Abstract
High-grade serous ovarian cancers have low survival rates because of their late presentation with extensive peritoneal metastases and frequent chemoresistance1, and require new treatments guided by novel insights into pathogenesis. Here we describe the intrinsic tumour-suppressive activities of interferon-ε (IFNε). IFNε is constitutively expressed in epithelial cells of the fallopian tube, the cell of origin of high-grade serous ovarian cancers, and is then lost during development of these tumours. We characterize its anti-tumour activity in several preclinical models: ovarian cancer patient-derived xenografts, orthotopic and disseminated syngeneic models, and tumour cell lines with or without mutations in Trp53 and Brca genes. We use manipulation of the IFNε receptor IFNAR1 in different cell compartments, differential exposure status to IFNε and global measures of IFN signalling to show that the mechanism of the anti-tumour activity of IFNε involves direct action on tumour cells and, crucially, activation of anti-tumour immunity. IFNε activated anti-tumour T and natural killer cells and prevented the accumulation and activation of myeloid-derived suppressor cells and regulatory T cells. Thus, we demonstrate that IFNε is an intrinsic tumour suppressor in the female reproductive tract whose activities in models of established and advanced ovarian cancer, distinct from other type I IFNs, are compelling indications of potential new therapeutic approaches for ovarian cancer.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Gene expression data were uploaded to GEO with SuperSeries accession number GSE201525. For the ID8 microarrays, raw and processed expression data were deposited with SubSeries accession number GSE201345. For the RNA-seq, the original multiplexed R1 and R2 FASTQ files were de-multiplexed using cutadapt57 (v3.0 with error rate 1 and action none) and uploaded to GEO, along with UMI counts generated by scPipe, with SubSeries accession numbers GSE201337 (PDX RNA-seq) and GSE215261 (Ifnar1−/− ID8 RNA-seq). Source data are provided with this paper.
References
Patch, A.-M. et al. Whole–genome characterization of chemoresistant ovarian cancer. Nature 521, 489–494 (2015).
US Cancer Statistics Working Group. US Cancer Statistics Data Visualizations Tool, based on 2019 submission data (1999–2017). Centers for Disease Control and Prevention www.cdc.gov/cancer/dataviz (2020).
Jayson, G. C., Kohn, E. C., Kitchener, H. C. & Ledermann, J. A. Ovarian cancer. Lancet 384, 1376–1388 (2014).
Tothill, R. W. et al. Novel molecular subtypes of serous and endometrioid ovarian cancer linked to clinical outcome. Clin. Cancer Res. 14, 5198–5208 (2008).
Vaughan, S. et al. Rethinking ovarian cancer: recommendations for improving outcomes. Nat. Rev. Cancer 11, 719–725 (2011).
Dias, M. P., Moser, S. C., Ganesan, S. & Jonkers, J. Understanding and overcoming resistance to PARP inhibitors in cancer therapy. Nat. Rev. Clin. Oncol. 18, 773–791 (2021).
Yeung, T. L. et al. Cellular and molecular processes in ovarian cancer metastasis. Am. J. Physiol. 309, C444–C456 (2015).
Worzfeld, T. et al. The unique molecular and cellular microenvironment of ovarian cancer. Front. Oncol. 7, 24 (2017).
Parker, B. S., Rautela, J. & Hertzog, P. J. Antitumour actions of interferons: implications for cancer therapy. Nat. Rev. Cancer 16, 131–144 (2016).
Fung, K. Y. et al. Interferon-ε protects the female reproductive tract from viral and bacterial infection. Science 339, 1088–1092 (2013).
Stifter, S. A. et al. Defining the distinct, intrinsic properties of the novel type I interferon, IFNϵ. J. Biol. Chem. 293, 3168–3179 (2018).
Hardy, M. P., Owczarek, C. M., Jermiin, L. S., Ejdebäck, M. & Hertzog, P. J. Characterization of the type I interferon locus and identification of novel genes. Genomics 84, 331–345 (2004).
