple dimensions, spanning time, space and strategy, often as part of the same study with multiple components. For clarity and brevity, we identified five major intervention ‘families’, which could be further fragmented into more granular intervention ‘types’. The families into which interventions were sorted were education, community actions, communications, incentives, and healthcare improvement and worker training. Among the 144 relevant studies, only 3 focused on the essential theme of vaccine access in a low-income context, and none of them were centred on COVID-19 vaccines16,17,18.
Supplementary Fig. 5 demonstrates the heterogeneity of effect sizes across these 235 different treatments (effect size range of –6 to 50 percentage points). Of all treatments reviewed, 35% had no significant effect on vaccine uptake. Perhaps unsurprisingly, owing to the variety of incentive types and sizes, the incentives group was strongly positively skewed, accounting for five out of the top ten effect sizes overall. However, the highest median effect size was among educational interventions (median = 6.25)19,20.
The intervention we conducted in Sierra Leone—whereby mobile health teams visited remote communities for 48–72 h to ease access burden—produced a larger percentage point effect size than 223 (95%) of the treatments reviewed.
Supplementary Table 2 provides details of the intervention approach used in each study. The majority of these studies were conducted in high-income settings (83%). Many of the vaccination campaigns evaluated were nudges and reminders by text messages, telephone or mailings (50%). Nudges are inexpensive, but often produce small or null effects. Other strategies involved visiting parents to educate them about the benefits of childhood immunization (25%) or sending community health workers (5%). Others offered direct financial incentives against a verified vaccination (9%).
Of special interest were recent studies that attempted to promote COVID-19 vaccinations. A study in Sweden21 offered monetary rewards of $24 to receive a COVID-19 vaccine, and this increased the vaccination rate by an extra 4 percentage points (from 72 to 76%). A financial incentive of $10–50 combined with other nudges in the United States did not produce any effect22. City-wide and state-wide lotteries offering financial rewards in the United States23,24 produced small or negative effects. Text-based reminders in the United States25,26 and defaulting people into a vaccination appointment in Italy (so that they are forced to opt out)27 increased vaccination rates between 0 and 3.5 percentage points.
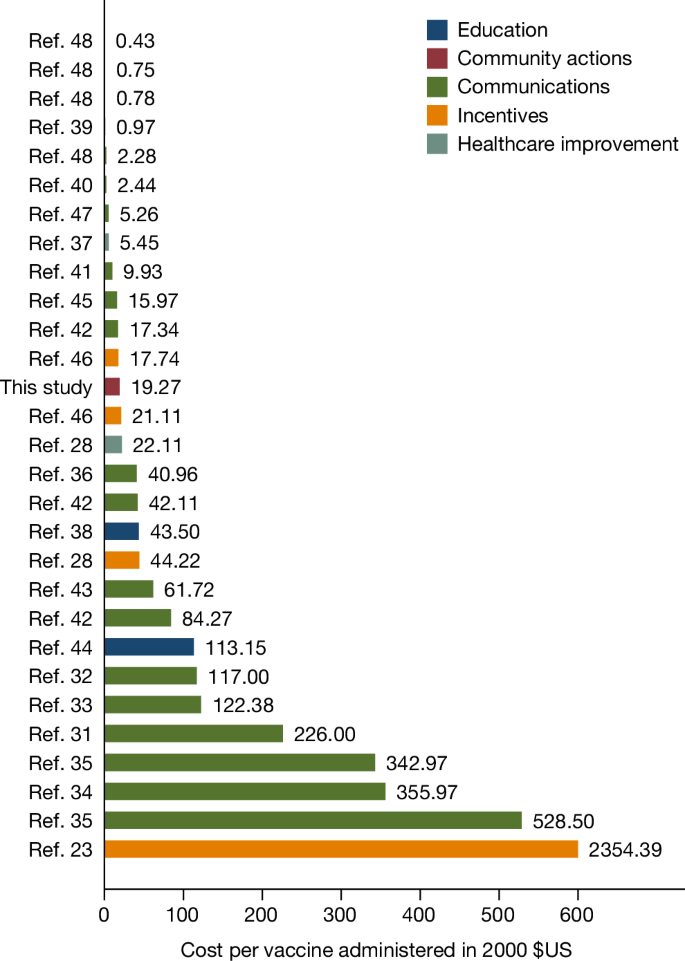
Cost-effectiveness relative to other strategies
Sending text message reminders or running city-wide lotteries are relatively inexpensive to implement, whereas delivering vaccines to remote areas is costly. It is therefore useful to compare not just percentage point effect sizes but also the cost of administering various programmes per vaccinated individual. Moreover, we chose to work in the most remote areas not covered by the Sierra Leone MoHS vaccination programmes precisely because they are too far away even from PHUs. We collected detailed cost data on our programme to compute this metric and compared it to other studies that provide such cost information (see the section ‘Literature review of vaccination uptake RCT studies’ in the Methods).
The total costs of our intervention to reach 100 villages was $156,023.5, or approximately $1,560 per village. This included all travel, administration and management and supervision costs, but excluded the cost of the vaccine doses, which were provided to Sierra Leone by the COVAX programme for free. This translates to a cost per dose administered of about $33.
