Abstract
Diffuse gliomas are the most common malignant brain tumours in adults and include glioblastomas and World Health Organization (WHO) grade II and grade III tumours (sometimes referred to as lower-grade gliomas). Genetic tumour profiling is used to classify disease and guide therapy1,2, but involves brain surgery for tissue collection; repeated tumour biopsies may be necessary for accurate genotyping over the course of the disease3,4,5,6,7,8,9,10. While the detection of circulating tumour DNA (ctDNA) in the blood of patients with primary brain tumours remains challenging11,12, sequencing of ctDNA from the cerebrospinal fluid (CSF) may provide an alternative way to genotype gliomas with lower morbidity and cost13,14. We therefore evaluated the representation of the glioma genome in CSF from 85 patients with gliomas who underwent a lumbar puncture because they showed neurological signs or symptoms. Here we show that tumour-derived DNA was detected in CSF from 42 out of 85 patients (49.4%) and was associated with disease burden and adverse outcome. The genomic landscape of glioma in the CSF included a broad spectrum of genetic alterations and closely resembled the genomes of tumour biopsies. Alterations that occur early during tumorigenesis, such as co-deletion of chromosome arms 1p and 19q (1p/19q codeletion) and mutations in the metabolic genes isocitrate dehydrogenase 1 (IDH1) or IDH21,2, were shared in all matched ctDNA-positive CSF–tumour pairs, whereas growth factor receptor signalling pathways showed considerable evolution. The ability to monitor the evolution of the glioma genome through a minimally invasive technique could advance the clinical development and use of genotype-directed therapies for glioma, one of the most aggressive human cancers.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All genomic results and associated clinical data for all patients in this study are publically available in the cBioPortal for Cancer Genomics at the following URL: http://www.cbioportal.org/study?id=glioma_msk_2018. The MSK-IMPACT data analysis pipeline can be found here: https://github.com/rhshah/IMPACT-Pipeline. The source data for Table 1 and Extended Data Fig. 1 are available in Supplementary Table 1. The source data for the multivariable analysis (Extended Data Table 2) are available in Supplementary Table 2. The source data for the matched pair analysis (Fig. 2a, b) are available in Supplementary Table 5 (separate MS Excel file).
References
Louis, D. N. et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 131, 803–820 (2016).
Cancer Genome Atlas Research Network. Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455, 1061–1068 (2008).
Suzuki, H. et al. Mutational landscape and clonal architecture in grade II and III gliomas. Nat. Genet. 47, 458–468 (2015).
Johnson, B. E. et al. Mutational analysis reveals the origin and therapy-driven evolution of recurrent glioma. Science 343, 189–193 (2014).
Aihara, K. et al. Genetic and epigenetic stability of oligodendrogliomas at recurrence. Acta Neuropathol. Commun. 5, 18 (2017).
Bai, H. et al. Integrated genomic characterization of IDH1-mutant glioma malignant progression. Nat. Genet. 48, 59–66 (2016).
Kim, H. et al. Whole-genome and multisector exome sequencing of primary and post-treatment glioblastoma reveals patterns of tumor evolution. Genome Res. 25, 316–327 (2015).
Kim, J. et al. Spatiotemporal evolution of the primary glioblastoma genome. Cancer Cell 28, 318–328 (2015).
Wang, J. et al. Clonal evolution of glioblastoma under therapy. Nat. Genet. 48, 768–776 (2016).
Lee, J. K. et al. Spatiotemporal genomic architecture informs precision oncology in glioblastoma. Nat. Genet. 49, 594–599 (2017).
Merker, J. D. et al. Circulating tumor DNA analysis in patients with cancer: American Society of Clinical Oncology and College of American Pathologists joint review. J. Clin. Oncol. 36, 1631–1641 (2018).
Bettegowda, C. et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci. Transl. Med. 6, 224ra24 (2014).
Pentsova, E. I. et al. Evaluating cancer of the central nervous system through next-generation sequencing of cerebrospinal fluid. J. Clin. Oncol. 34, 2404–2415 (2016).