Nagarajan, U. M. et al. Type I interferon signaling exacerbates Chlamydia muridarum genital infection in a murine model. Infect. Immun. 76, 4642–4648 (2008).
Stone, M. L. et al. Epigenetic therapy activates type I interferon signaling in murine ovarian cancer to reduce immunosuppression and tumor burden. Proc. Natl Acad. Sci. USA 114, E10981–E10990 (2017).
Labidi-Galy, S. I. et al. High grade serous ovarian carcinomas originate in the fallopian tube. Nat. Commun. 8, 1093 (2017).
Tan, T. Z. et al. CSIOVDB: a microarray gene expression database of epithelial ovarian cancer subtype. Oncotarget 6, 43843–43852 (2015).
Domcke, S., Sinha, R., Levine, D. A., Sander, C. & Schultz, N. Evaluating cell lines as tumour models by comparison of genomic profiles. Nat. Commun. 4, 2126 (2013).
Greenaway, J., Moorehead, R., Shaw, P. & Petrik, J. Epithelial–stromal interaction increases cell proliferation, survival and tumorigenicity in a mouse model of human epithelial ovarian cancer. Gynecol. Oncol. 108, 385–394 (2008).
Leong, H. S. et al. Efficient molecular subtype classification of high-grade serous ovarian cancer. J. Pathol. 236, 272–277 (2015).
Rodriguez, G. M., Galpin, K. J. C., McCloskey, C. W. & Vanderhyden, B. C. The tumor microenvironment of epithelial ovarian cancer and its influence on response to immunotherapy. Cancers 10, 242 (2018).
Preston, C. C., Goode, E. L., Hartmann, L. C., Kalli, K. R. & Knutson, K. L. Immunity and immune suppression in human ovarian cancer. Immunotherapy 3, 539–556 (2011).
Hwang, S. Y. et al. A null mutation in the gene encoding a type I interferon receptor component eliminates antiproliferative and antiviral responses to interferons α and β and alters macrophage responses. Proc. Natl Acad. Sci. USA. 92, 11284–11288 (1995).
Nesic, K. et al. Acquired RAD51C promoter methylation loss causes PARP inhibitor resistance in high-grade serous ovarian carcinoma. Cancer Res. 81, 4709–4772 (2021).
Ho, G.-Y. et al. Epithelial-to-mesenchymal transition supports ovarian carcinosarcoma tumorigenesis and confers sensitivity to microtubule-targeting with eribulin. Cancer Res. 82, 4457–4473 (2022).
Ishizuka, J. J. et al. Loss of ADAR1 in tumours overcomes resistance to immune checkpoint blockade. Nature 565, 43–48 (2019).
Salomoni, P. & Pandolfi, P. P. The role of PML in tumor suppression. Cell 108, 165–170 (2002).
Hou, J. et al. Gene expression profiling to predict and assess the consequences of therapy-induced virus eradication in chronic hepatitis C virus infection. J. Virol. 88, 12254–12264 (2014).
Walton, J. et al. CRISPR/Cas9-mediated Trp53and Brca2 knockout to generate improved murine models of ovarian high-grade serous carcinoma. Cancer Res. 76, 6118–6129 (2016).
Chen, L. et al. Hepatic gene expression discriminates responders and nonresponders in treatment of chronic hepatitis C viral infection. Gastroenterology 128, 1437–1444 (2005).
François-Newton, V. et al. USP18-based negative feedback control is induced by type I and type III interferons and specifically inactivates interferon α response. PLoS ONE 6, e22200 (2011).
Lheureux, S., Braunstein, M. & Oza, A. M. Epithelial ovarian cancer: evolution of management in the era of precision medicine. CA Cancer J. Clin. 69, 280–304 (2019).
Barriga, F. M. et al. MACHETE identifies interferon-encompassing chromosome 9p21.3 deletions as mediators of immune evasion and metastasis. Nat. Cancer 3, 1367–1385 (2022).
Bidwell, B. N. et al. Silencing of Irf7 pathways in breast cancer cells promotes bone metastasis through immune escape. Nat. Med. 18, 1224–1231 (2012).
