Abstract
The melanocortin system plays a critical role in the central regulation of food intake and energy balance. This system consists of neurons producing pro-opiomelanocortin (POMC), melanocortin receptors (MC4Rs), and the endogenous antagonist agouti-related peptide (AgRP). Pomc and Mc4r deficiency in rodents and humans causes early onset of obesity, whereas a loss of Agrp function is associated with leanness. Accumulating evidence shows that many chronic diseases, including obesity, might originate during early life. The melanocortin system develops during a relatively long period beginning during embryonic life with the birth of POMC and AgRP neurons and continuing postnatally with the assembly of their neuronal circuitry. The development of the melanocortin system requires the tight temporal regulation of molecular factors, such as transcription factors and axon guidance molecules, and cellular mechanisms, such as autophagy. It also involves a complex interplay of endocrine and nutritional factors. The disruption of one or more of these developmental factors can lead to abnormal maturation and function of the melanocortin system and has profound metabolic consequences later in life.
Similar content being viewed by others
Introduction
The melanocortin system is a critical component of brain pathways that regulate feeding behavior and energy homeostasis. The brain’s melanocortin system consists of pro-opiomelanocortin (POMC) neurons and neurons that produce agouti-related peptide (AgRP), an endogenous inverse agonist of melanocortins. There are two anatomically distinct POMC neuronal populations in the brain. The largest population of POMC neurons resides in the arcuate nucleus of the hypothalamus (ARH). A discrete population of POMC neurons is also found in the nucleus of the solitary tract (NTS) in the brainstem. In contrast, AgRP neurons are exclusively located in the ARH and coexpress neuropeptide Y (NPY). Pharmacological approaches revealed more than three decades ago that melanocortins have a potent and long-lasting inhibitory effect on feeding1. More recently, neuron- and gene-specific genetic studies have shown the importance of POMC neurons in mediating the physiological actions of metabolic hormones, such as leptin and insulin2,3. Opto- and chemogenetic experiments further indicated that although arcuate POMC neurons appear to be more involved in integrating long-term adiposity signals, the contribution of hindbrain POMC neurons seems to be more specific to the integration of short-term satiety signals4,5. In contrast, optogenetic stimulation of AgRP neurons rapidly evokes feeding4, whereas genetic ablation of AgRP neurons in adult animals causes starvation6,7.
The POMC-derived peptide alpha-melanocyte-stimulating hormone (αMSH) and AgRP modulate the activity of the melanocortin 4 receptor (MC4R). αMSH activates MC4R, while AgRP acts as an endogenous inverse agonist of MC4R, meaning that it suppresses constitutive MC4R activity and simultaneously antagonizes the effects of αMSH. The highest expression of MC4Rs is found in the hypothalamus and the brainstem8,9,10. Target neurons expressing MC4Rs include neurons producing oxytocin, thyrotropin-releasing hormone, and corticotrophin-releasing hormone in the paraventricular nucleus of the hypothalamus (PVH)10,11. The melanocortin system is universal and common to all mammals, including humans, nonhuman primates, and rodents, and mutations in the MC4R gene are the most common monogenic disorders that cause obesity in humans12.
In this review, we will first describe the major steps of melanocortin system development. We will also discuss the hormonal, molecular, cellular, and nutritional factors influencing the development of POMC and AgRP neurons.
Ontogenesis of the hypothalamic melanocortin system
POMC and AgRP neurons are derived from precursor cells found in the proliferative zone located in the inner and lower portions of the third ventricle, also known as the neuroepithelium of the third ventricle13 (Fig. 1). The most comprehensive animal models used to study the development of the melanocortin system are rodent models (mainly mice and rats), and a limited number of studies have also examined the development of this neuronal system in humans and nonhuman primates. Birth dating approaches using the thymidine analog bromodeoxyuridine 5-bromo-2′-deoxyuridine (BrdU) indicated that the majority of POMC and AgRP/NPY neurons in the mouse ARH are born primarily on embryonic day (E)11–E1214,15 (Fig. 1). However, some POMC neurons, which are located more laterally in the ARH, are generated as late as E13. Gene expression studies showed that neurons in the presumptive ARH begin to express Pomc mRNA on E10–E12, whereas Npy mRNA expression is not observed until E14 (ref. 15). These observations are consistent with the early determination of Pomc cell fate. Intriguingly, genetic cell lineage tracing studies revealed that approximately half of the Pomc-expressing precursors acquire a non-POMC fate in adult mice, and nearly one-quarter of the mature NPY neurons in the ARH share a common progenitor with POMC cells15. These data show the unique property of Pomc-expressing progenitors with respect to giving rise to antagonistic neuronal populations. Differentiated neurons then send out axonal processes to other target nuclei to convey neuronal information and control behavior. The majority of arcuate POMC and AgRP neurons have relatively short axons and connect primarily to neurons within the hypothalamus16. Axonal projections from the arcuate nucleus develop postnatally and provide inputs to the PVH between postnatal day (P) 8 and P10 in mice16 (Fig. 1). Using immunohistochemical techniques, Grove et al.17 confirmed that projections immunopositive for AgRP are immature at birth and develop mainly during the second week of postnatal life in rats. The same temporal pattern was observed for the development of POMC projections in mice18.
The development of a functional hypothalamus occurs in two major phases: the determination of cell numbers, which includes neurogenesis, neuronal migration, and cell fate, and the formation of functional circuits, which includes axon growth and the formation of functional synapses. In rodents, neurogenesis, neuronal migration, and cell fate occur during mid-to-late gestation, while axon growth and synapse formation occur primarily postnatally.
Mc4r mRNA is first expressed at E12 in the proliferative zone surrounding the lower portion of the third ventricle (also known as the neuroepithelium), and its expression peaks at E16 (ref. 19). These findings are particularly interesting because, as described above, it is known that neurons that compose various hypothalamic nuclei in adults are primarily derived from precursors that originate from this proliferative zone, raising the possibility that MC4R could be involved in hypothalamic neurogenesis. However, further studies are needed to determine the developmental stage during which MC4R becomes functional. Nevertheless, the observation that peripheral injection of the melanocortin agonist melanotan II (MTII) reduces milk intake and body weight as early as during the first 2 weeks of postnatal life suggests that MC4R receptors are present and functional in the hypothalamus at least soon after birth20. Consistent with this idea, in situ hybridization analysis showed that Mc4r mRNA is abundant in the hypothalamus, especially in the PVH at P10. Peripheral injection of MTII induces strong induction of cFos immunoreactivity (a marker of neuronal activation) in the PVH at P5–P15, further supporting the functionality of MC4R in the PVH during early postnatal life20. Moreover, Melnick et al.21 showed an age-dependent increase in the electrophysiological response of specific sets of PVH neurons to melanocortins, with a maximal response observed at P28–P35, suggesting that synapses between POMC and AgRP axons and PVH MC4R+ target neurons continue to build until puberty (Fig. 1).