Wang, Y. et al. Detection of tumor-derived DNA in cerebrospinal fluid of patients with primary tumors of the brain and spinal cord. Proc. Natl Acad. Sci. USA 112, 9704–9709 (2015).
Cheng, D. T. et al. Memorial Sloan Kettering-integrated mutation profiling of actionable cancer targets (MSK-IMPACT): a hybridization capture-based next-generation sequencing clinical assay for solid tumor molecular oncology. J. Mol. Diagn. 17, 251–264 (2015).
Brat, D. J. et al. Comprehensive, integrative genomic analysis of diffuse lower-grade gliomas. N. Engl. J. Med. 372, 2481–2498 (2015).
Eckel-Passow, J. E. et al. Glioma groups based on 1p/19q, IDH, and TERT promoter mutations in tumors. N. Engl. J. Med. 372, 2499–2508 (2015).
Tomita-Mitchell, A. et al. Mismatch repair deficient human cells: spontaneous and MNNG-induced mutational spectra in the HPRT gene. Mutat. Res. 450, 125–138 (2000).
Hunter, C. et al. A hypermutation phenotype and somatic MSH6 mutations in recurrent human malignant gliomas after alkylator chemotherapy. Cancer Res. 66, 3987–3991 (2006).
Alexandrov, L. B. et al. Signatures of mutational processes in human cancer. Nature 500, 415–421 (2013).
Brennan, C. W. et al. The somatic genomic landscape of glioblastoma. Cell 155, 462–477 (2013).
Parsons, D. W. et al. An integrated genomic analysis of human glioblastoma multiforme. Science 321, 1807–1812 (2008).
AACR Project GENIE Consortium. AACR Project GENIE: powering precision medicine through an international consortium. Cancer Discov. 7, 818–831 (2017).
Zehir, A. et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat. Med. 23, 703–713 (2017).
Wen, P. Y. et al. Response assessment in neuro-oncology clinical trials. J. Clin. Oncol. 35, 2439–2449 (2017).
Abecasis, G. R. et al. An integrated map of genetic variation from 1,092 human genomes. Nature 491, 56–65 (2012).
Thorvaldsdóttir, H., Robinson, J. T. & Mesirov, J. P. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief. Bioinform. 14, 178–192 (2013).
Shen, R. & Seshan, V. E. FACETS: allele-specific copy number and clonal heterogeneity analysis tool for high-throughput DNA sequencing. Nucleic Acids Res. 44, e131 (2016).
Acknowledgements
This research was supported by the National Brain Tumor Society Defeat GBM Initiative (I.K.M.), the National Institutes of Health (1 R35 NS105109 01 and P30CA008748), Cycle of Survival (I.K.M.), the American Brain Tumor Association (E.I.P.), the Marie Josée and Henry R. Kravis Center for Molecular Oncology, the MSK Brain Tumor Center, and the MSK Neuro-Oncology Research in Translation (NORTH) Program.
Reviewer information
Nature thanks A. Bardelli, O. Rueda, M. Taylor and R. Verhaak for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
A.M.M., R.H.S., E.I.P., L.M.D., R.J.Y., M.F.B. and I.K.M. conceived and designed the study. A.M.M., R.H.S., E.I.P., R.J.Y., M.F.B. and I.K.M. collected and assembled the data. A.M.M., R.H.S., E.I.P., M.P., S.B., N.D., A. Skakodub, S.D.S., L.L., F.M., X.J., C.G., A.V., M.M.S., V.T., C.W.B., M.R., R.J.Y., M.F.B. and I.K.M. were responsible for provision of the study materials and the patients. A.M.M., R.H.S., E.I.P., Y.Z., A.S.R., K.S.P., R.J.Y., M.F.B. and I.K.M. analysed and interpreted the data. M.P., C.C., S.A.M., A. Samoila and F.M. processed the CSF and blood samples. A.M.M., R.H.S., E.I.P., W.-Y.H., T.A.B., A.V., L.M.D., K.S.P., R.J.Y., M.F.B. and I.K.M. provided administrative, material and technical support. A.M.M., R.H.S., E.I.P., D.W.Y.T., C.G., L.M.D., K.S.P., R.J.Y., M.F.B. and I.K.M. wrote the manuscript. All authors approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
E.I.P. reports advisory roles with AstraZeneca. V.T. is a founding investigator of Blue Rock Therapeutics. K.S.P. reports stock ownership in Pfizer. L.M.D. reports advisory roles for Sapience Therapeutics, Tocagen, BTG International, Roche, and Syndax. R.J.Y. reports research funding from Agios and advisory roles with Icon plc, NordicNeuroLab, and Puma Biotechnology. M.F.B. reports advisory roles with Roche and research funding from Illumina. I.K.M. reports research funding from General Electric, Amgen, and Lilly; advisory roles with Agios, Puma Biotechnology, and Debiopharm Group; and honoraria from Roche for a presentation.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Interval between diagnosis and CSF collection, grouped by glioma subtype.
