Abstract
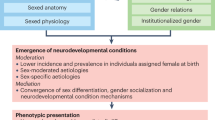
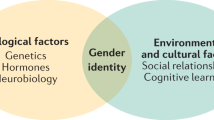
Sexual and gender minority (LGBT+) people face unique health disparities that must be considered by health-care providers to ensure equitable and inclusive care. Although traditionally LGBT+ health has not been integrated into neurology training, sexual orientation and gender identity have direct relevance to neurological health, driven by both systemic and interpersonal factors. In this Review, we summarize the evidence for associations between sexual orientation and gender identity with the prevalence and outcomes of various neurological conditions, including neurodegenerative diseases, epilepsy, stroke and neurodevelopmental disorders, among others. We describe important clinical considerations pertaining to LGBT+ people and recommend language and practices to promote inclusive care, as well as highlight gaps in need of further research and possible strategies to minimize these, including systematic collection of sexual orientation and gender identity and use of inclusive language.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ipsos Global Advisor. LGBT+ Pride 2023. Ipsos www.ipsos.com/sites/default/files/ct/news/documents/2023-05/Ipsos%20LGBT%2B%20Pride%202023%20Global%20Survey%20Report%20-%20rev.pdf (2023).
Rosendale, N. & Josephson, S. A. The importance of lesbian, gay, bisexual, and transgender health in neurology: what’s in a name? JAMA Neurol. 72, 855–856 (2015).
Wilson, B. D. M. et al. LGBT poverty in the United States. Williams Institute https://williamsinstitute.law.ucla.edu/publications/lgbt-poverty-us/ (2023).
Abril, S. B. et al. The worldwide offensive against the rights of LGBTQ+ people. EL PAÍS English https://english.elpais.com/international/2023-06-28/the-worldwide-offensive-against-the-rights-of-lgbtq-people.html (2023).
Rosendale, N. et al. Migraine, migraine disability, trauma, and discrimination in sexual and gender minority individuals. Neurology 99, e1549–e1559 (2022).
Flentje, A. et al. Minority stress, structural stigma, and physical health among sexual and gender minority individuals: examining the relative strength of the relationships. Ann. Behav. Med. 56, 573–591 (2022).
Streed, C. G. et al. Assessing and addressing cardiovascular health in people who are transgender and gender diverse: a scientific statement from the American Heart Association. Circulation 144, e136–e148 (2021).
Flentje, A., Heck, N. C., Brennan, J. M. & Meyer, I. H. The relationship between minority stress and biological outcomes: a systematic review. J. Behav. Med. 43, 673–694 (2020).
Zeeman, L. et al. A review of lesbian, gay, bisexual, trans and intersex (LGBTI) health and healthcare inequalities. Eur. J. Public Health 29, 974–980 (2019).
Casey, L. S. et al. Discrimination in the United States: experiences of lesbian, gay, bisexual, transgender, and queer Americans. Health Serv. Res. 54, 1454–1466 (2019).
James, S. E. et al. The report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality http://www.ustranssurvey.org/ (2019).
Brown, T. T. et al. Discrimination hurts: the effect of discrimination on the development of chronic pain. Soc. Sci. Med. 204, 1–8 (2018).
Mathur, V. A. et al. Multiple levels of suffering: discrimination in health-care settings is associated with enhanced laboratory pain sensitivity in sickle cell disease. Clin. J. Pain 32, 1076–1085 (2016).
Watson, R. J. et al. LGBTQ state policies: a lever for reducing SGM youth substance use and bullying. Drug Alcohol Depend. 221, 108659 (2021).
Chien, Y. S., Schwartz, G., Huang, L. & Kawachi, I. State LGBTQ policies and binge drinking among sexual minority youth in the US: a multilevel analysis. Soc. Psychiatry Psychiatr. Epidemiol. 57, 183–194 (2022).
Carbado, D. W., Crenshaw, K. W., Mays, V. M. & Tomlinson, B. Intersectionality: mapping the movements of a theory. Du Bois Rev. 10, 303–312 (2013).
