Abstract
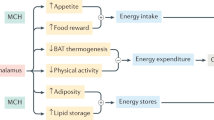
The state of somatic energy stores in metazoans is communicated to the brain, which regulates key aspects of behaviour, growth, nutrient partitioning and development1. The central melanocortin system acts through melanocortin 4 receptor (MC4R) to control appetite, food intake and energy expenditure2. Here we present evidence that MC3R regulates the timing of sexual maturation, the rate of linear growth and the accrual of lean mass, which are all energy-sensitive processes. We found that humans who carry loss-of-function mutations in MC3R, including a rare homozygote individual, have a later onset of puberty. Consistent with previous findings in mice, they also had reduced linear growth, lean mass and circulating levels of IGF1. Mice lacking Mc3r had delayed sexual maturation and an insensitivity of reproductive cycle length to nutritional perturbation. The expression of Mc3r is enriched in hypothalamic neurons that control reproduction and growth, and expression increases during postnatal development in a manner that is consistent with a role in the regulation of sexual maturation. These findings suggest a bifurcating model of nutrient sensing by the central melanocortin pathway with signalling through MC4R controlling the acquisition and retention of calories, whereas signalling through MC3R primarily regulates the disposition of calories into growth, lean mass and the timing of sexual maturation.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data used in the genetic association analyses are available from the UKBB upon application (https://www.ukbiobank.ac.uk). Data from the Fenland cohort can be requested by bona fide researchers for specified scientific purposes via the study website (https://www.mrc-epid.cam.ac.uk/research/studies/fenland/information-for-researchers/). Data will either be shared through an institutional data sharing agreement or arrangements will be made for analyses to be conducted remotely without the necessity for data transfer. The EPIC-Norfolk data can be requested by bona fide researchers for specified scientific purposes via the study website (https://www.mrc-epid.cam.ac.uk/research/studies/epic-norfolk/). Data will either be shared through an institutional data sharing agreement or arrangements will be made for analyses to be conducted remotely without the need for data transfer. ALSPAC data are available through a system of managed open access. Full details of the cohort and study design have been previously described and are available at http://www.alspac.bris.ac.uk. Please note that the study website contains details of all the data that are available through a fully searchable data dictionary and variable search tool (http://www.bristol.ac.uk/alspac/researchers/our-data/). Data for this project were accessed under the project number B2891. The application steps for ALSPAC data access are as follows: (1) please read the ALSPAC access policy, which describes the process of accessing the data in detail and outlines the costs associated with doing so. (2) You may also find it useful to browse the fully searchable research proposals database, which lists all research projects that have been approved since April 2011. (3) Please submit your research proposal for consideration by the ALSPAC Executive Committee. You will receive a response within 10 working days to advise you whether your proposal has been approved. If you have any questions about accessing data, please email alspac-data@bristol.ac.uk. For Genes & Health, data are available via http://www.genesandhealth.org/. Publicly available GWAS datasets utilized in the phenome-wide association study analyses are available from the Neale laboratory (http://www.nealelab.is/uk-biobank), Open Targets Genetics (https://genetics.opentargets.org/), Global Biobank Engine (https://biobankengine.stanford.edu/), Open GWAS IEU (https://gwas.mrcieu.ac.uk/) and Phenoscanner (http://www.phenoscanner.medschl.cam.ac.uk/). Mouse single-cell RNA sequencing data are available from Gene Expression Omnibus (GEO) accessions GSE93374, GSE87544, GSE92707 and GSE74672.
Code availability
Programming scripts were written to assist in the execution of publicly available functions and computer programs in our compute environment. For access to these scripts, readers may contact the corresponding author.
References
Friedman, J. M. The function of leptin in nutrition, weight, and physiology. Nutr. Rev. 60, S1–S14; discussion S68–S84, S85–S87 (2002).
Cone, R. D. Anatomy and regulation of the central melanocortin system. Nat. Neurosci. 8, 571–578 (2005).
Cowley, M. A. et al. Leptin activates anorexigenic POMC neurons through a neural network in the arcuate nucleus. Nature 411, 480–484 (2001).