Capobianco, A., Cottone, L., Monno, A., Manfredi, A. A. & Rovere-Querini, P. The peritoneum: healing, immunity, and diseases. J. Pathol. 243, 137–147 (2017).
Mitra, A. K. in Tumor Metastasis (ed. Xu, K.) Ch. 3 https://doi.org/10.5772/64700 (IntechOpen, 2016).
Roby, K. F. et al. Development of a syngeneic mouse model for events related to ovarian cancer. Carcinogenesis 21, 585–591 (2000).
Stifter, S. A. et al. Purification and biological characterization of soluble, recombinant mouse IFNβ expressed in insect cells. Protein Expr. Purif. 94, 7–14 (2014).
Brinkman, E. K., Chen, T., Amendola, M. & Van Steensel, B. Easy quantitative assessment of genome editing by sequence trace decomposition. Nucleic Acids Res. 42, e168 (2014).
R Core Team. R: A Language and Environment for Statistical Computing. https://www.r-project.org (R Foundation for Statistical Computing, 2019).
Ritchie, M. E. et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47 (2015).
Davis, S. & Meltzer, P. S. GEOquery: a bridge between the Gene Expression Omnibus (GEO) and BioConductor. Bioinformatics 23, 1846–1847 (2007).
Durinck, S. et al. BioMart and Bioconductor: a powerful link between biological databases and microarray data analysis. Bioinformatics 21, 3439–3440 (2005).
Durinck, S., Spellman, P. T., Birney, E. & Huber, W. Mapping identifiers for the integration of genomic datasets with the R/Bioconductor package biomaRt. Nat. Protoc. 4, 1184–1191 (2009).
Ritchie, M. E. et al. Empirical array quality weights in the analysis of microarray data. BMC Bioinformatics 7, 261 (2006).
McCarthy, D. J. & Smyth, G. K. Testing significance relative to a fold-change threshold is a TREAT. Bioinformatics 25, 765–771 (2009).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).
Alhamdoosh, M. et al. Combining multiple tools outperforms individual methods in gene set enrichment analyses. Bioinformatics 33, 414–424 (2017).
Tian, L. et al. scPipe: a flexible R/Bioconductor preprocessing pipeline for single-cell RNA-sequencing data. PLoS Comput. Biol. 14, e1006361 (2018).
Liao, Y., Smyth, G. K. & Shi, W. The R package Rsubread is easier, faster, cheaper and better for alignment and quantification of RNA sequencing reads. Nucleic Acids Res. 47, e47 (2019).
Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
Wakefield, M. J. Xenomapper: mapping reads in a mixed species context. J. Open Source Softw. 1, 18 (2016).
Robinson, M. D., McCarthy, D. J. & Smyth, G. K. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 26, 139–140 (2010).
Robinson, M. D. & Oshlack, A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol. 11, R25 (2010).
Liu, R. et al. Why weight? Modelling sample and observational level variability improves power in RNA-seq analyses. Nucleic Acids Res. 43, e97–e97 (2015).
Wu, D. & Smyth, G. K. Camera: a competitive gene set test accounting for inter-gene correlation. Nucleic Acids Res. 40, e133 (2012).
Phipson, B., Lee, S., Majewski, I. J., Alexander, W. S. & Smyth, G. K. Robust hyperparameter estimation protects against hypervariable genes and improves power to detect differential expression. Ann. Appl. Stat. 10, 946–963 (2016).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet.journal 17, 10 (2011).