Extended Data Table 9 provides a detailed breakdown of the fixed and variable components of our implementation costs. Of the $33, around 27% ($9) was fixed costs of training project staff and 73% ($23) was variable costs. The most expensive category (38% or $12.50) was transportation to these remote villages, which included the cost of renting vehicles and fuel. Salaries and subsistence allowances for the social mobilization and vaccination teams accounted for another one quarter of the total costs.
To conduct this intervention again at larger scale, the variable costs would need to be repeated, but not the fixed costs of training. At scale, the cost of this intervention would therefore approach about $23 per person vaccinated. The wide availability of a cadre of staff known as Ministry of Health volunteers—individuals already vetted by the ministry and available to work as mobilizers on special projects against per-diems—increases the potential for scaling this project nationwide in Sierra Leone. One potential challenge of replicating this project to other countries is to find trained staff who can take on that mobilization role.
Note that here we are looking at cost-effectiveness from the perspective of the planner (that is, the government) and do not consider the costs imposed on households. Depending on context, meeting attendance can be inconvenient or costly. In our context, villages are small. On average, people had to walk less than a couple of hundred metres to attend the meetings. Also, to minimize the inconvenience, meetings were held in the early evenings after people returned from their farms. As a result, the opportunity cost of time was low for most participants of the meeting.
Figure 6 provides the cost per vaccinated person in year 2000 US dollars for the subset of studies in Supplementary Table 2 that reported sufficiently detailed cost information for us to be able to compute this metric. Of the 235 different treatments identified in our literature review, only 33 (14%) directly stated the cost of the intervention per successfully administered vaccination. Furthermore, of these 33 interventions, 7 did not report a cost specific to the treatment group, but only the overall cost averaged over all groups of the study. In total, 57% of the vaccination campaigns exceeded our $33 benchmark. The mean value in Fig. 6 is $83 (s.d. = 132), even after excluding the most expensive approach.
The cost per vaccination administered (in year 2000 US dollars, calculated using inflation data sourced from the US Bureau of Labor Statistics). These are treatments from studies included in Supplementary Table 2 that explicitly provided information about the cost of the intervention per vaccine actually administered. This cost specifically refers to the intervention and does not include the cost of the vaccine itself. Studies that did not unequivocally state the cost of the intervention per vaccinated person were not included. The colour of each bar indicates the broad type of intervention. The cost per person vaccinated in our study was $32.70, which is approximately $19.27 in 2000 US dollars. The mean value in this figure is $83 (s.d. = 132) after excluding the most expensive approach. References 23,28,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48 are cited in this figure.
A study in rural India28 pursued a similar strategy to ours by setting up measles vaccination clinics. That treatment cost $75 (in 2022 dollars) per vaccine administered, but adding an incentive for the parents to bring their children to the clinic lowered the cost to $38 per child vaccinated. The only other COVID-19 vaccine study in our review to provide cost information21 offered $24 as a financial incentive to get vaccinated in Sweden. Unfortunately, that study did not report costs of other components of the programme, such as the cost of administering the incentive programme, verifying individual-specific vaccination information in the administrative records, sending two text message reminders, among others.
Discussion
Our findings showed that a simple last-mile vaccine intervention tripled vaccination rates within 48–72 h. In addition, auxiliary populations showed up to take advantage of these mobile vaccination centres, which more than doubled vaccination counts. Our intervention, despite being delivered in highly remote locations, is cost-effective relative to other efforts that aim to increase vaccination rates.
Policy implications
Vaccine equity remains an important policy goal10. Vaccination rates are severely lagging among rural populations in Africa. Therefore, achieving equity requires us to devise an effective strategy to reach this population. Our study provides some guidance on how to formulate that strategy.
The most immediate and direct implication of our results is for the government of Sierra Leone to replicate and expand this cost-effective programme to reach the 59% of the country’s population who reside in similar remote, rural areas outside PHU coverage. The largest expense of our intervention was the transport cost of reaching remote communities; therefore, an obvious implication is that we should bundle COVID-19 vaccines with other necessary mother, infant and child health interventions that can be simultaneously delivered on the same trip3. Such an approach could substantially reduce costs per person treated. However, this would still be expensive for a resource-constrained MoHS to launch at scale, and international partners must provide support. A recent study in rural Western Kenya29 demonstrates that such integrated approaches, combining HIV testing with other preventive health services such as bed nets and water filters, can be successfully implemented.
We have begun building the necessary coalition to implement such a bundling strategy to improve the cost-effectiveness and scalability of this last-mile-delivery intervention. The Sierra Leone MoHS has prioritized HPV vaccination for girls aged 10–12 years, and routine immunizations (DTP, measles, polio) for children aged 0– 6 years to bundle with any further COVID-19 vaccine delivery. It is reasonable to wonder whether COVID-19 vaccine distribution is a high-priority investment given the low incidence of COVID-19 in Africa. However, as the experience in India from April 2021 shows, new COVID-19 variants have the capability to devastate public health systems in developing countries30. Health infrastructure in a typical country in Africa is even more fragile than it is in India. If we pay the transport cost to take a bundle of health interventions to these remote communities, COVID-19 vaccines could easily be an element of that bundle.