Consideration of species differences in melanocortin circuit development
The marked differences in the normal ontogeny of hypothalamic development between rodents and human and nonhuman primates warrant attention. First, the regional development of the rodent hypothalamus proceeds on a timeline of days in rodents versus weeks to months in human and nonhuman primates. Second, although rodents exhibit considerable postnatal hypothalamic development, human and nonhuman primates undergo considerably more prenatal maturation of hypothalamic circuits. For example, although the hypothalamus is not mature until after weaning in rodents, hypothalamic neurogenesis and axon growth occur primarily during intrauterine life in nonhuman primates, including humans. Hypothalamic development has been studied in detail by Grove and collaborators in Japanese macaques. They reported that Pomc and Npy mRNA-containing neurons are found in the ARH of nonhuman primates at gestational day (G) 100. Although only a few AgRP/NPY fibers and no POMC fibers were detected in the PVH at this age, the density of AgRP/NPY fibers innervating the PVH markedly increased at G130 and G170, and POMC fibers were found in the PVH at G17022. In human fetuses, NPY-immunoreactive fibers are detected in the ARH and the PVH as early as 21 weeks of gestation23.
Hormonal factors that influence melanocortin neuron development
Leptin
The discovery of leptin led to a paradigm shift in understanding how food intake and body weight can be powerfully and dynamically regulated by hormonal signals24,25,26. In 1994, Friedman et al.24 used positional cloning and found that the ob gene encodes the hormone leptin, which is secreted by adipose tissue in proportion to its mass. Subsequently, other groups reported that leptin administration reduces body weight and food intake in leptin-deficient mice and humans27,28,29. A few years later, Ahima and colleagues reported that circulating leptin levels exhibit a distinct surge between P8 and P12 in mice30, yet exogenous leptin does modulate food intake, growth, or energy expenditure at this developmental stage31,32,33,34. Instead of acutely regulating food intake and body weight, neonatal leptin appears to be an important neurodevelopmental factor that influences the wiring of hypothalamic circuits (Fig. 2). The labeling of ARH axons combined with immunohistochemical analyses showed that POMC and AgRP neuronal projections are disrupted in leptin-deficient (ob/ob) mice35. The site of action for the developmental effects of leptin includes at least a direct action on ARH neurons because leptin induces neurite extension from isolated organotypic explants of the ARH ex vivo35. Remarkably, leptin appears to exert its developmental action on POMC neural projections during a discrete developmental critical period: exogenous leptin treatment up to P28 rescues AgRP projections in ob/ob mice35,36. In contrast, leptin treatment of ob/ob mice after P28 is relatively ineffective because it did not increase the density of either POMC or AgRP fibers in the PVH to levels that are characteristic of wild-type mice35,36. Together, these observations suggest the existence of a critical period for the neurotrophic effect of leptin on POMC and AgRP circuits that closes around puberty. More in-depth studies have examined leptin receptor signaling pathways that mediate the axonotrophic effect of leptin. The leptin receptor exists in several alternatively spliced isoforms, of which only the long form (LepRb) associates with Janus kinase 2 to mediate intracellular signaling. LepRb initiates multiple intracellular signal transduction pathways upon leptin binding that result in the activation of STAT family transcription factors, extracellular signal-regulated kinases (ERKs), and phosphoinositol-3 kinase/Akt. Developing POMC and AgRP neurons express LepRb37, and leptin administration in mouse neonates results in the activation of major LepRb signaling pathways, including STAT3, ERK, and Akt37,38. The disruption of POMC and AgRP axonal projections is observed in mice or rats that lack functional LepRb signaling (db/db mice and fa/fa rats, respectively)38,39. Moreover, a lack of functional LepRb→STAT3 signaling in vivo (s/s mice) or in vitro results in a reduced density of POMC fibers without altering the development of AgRP projections, showing the importance of this signaling pathway, specifically, in the development of POMC neural projections38. However, not all LepRb signaling pathways play a role in the formation of ARH projections. For example, mice that lack LepRb→ERK signaling (l/l mice) display densities of POMC and AgRP axons in the PVH that are comparable to those of wild-type mice38.
Ghrelin and growth hormone
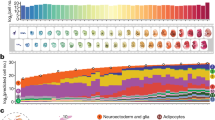
Ghrelin is a 28 amino acid hormone peptide that is mainly produced by the stomach and is an endogenous ligand for the growth hormone secretagogue receptor (GHSR). It is one of the most potent orexigenic signals that exerts its action on food intake by stimulating AgRP/NPY neurons, which in turn inhibit POMC neurons40,41. Although the marked orexigenic effect of ghrelin is not yet present before weaning in mice or rats42,43, ghrelin in early postnatal life does have a lasting developmental effect on the hypothalamic circuits involved in energy homeostasis43 (Fig. 2). Mice injected with an anti-ghrelin compound during neonatal life display increased densities of POMC- and AgRP-containing axons innervating the PVH. These structural alterations are accompanied by long-term metabolic defects, including elevated body weight, increased adiposity, and hyperglycemia43. However, if adult mice are treated with the anti-ghrelin compound, it does not alter POMC and AgRP circuits43. These findings suggest that, similar to leptin, the developmental action of ghrelin on arcuate projections is restricted to a critical neonatal window. The site of action for the developmental effects of ghrelin likely includes direct action on arcuate neurons because direct exposure of isolated ARH explants to ghrelin inhibits axonal outgrowth43. Ghrelin also interacts with LepRb→STAT3 signaling to block the neurotrophic effect of leptin43.
Ghrelin is a potent stimulator of growth hormone secretion44. Based on the documented finding that ghrelin influences hypothalamic development and can interact with leptin receptor signaling43, it is not surprising that the deletion of the growth hormone receptor in Leprb-expressing cells also alters the development of POMC and AgRP neuronal circuits45. In addition, selective loss of the growth hormone receptor in AgRP neurons affects AgRP axonal projections without affecting POMC circuits45, demonstrating a cell-autonomous effect of growth hormone on AgRP neuronal development.
GLP1
The incretin hormone glucagon-like peptide 1 (GLP1) is secreted postprandially by intestinal enteroendocrine cells to promote satiety and glucose-induced insulin release46. The administration of the GLP1-R agonist exendin-4 during the first week of postnatal life decreases the density of NPY fibers innervating the PVH and has a protective effect against both age-related and diet-induced obesity47. Moreover, genetic deletion of Glp1r in Sim1 neurons of the PVH reduces AgRP/NPY projections, while it increases POMC projections to the PVH47.