Acknowledgements
This work was supported by project grants from the National Health and Medical Research Council of Australia (NHMRC) to P.J.H., M.D.T., D.D.L.B. and the Stafford Fox Medical Research Foundation to C.L.S. This work was supported from the Operational Infrastructure Fund of the State Government of Victoria. Z.R.C.M. was supported by an Australian Postgraduate Award; M.B. and A.N.S. are supported by the Ovarian Cancer Foundation of Australia; N.E.M. was supported by a Fielding Foundation Fellowship; P.J.H. was supported by NHMRC Senior Principal Research fellowship and B.S.P. and C.L.S. were supported by Victorian Cancer Agency fellowship. The authors acknowledge E. M. Swisher, for BROCA sequencing of PDX; S. Stoev, R. Hancock and K. Barber for technical assistance with the PDX studies; use of the services and facilities at the Monash Histology Platform, MHTP FlowCore, medical genomics and animal services and Micromon Genomics at Monash University; and R. Smith for assistance with preparation of the manuscript. This work was also supported by the US Office of the Assistant Secretary of Defense for Health Affairs through the Ovarian Cancer Research Program under award no. W81XWH-15-1-0106. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the US Department of Defense. In conducting research using animals, the investigators adhered to the laws of Australia, the USA and regulations of the US Department of Agriculture, and received ethical approval for this research from the Animal Ethics Committees of Monash University and the Walter and Eliza Hall Institute of Medical Research. In conducting research using human tissues, the investigators adhered to the laws of Australia and received ethical approval for this research from the Walter and Eliza Hall Institute of Medical Research Human Research Ethics Committee.
Author information
Authors and Affiliations
Consortia
Contributions
Z.R.C.M. and N.K.C. were involved in performing mouse model experiments, analysis of endpoints, immunophenotyping, in vitro tumour growth assays, conceptualization, interpretation and write up of the work and editing the manuscript. N.E.M. was involved in assays of immune effects of IFNε, conceptualization and interpretation of data. C.J.V. and G.-Y.H. performed xenograft models, planned and interpreted data. L.J.G. performed bioinformatics analysis of RNA-seq and microarrays and contributed to editing the manuscript. A.Y.M., S.S.L. and N.A.d.W. produced, purified and assayed recombinant IFNs. J.A.G. performed microarray and RNA-seq experiments and analysis. M.D.T., G.W.-M., L.Y., S.R. and E.d.G. provided technical assistance and contributed to planning and analysis of animal models. N.B. and B.S.P. analysed tumour responses by IHC and analysed results. E.L.C. and M.J.W. performed genetic and bioinformatic analysis and tumour genomic data curation. M.B. and A.N.S. provided cell lines and advised and planned tumour growth experiments. O.M. and Australian Ovarian Cancer Study provided patient and tumour data, curated the databases and contributed to interpretation of data. I.A.M. provided ID8 tumour models and advised on planning and interpretation of results. D.D.L.B. advised on strategy and planning of tumour experiments and genomic data analysis. C.L.S. provided human tumour samples and associated data, performed xenografts, planned experiments and interpreted results. N.M.B. and P.J.H. performed conceptualization, methodology, formal analysis, investigation, contribution to original manuscript draft, review and editing the manuscript, supervision and acquisition of funding. All authors had input into review or editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors P.J.H., Z.R.C.M., N.B., S.S.L., N.A.d.W., N.E.M. and A.Y.M. are listed as inventors on the patent PCT/AU2018/050054 regarding use of IFNε as a method of treatment for cancer.
Peer review
Peer review information
Nature thanks Tyler Curiel and Kevin Elias for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Suppression of epithelial IFNε in high-grade serous ovarian cancer and IFNε effects on “primary” orthotopic tumour tissue in the ID8 model of ovarian cancer.