Shangani, S., Gamarel, K. E., Ogunbajo, A., Cai, J. & Operario, D. Intersectional minority stress disparities among sexual minority adults in the USA: the role of race/ethnicity and socioeconomic status. Cult. Health Sex. 22, 398–412 (2020).
HRC Foundation. Fatal violence against the transgender and gender-expansive community in 2022. hrc.org, https://www.hrc.org/resources/fatal-violence-against-the-transgender-and-gender-expansive-community-in-2022 (2022).
Dawson L., Long M. & Frederiksen B. LGBT+ people’s health status and access to care — issue brief — 10171. KFF www.kff.org/report-section/lgbt-peoples-health-status-and-access-to-care-issue-brief/ (2023).
Lavorgna, L. et al. Health-care disparities stemming from sexual orientation of Italian patients with multiple sclerosis: a cross-sectional web-based study. Mult. Scler. Relat. Disord. 13, 28–32 (2017).
Anderson, A. et al. Experiences of sexual and gender minority people living with multiple sclerosis in northern California: an exploratory study. Mult. Scler. Relat. Disord. 55, 103214 (2021).
Bayram, E., Weigand, A. J. & Flatt, J. D. Perceived discrimination in health care for LGBTQIA+ people living with Parkinson’s disease. J. Gerontol. Ser. B 78, 1459–1465 (2023).
Lambrou, N. H. et al. Subjective cognitive decline associated with discrimination in medical settings among transgender and nonbinary older adults. Int. J. Env. Res. Public Health 19, 9168 (2022).
Barrett, C., Crameri, P., Lambourne, S., Latham, J. & Whyte, C. Understanding the experiences and needs of lesbian, gay, bisexual and trans Australians living with dementia, and their partners: LGBT Australians and dementia. Australas. J. Ageing 34, 34–38 (2015).
Candrian, C., Burke, E. S., Kline, D. & Torke, A. M. Experiences of caregiving with Alzheimer’s disease in the LGBT community. BMC Geriatr. 23, 293 (2023).
Warrier, V. et al. Elevated rates of autism, other neurodevelopmental and psychiatric diagnoses, and autistic traits in transgender and gender-diverse individuals. Nat. Commun. 11, 3959 (2020).
George, R. & Stokes, M. A. Gender identity and sexual orientation in autism spectrum disorder. Autism 22, 970–982 (2018).
Hillier, A. et al. LGBTQ+ and autism spectrum disorder: experiences and challenges. Int. J. Transgend. Health 21, 98–110 (2020).
Hall, J. P., Batza, K., Streed, C. G., Boyd, B. A. & Kurth, N. K. Health disparities among sexual and gender minorities with autism spectrum disorder. J. Autism Dev. Disord. 50, 3071–3077 (2020).
Ghebrehiwet, M. et al. Inequities in epilepsy: a scoping review. Neurol. Clin. Pract. 13, e200211 (2023).
Waldman, G. & Benson, R. Epilepsy care in transgender patients. Curr. Neurol. Neurosci. Rep. 22, 451–458 (2022).
Johnson, E. L. & Kaplan, P. W. Caring for transgender patients with epilepsy. Epilepsia 58, 1667–1672 (2017).
Birbeck, G. L. et al. Evidence-based guideline: antiepileptic drug selection for people with HIV/AIDS. Neurology 78, 139–145 (2012).
Reimers, A., Brodtkorb, E. & Sabers, A. Interactions between hormonal contraception and antiepileptic drugs: clinical and mechanistic considerations. Seizure 28, 66–70 (2015).
Herzog, A. G. et al. Differential effects of antiepileptic drugs on sexual function and hormones in men with epilepsy. Neurology 65, 1016–1020 (2005).
Christensen, J. et al. Oral contraceptives induce lamotrigine metabolism: evidence from a double-blind, placebo-controlled trial. Epilepsia 48, 484–489 (2007).
Trinh, M. H., Agénor, M., Austin, S. B. & Jackson, C. L. Health and healthcare disparities among U.S. women and men at the intersection of sexual orientation and race/ethnicity: a nationally representative cross-sectional study. BMC Public Health 17, 964 (2017).