For the comparison between the GBM (IDH WT) and the LGG (IDH WT) groups, P not significant at 0.16; between GBM (IDH WT) and LGG (IDH mutant), P = 0.0000000689; between LGG (IDH WT) and LGG (IDH mutant), P = 0.0054. Wilcoxon two-sample test was used for two-way comparisons. No adjustments were made for multiple comparisons. The box-plot elements are as follows: all patients (n = 85, grey): median, 510; minimum, 62; maximum, 9,122; 25th percentile, 273; 75th percentile, 1,606. GBM (IDH WT) (n = 44, red): median, 355; minimum, 62; maximum, 1,606; 25th percentile, 193; 75th percentile, 528. LGG (IDH WT) (n = 12, green): median, 473; minimum, 79; maximum, 2,982; 25th percentile, 292; 75th percentile, 1,013. LGG (IDH mutant) (n = 24, blue): median, 2,077; minimum, 63; maximum, 7,669; 25th percentile, 1,061; 75th percentile, 4,274. *Five patients were excluded from sub-group analysis owing to unknown IDH status (n = 3) or IDH mutant GBM (n = 2).
Extended Data Fig. 2 Glioma growth towards CSF spaces.
Representative brain MRI examples (T1 post-contrast) from patients with distinct patterns of tumour spread. Spread of enhancing disease to the pial, subependymal and subarachnoid spaces was used as an imaging surrogate to estimate tumour spread into the CSF, which is otherwise not visible by MRI. a, Enhancing leptomeningeal spread along bilateral cranial nerves VII and VIII (arrows). b, Enhancing pial spread to the surface of the pons (arrows). c, Nodular and curvilinear enhancing subependymal spread along both lateral ventricles (arrows).
Extended Data Fig. 3 Interval between CSF collection and death for patients with positive (blue) and negative (red) CSF ctDNA.
a, All patients with glioma. Median overall survival (OS): for CSF ctDNA-positive patients, 3.15 months (95% confidence interval, 1.97–4.63); for CSF ctDNA-negative patients, 11.91 months (95% confidence interval, 8.40–30.81). The log-rank P value for comparing the survival experience of all patients with glioma stratified by ctDNA status was 0.0000078675. b, Patients with GBM (IDH WT). Median overall survival: for CSF ctDNA-positive subjects, 2.04 months (95% confidence interval, 0.98–3.77); for CSF ctDNA-negative subjects, 9.89 months (95% confidence interval, 5.54–12.39). The log-rank P value for comparing the survival experience of patients with GBM (IDH WT) by ctDNA status was 0.000062396 (log-rank test, two-sided).
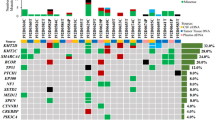
Extended Data Fig. 4 Concordance between CSF and tumour in glioma subtype-defining genes.
Shown are combinations of genetic alterations (LGG signatures) that are consistently congruent between the CSF and tumour (10/10). This was also the case in glioblastoma (20/20).
Extended Data Fig. 5 DNA hypermutation signature in CSF.