The other direct implication is to replicate such a programme in neighbouring countries with similar last-mile delivery challenges. The majority of people in sub-Saharan Africa live in rural areas7, so overcoming access challenges through such initiatives holds enormous potential for both achieving vaccine equity and maximizing global coverage.
Our study showed that low-income countries need to experiment with creative ideas to overcome logistical challenges, such as setting up temporary clinics and sending both vaccine doses and nurses to remote locations on motorcycles. A broader implication for international development partners and pharmaceutical companies is that they need to facilitate and underwrite such experimentation by making vaccine doses and budgets readily available to allow ministries of health to learn what approaches work best in a given context. Local institutions need to engage in ‘learning by doing’, which is impossible without a reliable supply of vaccines and incentives for staff to tinker with new, innovative ideas.
Study limitations
The intervention we implemented had two important limitations. The $33 cost (per person vaccinated) varied substantially across villages because the number of individuals per village that we managed to vaccinate varied (the vaccination rate ranged from 0 to 69%). Village leaders did not allow us to conduct the intervention at all in 2 of the 100 treatment villages, which inflates the overall average cost of our intervention. Any replication should try to identify early the villages where such refusals might occur and find ways to avoid having the entire vaccination team travel there.
Second, we observed large cross-team variation in performance. Supplementary Fig. 4 shows that some of our teams administered more than twice as many vaccines as other teams (the number of vaccines administered ranged from 0 to 146 per village, mean = 48, s.d. = 31, median = 42). Some of these differences could be due to differences in village characteristics, but our implementation experience suggests that variability in team effort also played a part. Providing good performance incentives to teams could improve the cost-effectiveness of this strategy. Given that a large proportion of the expense of the intervention is the cost of travelling to the remote village, we should strategize to ensure that we maximize the vaccination rate within the 48–72 h window once we get there.
Methods
Ethics approval
We received Institutional Review Board (IRB) approval from the Sierra Leone Ethics and Scientific Review Committee (SLERC 20220210), Yale University (2000031541) and Wageningen University (WUR 20220222). The research protocol was pre-registered at the ISRCTN Registry (study identifier ISRCTN17878735). All study participants completed informed consent.
The study was implemented in close collaboration between the researchers, the Government of Sierra Leone’s Expanded Programme on Immunization (EPI) at the MoHS, their National COVID-19 Emergency Response Centre and Concern Worldwide (an international NGO who partners with MoHS on health projects). This collaboration came together because all partners had the joint goal of addressing barriers to vaccine adoption in rural Sierra Leone. Although all partners are responsible for the research design, only the Ministry of Health team was responsible for actually distributing and administering vaccines. We had a memorandum of understanding in place to govern this collaboration.
Village study sample
To determine the sample size, we ran a power calculation assuming a 5% significance level with 80% power. We assumed an intra-cluster correlation of 0.15 as decisions to take a vaccine are probably highly correlated within a village. Average village populations are 2,480 people. We assumed an eligible population of 50% and a baseline vaccination rate of 2.5%. Based on the treatment effects reported in the literature for similar studies, we took a conservative approach and set our expected minimum detectable effect at 0.05. We oversampled slightly and the final design included 150 communities across the three treatment groups in a 1:1:1 ratio.
We chose study sites in collaboration with the MoHS. We started with the 2015 Sierra Leone census, which contains data on 20,659 communities in 166 chiefdoms across 16 districts. We selected 7 largely rural districts (Koinadugu, Falaba, Karene, Kambia, Tonkolili, Bombali and Port Loko), limiting the sample to 8,784 communities in 54 chiefdoms. We then restricted our sampling frame to communities that, according to the 2015 census, had no health clinic within 5 miles (about 8 km) of the community centre, the standard PHU catchment area (Extended Data Table 10), resulting in 1,849 communities. From this list, we excluded very small communities that contained fewer than 19 structures and communities for which latitude and longitude were missing. The final sampling frame consisted of 420 communities located in 49 chiefdoms and 7 districts. Within each district, we then matched communities on the following strata: (1) the share of the population that was immunized; (2) the age of the population; (3) literacy levels; and (4) the distance from the closest clinic. This allowed us to identify communities that had the most similar characteristics within a district and used this to assign the most similar communities to one of the treatment groups and establish comparable ‘triplets’. This resulted in 106 triplets in total. We then randomly selected 50 triplets using district as a blocking variable. The final list included 9 triplets each for Koinadugu and Falaba districts, 8 triplets for Karene district and 6 triplets each for Port Loko, Tonkolili, Kambia and Bombali districts.
Randomization
Randomization to vaccine access treatments
Within each of the 50 triplets, we randomized villages into control, door-to-door and small-group treatment groups. This resulted in 50 villages assigned to control, 50 to door-to-door and 50 to small group (Supplementary Fig. 1). The sample was well balanced on observable characteristics (the F-statistic at the bottom of Extended Data Table 2 is small and not significant).