Amylin
Amylin is a hormone produced by pancreatic β-cells and is coreleased with insulin in response to caloric intake. The amylin receptor comprises the core calcitonin receptor (CTR), which heterodimerizes with one or several receptor activity-modifying proteins (RAMP-1, -2, and -3). The primary role of amylin in adults is to reduce food intake by promoting meal-ending satiation and maintaining glucose homeostasis. During development, amylin is detected in the blood circulation of embryos, where it appears to act through RMAP1-3 to influence the neurogenesis of POMC neurons48 (Fig. 2). During postnatal life, amylin continues to be secreted in the blood circulation49, and a loss of amylin or Ramp1/3 disrupts the development of POMC and AgRP projections to the PVH50.
Molecular programs of melanocortin neuron development
Transcription factors
Homeobox genes belong to a class of transcription factors that play important roles in regionalization, patterning, and cell differentiation during embryogenesis and organ development. The homeobox genes orthopedia (Otp), Nkx2.1, and Bsx are highly expressed in the ventral hypothalamus during embryonic development. Loss-of-function studies indicated that while Nkx2.1 and Otp are essential for the normal morphological development of the hypothalamus, including the ARH, Bsx is not required51,52,53 (Fig. 2). The homeobox gene Nkx2.1, also known as thyroid transcription factor 1 (Ttf-1), plays a particularly important role in ARH specification. The ablation of Nkx2.1 impairs the formation of the ventral hypothalamic primordium, resulting in the absence of ARH formation51,54. However, the ventromedial nucleus (VMH), dorsomedial nucleus (DMH), and lateral hypothalamic area (LHA) are present. The expression of Nkx2.1 in postmitotic cells suggests that it further plays a role in the differentiation and maintenance of ARH neurons in the ventral portion of the hypothalamus55,56. Deficiency in Nkx2.1 prior to the onset of Pomc expression markedly reduces Pomc cell numbers57. However, the number of NPY neurons was not affected in Nkx2.1 knockout mice, and the POMC neuronal cell number was not affected if Nkx2.1 deletion occurred in postmitotic Pomc neurons57. The LIM-homeodomain transcription factor Islet 1 (Isl1) is upregulated in hypothalamic Nkx2.1 progenitor cells at E10, i.e., just before the onset of neuropeptide expression58,59. Consistent with the role of Isl1 in the phenotypic determination of ARH neurons, loss-of-function studies revealed that Isl1 promotes the terminal differentiation of Pomc, Agrp, and Npy expression58,59. In contrast, the deletion of the transcription factor Dlx1/2 in Nkx2.1-expressing progenitors increases Agrp expression without affecting Pomc expression60. More in-depth molecular studies revealed that Dlx1/2 controls Agrp expression by binding to and repressing the expression of the homeodomain transcription factor Otp, which is also known to influence ARH morphogenesis52,53,60. Thus, the loss of Otp in Agrp neurons results in a dramatic reduction in the number of Agrp mRNA-expressing cells61. Notably, Otp expression is absent in the hypothalamus of Isl1 knockout embryos58, suggesting that, in addition to Dlx1/2, Isl1 is also required for the expression of Otp in the future ARH. Sonic hedgehog (Shh), SIX homeobox 3 (Six3), and retinal anterior neural fold homeobox (Rax) were also identified as critical regulators of ventral hypothalamus development and POMC development. Shh signaling increases Nkx2.1 expression62, and the deletion of Shh in Nkx2.1 progenitors affects the development of POMC neurons63. Six3 is a regulator of forebrain development, including the hypothalamus64, and is required for Shh expression65. Finally, Rax is also important for the formation of the ventral neural tube. Mice lacking Rax in Six3-expressing cells do not show ventral hypothalamic Nkx2.1 expression and never express POMC66.
The oligodendrocyte transcription factor family (Olig1 and Olig2) are basic helix–loop–helix (bHLH) transcription factors highly expressed in the periventricular regions of the brain, such as the hypothalamus67,68. Lineage tracing experiments indicate that a number of POMC and NPY cells are derived from Olig1 progenitors69. The majority of Olig1 progenitors also express bone morphogenetic protein receptor 1A (Bmpr1A)69, and when Bmpr1A is deleted in Olig1-expressing cells, it decreases and increases the number of POMC and AgRP neurons, respectively69. Neurogenin 3 (Ngn3) is another bHLH transcription factor expressed in hypothalamic progenitors, and it plays an opposite role in the specification of Pomc and Npy neurons: while neurogenin 3 promotes the embryonic development of Pomc neurons, it inhibits Npy neuronal development70,71. However, not all POMC neurons are derived from Ngn3 progenitors. Using a mouse model of Mash1 deficiency, McNay et al.72 further reported that this bHLH transcription factor has a pro-neural function and acts upstream of Ngn3 to regulate neurogenesis in the ventral hypothalamus. A loss of Mash1 results in the disappearance of Ngn3 expression in ARH progenitors and is associated with a dramatic reduction in the number of POMC and NPY neurons72. The Notch signaling pathway also appears to mediate its developmental effects on POMC and NPY neuronal development through Mash1. Mice lacking Notch signaling in Nkx2.1-expressing cells display an increased number of POMC and NPY neurons associated with an induction in Mash1 expression72,73. In addition, mice with a constitutively active Notch1 intracellular domain show a complete loss of POMC and NPY neurons73, mirroring the effects of Mash1-deficient mice72.
As described above, Pomc-expressing progenitors in the ARH have the unique ability to differentiate into functional mature NPY neurons15. Recent data from our laboratory investigated the molecular mechanisms involved in this developmental switch and identified miR-103/107 as candidates involved in Pomc progenitor differentiation (Fig. 2). A loss of the microRNA (miRNA)-processing enzyme Dicer increases the proportion of Pomc progenitors acquiring an NPY phenotype74. Moreover, the silencing of miR-103/107 specifically decreases the number of Pomc-expressing cells and increases the proportion of Pomc progenitors differentiating into NPY neurons74. Postnatal maintenance of Pomc and Npy peptidergic identity also depends on the expression of the transcription factor T-box 3 (Tbx3)75. Because the majority of miRNAs exert their effects on gene expression by targeting transcription factors, it would be interesting to study whether there is a link between miRNAs and Tbx3 and Pomc/Npy gene expression.