Hill, J. W. et al. Direct insulin and leptin action on pro-opiomelanocortin neurons is required for normal glucose homeostasis and fertility. Cell Metab. 11, 286–297 (2010).
Varela, L. & Horvath, T. L. Leptin and insulin pathways in POMC and AgRP neurons that modulate energy balance and glucose homeostasis. EMBO Rep. 13, 1079–1086 (2012).
Chen, A. S. et al. Role of the melanocortin-4 receptor in metabolic rate and food intake in mice. Transgenic Res. 9, 145–154 (2000).
Fan, W., Boston, B. A., Kesterson, R. A., Hruby, V. J. & Cone, R. D. Role of melanocortinergic neurons in feeding and the agouti obesity syndrome. Nature 385, 165–168 (1997).
Vaisse, C., Clement, K., Guy-Grand, B. & Froguel, P. A frameshift mutation in human MC4R is associated with a dominant form of obesity. Nat. Genet. 20, 113–114 (1998).
Yeo, G. S. et al. A frameshift mutation in MC4R associated with dominantly inherited human obesity. Nat. Genet. 20, 111–112 (1998).
Huszar, D. et al. Targeted disruption of the melanocortin-4 receptor results in obesity in mice. Cell 88, 131–141 (1997).
Farooqi, I. S. et al. Clinical spectrum of obesity and mutations in the melanocortin 4 receptor gene. N. Engl. J. Med. 348, 1085–1095 (2003).
Krakoff, J. et al. Lower metabolic rate in individuals heterozygous for either a frameshift or a functional missense MC4R variant. Diabetes 57, 3267–3272 (2008).
Brown, P. I. & Brasel, J. in The Malnourished Child Nestlé Nutrition Workshop Series (eds Lewinter-Suskind, L. & Suskind, R. M.) 213–228 (Nestlé Nutrition Institute and Vevey/Raven Press, 1990).
Clement, K. et al. A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction. Nature 392, 398–401 (1998).
Strobel, A., Issad, T., Camoin, L., Ozata, M. & Strosberg, A. D. A leptin missense mutation associated with hypogonadism and morbid obesity. Nat. Genet. 18, 213–215 (1998).
Roselli-Rehfuss, L. et al. Identification of a receptor for gamma melanotropin and other proopiomelanocortin peptides in the hypothalamus and limbic system. Proc. Natl Acad. Sci. USA 90, 8856–8860 (1993).
Gantz, I. et al. Molecular cloning of a novel melanocortin receptor. J. Biol. Chem. 268, 8246–8250 (1993).
Butler, A. A. et al. A unique metabolic syndrome causes obesity in the melanocortin-3 receptor-deficient mouse. Endocrinology 141, 3518–3521 (2000).
Chen, A. S. et al. Inactivation of the mouse melanocortin-3 receptor results in increased fat mass and reduced lean body mass. Nat. Genet. 26, 97–102 (2000).
Renquist, B. J. et al. Melanocortin-3 receptor regulates the normal fasting response. Proc. Natl Acad. Sci. USA 109, E1489–E1498 (2012).
Wood, A. R. et al. Defining the role of common variation in the genomic and biological architecture of adult human height. Nat. Genet. 46, 1173–1186 (2014).
Day, F. R. et al. Genomic analyses identify hundreds of variants associated with age at menarche and support a role for puberty timing in cancer risk. Nat. Genet. 49, 834–841 (2017).
Demidowich, A. P., Jun, J. Y. & Yanovski, J. A. Polymorphisms and mutations in the melanocortin-3 receptor and their relation to human obesity. Biochim. Biophys. Acta Mol. Basis Dis. 1863, 2468–2476 (2017).
Marouli, E. et al. Rare and low-frequency coding variants alter human adult height. Nature 542, 186–190 (2017).
Mencarelli, M. et al. Rare melanocortin-3 receptor mutations with in vitro functional consequences are associated with human obesity. Hum. Mol. Genet. 20, 392–399 (2011).
Zegers, D. et al. Identification of three novel genetic variants in the melanocortin-3 receptor of obese children. Obesity (Silver Spring) 19, 152–159 (2011).