Household-level random assignment to door-to-door treatment
Within the villages randomly assigned to the door-to-door treatment group, we randomly selected up to 20 residential structures from the community census list to receive a visit from the social mobilization team.
Data collection
Community census listing and baseline survey
Before any intervention activities took place, the research team implemented a community census to enumerate all households in all 150 villages. The research team went door to door to each residential structure and asked how many households resided in the structure. They then interviewed each household head to create a roster of those who ‘eat from the same pot; and reside under the same roof for at least the past 9 months (aside from newborn babies).’ For each household member, enumerators asked about the sex, age and vaccination status. The total census includes N = 29,588 people. Migrant household members who were temporarily away on the day of the visit would have been missed from this listing.
Next, the research team randomly selected a sample of 20 households per village from the households listed in the census to conduct a short (baseline) survey with the household head to record household characteristics (age, sex and education), access to land and food security. The total baseline sample included N = 2,240 respondents.
Exit and endline surveys
After the interventions were implemented, the research team conducted an exit survey of those who received a vaccine at each mobile vaccination clinic. The survey recorded the vaccination status verified using visual inspection of the vaccination card, as well as age and sex.
During the exit survey, enumerators also recorded where people came from and their district and village name (if different from the implementation site). To assess between-village spillovers, we then matched the names of reported villages back to our list of control villages. Using a hard match on district names and then a Levenshtein distance metric to match village names, allowing for a string distance of 2, we found only 8 matches. Using a more conservative cut-off of 1, no overlap was found. Our within-sample spillovers were small or non-existent owing to the large physical distance between pairs of sample villages. The minimum straight-line distance between project treatment and control villages was 8.5 miles (13.7 km), which would take at least 2–3 h to traverse by foot. Any spillover benefits largely accrued to others who were not part of the experimental pool.
For a subsample, the research team conducted a follow-up survey to capture knowledge of COVID-19 and COVID-19 vaccines as well as trust in various sources of information. We used data from 878 respondents in 45 villages for which we observed triplets (that is, where we had information on all treatment groups and a 1:1:1 ratio). We collected data from a total of 105 villages (50 control, 30 door-to-door and 25 small-group treatment group villages); however, only for 45 villages did we observe all three treatment groups and therefore provide a clean comparison. Respondents in this subsample of villages were highly similar to those in the overall sample. An overall F-test did not reject the equality of means: P = 0.668 (Extended Data Table 10).
In treatment villages, these questions were part of the exit survey and implemented 1 day after intervention activities were completed. In control villages, households were visited only once. From a design perspective, we would have ideally captured outcomes at both baseline and endline in each village. It was, however, highly unlikely that these remote places would have been visited by other health personnel from the MoHS or NGOs in the 5-day period between baseline and endline, or that a large number of people would have incurred the cost of visiting the community health clinic for receiving a COVID-19 vaccine. In addition, the costs of revisiting communities in these remote locations are high (the largest line item on the budget relates to transportation costs; Extended Data Table 9). We verified that there was no vaccination drive conducted during this period. Furthermore, we use the fact that our baseline survey was conducted over a few weeks across communities to inspect the temporal trends in the data. A simple regression of baseline vaccination rates on the date of the baseline survey did not reveal any trend. This reduces the concern that our choice to not revisit control villages affects the conclusions we draw.
Research assistants were blinded with respect to treatment groups and study hypothesis.
Intervention details
Timeline of activities
The research team collaborated closely with the Ministry of Health vaccination team. Both the team of vaccinators and social mobilizers from the MoHS and enumerators in charge of the survey received extensive training on implementation protocols. Only those individuals who were considered proficient after examination were retained for implementation or data collection. Within each village the teams followed several steps outlined below (see Supplementary Fig. 1 for further details). On day 1–2, the research team implemented census listing and baseline surveys described above. On days 3–5, the social mobilizer team engaged in small-group and door-to-door mobilization, the MoHS performed a vaccination drive and the research team conducted exit surveys in treatment villages. On day 6, the research team implemented endline surveys.
Social mobilization
The MoHS trained community mobilizers on COVID-19 vaccine safety and efficacy, vaccine types and availability. All mobilizers were trained on how to respond to questions and to counter any misinformation about COVID-19. They were also trained on WHO-recommended safe practices relating to COVID-19 and were instructed to maintain social-distancing protocols and to wear masks when social distancing could not be guaranteed. Additional masks were made available for free for community members.
Community social mobilizers arrived at the village before the mobile vaccination teams. The community mobilizer engaged with local community leaders, including the town chief, section chief, paramount chief, mammy queen, town elders, youth leaders, community health officers, imams, and any other relevant authorities, to seek permission to organize a village information session. The information session took place at a central location, often the community centre or any other convenient location amenable to safe COVID-19 practices.
At the information session, the mobilizer informed community members about COVID-19, available vaccines and evidence about the safety and efficacy of vaccines in preventing transmission and severe illness. People were also informed about the mobile vaccination team and operating procedures during the vaccination drive. They encouraged participants to spread this message to other members of the community not present during the meeting.
In two treatment villages, the MoHS vaccination team did not receive permission from village authorities to conduct the vaccination drive.