Axon guidance molecules
Axons grow by sending out a highly plastic and sensitive structure called a “growth cone,” which travels toward the target with the elongating neurite trailing behind. As described above, metabolic hormones, including leptin, are critical factors influencing initial POMC and AgRP/NPY axon outgrowth. Growing POMC axons must then choose a path to follow and decide the direction to go on this path to innervate the proper nucleus (e.g., the PVH). The pathways are defined by cell–cell interactions and diffusible chemorepulsive and chemoattractive cues76. The diffusible axon guidance cues semaphorins are highly expressed in the PVH during development, and POMC neurons express the semaphorin receptors neuropilin 1 and 2 (ref. 77). Supporting a role for neuropilins/semaphorins in POMC axon guidance, a loss of neuropilin 2 receptors in POMC neurons specifically disrupts the development of POMC axonal projections to the PVH77. These structural alterations are accompanied by metabolic dysregulation, including increased body weight and glucose intolerance77. Notably, exome sequencing experiments identified variants in the semaphorin and neuropilin families associated with severe obesity in humans77, demonstrating the translational importance of these findings. The formation of POMC neural neuronal connectivity also involves cell–cell adhesion proteins. Supporting this idea, POMC neurons are enriched in the cell-to-cell contact molecules Efnb1 (EphrinB1) and Efnb2 (EphrinB2) during postnatal development, and a loss of Efnb1 or Efnb2 in Pomc-expressing progenitors decreases the amount of excitatory glutamatergic inputs78. In addition, mice that are deficient in contactin, a cell adhesion molecule involved in the formation of axonal projections, have a reduced density of POMC fibers in the PVH during postnatal development79.
Cellular factors underlying melanocortin neuron development
Autophagy
Axonal growth involves dynamic remodeling of cytosolic structures and requires protein degradation and turnover to replace damaged organelles and proteins. The maintenance of cell function and growth is achieved with autophagy, which is an important cellular degradation system that engulfs parts of the cytoplasm and organelles within double-membrane vesicles, known as autophagosomes, to turn over and recycle these cellular constituents80. This cellular process is also critical in the supply of nutrients for survival during starvation81. Constitutive autophagy is detected in the hypothalamus, including in arcuate POMC neurons, during critical periods of axon growth and development82. A loss of the autophagy-related protein (Atg) gene Atg7 disrupts the maturation of POMC axonal projections and causes lifelong metabolic perturbations82 (Fig. 2). As described above, leptin is a critical neurotrophic factor for POMC circuits, and direct crosstalk has been described between leptin and hypothalamic autophagy during perinatal life83. Supporting a role for autophagy in mediating the trophic effects of leptin, a loss of autophagy in POMC neurons exacerbates the metabolic and neurodevelopmental deficits observed in leptin-deficient ob/ob mice83.
Primary cilia
Another cellular signaling system that plays an important role in brain development and function is the primary cilium, which is a microscopic sensory antennae that cells in many vertebrate tissues use to gather information about their environment. It is an organelle found on the cell surface of most mammalian cells, including hypothalamic neurons84. For example, during embryonic development, primary cilia are important mediators of Shh, which is a critical regulator of the ventral patterning of the hypothalamus85. Moreover, a strong interaction between primary cilia and autophagy has been reported, including in the developing hypothalamus86. Cilia begin to be observed in hypothalamic neurons on E12, and the number and length of primary cilia gradually increase thereafter to reach an adult-like pattern at P14 (ref. 86). A disruption of cilia formation in developing POMC neurons, but not in adult POMC neurons, increases body weight, fat mass, and food intake; reduces energy expenditure; and alters glucose homeostasis during adult life86. Neuroanatomically, a reduction in the number of POMC neurons was observed in juvenile mice lacking primary cilia on POMC neurons, but POMC cell numbers were normal in adult mutant mice. This reduction in POMC cell numbers during the preweaning period is attributed to a decrease in neurogenesis during embryonic development (in opposition to an effect on apoptosis), and the adult normalization in POMC cell number is attributed to a compensatory increase in neurogenesis after weaning86. A loss of primary cilia also alters axonal and dendritic growth, resulting in a reduced density of POMC fibers innervating the PVH, DMH, and LHA86 (Fig. 2). It also blocks the ability of leptin to promote the development of POMC projections in ob/ob mice86. Because a subpopulation of Pomc progenitor cells also give birth to NPY neurons (see above and ref. 15), it is not surprising that mice lacking primary cilia from embryonic POMC neurons also display a reduction in NPY cell numbers and NPY fibers innervating the PVH86. The interaction between primary cilia and the melanocortin system appears bidirectional. Consistent with this idea, Siljee et al.87 reported that MC4-R colocalizes with adenylate cyclase 3 in the primary cilia of a subset of PVH neurons and that the inhibition of primary cilia adenylyl cyclase signaling increases body weight.
Effect of perinatal nutrition on the development of the melanocortin system
Obesity has reached alarming rates worldwide and is associated with several life-threatening conditions, such as hypertension and type-2 diabetes. The prevalence of obesity among pregnant women is also at an all-time high, and it represents a significant risk factor for the development of metabolic diseases in offspring. Obesity is determined by genetics and obesogenic environments, such as diets rich in fat and/or sugar. Maternal high-fat diet (HFD) feeding during pregnancy and/or lactation in rodents is a useful experimental approach for studying the consequences of maternal obesity on the development of offspring’s future health outcomes. Similar to what is observed in humans, offspring born to obese females fed an HFD (45–60% of calories from fat) during gestation and/or lactation become progressively overweight, hyperphagic, and glucose intolerant, and they display an increase in adiposity88,89. These metabolic alterations are associated with a disrupted development of POMC and AgRP/NPY projections to the PVH in both mice and rats89,90,91,92,93 (Fig. 2). Notably, maternal consumption of an HFD during lactation alone (but not during pregnancy alone) appears sufficient to cause obesity and diabetes and alter the development of POMC and AgRP projections90, showing the importance of postnatal nutrition, specifically, in hypothalamic programming. A similar reduction in AgRP axonal projections has been reported in nonhuman primates following maternal HFD exposure91. The rat model of diet-induced obesity (DIO) developed by Levin et al.94 also provides a valuable tool for studying obesity, in part because Levin’s DIO rats share several features with humans with obesity, including polygenic inheritance. Therefore, this animal model is particularly well suited for studying the relative contribution of genetic versus environmental factors in metabolic programming. Animals born to genetically obese-prone DIO dams display a reduction in the number of POMC and AgRP axons innervating the PVH95. In addition, significant remodeling of synapses onto POMC neurons has been observed in DIO rats, particularly in response to nutritional challenges96. DIO rats fed a chow diet display increased inhibitory inputs to POMC neurons compared to obesity-resistant rats. In addition, DIO rats fed an HFD display a loss of synapses onto POMC neurons, whereas high-fat feeding in control obesity-resistant rats causes an increase in POMC synaptic coverage96.