Lee, Y. S., Poh, L. K. & Loke, K. Y. A novel melanocortin 3 receptor gene (MC3R) mutation associated with severe obesity. J. Clin. Endocrinol. Metab. 87, 1423–1426 (2002).
Studenski, S. A. et al. The FNIH Sarcopenia Project: rationale, study description, conference recommendations, and final estimates. J. Gerontol. A Biol. Sci. Med. Sci. 69, 547–558 (2014).
Kim, T. N. et al. Comparisons of three different methods for defining sarcopenia: an aspect of cardiometabolic risk. Sci. Rep. 7, 6491 (2017).
Boyd, A. et al. Cohort profile: the ‘children of the 90s’-the index offspring of the Avon Longitudinal Study of Parents and Children. Int. J. Epidemiol. 42, 111–127 (2013).
Wade, K. H. et al. Loss-of-function mutations in the melanocortin 4 receptor in a UK birth cohort. Nat. Med. 27, 1088–1096 (2021).
Lotta, L. A. et al. A cross-platform approach identifies genetic regulators of human metabolism and health. Nat. Genet. 53, 54–64 (2021).
Khaw, K. T. et al. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med. 5, e12 (2008).
Pietzner, M. et al. Plasma metabolites to profile pathways in noncommunicable disease multimorbidity. Nat. Med. 27, 471–479 (2021).
Tapanainen, J. et al. Short and long term effects of growth hormone on circulating levels of insulin-like growth factor-I (IGF-I), IGF-binding protein-1, and insulin: a placebo-controlled study. J. Clin. Endocrinol. Metab. 73, 71–74 (1991).
Finer, S. et al. Cohort profile: East London Genes & Health (ELGH), a community-based population genomics and health study in British Bangladeshi and British Pakistani people. Int. J. Epidemiol. 49, 20–21i (2020).
de Onis, M. et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 85, 660–667 (2007).
Campbell, J. N. et al. A molecular census of arcuate hypothalamus and median eminence cell types. Nat. Neurosci. 20, 484–496 (2017).
Sweeney, P. et al. The melanocortin-3 receptor is a pharmacological target for the regulation of anorexia. Sci. Transl. Med. 13, eabd6434 (2021).
Lam, B. Y. H. et al. Heterogeneity of hypothalamic pro-opiomelanocortin-expressing neurons revealed by single-cell RNA sequencing. Mol. Metab. 6, 383–392 (2017).
Romanov, R. A. et al. Molecular interrogation of hypothalamic organization reveals distinct dopamine neuronal subtypes. Nat. Neurosci. 20, 176–188 (2017).
Chen, R., Wu, X., Jiang, L. & Zhang, Y. Single-cell RNA-seq reveals hypothalamic cell diversity. Cell Rep. 18, 3227–3241 (2017).
Backholer, K. et al. Kisspeptin cells in the ewe brain respond to leptin and communicate with neuropeptide Y and proopiomelanocortin cells. Endocrinology 151, 2233–2243 (2010).
Cocchi, D., De Gennaro Colonna, V., Bagnasco, M., Bonacci, D. & Muller, E. E. Leptin regulates GH secretion in the rat by acting on GHRH and somatostatinergic functions. J. Endocrinol. 162, 95–99 (1999).
Tannenbaum, G. S., Gurd, W. & Lapointe, M. Leptin is a potent stimulator of spontaneous pulsatile growth hormone (GH) secretion and the GH response to GH-releasing hormone. Endocrinology 139, 3871–3875 (1998).
Wang, L. & Moenter, S. M. Differential roles of hypothalamic AVPV and arcuate kisspeptin neurons in estradiol feedback regulation of female reproduction. Neuroendocrinology 110, 172–184 (2020).
Dunger, D. B., Ahmed, M. L. & Ong, K. K. Effects of obesity on growth and puberty. Best Pract. Res. Clin. Endocrinol. Metab. 19, 375–390 (2005).
Hauspie, R. C., Vercauteren, M. & Susanne, C. Secular changes in growth and maturation: an update. Acta Paediatr. Suppl. 423, 20–27 (1997).