Door-to-door campaign
In 50 of the 100 villages randomly selected for treatment, community mobilizers approached up to 20 structures randomly selected from the census list, after the group information session was completed. The proportion of each community assigned to treatment therefore varied with the population of the community. In four small communities, all structures were assigned. Owing to logistical complexities and costs, in some communities, mobilizers did not include highly remote village structures (more than 15 min walk from the village centre). This excluded a total of 10 structures (including 40 people aged ≥12 years). Social mobilizers met in private with residents and delivered the same information as was presented at the community meeting. In addition, they addressed people’s concerns in private. If the individuals were immediately convinced to get vaccinated, the social mobilizer would guide them to the vaccination site before moving on to the next household. Neighbours not assigned to receive a home visit were present during the information session in a few cases. In 75% of the communities, these ‘compliance issues’ were limited to representatives of three or fewer control households, and the majority of communities had no non-compliance of this kind.
Small-group mobilization
In the other 50 treatment villages, after the group information session, social mobilizers searched for small groups of people around the village to converse with. Such groups included women washing clothes around the river, individuals gathered at the ataya (tea) shops, residents playing a game of draughts, groups of people around the mosque or church or farm, or residents gathered near the town chief’s house. Social mobilizers repeated the same information presented during the community information session. If people inside the small group had already taken the vaccine before this second session, they were invited to talk about their experience. After the session, if residents wanted to take the vaccine, the social mobilizer would guide them to the vaccination site before moving on.
Mobile vaccination drive
Vaccines were transported in approved cool boxes or vaccine carriers appropriate for transportation to remote locations. In each treatment village, the MoHS mobile vaccination teams worked with community leaders to select a suitable venue for the vaccination drive. The venue was chosen with the following requirements in mind: it needed to accommodate a waiting area (with some shelter); an arrival and check-in area where patient information can be gathered, maintaining confidentiality; a space for clinical assessment and vaccine administration, including vaccine preparation, maintaining patient confidentiality, privacy and social distancing; an area and system for post-administration observation of patients.
Individuals below 12 years of age were excluded from vaccinations. MoHS teams determined on-site whether a person deemed ‘at risk’ (for example, pregnant or suffering from severe disease) would also be excluded. After the vaccine was administered, recipients were asked to remain in close proximity to the vaccination team for a minimum of 15 min in the event that they experienced any unexpected side effect.
Vaccine teams were compliant with MoHS requirements for the storage, preparation, administration and disposal of the vaccine and associated materials. They followed infection prevention and controls and checked the eligibility of people to be vaccinated using the patient checklist.
Mobile teams adhered to MoHS guidelines on informed consent to receive COVID-19 vaccination, ensuring it was taken only by people with the mental capacity to consent to the administration of the vaccines, and taken freely, voluntarily and without coercion. Participants were allowed to withdraw consent at any time.
All vaccine teams received training on vaccinations, including the management of adverse events following immunization. All such events had to be reported using national reporting systems to the MoHS.
Statistical analysis
To estimate the impact of the intervention on the adult vaccination rate (Extended Data Table 3), we estimated intent-to-treat effects using OLS on individual-level data as follows:
where Yi,j is the vaccination status of individual i, in village j, Tpooled is the village assignment to either door-to-door or small-group treatment groups, αk is a vector of randomization block fixed effects (that is, triplet) and ϵi,j are heteroscedasticity-robust standard errors clustered at the village level. We estimated effects using a linear estimator (OLS) that accounts for high dimensional fixed effects49. In additional analyses, we added to the right-hand side of this equation Yi,j,bl, the baseline vaccination status, and Xj, the vector of covariates that were unbalanced at baseline. We also estimated equation (1) at the village level and for each group, by estimating both β1,jTdoor to door and β2,jTsmall group for the door-to-door and small-group treatment groups, respectively (Extended Data Table 1).
To estimate the vaccination count (Extended Data Table 4), we estimated a village-level intent-to-treat effect using OLS on village-level data as follows:
where Yj is the number of people vaccinated in village j, Tpooled is the village assignment to either door-to-door and small-group treatment groups, αk is a vector of randomization block fixed effects (that is, triplets) and ϵj is the heteroscedasticity-robust standard error. We estimated equation (2) for several types of respondents. That is, those who were part of the village census, migrants, returnees and those not present during census, and those from other villages, and added Xj, a vector of covariates that were unbalanced at baseline.
To assess the individual-level effect of the door-to-door campaign, we restricted our sample to the 50 villages assigned to the door-to-door campaign (that is, Tdoor to door = 1), and estimated intent-to-treat effects using OLS as follows:
where Yi,s is the vaccination status of individual i in structure s (hut or house), Tdoor to door is the individual-level assignment to receive a visit by the social mobilization team to a structure, αj is a vector of randomization block fixed effect (that is, the village) and μi,s is the heteroscedasticity-robust standard error clustered at the structure level.
For the survey-based outcomes on COVID-19 vaccine knowledge and trust, we estimated equation (1), replacing the dependent variable with the survey responses described above, using the subsample of 45 villages where this dataset was collected and we had data on the full randomization blocks.