Disease course for patient 36 with GBM with two tumour resections and one CSF collection. The patient received 14 monthly cycles of temozolomide (TMZ) following the initial tumour resection and postoperative radiation (RT)/TMZ. The initial tumour harboured five mutations, the recurrent tumour 120 mutations and the CSF 132 mutations. MRIs (T1 post-contrast) are shown from the time of diagnosis, first recurrence and second recurrence. The original tumour was in the right parietal lobe and recurrence was in the right frontal lobe. Diamond, tumour samples profiled; circle, CSF sample profiled. Bev, bevacizumab. The bar graph shows the precise number of SNVs that were called by the IMPACT pipeline in the recurrent tumour (n = 120 independent somatic SNVs) and in CSF ctDNA (n = 132 independent somatic SNVs; INDELs were excluded). Bar graphs show the precise number of SNVs for each of the possible trinucleotide combinations.
Extended Data Fig. 6 Variant allelic frequencies for all SNVs in two independently collected CSF samples from patient 34 with DNA hypermutation.
Scatter plot of variant allelic frequencies for all SNVs in two independently collected CSF samples from patient 34. Both CSF replicates harboured more than 200 SNVs. Pearson correlation coefficient (r2 = 0.966) was calculated using a linear regression model in R (following Gist (https://gist.github.com/rhshah/3f4965a80886affb96d847dc2ecf69f5)).
Extended Data Fig. 7 Divergence of tumour and CSF profiles over time.
The histogram (top) depicts the interval (in days) between tumour and CSF collection. The pie charts (bottom) show that the samples that were collected at a very close interval (<3 weeks; red) had a higher percentage of shared mutations (79%) than the samples that were collected at a longer interval (>1,000 days; blue)(29%).
Extended Data Fig. 8 Evolution of the glioma genome.
a, Disease course of patient 28 (GBM (IDH WT)) who received treatment with concurrent RT/TMZ, bevacizumab, and a PD-1 inhibitor. The patient underwent three tumour resections and one CSF collection and all four biospecimens were sequenced. The CDK4 amplification was seen in all four samples. Amplifications of PDGFRA/KIT were observed in tumour sample 3, whereas the later CSF sample (4) no longer showed the PDGFRA/KIT amplification. b, Disease course of patient 7 (IDH mutant anaplastic astrocytoma). The patient underwent four tumour resections and two CSF collections. All six samples were profiled. MRIs (T1 post-contrast) correspond to the time of each tissue resection or CSF recollection. Bottom, heat map shows all mutations across the six samples. Diamond, tumour samples profiled; circle, CSF samples profiled. Heat map indicates the variant allelic frequency of the indicated SNVs.
Supplementary information
Supplementary Tables
This file contains Supplementary Tables 1-4. Supplementary Table 1 includes the demographic data for the patients in our glioma cohort. Supplementary Table 2 contains the source data for the multivariable model for overall survival from the time of CSF collection. Supplementary Table 3 contains comparison data between plasma and CSF ctDNA. Supplementary Table 4 details the sequence variants detected in the plasma ctDNA
Supplementary Table 5
Matched pair analysis complete mutation list. SNVs detected in tumor and CSF from 36 patients with glioma with positive CSF ctDNA and available tumor tissue for comparison
Rights and permissions
About this article
Cite this article
Miller, A.M., Shah, R.H., Pentsova, E.I. et al. Tracking tumour evolution in glioma through liquid biopsies of cerebrospinal fluid. Nature 565, 654–658 (2019). https://doi.org/10.1038/s41586-019-0882-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-019-0882-3
This article is cited by
-
BCOR::CREBBP fusion in malignant neuroepithelial tumor of CNS expands the spectrum of methylation class CNS tumor with BCOR/BCOR(L1)-fusion
Acta Neuropathologica Communications (2024)
-
IDH1 mutation is detectable in plasma cell-free DNA and is associated with survival outcome in glioma patients
BMC Cancer (2024)
-
Beyond invasive biopsies: using VASARI MRI features to predict grade and molecular parameters in gliomas
Cancer Imaging (2024)
-
Sequencing of cerebrospinal fluid cell-free DNA facilitated early differential diagnosis of intramedullary spinal cord tumors
npj Precision Oncology (2024)
-
Single-cell atlas reveals the immunosuppressive microenvironment and Treg cells landscapes in recurrent Glioblastoma
Cancer Gene Therapy (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.