Diaz, M. A. & Rosendale, N. Exploring stroke risk factors and outcomes in sexual and gender minority people. Neurol. Clin. Pract. 13, e200106 (2003).
Defreyne, J., de Bruaene, L. D. L. V., Rietzschel, E., Schuylenbergh, J. V. & T’Sjoen, G. G. R. Effects of gender-affirming hormones on lipid, metabolic, and cardiac surrogate blood markers in transgender persons. Clin. Chem. 65, 119–134 (2019).
Nota Nienke, M. et al. The occurrence of acute cardiovascular events in transgender individuals receiving hormone therapy: results from a large cohort study. Circulation 139, 1461–1462 (2019).
Getahun, D. et al. Cross-sex hormones and acute cardiovascular events in transgender persons: a cohort study. Ann. Intern. Med. 169, 205–213 (2018).
Maraka, S. et al. Sex steroids and cardiovascular outcomes in transgender individuals: a systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 102, 3914–3923 (2017).
Diaz, M. & Rosendale, N. Diagnosis, treatment, and prevention of stroke in transgender adults. Curr. Treat. Options Neurol. 24, 409–428 (2022).
Coleman, E. et al. Standards of care for the health of transgender and gender diverse people, version 8. Int. J. Transgend. Health 23, S1–S259 (2022).
Safavi-Naeini, P. & Razavi, M. Postural orthostatic tachycardia syndrome. Tex. Heart Inst. J. 47, 57–59 (2020).
Boris, J. R., McClain, Z. B. R. & Bernadzikowski, T. Clinical course of transgender adolescents with complicated postural orthostatic tachycardia syndrome undergoing hormonal therapy in gender transition: a case series. Transgend. Health 4, 331–334 (2019).
Tran, H. A. & Reeves, G. E. Hepatitis C infection and thyrotoxic periodic paralysis — a novel use of an old drug. Am. J. Med. Sci. 336, 515–518 (2008).
Lanman, T. A. et al. Sexual reassignment fails to prevent Kennedy’s disease. J. Neuromuscul. Dis. 3, 121–125 (2016).
Patel, R. A., Stebbins, G. & Witek, N. Sexual orientation and gender identity documentation at an academic movement disorders neurology clinic. Clin. Park. Relat. Disord. 7, 100164 (2022).
Patel, R. & Kompoliti, K. Sex and gender differences in Parkinson’s disease. Neurol. Clin. 41, 371–379 (2023).
Parkinson’s Foundation. LGBTQ+ & Parkinson’s. Parkinson’s Foundation www.parkinson.org/living-with-parkinsons/finding-care/lgbtq (2023).
Flatt, J. D. et al. Correlates of subjective cognitive decline in lesbian, gay, bisexual, and transgender older adults. J. Alzheimers Dis. 64, 91–102 (2018).
Guo, Y. et al. Prevalence of Alzheimer’s and related dementia diseases and risk factors among transgender adults, Florida, 2012-2020. Am. J. Public Health 112, 754–757 (2022).
Barbee, H. & McKay, T. Do supportive work environments matter for minority aging? Work stress and subjective cognitive impairment among middle-age and older lesbian, gay, bisexual, transgender, and queer adults. Acta Psychol. 237, 103949 (2023).
Barrett, C., Crameri, P., Lambourne, S., Latham, J. R. & Whyte, C. Understanding the experiences and needs of lesbian, gay, bisexual and trans Australians living with dementia, and their partners. Australas. J. Ageing 34, 34–38 (2023).
Pakpoor, J., Wotton, C. J., Schmierer, K., Giovannoni, G. & Goldacre, M. J. Gender identity disorders and multiple sclerosis risk: a national record-linkage study. Mult. Scler. 22, 1759–1762 (2016).
Rosendale, N., Wong, J. O., Flatt, J. D. & Whitaker, E. Sexual and gender minority health in neurology: a scoping review. JAMA Neurol. 78, 747–754 (2021).
Nota, N. M. et al. The occurrence of benign brain tumours in transgender individuals during cross-sex hormone treatment. Brain 141, 2047–2054 (2018).