Kuhnen, P. et al. Proopiomelanocortin deficiency treated with a melanocortin-4 receptor agonist. N. Engl. J. Med. 375, 240–246 (2016).
Roa, J. & Herbison, A. E. Direct regulation of GnRH neuron excitability by arcuate nucleus POMC and NPY neuron neuropeptides in female mice. Endocrinology 153, 5587–5599 (2012).
Manfredi-Lozano, M. et al. Defining a novel leptin–melanocortin–kisspeptin pathway involved in the metabolic control of puberty. Mol. Metab. 5, 844–857 (2016).
Salomon, F., Cuneo, R. C., Hesp, R. & Sonksen, P. H. The effects of treatment with recombinant human growth hormone on body composition and metabolism in adults with growth hormone deficiency. N. Engl. J. Med. 321, 1797–1803 (1989).
Doherty, T. J. Invited review: aging and sarcopenia. J. Appl. Physiol. 95, 1717–1727 (2003).
McCance, R. A. & Widdowson, E. M. The determinants of growth and form. Proc. R. Soc. Lond. B Biol. Sci. 185, 1–17 (1974).
Sudlow, C. et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Eastwood, S. V. et al. Algorithms for the capture and adjudication of prevalent and incident diabetes in UK Biobank. PLoS ONE 11, e0162388 (2016).
Powell, R. M. et al. Development and validation of total and regional body composition prediction equations from anthropometry and single frequency segmental bioelectrical impedance with DEXA. Preprint at medRxiv https://doi.org/10.1101/2020.12.16.20248330 (2020).
Zhao, Y. et al. GIGYF1 loss of function is associated with clonal mosaicism and adverse metabolic health. Nat. Commun. 12, 4178 (2021).
McLaren, W. et al. The Ensembl variant effect predictor. Genome Biol. 17, 122 (2016).
Rentzsch, P., Witten, D., Cooper, G. M., Shendure, J. & Kircher, M. CADD: predicting the deleteriousness of variants throughout the human genome. Nucleic Acids Res. 47, D886–D894 (2019).
Loh, P. R. et al. Efficient Bayesian mixed-model analysis increases association power in large cohorts. Nat. Genet. 47, 284–290 (2015).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 4, 7 (2015).
Van Hout, C. V. et al. Exome sequencing and characterization of 49,960 individuals in the UK Biobank. Nature 586, 749–756 (2020).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562, 203–209 (2018).
Millard, L. A. C., Davies, N. M., Gaunt, T. R., Davey Smith, G. & Tilling, K. Software application profile: PHESANT: a tool for performing automated phenome scans in UK Biobank. Int. J. Epidemiol. 47, 29–35 (2018).
Ghoussaini, M. et al. Open Targets Genetics: systematic identification of trait-associated genes using large-scale genetics and functional genomics. Nucleic Acids Res. 49, D1311–D1320 (2021).
Elsworth, B. et al. The MRC IEU OpenGWAS data infrastructure. Preprint at bioRxiv https://doi.org/10.1101/2020.08.10.244293 (2020).
McInnes, G. et al. Global Biobank Engine: enabling genotype–phenotype browsing for biobank summary statistics. Bioinformatics 35, 2495–2497 (2019).
Kamat, M. A. et al. PhenoScanner V2: an expanded tool for searching human genotype–phenotype associations. Bioinformatics 35, 4851–4853 (2019).
Howe, L. D. et al. Changes in ponderal index and body mass index across childhood and their associations with fat mass and cardiovascular risk factors at age 15. PLoS ONE 5, e15186 (2010).
Frysz, M., Howe, L. D., Tobias, J. H. & Paternoster, L. Using SITAR (superimposition by translation and rotation) to estimate age at peak height velocity in Avon Longitudinal Study of Parents and Children. Wellcome Open Res. 3, 90 (2018).
Li, H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. Preprint at arXiv https://export.arxiv.org/abs/1303.3997 (2013).
Koboldt, D. C. et al. VarScan 2: somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res. 22, 568–576 (2012).
Wade, K. H. et al. Loss-of-function mutations in the melanocortin 4 receptor in a UK birth cohort. Nat. Med. 27, 1088–1096 (2021).