For our analysis of the treatment effects by subgroup, we estimated equation (1) separately for men, women, various age groups (18–24 years, 25–54 years and >55 years), and sample splits based on whether the household head had any schooling, owns any land or reduced portions of food. To test for differences across subgroups, we estimate equation (1) and interact the subgroup variable with treatment.
In the results presented in Extended Data Tables 6 and 7, we also adjusted for the fact that we conducted multiple tests on the same dataset by implementing FDR corrections and report the FDR q values50. We also report the bootstrapped P value51 to account for regressions with a small number of clusters.
Literature review of vaccination uptake RCT studies
We conducted a literature review of articles in PubMed published between 1 January 2000 and 7 January 2023 using the search terms ‘(vaccin*[Title/Abstract] OR immun*[Title/Abstract]) AND additional search term[Title/Abstract]) AND (Randomized Controlled Trial[Publication Type])’, with the following additional search terms: ‘access’; ‘community-based’; ‘cost effect*’; ‘demand’; ‘hesitant’; ‘incentive*’; ‘intervention*’; ‘mobile’; ‘nudge*’; ‘rural’; and ‘supply’. These searches returned 3,615 unique articles. We screened out articles that were not related to vaccine uptake or that did not use a RCT, which reduced the sample to 141 articles. We appended a further 20 relevant studies that were identified by snowballing and rejected 17 papers that did not have a control group, did not report the percentage-point change in vaccine uptake or did not include a test statistic. The final list of 144 articles comprises 234 distinct interventions for which we can report a percentage-point change relative to a control group (Supplementary Table 2). Of these, 33 interventions (14%) reported information about the cost of the intervention per vaccine administered. This cost specifically refers to the cost of implementing the intervention and does not include the cost of the vaccine itself. Studies that did not unequivocally state the cost of the intervention per vaccinated person were not included in our cost-effectiveness comparisons. Two studies reported the cost in currencies other than US dollars52,53, and these costs were converted to the US dollar equivalent for the year the study was published, using exchange rate data from the respective countries’ national statistics agencies. We did not analyse publication bias.
Deviations from pre-registered hypotheses
We pre-registered our research protocol and hypotheses at the ISRCTN registry (study ISRCTN17878735).
We report on our main hypothesis in Fig. 2 and Extended Data Table 3. In addition to reporting on our main pre-registered outcome (adult vaccination rate), we also report on the total immunizations given per vaccination site because many more people showed up to our temporary clinics from neighbouring villages or were not present during the pre-intervention census, and we had not anticipated this. Figure 3 and Extended Data Table 4 therefore report on the count of all individuals (aged 12 years and above) who visited our clinics to receive a vaccination. This metric is necessary to correctly compute the cost-effectiveness.
The heterogeneity analysis reported in Fig. 5, in which we analysed whether vaccination rates differ by age, sex, schooling and wealth variables, was not pre-specified and followed heterogeneity tests that are common in the vaccine literature54.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The primary survey data forming part of this study were collected using SurveyCTO software (v.2.81). These de-identified datasets are available in the Harvard Dataverse at https://doi.org/10.7910/DVN/PRXF5Z.
Code availability
All analysis for this paper was conducted using Stata SE 17. Replication files and de-identified data are available in the Harvard Dataverse at https://doi.org/10.7910/DVN/PRXF5Z.
References
Mathieu, E. et al. Coronavirus (COVID-19) vaccinations. Our World in Data https://ourworldindata.org/covid-vaccinations (2020).
Mobarak, A. M. et al. End COVID-19 in low-and middle-income countries. Science 375, 1105–1110 (2022).
Partapuri, T., Steinglass, R. & Sequeira, J. Integrated delivery of health services during outreach visits: a literature review of program experience through a routine immunization lens. J. Infect. Dis. 205, S20–S27 (2012).
Egger, D. et al. Falling living standards during the COVID-19 crisis: quantitative evidence from nine developing countries. Sci. Adv. 7, eabe0997 (2021).
Oehler, R. L. & Vega, V. R. Worldwide vaccine inequality threatens to unleash the next COVID-19 variant. Int. J. Infect. Dis. 123, 133–135 (2022).
Solís Arce, J. S. et al. COVID-19 vaccine acceptance and hesitancy in low-and middle-income countries. Nat. Med. 27, 1385–1394 (2021).
DataBank, World Development Indicators (The World Bank, accessed 1 December 2023); https://databank.worldbank.org/source/world-development-indicators.
Asadullah, M. N., Savoia, A. & Mahmud, W. Paths to development: is there a Bangladesh surprise? World Develop. 62, 138–154 (2014).
Global Biopharma CEO/Top Executives COVID-19 Media Briefing. IFPMA (7 September 2021); https://www.youtube.com/watch?v=qA7oos7sU8Y.
Ye, Y. et al. Equitable access to COVID-19 vaccines makes a life-saving difference to all countries. Nat. Hum. Behav. 6, 207–216 (2022).
Ramachandran, R., Ross, J. S. & Miller, J. E. Access to COVID-19 vaccines in high-, middle-, and low-income countries hosting clinical trials. JAMA Netw. Open 4, e2134233 (2021).