Tollinche, L. E., Rosa, W. E. & van Rooyen, C. D. Perioperative considerations for person-centered gender affirming surgery. Adv. Anesth. 39, 77–96 (2021).
Johannsen, M., Christensen, S., Zachariae, R. & Jensen, A. Socio-demographic, treatment-related, and health behavioral predictors of persistent pain 15 months and 7–9 years after surgery: a nationwide prospective study of women treated for primary breast cancer. Breast Cancer Res. Treat. 152, 645–658 (2015).
Jolly, D., Chrisos, H. A., Kaufman-Goldberg, T., Ganor, O. & Taghinia, A. H. Median nerve neuropathy following radial forearm free flap phalloplasty: a case report. Plast. Reconstr. Surg. Glob. Open 8, e3027 (2020).
Orozco-Poore, C. & Keuroghlian, A. S. Neurological considerations for “nerve-sparing” cosmetic genital surgeries performed on children with XX chromosomes diagnosed with 21-hydroxylase congenital adrenal hyperplasia and clitoromegaly. LGBT Health https://doi.org/10.1089/lgbt.2022.0160 (2023).
Pringsheim, T. & Gooren, L. Migraine prevalence in male to female transsexuals on hormone therapy. Neurology 63, 593–594 (2004).
Yalinay Dikmen, P. et al. Primary headaches among gender dysphoric female-to-male individuals: a cross-sectional survey on gender transition experience. Headache 61, 1194–1206 (2021).
Nagata, J. M., Ganson, K. T., Tabler, J., Blashill, A. J. & Murray, S. B. Disparities across sexual orientation in migraine among US adults. JAMA Neurol. 78, 117–118 (2021).
Ahmad, S. R. & Rosendale, N. Sex and gender considerations in episodic migraine. Curr. Pain Headache Rep. 26, 505–516 (2022).
Hranilovich, J. A., Kaiser, E. A., Pace, A., Barber, M. & Ziplow, J. Headache in transgender and gender-diverse patients: a narrative review. Headache 61, 1040–1050 (2021).
Caceres, B. A. & Hickey, K. T. Examining sleep duration and sleep health among sexual minority and heterosexual adults: findings from NHANES (2005–2014). Behav. Sleep Med. 18, 345–357 (2020).
Gennaro, L. D. & Cordone, S. Mounting evidence on the relationship between sleep and Alzheimer’s disease. J. Integr. Neurosci. 23, 21 (2024).
Christensen, K. A., van Dyk Seager, I. & Klaver, E. Elevated insomnia symptom severity in university students: the role of sexual orientation and internalizing symptoms. J. Am. Coll. Health https://doi.org/10.1080/07448481.2022.2145897 (2023).
Huang, X. et al. Burden of sleep disturbances and associated risk factors: a cross-sectional survey among HIV-infected persons on antiretroviral therapy across China. Sci. Rep. 7, 3657 (2017).
Levenson, J. C., Thoma, B. C., Hamilton, J. L., Choukas-Bradley, S. & Salk, R. H. Sleep among gender minority adolescents. Sleep 44, zsaa185 (2021).
Eom, Y. J. et al. Discrimination keeps transgender people awake at night: a nationwide cross-sectional survey of 583 transgender adults in South Korea. Sleep Health 8, 580–586 (2022).
Choo, S. et al. Association between discrimination and poor sleep health outcomes among 2192 South Korean gay, lesbian, and bisexual adults: a nationwide cross-sectional survey. Sleep Health 8, 587–592 (2022).
Gavidia, R. et al. Gender identity and transition: relationships with sleep disorders in US youth. J. Clin. Sleep Med. 18, 2553–2559 (2022).
Moreno, A., Laoch, A. & Zasler, N. D. Changing the culture of neurodisability through language and sensitivity of providers: creating a safe place for LGBTQIA+ people. Neurorehabilitation 41, 375–393 (2017).
Rosendale, N. et al. Systematic collection of sexual orientation and gender identity in a public health system: the San Francisco Health Network SO/GI Systems-Change Initiative. Jt Comm. J. Qual. Patient Saf. 46, 549–557 (2020).