Lindsay, T. et al. Descriptive epidemiology of physical activity energy expenditure in UK adults (the Fenland study). Int. J. Behav. Nutr. Phys. Act. 16, 126 (2019).
Williams, S. A. et al. Plasma protein patterns as comprehensive indicators of health. Nat. Med. 25, 1851–1857 (2019).
Pietzner, M. et al. Genetic architecture of host proteins involved in SARS-CoV-2 infection. Nat. Commun. 11, 6397 (2020).
Willer, C. J., Li, Y. & Abecasis, G. R. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics 26, 2190–2191 (2010).
Day, N. et al. EPIC-Norfolk: study design and characteristics of the cohort. European Prospective Investigation of Cancer. Br. J. Cancer 80 95–103 (1999).
Narasimhan, V. M. et al. Health and population effects of rare gene knockouts in adult humans with related parents. Science 352, 474–477 (2016).
Bayraktar, O. A. et al. Astrocyte layers in the mammalian cerebral cortex revealed by a single-cell in situ transcriptomic map. Nat. Neurosci. 23, 500–509 (2020).
Bankhead, P. et al. QuPath: open source software for digital pathology image analysis. Sci. Rep. 7, 16878 (2017).
Schmidt, U., Weigert, M., Broaddus, C. & Myers, G. Cell Detection with Star-Convex Polygons in MICCAI 2018265–273 (Springer Nature Switzerland, 2018)
Widmann, J. et al. RNASTAR: an RNA structural alignment repository that provides insight into the evolution of natural and artificial RNAs. RNA 18, 1319–1327 (2012).
Stuart, T. et al. Comprehensive integration of single-cell data. Cell 177, 1888–1902.e21 (2019).
Acknowledgements
MC3R genetic analysis, next-generation sequencing and functional analysis were supported by the UK Medical Research Council (MRC) Metabolic Diseases Unit (MC_UU_00014/1), Wellcome (WT 095515/Z/11/Z) and the National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre. K.R., K.D., D.R., I.C., A.P.C. and G.S.Y. are supported by the MRC Metabolic Disease Unit (MC_UU_00014/1). S.O. is supported by a Wellcome Investigator award (WT 095515/Z/11/Z) and the NIHR Cambridge Biomedical Research Centre. B.Y.H.L. is supported by a Biotechnology and Biological Sciences Research Council (BBSRC) Project Grant (BB/S017593/1). A.W. and S.B. hold PhD studentships supported by Wellcome. J.A.T. is supported by an NIHR Clinical Lectureship (CL-2019-14-504). A.M. holds a PhD studentship supported jointly by the University of Cambridge Experimental Medicine Training Initiative programme in partnership with AstraZeneca (EMI-AZ). G.K.C.D. is supported by the BBSRC Doctoral Training Programme. Next-generation sequencing was performed via Wellcome–MRC IMS Genomics and transcriptomics core facility supported by the MRC (MC_UU_00014/5) and the Wellcome (208363/Z/17/Z) and the Cancer Research UK Cambridge Institute Genomics Core. The histology core is supported by the MRC (MC_UU_00014/5). We thank P. Barker and K. Burling of the Cambridge NIHR Biomedical Research Centre Clinical Biochemistry Assay Laboratory for their assistance with biochemical assays. The EPIC-Norfolk study (https://doi.org/10.22025/2019.10.105.00004) has received funding from the MRC (MR/N003284/1 and MC-UU_12015/1) and Cancer Research UK (C864/A14136). The genetics work in the EPIC-Norfolk study was funded by the MRC (MC_PC_13048). Metabolite measurements in the EPIC-Norfolk study were supported by the MRC Cambridge Initiative in Metabolic Science (MR/L00002/1) and the Innovative Medicines Initiative Joint Undertaking under EMIF grant agreement no. 115372. We are grateful to all of the participants who have been part of the project and to the many members of the study teams at the University of Cambridge who have enabled this research. The Fenland study (https://doi.org/10.22025/2017.10.101.00001) is funded by the MRC (MC_UU_12015/1). We are grateful to all of the volunteers and to the general practitioners and practice staff for assistance with recruitment. We thank the Fenland study investigators, Fenland study co-ordination team and the Epidemiology Field, Data and Laboratory teams. We further acknowledge support for genomics and metabolomics from the MRC (MC_PC_13046). Proteomic measurements were supported and governed by a collaboration agreement between the University of Cambridge and Somalogic. F.R.D., N.J.W., K.K.O., C.L. and J.R.B.P. are funded by the MRC (MC_UU_12015/1, MC_UU_12015/2, MC_UU_00006/1 and MC_UU_00006/2). N.J.W. is an NIHR Senior Investigator. We are grateful for funding to the BIA prediction equations, supported by the NIHR Biomedical Research Centre Cambridge (IS-BRC-1215-20014). The NIHR Cambridge Biomedical Research Centre is a partnership between Cambridge University Hospitals NHS Foundation Trust and the University of Cambridge, funded by the NIHR. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. We thank A. Mesut Erzurumluoglu, L. Wittemans, E. Wheeler, I. Stewart, M. Pietzner, M. Koprulu, E. De Lucia Rolfe, R. Powell and N. Kerrison for providing help with and access to GWAS meta-analysis summary statistics for body composition measures and biomarkers in the UKBB, metabolomics measures in the EPIC-Norfolk study, proteomics measures in the MRC Fenland study, as well as help with genotype quality control in the Fenland study and the UKBB. The MRC, Wellcome (217065/Z/19/Z) and the University of Bristol provide core support for ALSPAC. Genome-wide association data were generated by sample logistics and genotyping facilities at Wellcome Sanger Institute and LabCorp (Laboratory Corporation of America) using support from 23andMe. A.G.S. was supported by the study of ‘Dynamic longitudinal exposome trajectories in cardiovascular and metabolic non-communicable diseases’ (H2020-SC1-2019-Single-Stage-RTD, project ID 874739). K.W. was supported by the Elizabeth Blackwell Institute for Health Research, University of Bristol and the Wellcome Institutional Strategic Support Fund (204813/Z/16/Z). N.T. is a Wellcome Trust Investigator (202802/Z/16/Z), is the principal investigator of the ALSPAC (MRC & WT 217065/Z/19/Z), is supported by the University of Bristol NIHR Biomedical Research Centre (BRC-1215-2001), the MRC Integrative Epidemiology Unit (MC_UU_00011) and works within the Cancer Research UK Integrative Cancer Epidemiology Programme (C18281/A19169). We are extremely grateful to all of the families who took part in the ALSPAC study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. The Rowitch laboratory receives funding from Wellcome and the ERC Advanced Grant (REP-789054-1). Genes & Health is/has recently been core funded by Wellcome (WT102627 and WT210561), the MRC (M009017), Higher Education Funding Council for England Catalyst, Barts Charity (845/1796), Health Data Research UK (for London substantive site), and research delivery support from the NHS NIHR Clinical Research Network (North Thames). Additional funding for recall was provided by a pump priming award to S.F. (SCA/PP/12/19) from the Diabetes Research and Wellness Foundation. E.G.B. and X.D. are supported by the Wellcome (208987/Z/17/Z) and Barts Charity (project grant to E.G.B.). We thank Social Action for Health, Centre of The Cell, members of our Community Advisory Group, and staff who have recruited and collected data from volunteers; the NIHR National Biosample Centre (UK Biocentre), the Social Genetic and Developmental Psychiatry Centre (King’s College London), Wellcome Sanger Institute, and Broad Institute for sample processing, genotyping, sequencing and variant annotation; Barts Health NHS Trust, NHS Clinical Commissioning Groups (Hackney, Waltham Forest, Tower Hamlets and Newham), East London NHS Foundation Trust, Bradford Teaching Hospitals NHS Foundation Trust, and Public Health England (especially D. Wyllie) for GDPR-compliant data sharing; and most of all, we thank all of the volunteers participating in Genes & Health. R.D.C. receives funding from US National Institutes of Health (NIH) grants DK070332 and DK126715. P.S. is funded by NIH F32HD095620 and K99DK127065. R.B.S. receives funding from the NIH (DK106476). M.N.B. is funded by the NIH (F32DK123879). This research has been conducted using data from UK Biobank, a major biomedical database (https://www.ukbiobank.ac.uk), application numbers 32974 and 44448.
