Abstract
Disease staging, whereby the spatial extent and load of brain pathology are used to estimate the severity of Alzheimer disease (AD), is pivotal to the gold-standard neuropathological diagnosis of AD. Current in vivo diagnostic frameworks for AD are based on abnormal concentrations of amyloid-β and tau in the cerebrospinal fluid or on PET scans, and breakthroughs in molecular imaging have opened up the possibility of in vivo staging of AD. Focusing on the key principles of disease staging shared across several areas of medicine, this Review highlights the potential for in vivo staging of AD to transform our understanding of preclinical AD, refine enrolment criteria for trials of disease-modifying therapies and aid clinical decision-making in the era of anti-amyloid therapeutics. We provide a state-of-the-art review of recent biomarker-based AD staging systems and highlight their contributions to the understanding of the natural history of AD. Furthermore, we outline hypothetical frameworks to stage AD severity using more accessible fluid biomarkers. In addition, by applying amyloid PET-based staging to recently published anti-amyloid therapeutic trials, we highlight how biomarker-based disease staging frameworks could illustrate the numerous pathological changes that have already taken place in individuals with mildly symptomatic AD. Finally, we discuss challenges related to the validation and standardization of disease staging and provide a forward-looking perspective on potential clinical applications.
Key points
-
Disease staging systems are used across medicine to measure disease severity, estimate patient prognosis, determine eligibility for clinical trials and guide clinical care.
-
Staging systems provide a model of the natural history of a disease as well as a framework to validate new biomarkers and test new interventions.
-
Alzheimer disease (AD) has a long preclinical phase in which multiple biological changes are observable in the absence of symptoms; biomarker-based staging systems are well suited to detect and monitor these changes over the natural history of AD.
-
Biomarker-based staging using the topography of PET ligand uptake provides information about AD severity and aids prediction of clinical outcomes.
-
Recent work has highlighted the potential of fluid biomarker panels for the staging of AD and the development of plasma biomarker panels will substantially increase the accessibility of biomarker-based AD staging.
-
Biomarker-based AD staging might help to guide clinical decision-making; for example, evidence suggests that individuals with lower levels of tau tracer uptake on PET respond better to anti-amyloid monoclonal antibody therapy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Nichols, E. et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 88–106 (2019).
Jack, C. R. et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 14, 535–562 (2018).
Hyman, B. T. et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement. 8, 1–13 (2012).
McKhann, G. et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging- Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7, 263–269 (2011).
Beach, T. G., Monsell, S. E., Phillips, L. E. & Kukull, W. Accuracy of the clinical diagnosis of Alzheimer disease at National Institute on Aging Alzheimer Disease Centers, 2005-2010. J. Neuropathol. Exp. Neurol. 71, 266–273 (2012).
Therriault, J. et al. Frequency of biologically defined AD in relation to age, sex, APOEε4, and cognitive impairment. Neurology 96, e975–e985 (2021).
Jack, C. R. et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 12, 207–216 (2013).
Bateman, R. J. et al. Clinical and biomarker changes in dominantly inherited Alzheimer’s disease. N. Engl. J. Med. 367, 795–804 (2012).
Villemagne, V. L. et al. Amyloid-β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol. 12, 357–367 (2013).
Krishnadas, N. et al. Rates of regional tau accumulation in ageing and across the Alzheimer’s disease continuum: an AIBL 18F-MK6240 PET study. eBioMedicine 88, 104450 (2023).
Gonnella, J. S., Hornbrook, M. C. & Louis, D. Z. Staging of disease: a case-mix measurement. JAMA 251, 637–644 (1984).
Amin, M. B. et al. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 67, 93–99 (2017).
Sims, J. R. et al. Donanemab in early symptomatic Alzheimer disease the TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA 330, 512–527 (2023).
Gauthier, S., Webster, C., Servaes, S., Morais, J. & Rosa‐Neto, P. World Alzheimer Report. Alzheimer’s Disease International https://www.alzint.org/u/World-Alzheimer-Report-2022.pdf (2022).