Kulle, A.-C., Schumacher, S. & von Bieberstein, F. Mobile vaccination units substantially increase COVID-19 vaccinations: evidence from a randomized controlled trial. J. Public Health https://doi.org/10.1093/pubmed/fdad213 (2023).
Sharma, M., Ying, R., Tarr, G. & Barnabas, R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature 528, S77–S85 (2015).
Mobarak, A. M. & Saldanha, N. A. Remove barriers to technology adoption for people in poverty. Nat. Hum. Behav. 6, 480–482 (2022).
Chater, N. & Loewenstein, G. The i-frame and the s-frame: How focusing on the individual-level solutions has led behavioral public policy astray. Behav. Brain Sci. 46, e147 (2022).
Ateudjieu, J. et al. Tracking demographic movements and immunization status to improve children’s access to immunization: field-based randomized controlled trial. JMIR Public Health Surveill. 8, e32213 (2022).
Sengupta, P. et al. Evaluation of a community-based intervention to improve routine childhood vaccination uptake among migrants in urban slums of Ludhiana, India. J. Public Health 39, 805–812 (2017).
Habib, M. A. et al. Community engagement and integrated health and polio immunisation campaigns in conflict-affected areas of Pakistan: a cluster randomised controlled trial. Lancet Global Health 5, e593–e603 (2017).
Usman, H. R. et al. Randomized controlled trial to improve childhood immunization adherence in rural Pakistan: redesigned immunization card and maternal education. Trop. Med. Int. Health 16, 334–342 (2011).
Andersson, N. et al. Evidence-based discussion increases childhood vaccination uptake: a randomised cluster controlled trial of knowledge translation in Pakistan. BMC Int. Health Hum. Rights 9, S8 (2009).
Campos-Mercade, P. et al. Monetary incentives increase COVID-19 vaccinations. Science 374, 879–882 (2021).
Chang, T., Jacobson, M., Shah, M., Pramanik, R. & Shah, S. B. Financial Incentives and Other Nudges do not Increase COVID-19 Vaccinations Among the Vaccine Hesitant. National Bureau of Economic Research (October 2021); https://www.nber.org/papers/w29403.
Milkman, K. L. et al. A citywide experiment testing the impact of geographically targeted, high-pay-off vaccine lotteries. Nat. Hum. Behav. 6, 1515–1524 (2022).
Lang, D., Esbenshade, L. & Willer, R. Did Ohio’s vaccine lottery increase vaccination rates? A pre-registered, synthetic control study. J. Exp. Pol. Sci. https://doi.org/10.1017/XPS.2021.32 (2022).
Dai, H. et al. Behavioural nudges increase COVID-19 vaccinations. Nature 597, 404–409 (2021).
Rabb, N. et al. Evidence from a statewide vaccination RCT shows the limits of nudges. Nature 604, 404–409 (2022).
Tentori, K. et al. Nudging covid-19 vaccine uptake by changing the default: a randomized controlled trial. Med. Decis. Mak. 42, 837–841 (2022).
Banerjee, A. V., Duflo, E., Glennerster, R. & Kothari, D. Improving immunisation coverage in rural India: clustered randomised controlled evaluation of immunisation campaigns with and without incentives. BMJ 340, c2220 (2010).
Lugada, E. et al. Rapid implementation of an integrated large-scale HIV counseling and testing, malaria, and diarrhea prevention campaign in rural kenya. PLOS ONE 5, e12435 (2010).
Islam, S., Islam, T. & Islam, M. R. New coronavirus variants are creating more challenges to global healthcare system: a brief report on the current knowledge. Clin. Pathol. https://doi.org/10.1177/2632010X221075 (2022).
Dini, E. F., Linkins, R. W. & Sigafoos, J. The impact of computer-generated messages on childhood immunization coverage. Am. J. Prev. Med. 18, 132–139 (2000).
Krieger, J. W., Castorina, J. S., Walls, M. L., Weaver, M. R. & Ciske, S. Increasing influenza and pneumococcal immunization rates: a randomized controlled study of a senior center–based intervention. Am. J. Prev. Med. 18, 123–131 (2000).
Winston, C. A., Mims, A. D. & Leatherwood, K. A. Increasing pneumococcal vaccination in managed care through telephone outreach. Am. J. Manag. Care 13, 581–588 (2007).
Szilagyi, P. G. et al. Effectiveness of a citywide patient immunization navigator program on improving adolescent immunizations and preventive care visit rates. Arch. Pediatr. Adolesc. Med. 165, 547–553 (2011).
Szilagyi, P. G. et al. A randomized trial of the effect of centralized reminder/recall on immunizations and preventive care visits for adolescents. Acad. Pediatr. 13, 204–213 (2013).
O’Leary, S. T. et al. Effectiveness and cost of bidirectional text messaging for adolescent vaccines and well care. Pediatrics 136, e1220–e1227 (2015).
Busso, M, Cristia, J. & Humpage, S. Did you get your shots? Experimental evidence on the role of reminders. J. Health Econ. 44, 226–237 (2015).
Yoo, B.-K. et al. Cost effectiveness analysis of Year 2 of an elementary school-located influenza vaccination program–Results from a randomized controlled trial. BMC Health Serv. Res. 15, 511 (2015).