Author information
Authors and Affiliations
Consortia
Contributions
B.Y.H.L., A.W., S.F., A.M., K.W., N.T., K.K.O., C.L., J.R.B.P., G.S.Y. and S.O. designed the study. B.Y.H.L., A.W., K.D., A.M., S.B. and J.R.-S. planned and performed the in vitro experiments. B.Y.H.L. and A.W. conducted the bioinformatic and genetic analyses on the UKBB and Genes & Health data. A.W., F.R.D., N.J.W., K.K.O., J.R.B.P. and C.L. conducted the genotype–phenotype association on the UKBB, Fenland and EPIC data. K.R. and K.D. conducted the next-generation sequencing for ALSPAC and Sanger sequencing for ALSPAC and Genes & Health. B.Y.H.L. and A.M. conducted genetics and bioinformatic analyses of ALSPAC. A.G.S., K.W. and N.T. lead the analysis of phenotypic association in ALSPAC. P.S., D.T.P., K.L.J.E., R.N.L. and R.D.C. performed the study on Mc3r-null mice. B.Y.H.L. performed the single-cell data analysis. I.C., D.R. and A.P.C. lead the mouse studies in Cambridge. J.A.T., G.K.C.D., K.E.R., S.H., Z.X., D.H.R., M.N.B. and R.B.S. conducted the histology, single-molecule fluorescent in situ hybridization and imaging analyses. S.F., A.K., R.C.T., H.C.M., D.A.v.H. and the Genes & Health team managed the cohort. D.A.v.H., H.C.M., E.G.B. and X.D. led the genetic analysis. S.F. coordinated and conducted the clinical recall. B.Y.H.L., A.W., S.F., F.R.D., A.G.S., K.W., N.T., K.K.O., C.L., J.R.B.P., G.S.Y. and S.O. wrote the manuscript and it was reviewed by all authors. This publication is the work of the authors, and C.L., J.R.B.P., G.S.Y. and S.O. will serve as guarantors for the contents of this paper.
Corresponding author
Ethics declarations
Competing interests
S.O. has undertaken remunerated consultancy work for Pfizer, AstraZeneca, GSK and ERX Pharmaceuticals. D.A.v.H. has an unrestricted research grant from Alnylam Pharmaceuticals. P.S. and R.D.C. hold equity in Courage Therapeutics Inc. and are inventors of intellectual property optioned to Courage Therapeutics Inc. R.D.C. chairs the Scientific Advisory Board at Courage Therapeutics Inc. All remaining authors declare no competing interests.
Additional information
Peer review information Nature thanks the anonymous reviewers for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Functionally characterised MC3R mutations.
Complete, partial loss-of-function (LoF) and wild-type like mutations are marked in purple, dark yellow and green respectively. Coloured rectangles indicate cohort(s) in which mutations were identified: Red = UK Biobank (UKBB); Blue = Avon Longitudinal Study of Parents & Children (ALSPAC); Light Brown = Genes & Health (G&H).
Extended Data Fig. 2 PheWAS analysis of MC3R genetic risk score.
A CADD-weighted MC3R genetic risk score was constructed (see Methods) and used to conduct a phenome-wide analysis (pheWAS) with publicly available summary statistics. Solid black line indicates Bonferroni multiple-testing threshold of p < 1.046e-4, dashed line indicates nominal significance threshold p < 0.05.
Extended Data Fig. 3 Effect of MC3R Loss-of-Function mutations on height (cm) across time.
Carriers of MC3R LoF mutations (dark blue) had lower height throughout early life course compared to the reference group (light blue) after adjusting for sex and age. Figures only show results where the mutation group was represented by at least one individual at all time points between birth and 24 years. Mean ± 95% CI shown, N and p-values are listed in Supplementary Table 4.
Extended Data Fig. 4 MC3R is essential for normal cycle length and for fasting-induced suppression of the reproductive axis.
a, b, Representative traces of progression through the oestrous cycle in WT (a) and Mc3r−/− (b) mice following an overnight fast. D = Dioestrous; M = Metoestrous; E = Oestrous.