Livingston, G. et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396, 413–446 (2020).
Reisberg, B., Ferris, S., De Leon, M. & Crook, T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am. J. Psychiatry 139, 1136–1139 (1982).
FDA. Early Alzheimer’s Disease: Developing Drugs for Treatment; Draft Guidance for Industry. FDA https://www.fda.gov/media/110903/download (2018).
Morris, J. C. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 43, 2412–2414 (1993).
Petersen, R. C. Mild cognitive impairment as a diagnostic entity. J. Intern. Med. 256, 183–194 (2004).
Petersen, R. C. et al. NIA-AA Alzheimer’s disease framework: clinical characterization of stages. Ann. Neurol. 89, 1145–1156 (2021).
Schneider, J. A., Arvanitakis, Z., Bang, W. & Bennett, D. A. Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology 69, 2197–2204 (2007).
Montine, T. J. et al. National Institute on Aging–Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol. 123, 1–11 (2012).
Thal, D. R., Rüb, U., Orantes, M. & Braak, H. Phases of AB-deposition in the human brain and its relevance for the development of AD. Neurology 58, 1791–1800 (2002).
Braak, H., Alafuzoff, I., Arzberger, T., Kretzschmar, H. & Tredici, K. Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol. 112, 389–404 (2006).
Braak, H. & Braak, E. Staging of Alzheimer’s disease-related neurofibrillary changes. Neurobiol. Aging 16, 271–278 (1995).
Mirra, S. S. et al. The consortium to establish a registry for Alzheimer’s disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 41, 479–486 (1991).
Montine, T. J. et al. Multisite assessment of NIA-AA guidelines for the neuropathologic evaluation of Alzheimer’s disease. Alzheimers Dement. 12, 164–169 (2016).
Jansen, W. J. et al. Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA 313, 1924–1938 (2015).
Jack, C. R. et al. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology 87, 539–547 (2016).
Knopman, D. S., Petersen, R. C. & Jack, C. R. A brief history of “Alzheimer disease”: multiple meanings separated by a common name. Neurology 92, 1053–1059 (2019).
Schmitt, F. A. et al. "Preclinical” AD revisited: neuropathology of cognitively normal older adults. Neurology 55, 370–376 (2000).
Knopman, D. S. et al. Neuropathology of cognitively normal elderly. J. Neuropathol. Exp. Neurol. 62, 1087–1095 (2003).
Petersen, R. C. et al. Neuropathologic features of amnestic mild cognitive impairment. Arch. Neurol. 63, 655–672 (2006).
Schneider, J. A., Arvanitakis, Z., Leurgans, S. E. & Bennett, D. A. The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann. Neurol. 66, 200–208 (2009).
Gordon, B. A. et al. Tau PET in autosomal dominant Alzheimer’s disease: relationship with cognition, dementia and other biomarkers. Brain 142, 1063–1076 (2019).
Jansen, W. J. et al. Prevalence estimates of amyloid abnormality across the Alzheimer disease clinical spectrum. JAMA Neurol. 79, 228–243 (2022).
Jack, C. R. et al. Prevalence of biologically vs clinically defined Alzheimer spectrum entities using the National Institute on Aging-Alzheimer’s Association Research Framework. JAMA Neurol. 76, 1174–1183 (2019).
Jack, C. R. et al. Age-specific and sex-specific prevalence of cerebral β-amyloidosis, tauopathy, and neurodegeneration in cognitively unimpaired individuals aged 50–95 years: a cross-sectional study. Lancet Neurol. 16, 435–444 (2017).
McDade, E. et al. Longitudinal cognitive and biomarker changes in dominantly inherited Alzheimer disease. Neurology 91, E1295–E1306 (2018).
Liang, C. S. et al. Mortality rates in Alzheimer’s disease and non-Alzheimer’s dementias: a systematic review and meta-analysis. Lancet Healthy Longev. 2, e479–e488 (2021).