The precise mechanisms that underlie the maternal obesity-induced alterations in melanocortin system development have only begun to be elucidated. Several studies have indicated that abnormal leptin and insulin signaling during postnatal development may represent a likely cause of HFD- and DIO-induced alterations in hypothalamic development. For example, DIO rats and animals born to obese dams display an abnormal organization of projection pathways derived from the ARH that appear to be the result of the diminished responsiveness of ARH neurons to the trophic actions of leptin during critical periods of postnatal development95. Moreover, animals born to obese dams are hyperleptinemic, which is associated with hypothalamic leptin resistance, and improving leptin sensitivity with the endoplasmic reticulum stress-relieving drug tauroursodeoxycholic acid normalizes metabolic and neurodevelopmental deficits in these animals91. At the cellular level, a reduction in cilia length and frequency has been reported in the ARH of pups born to obese dams, suggesting that the alteration of this cellular system is critical for hypothalamic development and that leptin signaling could contribute to obesity-induced perturbations of hypothalamic development86. Changes in insulin signaling could also mediate the neurodevelopmental effects of maternal obesity. Mothers fed an HFD and their offspring are hyperinsulinemic, and deleting the insulin receptor in POMC neurons prevents the diet-induced disruption of POMC projections90. More recently, Dearden et al.97 reported that the offspring of obese dams display a reduction in POMC cell numbers that likely results from a diminished neurogenic action of insulin during embryonic development. Similarly, amylin, which is coreleased with insulin by pancreatic β-cells, appears to be involved in the nutritional programming of melanocortin circuits. The offspring of obese dams are hyperamylinemic from embryonic age throughout adulthood. Amylin fails to activate hypothalamic amylin receptor signaling if animals are born to obese mothers, which is associated with an inability of amylin to promote POMC neurogenesis48. Similarly, knocking down CTR in the ventromedial part of the hypothalamus of obesity-resistant rats (a region that encompasses the ARH + VMH) alters the development of POMC circuits98. In contrast, neonatal amylin treatment in DIO rats enhances STAT3 signaling in the ARH, accompanied by a restoration of AgRP and POMC fibers98.
In part because of the importance of postnatal brain development in rodents, including that of POMC and AgRP neurons, animal models of postnatal metabolic programming have also been extensively studied. The reduction in litter size in rodents has proven to be a very useful model to manipulate the postnatal diet specifically. This model was first characterized by the pioneering works of Kennedy99, Widdowson and McCance100, who reported more than 60 years ago that pups raised in small litters (SL) display an almost fourfold difference in preweaning growth compared to pups raised in large litters. This weight difference persisted throughout life and even increased as the rats were weaned onto a regular chow diet. Similar to animals born to obese dams, pups raised in SL display early life hyperleptinemia associated with hypothalamic leptin resistance101,102. Postnatal overnutrition also results in reduced responsiveness of hypothalamic neurons to ghrelin during neonatal life, which appears to be the consequence of altered transport of the hormone across the blood–brain barrier103. These endocrine changes during critical periods of postnatal development are associated with a dysregulation of the melanocortin system (Fig. 2). Reduced arcuate Pomc expression has been reported in rats raised in SL87,104. It is known that epigenetic mechanisms of gene regulation, such as DNA methylation and histone modifications, such as methylation, regulate gene expression in response to environmental stimuli. Plagemann and colleagues therefore studied the methylation status of CpG dinucleotides of the Pomc promoter in rats raised in SL. They found that postnatal overfeeding causes alterations in the methylation of the Pomc promoter, particularly on the CpG dinucleotides within the two Sp1‐related binding sequences (Sp1, NF‐κB) that are critical for leptin and insulin’s effects on Pomc gene expression105. Similarly, human studies have shown that childhood obesity is associated with Pomc hypermethylation106. In addition to altering Pomc gene expression in the ARH, postnatal overfeeding also disrupts the neurophysiological responses of PVH neurons to αMSH and AgRP107.
Conclusion
It is now clear from a variety of epidemiological and experimental studies that many chronic diseases, including obesity and type-2 diabetes, may have their roots during neonatal development. A perturbed environment in early life is thought to elicit a range of cellular adaptive responses in key systems, the melanocortin system being one of them. In rodents, the development of the melanocortin system is initiated during mid-gestation and continues during the postnatal period. These developmental windows represent important periods of vulnerability during which perturbations in the perinatal environment may lead to abnormal POMC and AgRP neuron development, causing lifelong metabolic diseases. Therefore, it will be critical to have a comprehensive knowledge of factors that are detrimental or beneficial for the development of the melanocortin system if we want to design intervention studies or treatments. The marked species difference in terms of hypothalamic developmental trajectories is important to consider, as rodents and humans may exhibit different periods of vulnerability to developmental insults or different responses to therapeutic interventions based on the temporal and regional maturation patterns of the hypothalamus. Nevertheless, the mature hypothalamus, whether in rodents or primates, can still exhibit neuroplastic responses, although the degree and nature of hypothalamic remodeling may differ between adults and neonates.
References
Poggioli, R., Vergoni, A. V. & Bertolini, A. ACTH-(1-24) and alpha-MSH antagonize feeding behavior stimulated by kappa opiate agonists. Peptides 7, 843–848 (1986).
Belgardt, B. F. & Brüning, J. C. CNS leptin and insulin action in the control of energy homeostasis. Ann. NY Acad. Sci. 1212, 97–113 (2010).
Williams, K. W. & Elmquist, J. K. From neuroanatomy to behavior: central integration of peripheral signals regulating feeding behavior. Nat. Neurosci. 15, 1350–1355 (2012).
Aponte, Y., Atasoy, D. & Sternson, S. M. AGRP neurons are sufficient to orchestrate feeding behavior rapidly and without training. Nat. Neurosci. 14, 351–355 (2011).
Zhan, C. et al. Acute and long-term suppression of feeding behavior by POMC neurons in the brainstem and hypothalamus, respectively. J. Neurosci. 33, 3624–3632 (2013).
Luquet, S., Perez, F. A., Hnasko, T. S. & Palmiter, R. D. NPY/AgRP neurons are essential for feeding in adult mice but can be ablated in neonates. Science 310, 683–685 (2005).
Gropp, E. et al. Agouti-related peptide-expressing neurons are mandatory for feeding. Nat. Neurosci. 8, 1289–1291 (2005).
Mountjoy, K. G., Mortrud, M. T., Low, M. J., Simerly, R. B. & Cone, R. D. Localization of the melanocortin-4 receptor (MC4-R) in neuroendocrine and autonomic control circuits in the brain. Mol. Endocrinol. 8, 1298–1308 (1994).
Kishi, T. et al. Expression of melanocortin 4 receptor mRNA in the central nervous system of the rat. J. Comp. Neurol. 457, 213–235 (2003).