(a) mRNA expression (mean ± interquartile range) of IFNε in the CSIOVDB cohort13. Significance was determined by Mann-Whitney U tests compared to healthy Fallopian tube epithelium (FTE). Doubling times of (b) CaOV3 and (c) OVCAR4 cell cultures treated with 1–1,000 IU/ml of IFNε for 48 h. Cell proliferation was measured using xCELLigence. Data is presented as mean ± SD of n = 3 independent experiments performed in technical quadruplicates. Significance was determined by one-way ANOVA with Dunnett’s multiple comparisons test. (d–i) ID8 cells were implanted into C57BL/6J mice via intrabursal injection of the left ovary to form orthotopic ovarian tumours and peritoneal metastases. (d) Images show excised ovaries and uterine horn of mice treated with PBS or IFNε (500 IU per dose); (e) weights of orthotopic tumour-bearing ovaries from mice treated with PBS or IFNε (50 or 500 IU per dose) (“developing” model) and mice that commenced treatment with IFNε or IFNβ (500 IU per dose) 4 weeks post-implantation (“established” model). Data is presented as mean ± SD of individual mice, n = 6 mice per group. (f–i) Multiplex IHC staining of IRF9 (f,g) and CD3 (h,i) expression in “primary” ID8 ovarian tumors derived from vehicle- or IFNε-treated mice (500 IU per dose) as shown for 2 mice per group as representative of n = 5. Data shown are means ± SD of individual data points. Significance was determined by unpaired two-tailed t-test. Scale bars = 200 μm. ****p < 0.0001, ***p < 0.001, **p < 0.01, *p < 0.05.
Extended Data Fig. 2 Disease scores and immunophenotyping of peritoneal cells in orthotopic and disseminated models of ovarian cancer.
Ascites volume and peritoneal haemorrhaging (RBC count within peritoneal fluid) were measured in the “developing”, “established” (a,c), and “advanced” (b,d) models of ovarian cancer, as described in Fig. 2 and the Methods. Data are presented as means ± SD of individual mice: in both “developing” and “established” models n = 6 mice per treatment, in the “advanced” model n = 5 mice per IFN treatment and n = 3 mice treated with PBS. Significance was determined by Kruskal-Wallis test with Dunn’s multiple comparisons test (a,c), or one-way ANOVA with Dunnett’s multiple comparisons test (b,d). The numbers of immune cells in peritoneal lavage fluid from mice with (e) “developing” or “established” orthotopic tumours, and (f) “advanced” disseminated tumours were determined by flow cytometry. Data shown are means of immune cell counts measured for each treatment group and presented in stacked bar graphs. Significance was determined by two-way ANOVA with Tukey’s multiple comparisons test. IFN-driven immune cell activation in orthotopic ovarian tumour models demonstrated by (g) PD1 levels on CD4+ T cells and CD69 expression on (h) CD4+ T cells, (i) CD8+ T cells and (j) NK cells, as detected by flow cytometry. Data are presented as means ± SD of individual data points, in both “developing” and “established” models n = 6 mice per group. Significance was determined by one-way ANOVA with Dunnett’s multiple comparisons test. ****p < 0.0001, ***p < 0.001, **p < 0.01, *p < 0.05. NT: non-tumour bearing; RBC: red blood cells.
Extended Data Fig. 3 Mechanisms of intrinsic anti-tumour activities of IFNε in vitro.
(a) CD107a expression was measured as a marker of degranulation on NK cells from in vivo primed PECs co-cultured with ID8 cells. Data is presented as mean ± SD of individual mice (n = 3 per group). Significance was determined by unpaired two-tailed t-test. (b) Plots show induction of apoptosis (Annexin V-FITC/PI staining) in ID8 cells treated with IFNε or PBS, as measured by flow cytometry. Data presented as representative plots from n = 6 independent experiments. (c) Plots show inhibition of proliferation of ID8 cells treated with 100 or 1,000 IU/ml of IFNε (top panel) or IFNβ (bottom panel) for 48 h. Cell proliferation was measured by xCELLigence and is representative of n = 3 independent experiments. (d) Heat maps of log2 fold changes comparing IFN-treated ID8 cells to untreated controls, showing differentially expressed genes associated with cell cycle and apoptosis or cell death gene sets from the Molecular Signatures Database (scale truncated to ± 5). Expression data is derived from n = 3 independent experiments, performed in technical triplicate. (e) Images show examples of characteristic nodule formation throughout the mesentery (dotted lines) and adhered to the peritoneal wall (black arrows) of WT and Ifnar1−/− mice with disseminated tumour treated with PBS or IFNε. (f) Stacked bar graph summarising the number of immune cells present in peritoneal lavage fluid from WT and Ifnar1−/− mice as described in Fig. 3. Data shown are means of immune cell counts measured for each treatment group and genotype. Significance was determined by two-way ANOVA with Tukey’s multiple comparisons test, n = 6 mice per IFNε treatment group, n = 5 WT mice treated with PBS, n = 8 Ifnar1−/− mice treated with PBS. ***p < 0.001, *p < 0.05. NT: non-tumour bearing.