Morris, J. C. et al. Autosomal dominant and sporadic late onset Alzheimer’s disease share a common in vivo pathophysiology. Brain 145, 3594–3607 (2022).
Sperling, R. A. et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7, 280–292 (2011).
Ossenkoppele, R. et al. Amyloid and tau PET-positive cognitively unimpaired individuals are at high risk for future cognitive decline. Nat. Med. 28, 2381–2387 (2022).
Strikwerda-Brown, C. et al. Association of elevated amyloid and tau positron emission tomography signal with near-term development of Alzheimer disease symptoms in older adults without cognitive impairment. JAMA Neurol. 79, 975–985 (2022).
Bergeron, D. et al. Prevalence of amyloid-β pathology in distinct variants of primary progressive aphasia. Ann. Neurol. 84, 729–740 (2018).
Quadalti, C. et al. Clinical effects of Lewy body pathology in cognitively impaired individuals. Nat. Med. 29, 1964–1970 (2023).
Palmqvist, S. et al. Cognitive effects of Lewy body pathology in clinically unimpaired individuals. Nat. Med. 29, 1971–1978 (2023).
Hansson, O. Biomarkers for neurodegenerative diseases. Nat. Med. 27, 954–963 (2021).
Horie, K. et al. CSF tau microtubule-binding region identifies pathological changes in primary tauopathies. Nat. Med. 28, 2547–2554 (2022).
Ashton, N. J. et al. An update on blood-based biomarkers for non-Alzheimer neurodegenerative disorders. Nat. Rev. Neurol. 16, 265–284 (2020).
Scheltens, P. et al. Alzheimer’s disease. Lancet 397, 1577–1590 (2021).
Jones, D. et al. A computational model of neurodegeneration in Alzheimer’s disease. Nat. Commun. 13, 1643 (2022).
De Picker, L. J. et al. TSPO PET brain inflammation imaging: a transdiagnostic systematic review and meta-analysis of 156 case-control studies. Brain Behav. Immun. 113, 415–431 (2023).
Mattsson, N., Palmqvist, S., Stomrud, E., Vogel, J. & Hansson, O. Staging β-amyloid pathology with amyloid positron emission tomography. JAMA Neurol. 76, 1319–1329 (2019).
Palmqvist, S. et al. Earliest accumulation of β-amyloid occurs within the default-mode network and concurrently affects brain connectivity. Nat. Commun. 8, 1214–1226 (2017).
Fantoni, E., Collij, L., Alves, I. L., Buckley, C. & Farrar, G. The spatial-temporal ordering of amyloid pathology and opportunities for PET imaging. J. Nucl. Med. 61, 166–171 (2020).
Grothe, M. J. et al. In vivo staging of regional amyloid deposition. Neurology 89, 2031–2038 (2017).
Jelistratova, I., Teipel, S. J. & Grothe, M. J. Longitudinal validity of PET-based staging of regional amyloid deposition. Hum. Brain Mapp. 41, 4219–4231 (2020).
Levin, F. et al. In vivo staging of regional amyloid progression in healthy middle-aged to older people at risk of Alzheimer’s disease. Alzheimers Res. Ther. 13, 178 (2021).
Collij, L. E. et al. Multitracer model for staging cortical amyloid deposition using PET imaging. Neurology 95, e1538–e1553 (2020).
Ozlen, H. et al. Spatial extent of amyloid-β levels and associations with tau-PET and cognition. JAMA Neurol. 79, 1025–1035 (2022).
Collij, L. E. et al. Visual assessment of [18F]flutemetamol PET images can detect early amyloid pathology and grade its extent. Eur. J. Nucl. Med. Mol. Imaging 48, 2169–2182 (2021).
Therriault, J. et al. Biomarker modeling of Alzheimer’s disease using PET-based Braak staging. Nat. Aging 2, 526–535 (2022).
Jack, C. R. et al. Brain β-amyloid load approaches a plateau. Neurology 80, 890–896 (2013).
Klunk, W. E. et al. The Centiloid project: standardizing quantitative amyloid plaque estimation by PET. Alzheimers Dement. 11, 1–15.e1-4 (2015).