Liu, H. et al. Transgenic mice expressing green fluorescent protein under the control of the melanocortin-4 receptor promoter. J. Neurosci. 23, 7143–7154 (2003).
Lu, X. Y., Barsh, G. S., Akil, H. & Watson, S. J. Interaction between alpha-melanocyte-stimulating hormone and corticotropin-releasing hormone in the regulation of feeding and hypothalamo-pituitary-adrenal responses. J. Neurosci. 23, 7863–7872 (2003).
Coll, A. P., Farooqi, I. S. & O’Rahilly, S. The hormonal control of food intake. Cell 129, 251–262 (2007).
Sauer, F. C. Mitosis in the neural tube. J. Comp. Neurol. 62, 377–405 (1935).
Khachaturian, H. et al. Development of hypothalamic opioid neurons: a combined immunocytochemical and [3H]thymidine autoradiographic study. Neuropeptides 5, 477–480 (1985).
Padilla, S. L., Carmody, J. S. & Zeltser, L. M. Pomc-expressing progenitors give rise to antagonistic neuronal populations in hypothalamic feeding circuits. Nat. Med. 16, 403–405 (2010).
Bouret, S. G., Draper, S. J. & Simerly, R. B. Formation of projection pathways from the arcuate nucleus of the hypothalamus to hypothalamic regions implicated in the neural control of feeding behavior in mice. J. Neurosci. 24, 2797–2805 (2004).
Grove, K. L., Allen, S., Grayson, B. E. & Smith, M. S. Postnatal development of the hypothalamic neuropeptide Y system. Neuroscience 116, 393–406 (2003).
Nilsson, I., Johansen, J. E., Schalling, M., Hokfelt, T. & Fetissov, S. O. Maturation of the hypothalamic arcuate agouti-related protein system during postnatal development in the mouse. Dev. Brain Res. 155, 147–154 (2005).
Mountjoy, K. G. & Wild, J. M. Melanocortin-4 receptor mRNA expression in the developing autonomic and central nervous systems. Dev. Brain Res. 107, 309–314 (1998).
Glavas, M. M., Joachim, S. E., Draper, S. J., Smith, M. S. & Grove, K. L. Melanocortinergic activation by Melanotan II inhibits feeding and increases uncoupling protein 1 messenger ribonucleic acid in the developing rat. Endocrinology 148, 3279–3287 (2007).
Melnick, I., Pronchuck, N., Cowley, M. A., Grove, K. L. & Colmers, W. F. Developmental switch in neuropeptide Y and melanocortin effects in the paraventricular nucleus of the hypothalamus. Neuron 56, 1103–1115 (2007).
Grayson, B. E. et al. Prenatal development of hypothalamic neuropeptide systems in the nonhuman primate. Neuroscience 143, 975–986 (2006).
Koutcherov, Y., Mai, J. K., Ashwell, K. W. & Paxinos, G. Organization of human hypothalamus in fetal development. J. Comp. Neurol. 446, 301–324 (2002).
Zhang, Y. et al. Position cloning of the mouse obese gene and its human homologue. Nature 372, 425 (1994).
Kojima, M. et al. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 402, 656–660 (1999).
Nakazato, M. et al. A role for ghrelin in the central regulation of feeding. Nature 409, 194–198 (2001).
Halaas, J. L. et al. Weight-reducing effects of the plasma protein encoded by the obese gene. Science 269, 543–546 (1995).
Pelleymounter, M. et al. Effects of the obese gene product on body weight regulation in ob/ob mice. Science 269, 540–543 (1995).
Campfield, L. A., Smith, F. J., Guisez, Y., Devos, R. & Burn, P. Recombinant mouse OB protein: evidence for a peripheral signal linking adiposity and central neural networks. Science 269, 546–549 (1995).
Ahima, R., Prabakaran, D. & Flier, J. Postnatal leptin surge and regulation of circadian rhythm of leptin by feeding. Implications for energy homeostasis and neuroendocrine function. J. Clin. Invest. 101, 1020–1027 (1998).
Ahima, R. S. & Hileman, S. M. Postnatal regulation of hypothalamic neuropeptide expression by leptin: implications for energy balance and body weight regulation. Regul. Pept. 92, 1–7 (2000).
Proulx, K., Richard, D. & Walker, C.-D. Leptin Regulates Appetite-Related Neuropeptides in the Hypothalamus of Developing Rats without Affecting Food Intake. Endocrinology 143, 4683–4692 (2002).
Mistry, A., Swick, A. & Romsos, D. Leptin alters metabolic rates before acquisition of its anorectic effect in developing neonatal mice. Am. J. Physiol. 277, R742–R747 (1999).
Schmidt, I. et al. The effect of leptin treatment on the development of obesity in overfed suckling Wistar rats. Int. J. Obes. Relat. Metab. Disord. 25, 1168–1174 (2001).
Bouret, S. G., Draper, S. J. & Simerly, R. B. Trophic action of leptin on hypothalamic neurons that regulate feeding. Science 304, 108–110 (2004).
Kamitakahara, A., Bouyer, K., Wang, C. H. & Simerly, R. A critical period for the trophic actions of leptin on AgRP neurons in the arcuate nucleus of the hypothalamus. J. Comp. Neurol. 526, 133–145 (2017).
Caron, E., Sachot, C., Prevot, V. & Bouret, S. G. Distribution of leptin-sensitive cells in the postnatal and adult mouse brain. J. Comp. Neurol. 518, 459–476 (2010).
Bouret, S. G., Bates, S. H., Chen, S., Myers, M. G. & Simerly, R. B. Distinct roles for specific leptin receptor signals in the development of hypothalamic feeding circuits. J. Neurosci. 32, 1244–1252 (2012).
Bouret, S. & Simerly, R. B. Development of leptin-sensitive circuits. J. Neuroendocrinol. 19, 575–582 (2007).
Tschöp, M., Smiley, D. L. & Heiman, M. L. Ghrelin induces adiposity in rodent. Nature 407, 908–913 (2000).
Cowley, M. A. et al. The distribution and mechanism of action of ghrelin in the CNS demonstrates a novel hypothalamic circuits regulating energy homeostasis. Neuron 37, 649–661 (2003).
Piao, H. et al. Ghrelin stimulates milk intake by affecting adult type feeding behaviour in postnatal rats. J. Neuroendocrinol. 20, 330–334 (2008).
Steculorum, S. M. et al. Ghrelin programs development of hypothalamic feeding circuits. J. Clin. Invest. 125, 846–858 (2015).
Tolle, V. et al. In vivo and in vitro effects of ghrelin/motilin-related peptide on growth hormone secretion in the rat. Neuroendocrinology 73, 54–61 (2001).