Haider, A. et al. Assessment of patient-centered approaches to collect sexual orientation and gender identity information in the emergency department: the EQUALITY study. JAMA Netw. Open 1, e186506 (2018).
Lapinski, J. et al. Best practices in transgender health: a clinician’s guide. Prim. Care 45, 687–703 (2018).
Deutsch, M. B. et al. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J. Am. Med. Inf. Assoc. 20, 700–703 (2013).
Wall, C. S. J., Patev, A. J. & Benotsch, E. G. Trans broken arm syndrome: a mixed-methods exploration of gender-related medical misattribution and invasive questioning. Soc. Sci. Med. 320, 115748 (2023).
NCSH. Sexual health and your patients: a provider’s guide. National Coalition for Sexual Health https://nationalcoalitionforsexualhealth.org/tools/for-healthcare-providers/sexual-health-and-your-patients-a-providers-guide (2023).
Bermea, A. M., Slakoff, D. C. & Goldberg, A. E. Intimate partner violence in the LGBTQ+ community: experiences, outcomes, and implications for primary care. Prim. Care 48, 329–337 (2021).
Canibaño, B. et al. Pregnancy-related issues in women with multiple sclerosis: an evidence-based review with practical recommendations. J. Drug Assess. 9, 20–36 (2020).
Cheng, P. J., Pastuszak, A. W., Myers, J. B., Goodwin, I. A. & Hotaling, J. M. Fertility concerns of the transgender patient. Transl. Androl. Urol. 8, 209–218 (2019).
Afanasjeva, J., Gabay, M., Poznanski, T. & Kerns, S. Transdermal patch administration and magnetic resonance imaging (MRI)—2020. Hosp. Pharm. 57, 117–120 (2022).
Braybrook, D. et al. Communication about sexual orientation and gender between clinicians, LGBT+ people facing serious illness and their significant others: a qualitative interview study of experiences, preferences and recommendations. BMJ Qual. Saf. 32, 109–120 (2022).
Candrian, C. & Cloyes, K. G. “She’s dying and I can’t say we’re married?”: end-of-life care for LGBT older adults. Gerontologist 61, 1197–1201 (2020).
Reich, A. J. et al. Advance care planning experiences among sexual and gender minority people. JAMA Netw. Open 5, e2222993 (2022).
Kronk, C. A. et al. Transgender data collection in the electronic health record: current concepts and issues. J. Am. Med. Inform. Assoc. 29, 271–284 (2022).
Human Rights Campaign Foundation. Healthcare equality index 2022. HRC Digital Reports https://reports.hrc.org/hei-2022 (2023).
Rosenwohl-Mack, A. et al. A national study on the physical and mental health of intersex adults in the U.S. PLoS ONE 15, e0240088 (2020).
Holzer, J. K., Ellis, L. & Merritt, M. W. Why we need community engagement in medical research. J. Investig. Med. 62, 851–855 (2014).
HIV drug interactions. University of Liverpool www.hiv-druginteractions.org/interactions/87149 (2023).
Fariba, K. A. & Saadabadi, A. Topiramate. In StatPearls www.ncbi.nlm.nih.gov/books/NBK554530/ (StatPearls Publishing, 2023).
Author information
Authors and Affiliations
Contributions
S.G.V. and J.A. researched data for the article. All authors contributed substantially to discussion of the content. S.G.V. and J.A. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks Z L’Erario, Cole Harrington and Atlaf Saadi for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
NIH PhenX Toolkit: https://www.phenxtoolkit.org/collections/view/6
The Human Rights Campaign Foundations’ Healthcare Equality Index (HEI): https://www.thehrcfoundation.org/professional-resources/hei-scoring-criteria
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Volpe, S.G., Ahmad, J., Patel, R.A. et al. Neurological care for LGBT+ people. Nat Rev Neurol (2024). https://doi.org/10.1038/s41582-024-00944-0
Accepted:
Published:
DOI: https://doi.org/10.1038/s41582-024-00944-0