Herrett, E. et al. Text messaging reminders for influenza vaccine in primary care: a cluster randomised controlled trial (TXT4FLUJAB). BMJ Open 6, e010069 (2016).
Regan, A. K., Bloomfield, L., Peters, I. & Effler, P. V. Randomized controlled trial of text message reminders for increasing influenza vaccination. Ann. Fam. Med. 15, 507–514 (2017).
Kempe, A. et al. Centralized reminder/recall to increase immunization rates in young children: how much bang for the buck? Acad. Pediatr. 17, 330–338 (2017).
Hurley, L. P. et al. RCT of centralized vaccine reminder/recall for adults. Am. J. Prev. Med. 55, 231–239 (2018).
Yokum, D., Lauffenburger, J. C., Ghazinouri, R. & Choudhry, N. K. Letters designed with behavioural science increase influenza vaccination in Medicare beneficiaries. Nat. Hum. Behav. 2, 743–749 (2018).
Powell-Jackson, T., Fabbri, C., Dutt, V., Tougher, S. & Singh, K. Effect and cost-effectiveness of educating mothers about childhood DPT vaccination on immunisation uptake, knowledge, and perceptions in Uttar Pradesh, India: a randomised controlled trial. PLOS Med. 15, e1002519 (2018).
Szilagyi, P. et al. Effect of state immunization information system centralized reminder and recall on HPV vaccination rates. Pediatrics 145, e20192689 (2020).
Yue, M., Wang, Y., Low, C. K., Yoong, J. S.-Y. & Cook, A. R. Optimal design of population-level financial incentives of influenza vaccination for the elderly. Value Health 23, 200–208 (2020).
Kawakatsu, Y., Oyeniyi Adesina, A., Kadoi, N. & Aiga, H. Cost-effectiveness of SMS appointment reminders in increasing vaccination uptake in Lagos, Nigeria: a multi-centered randomized controlled trial. Vaccine 38, 6600–6608 (2020).
Gurfinkel, D. et al. Centralized reminder/recall for human papillomavirus vaccination: findings from two states—A randomized clinical trial. J. Adolesc. Health 69, 579–587 (2021).
Correia, S. REGHDFE: Stata module to perform linear or instrumental-variable regression absorbing any number of high-dimensional fixed effects. Statistical Software Components S457874, Boston College Department of Economics https://ideas.repec.org/c/boc/bocode/s457874.html (2017).
Anderson, M. L. Multiple inference and gender differences in the effects of early intervention: a reevaluation of the Abecedarian, Perry Preschool, and Early Training projects. J. Am. Stat. Assoc. 103, 1481–1495 (2008).
Cameron, A. C., Gelbach, J. B. & Miller, D. L. Bootstrap-based improvements for inference with clustered errors. Rev. Econ. Stat. 90, 414–427 (2008).
Herrett, E. et al. Text messaging reminders for influenza vaccine in primary care: a cluster randomised controlled trial (TXT4FLUJAB). BMJ Open 6, e010069 (2016).
Yue, M. et al. Optimal design of population-level financial incentives of influenza vaccination for the elderly. Value Health 23, 200–208 (2020).
Lazarus, J. V. et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 27, 225–228 (2021).
Acknowledgements
Funding support for this research was provided by Weiss Asset Management, the Dutch Research Council (NWO) (VI.Vidi.191.154), UKRI and the International Growth Centre (SLE - 21148). We are indebted and thankful to study participants for giving their time; O. Sawaneh, A. Turray and our team of enumerators for excellent research assistance; J. W. Ansumana, A. K. Kemoh, N. S. Kamara, T. Boima and the wider team the MoHS of the Government of Sierra Leone; the district organization officers for the districts we went to (A. S. Conteh, A. Sesay, J. Kalokoh, M. Sesay, L. Mansaray, I. Bangura, D. Kanu and A. D. D. Sesay); and the team at Concern Worldwide, Yale Research Initiative on Innovation and Scale (Y-RISE) and the International Growth Centre.
Author information
Authors and Affiliations
Contributions
N.F.M., A.M.M., M.V., S.C. and D.M.K. conceptualized the project. V.R. and M.L. curated the data. V.R., M.L., E.T., M.R. and M.V. undertook formal analyses. N.F.M., A.M.M. and M.V. acquired funding. N.F.M., M.L., M.R., S.C., S.K. and J.N. performed the investigations. N.F.M., A.M.M., M.V., V.R. and M.L. designed the methodology. N.F.M. and M.V. administrated the project. M.L., V.R., S.K., J.N. and M.R. supervised the work. All authors validated the findings. V.R., E.T., M.V. and M.R. visualized the data. A.M.M. and M.V. wrote the first draft, with all authors contributing to writing, and all authors contributed to the review and editing of the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature thanks Jake Bowers and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meriggi, N.F., Voors, M., Levine, M. et al. Last-mile delivery increases vaccine uptake in Sierra Leone. Nature 627, 612–619 (2024). https://doi.org/10.1038/s41586-024-07158-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-024-07158-w
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.