Extended Data Fig. 4 Effect of huIFNε, huIFNβ and muIFNε in PDX models of HGSOC.
Two PDX models of HGSOC were performed using tumours obtained from two different patients, as described in the Methods. PDX #111 demonstrated induction of ISGs with huIFNε treatment and was designated a “responder” to IFNε. (a) Total number of metastatic deposits found in the peritoneal cavity in mice bearing “responder” PDX #111 tumours, treated with either PBS or equivalent IU of huIFNβ, huIFNε or muIFNε. Data is presented as mean ± SD of individual mice. Significance was determined by Mann-Whitney U test. (b,c) Plots of log2 fold changes of significantly differentially expressed genes in tumour cells from (b) huIFNε vs huIFNβ and (c) huIFNε vs muIFNε treated mice, highlighting significantly differentially up- and down-regulated genes with huIFNε treatment (red and blue respectively). (d) Heat map of RNA-seq analysis of mice bearing tumours from “responder” PDX #111 and “non-responder” PDX #183, showing all genes identified from the Reactome IFN alpha/beta signalling gene set. Genes in bold were significantly induced by huIFNε in the “responder” PDX and also had significantly higher basal levels in the “non-responder” PDX (scale truncated to ± 6). For PDX #111, n = 6 mice per treatment group. For PDX #183, n = 7 mice treated with PBS or huIFNβ, n = 6 mice treated with huIFNε or muIFNε.
Extended Data Fig. 5 Effect of IFNε in the human oncogene mutated ID8TB model of advanced ovarian cancer.
(a–d) ID8TB cells were implanted via intraperitoneal injection and administered muIFNε therapy (100–1,000 IU/dose), as described previously. Quantitation of (a) the total number of peritoneal metastases, (b) mesentery tumour burden, (c) volume of ascites fluid, and (d) peritoneal haemorrhage score. Data are expressed as means ± SD of individual mice. Significance was determined by Kruskal-Wallis test with Dunn’s multiple comparisons test. (e–o) ID8TB cells were implanted via intraperitoneal injection and administered muIFNε therapy (500 IU/dose), as described previously. Quantitation of (e) the total number of peritoneal metastases, (f) mesentery tumour burden, (g) volume of ascites fluid, and (h) degree of peritoneal haemorrhaging (RBC count within peritoneal lavage fluid). The numbers of peritoneal lavage (i) lymphocytes (CD4+ T cells, CD8+ T cells, Tregs and NK cells) and (j) myeloid cells (MDSC, neutrophils, monocytes and dendritic cells) were detected by flow cytometry. Data shown are means of immune cell counts measured for each treatment group, presented in stacked bar graphs. Significance was determined by two-way ANOVA with Tukey’s multiple comparisons test. IFNε-driven immune cell activation in peritoneal lymphocytes demonstrated by CD69 expression on (k) NK cells, (l) CD4+ T cells, and (m) CD8+ T cells, or PD1 expression on (n) CD4+ and (o) CD8+ T cells, as detected by flow cytometry. Data are expressed as means ± SD of individual mice. Significance was determined by unpaired two-tailed t-test. For a–d, n = 5 mice in the NT group, n = 10 mice in all other groups. For e–o, n = 9 mice treated with PBS, n = 8 mice treated with IFNε. ****p < 0.0001, ***p < 0.001, **p < 0.01, *p < 0.05. RBC: red blood cell; Treg: T regulatory cell; DC: dendritic cell; NT: non-tumour bearing.
Extended Data Fig. 6 Validation of Ifnar1−/− ID8TB cells.