Wasinski, F. et al. Growth hormone receptor deletion reduces the density of axonal projections from hypothalamic arcuate nucleus neurons. Neuroscience 434, 136–147 (2020).
Drucker, D. J. Glucagon-like peptides. Diabetes 47, 159–169 (1998).
Rozo, A. V. et al. Neonatal GLP1R activation limits adult adiposity by durably altering hypothalamic architecture. Mol. Metab. 6, 748–759 (2017).
Li, C. et al. Amylin receptor insensitivity impairs hypothalamic POMC neuron differentiation in the male offspring of maternal high-fat diet-fed mice. Mol. Metab. 44, 101135 (2020).
Abegg, K. et al. Involvement of amylin and leptin in the development of projections from the area postrema to the nucleus of the solitary tract. Front. Endocrinol. (Lausanne) 8, 324 (2017).
Lutz, T. A. et al. Amylin selectively signals onto POMC neurons in the arcuate nucleus of the hypothalamus. Diabetes 67, 805–817 (2018).
Kimura, S. et al. The T/ebp null mouse: thyroid-specific enhancer-binding protein is essential for the organogenesis of the thyroid, lung, ventral forebrain, and pituitary. Genes Dev. 10, 60–69 (1996).
Acampora, D. et al. Progressive impairment of developing neuroendocrine cell lineages in the hypothalamus of mice lacking the Orthopedia gene. Genes Dev. 13, 2787–2800 (1999).
Wang, W. & Lufkin, T. The murine Otp homeobox gene plays an essential role in the specification of neuronal cell lineages in the developing hypothalamus. Dev. Biol. 227, 432–449 (2000).
Marín, O., Baker, J., Puelles, L. & Rubenstein, J. L. R. Patterning of the basal telencephalon and hypothalamus is essential for guidance of cortical projections. Development 129, 761–773 (2002).
Sussel, L., Marin, O., Kimura, S. & Rubenstein, J. L. Loss of Nkx2.1 homeobox gene function results in a ventral to dorsal molecular respecification within the basal telencephalon: evidence for a transformation of the pallidum into the striatum. Development 126, 3359–3370 (1999).
Yee, C. L., Wang, Y., Anderson, S., Ekker, M. & Rubenstein, J. L. R. Arcuate nucleus expression of NKX2.1 and DLX and lineages expressing these transcription factors in neuropeptide Y+, proopiomelanocortin+, and tyrosine hydroxylase+ neurons in neonatal and adult mice. J. Comp. Neurol. 517, 37–50 (2009).
Orquera, D. P. et al. The homeodomain transcription factor NKX2.1 Is essential for the early specification of melanocortin neuron identity and activates Pomc expression in the developing hypothalamus. J. Neurosci. 39, 4023–4035 (2019).
Nasif, S. et al. Islet 1 specifies the identity of hypothalamic melanocortin neurons and is critical for normal food intake and adiposity in adulthood. Proc. Natl Acad. Sci. USA 112, E1861–E1870 (2015).
Lee, B., Lee, S., Lee, S. K. & Lee, J. W. The LIM-homeobox transcription factor Isl1 plays crucial roles in the development of multiple arcuate nucleus neurons. Development 143, 3763–3773 (2016).
Lee, B. et al. Dlx1/2 and Otp coordinate the production of hypothalamic GHRH- and AgRP-neurons. Nat. Commun. 9, 2026 (2018).
Hu, Y. et al. Development and characterization of an Otp conditional loss of function allele. Genesis 58, e23370 (2020).
Manning, L. et al. Regional morphogenesis in the hypothalamus: a BMP-Tbx2 pathway coordinates fate and proliferation through Shh downregulation. Dev. Cell 11, 873–885 (2006).
Shimogori, T. et al. A genomic atlas of mouse hypothalamic development. Nat. Neurosci. 13, 767–775 (2010).
Lagutin, O. V. et al. Six3 repression of Wnt signaling in the anterior neuroectoderm is essential for vertebrate forebrain development. Genes Dev. 17, 368–379 (2003).
Geng, X. et al. Haploinsufficiency of Six3 fails to activate Sonic hedgehog expression in the ventral forebrain and causes holoprosencephaly. Dev. Cell 15, 236–247 (2008).
Lu, F. et al. Rax is a selector gene for mediobasal hypothalamic cell types. J. Neurosci. 33, 259–272 (2013).
Takebayashi, H. et al. Dynamic expression of basic helix-loop-helix Olig family members: implication of Olig2 in neuron and oligodendrocyte differentiation and identification of a new member, Olig3. Mech. Dev. 99, 143–148 (2000).
Zhou, Q., Wang, S. & Anderson, D. J. Identification of a novel family of oligodendrocyte lineage-specific basic helix-loop-helix transcription factors. Neuron 25, 331–343 (2000).
Peng, C. Y., Mukhopadhyay, A., Jarrett, J. C., Yoshikawa, K. & Kessler, J. A. BMP receptor 1A regulates development of hypothalamic circuits critical for feeding behavior. J. Neurosci. 32, 17211–17224 (2012).
Pelling, M. et al. Differential requirements for neurogenin 3 in the development of POMC and NPY neurons in the hypothalamus. Dev. Biol. 349, 406–416 (2011).
Anthwal, N. et al. Conditional deletion of neurogenin-3 using Nkx2.1iCre results in a mouse model for the central control of feeding, activity and obesity. Dis. Model. Mech. 6, 1133–1145 (2013).
McNay, D. E. G., Pelling, M., Claxton, S., Guillemot, F. ß & Ang, S.-L. Mash1 is required for generic and subtype differentiation of hypothalamic neuroendocrine cells. Mol. Endocrinol. 20, 1623–1632 (2006).
Aujla, P. K., Naratadam, G. T., Xu, L. & Raetzman, L. T. Notch/Rbpjκ signaling regulates progenitor maintenance and differentiation of hypothalamic arcuate neurons. Development 140, 3511–3521 (2013).
Croizier, S., Park, S., Maillard, J. & Bouret, S. G. Central Dicer-miR-103/107 controls developmental switch of POMC progenitors into NPY neurons and impacts glucose homeostasis. Elife 7, e40429 (2018).
Quarta, C. et al. Functional identity of hypothalamic melanocortin neurons depends on Tbx3. Nat. Metab. 1, 222–235 (2019).
Tessier-Lavigne, M. & Goodman, C. S. The molecular biology of axon guidance. Science 274, 1123–1133 (1996).
van der Klaauw, A. A. et al. Human Semaphorin 3 variants link melanocortin circuit development and energy balance. Cell 176, 729–742.e718 (2019).