Extended Data Fig. 5 Mc3r is expressed in several cell populations in the mouse hypothalamus.
a, T-SNE plot showing 28 neuronal clusters (0–27) of the mouse hypothalamus from a combined dataset consisting of 18,427 neurons from 4 published studies. b, Mc3r is expressed in several neuronal populations (log2 normalised expression in dark red). c, Multiplexed smFISH showing the co-expression of Mc3r (white) Kiss1 (red) and Tac2 (green) in the arcuate nucleus. (Representative example shown, n = 3 mice, scale bar = 20μm). d, Venn diagram showing the number of cells expressing Kiss1 (left, red), Tac2 (right, green), or both (KNDy, centre). e, Violin plots showing the number of Mc3r mRNA punta in Kiss1 only, KNDy, and Tac2 only cells. Mean percentages of cells ± SEM with detected Mc3r are shown, data collected from 3 mice.
Extended Data Fig. 6 Expression of Mc3r and Lepr in KNDy and GHRH neurons.
a, b, Mc3r expression is more prominent compared to Mc4r and Lepr in Tac2 (KNDy) (cluster 7, blue) (a) and GHRH neurons (cluster 15, green) (b). c, Violin plots showing expression of Kiss1, Tac2, Ghrh, Mc3r and Lepr in KNDy and Ghrh neurons in the Campbell38 and the Chen42 dataset separately. The Lam40 and Romanov41 datasets are not shown due to low cell count (<10).
Extended Data Fig. 7 Human smFISH showing the co-expression of MC3R, KISS1, and GHRH in the human hypothalamic arcuate nucleus.
a, Annotated overview MC3R and KISS1 co-expression: MC3R = grey, KISS = magenta and MC3R+KISS1 = white (scale bar = 200μm). High-powered micrograph (squared area) below shows the staining of MC3R (white) and Kiss1 (magenta) mRNA punta in 2 representative cells (teal = DAPI, scale bar = 10μm). N = 2 slides. b, Annotated overview of MC3R and GHRH co-expression: MC3R = grey, GHRH = green and MC3R+KISS1 = white (scale bar = 200μm). High-powered micrograph (squared area) below shows the staining of MC3R and GHRH mRNA punta in a representative cell (teal = DAPI, scale bar = 4μm). N = 2 slides.
Extended Data Fig. 8 Mc3r expression in kisspeptin neurons in the mouse hypothalamus at P16, P28 and P48.
a–c, Representative smFISH showing the co-expression of Mc3r and Kiss1 in the anteroventral periventricular nucleus (AVPV) at P16 (a); P28 (b) and P48 (c) (N = 3 mice for all age groups): Mc3r = green, Kiss1 = red (scale bar = 20μm).
Supplementary information
Supplementary Information
This file contains a note of the effect of MC3R complete loss-of-function (cLoF) mutations on trajectories of BMI and height in the Avon Longitudinal Study of Parents and Children (ALSPAC), and members of the Genes & Health Research Team.
Supplementary Tables
This file contains Supplementary Tables 1–15.
Rights and permissions
About this article
Cite this article
Lam, B.Y.H., Williamson, A., Finer, S. et al. MC3R links nutritional state to childhood growth and the timing of puberty. Nature 599, 436–441 (2021). https://doi.org/10.1038/s41586-021-04088-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-021-04088-9
This article is cited by
-
Metabolic control of puberty: 60 years in the footsteps of Kennedy and Mitra’s seminal work
Nature Reviews Endocrinology (2024)
-
Protection against overfeeding-induced weight gain is preserved in obesity but does not require FGF21 or MC4R
Nature Communications (2024)
-
Targeting the central melanocortin system for the treatment of metabolic disorders
Nature Reviews Endocrinology (2023)
-
Evaluation of the MC3R gene pertaining to body weight and height regulation and puberty development
Scientific Reports (2023)
-
Genetische und epigenetische Einflüsse auf den Pubertätsverlauf in Bezug auf Pubertas praecox vera und Pubertas tarda
Gynäkologische Endokrinologie (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.