(a) Tracking of Indels by Decomposition (TIDE) analysis of the 1CF10 Ifnar1−/− cell clone (green lines) versus empty vector (EV) transfected control ID8TB cells (black lines), demonstrating increased sequence discordance around and following the expected cut site. (b) Inference of CRISPR Edits (ICE) analysis depicting a single ‘G’ base insertion at base 56 in the edited sample (1CF10) compared to the control (EV) sample. This insertion is anticipated to produce a frame-shift error and consequent introduction of an early stop codon. (c) Histograms depict surface IFNAR1 staining in WT and 1CF10 cells stained with anti-IFNAR1, and WT cells stained with an isotype control antibody. The MFI values for IFNAR1/IgG in each sample are listed to the right of the histogram. (d-e) EV and 1CF10 cells were treated in technical triplicate in vitro with 10,000 IU/ml muIFNβ or left untreated (UT). Gene expression was measured by RNA-seq: (d) heat map depicts significant differences in Hallmark gene sets between UT EV and 1CF10 cells (basal gene expression) and between UT and IFNβ stimulated EV and 1CF10 cells (IFN response). Heat map colour shows the average log2 fold change of genes in each gene set (scale truncated to ± 2); individual p values are presented on the figure. (e) Heat map depicting log2 expression of all genes identified from the Hallmark IFN alpha response gene set, relative to EV UT controls (scale truncated to ± 6). Genes in bold were significantly induced by IFNβ in the EV cellls and also had significantly lower basal levels in the UT 1CF10 cells (f) Proliferation of EV and 1CF10 cells treated with muIFNε or muIFNβ, expressed as percentage CFSE MFI of vehicle control-treated cells, with increased % CFSE MFI indicative of inhibition of cell proliferation. Data depicts mean ± SD of n = 4 independent experiments. Significance was determined by two-way ANOVA with Dunnett’s multiple comparisons test; p values for relevant comparisons depicted.
Extended Data Fig. 7 Immunophenotyping of Ifnar1−/− ID8TB model of advanced ovarian cancer.
WT or Ifnar1−/− ID8TB cells were implanted i.p. prior to commencing muIFNε treatment. (a) The numbers of peritoneal lavage myeloid cells (MDSC, neutrophils, monocytes, dendritic cells, large peritoneal macrophages (LPM), small peritoneal macrophages (SPM), F480loMHCII− cells and SiglecF+ cells) were detected by flow cytometry. (b) The numbers of peritoneal lavage lymphocytes (CD4+ T cells, CD8+ T cells, Tregs, B cells and NK cells) were detected by flow cytometry. Data shown for a & b are means of immune cell counts measured for each treatment group, presented in stacked bar graphs. (c) Pearson correlation matrix of all disease scores and measurements of peritoneal immune cell numbers, proliferation and activation by flow cytometry.
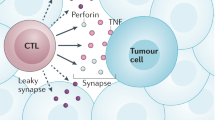
Extended Data Fig. 8 Summary of the mechanism of anti-tumour actions of IFNε.
Wild type (WT) tumours grow in WT mice treated with PBS (i); but tumours shrink when treated with IFNε (ii); with unresponsive Ifnar1−/− mouse immune cells (iii), tumours shrink partially due to the direct actions of IFNε on the responsive tumour cells (1), but inhibition is less than in model (ii); with unresponsive Ifnar1−/− tumour cells (iv), IFNε activates immune cells (2) to kill tumour cells to a greater degree than model (iii) and similar to the inhibition in model (ii). IFNε-treated tumour cells can produce non-IFN signals to immune cells (3) which influence tumour growth in scenarios (ii) and (iii). Created with Biorender.com.
Supplementary information
Supplementary Figures
Supplementary Figs. 1–4, which show the various gating strategies used.
Source data
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marks, Z.R.C., Campbell, N.K., Mangan, N.E. et al. Interferon-ε is a tumour suppressor and restricts ovarian cancer. Nature 620, 1063–1070 (2023). https://doi.org/10.1038/s41586-023-06421-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-023-06421-w
This article is cited by
-
A protective role for interferon-ε in ovarian cancer
Nature Reviews Immunology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.