Gervais, M., Labouèbe, G., Picard, A., Thorens, B. & Croizier, S. EphrinB1 modulates glutamatergic inputs into POMC-expressing progenitors and controls glucose homeostasis. PLoS Biol. 18, e3000680 (2020).
Nilsson, I., Johansen, J. E., Schalling, M., Hˆkfelt, T. & Fetissov, S. O. Maturation of the hypothalamic arcuate agouti-related protein system during postnatal development in the mouse. Dev. Brain Res. 155, 147–154 (2005).
Klionsky, D. J. Autophagy: from phenomenology to molecular understanding in less than a decade. Nat. Rev. Mol. Cell Biol. 8, 931–937 (2007).
Komatsu, M. et al. Impairment of starvation-induced and constitutive autophagy in Atg7-deficient mice. J. Cell Biol. 169, 425–434 (2005).
Coupe, B. et al. Loss of autophagy in pro-opiomelanocortin neurons perturbs axon growth and causes metabolic dysregulation. Cell Metab. 15, 247–255 (2012).
Park, S., Aintablian, A., Coupe, B. & Bouret, S. G. The endoplasmic reticulum stress-autophagy pathway controls hypothalamic development and energy balance regulation in leptin-deficient neonates. Nat. Commun. 11, 1914 (2020).
Fuchs, J. L. & Schwark, H. D. Neuronal primary cilia: a review. Cell Biol. Int. 28, 111–118 (2004).
Carreno, G. et al. Hypothalamic sonic hedgehog is required for cell specification and proliferation of LHX3/LHX4 pituitary embryonic precursors. Development 144, 3289–3302 (2017).
Lee, C. H. et al. Primary cilia mediate early life programming of adiposity through lysosomal regulation in the developing mouse hypothalamus. Nat. Commun. 11, 5772 (2020).
Siljee, J. E. et al. Subcellular localization of MC4R with ADCY3 at neuronal primary cilia underlies a common pathway for genetic predisposition to obesity. Nat. Genet. 50, 180 (2018).
Chen, H., Simar, D. & Morris, M. J. Hypothalamic neuroendocrine circuitry is programmed by maternal obesity: interaction with postnatal nutritional environment. PLoS ONE 4, e6259 (2009).
Kirk, S. L. et al. Maternal obesity induced by diet in rats permanently influences central processes regulating food intake in offspring. PLoS ONE 4, e5870 (2009).
Vogt, M. C. et al. Neonatal insulin action impairs hypothalamic neurocircuit formation in response to maternal high-fat feeding. Cell 156, 495–509 (2014).
Park, S., Jang, A. & Bouret, S. G. Maternal obesity-induced endoplasmic reticulum stress causes metabolic alterations and abnormal hypothalamic development in the offspring. PLoS Biol. 18, e3000296 (2020).
Haddad-Tóvolli, R. et al. Pro-opiomelanocortin (POMC) neuron translatome signatures underlying obesogenic gestational malprogramming in mice. Mol. Metab. 36, 100963 (2020).
Sullivan, E. L. et al. Maternal and postnatal high-fat diet consumption programs energy balance and hypothalamic melanocortin signaling in nonhuman primate offspring. Am. J. Physiol. Regul. Integr. Comp. Physiol. 313, R169–r179 (2017).
Levin, B. E., Dunn-Meynell, A. A., Balkan, B. & Keesey, R. E. Selective breeding for diet-induced obesity and resistance in Sprague-Dawley rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 273, R725–R730 (1997).
Bouret, S. G. et al. Hypothalamic neural projections are permanently disrupted in diet-induced obese rats. Cell Metab. 7, 179–185 (2008).
Horvath, T. L. et al. Synaptic input organization of the melanocortin system predicts diet-induced hypothalamic reactive gliosis and obesity. Proc. Natl Acad. Sci. USA 107, 14875–14880 (2010).
Dearden, L., Buller, S., Furigo, I. C., Fernandez-Twinn, D. S. & Ozanne, S. E. Maternal obesity causes fetal hypothalamic insulin resistance and disrupts development of hypothalamic feeding pathways. Mol. Metab. 42, 101079 (2020).
Johnson, M. D. et al. Early postnatal amylin treatment enhances hypothalamic leptin signaling and neural development in the selectively bred diet-induced obese rat. Am. J. Physiol. Regul. Integr. Comp. Physiol. 311, R1032–R1044 (2016).
Kennedy, G. C. The development with age of hypothalamic restraint upon the appetite of the rat. J. Endocrinol. 16, 9/17 (1957).
Widdowson, E. M. & McCance, R. Some effects of accelerating growth. I. General somatic development. Proc. R. Soc. Lond. B Biol. Sci. 152, 188–206 (1960).
Glavas, M. M. et al. Early overnutrition results in early-onset arcuate leptin resistance and increased sensitivity to high-fat diet. Endocrinology 151, 1598–1610 (2010).
Roberts, B. L., Bennett, C. M., Carroll, J. M., Lindsley, S. R. & Kievit, P. Early overnutrition alters synaptic signaling and induces leptin resistance in arcuate proopiomelanocortin neurons. Physiol. Behav. 206, 166–174 (2019).
Collden, G. et al. Neonatal overnutrition causes early alterations in the central response to peripheral ghrelin. Mol. Metab. 4, 15–24 (2015).
Srinivasan, M. et al. A high-carbohydrate diet in the immediate postnatal life of rats induces adaptations predisposing to adult-onset obesity. J. Endocrinol. 197, 565–574 (2008).
Plagemann, A. et al. Hypothalamic proopiomelanocortin promoter methylation becomes altered by early overfeeding: an epigenetic model of obesity and the metabolic syndrome. J. Physiol. 587, 4963–4976 (2009).
Kuehnen, P. et al. An Alu element-associated hypermethylation variant of the POMC gene is associated with childhood obesity. PLoS Genet. 8, e1002543 (2012).
Davidowa, H., Li, Y. & Plagemann, A. Altered responses to orexigenic (AGRP, MCH) and anorexigenic (a-MSH, CART) neuropeptides of paraventricular hypothalamic neurons in early postnatally overfed rats. Eur. J. Neurosci. 18, 613–621 (2003).
Acknowledgements
Work from the author’s laboratory is supported by the French National Institute of Health (Inserm, grant 1172) and the Foundation for Prader-Willi Research. Figures were created with BioRender.com.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bouret, S.G. Developmental programming of hypothalamic melanocortin circuits. Exp Mol Med 54, 403–413 (2022). https://doi.org/10.1038/s12276-021-00625-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s12276-021-00625-8
This article is cited by
-
The role of central neurotransmitters in appetite regulation of broilers and layers: similarities and differences
Veterinary Research Communications (2024)