Pemberton, H. G. et al. Quantification of amyloid PET for future clinical use: a state-of-the-art review. Eur. J. Nucl. Med. Mol. Imaging 49, 3508–3528 (2022).
La Joie, R. et al. Multisite study of the relationships between antemortem [11C]PIB-PET Centiloid values and postmortem measures of Alzheimer’s disease neuropathology. Alzheimers Dement. 15, 205–216 (2019).
Jack, C. R. et al. Defining imaging biomarker cut points for brain aging and Alzheimer’s disease. Alzheimers Dement. 13, 205–216 (2017).
Therriault, J. et al. Amyloid beta plaque accumulation with longitudinal [18F]AZD4694 PET. Alzheimers Dement. 15, e12391 (2023).
Schöll, M. et al. PET imaging of tau deposition in the aging human brain. Neuron 89, 971–982 (2016).
Johnson, K. A. et al. Tau positron emission tomographic imaging in aging and early Alzheimer disease. Ann. Neurol. 79, 110–119 (2016).
Lowe, V. J. et al. Widespread brain tau and its association with ageing, Braak stage and Alzheimer’s dementia. Brain 141, 271–287 (2018).
Macedo, A. C. et al. The use of tau PET to stage Alzheimer disease according to the Braak staging framework. J. Nucl. Med. 64, 1171–1178 (2023).
St-Onge, F. et al. Tau accumulation and its spatial progression across the Alzheimer’s disease spectrum. Preprint at medRxiv https://doi.org/10.1101/2023.06.02.23290880 (2023).
Pascoal, T. A. et al. 18F-MK-6240 PET for early and late detection of neurofibrillary tangles. Brain 143, 2818–2830 (2020).
Costoya-Sánchez, A. et al. Increased medial temporal tau positron emission tomography uptake in the absence of amyloid-β positivity. JAMA Neurol. 80, 1051–1061 (2023).
Crary, J. F. et al. Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol. 128, 755–766 (2014).
Wuestefeld, A. et al. Age-related and amyloid-beta-independent tau deposition and its downstream effects. Brain 146, 3192–3205 (2023).
Therriault, J. & Grothe, M. J. Towards in vivo PET imaging of primary age-related tauopathy. Brain 146, 3106–3109 (2023).
Jagust, W. Imaging the evolution and pathophysiology of Alzheimer disease. Nat. Rev. Neurosci. 19, 687–700 (2018).
Riley, K. P., Snowdon, D. A. & Markesbery, W. R. Alzheimer’s neurofibrillary pathology and the spectrum of cognitive function: findings from the Nun Study. Ann. Neurol. 51, 567–577 (2002).
Whitwell, J. L. et al. MRI correlates of neurofibrillary tangle pathology at autopsy: a voxel-based morphometry study. Neurology 71, 743–749 (2008).
Macedo, A. C. et al. Clinical correlates of the PET-based Braak staging framework in Alzheimer’s disease. J. Prev. Alzheimers Dis. https://doi.org/10.14283/jpad.2024.15 (2024).
Smith, R. et al. Tau-PET is superior to phospho-tau when predicting cognitive decline in symptomatic AD patients. Alzheimers Dement. 19, 2497–2507 (2023).
Ossenkoppele, R. et al. Accuracy of tau positron emission tomography as a prognostic marker in preclinical and prodromal Alzheimer disease. JAMA Neurol. 78, 961–971 (2021).
Montoliu-Gaya, L. et al. Mass spectrometric simultaneous quantification of tau species in plasma shows differential associations with amyloid and tau pathologies. Nat. Aging 3, 661–669 (2023).
Mintun, M. A. et al. Donanemab in early Alzheimer’s disease. N. Engl. J. Med. 384, 1691–1704 (2021).
Therriault, J. et al. Staging of Alzheimer’s disease: past, present, and future perspectives. Trends Mol. Med. 28, 726–741 (2022).
Whittington, A. & Gunn, R. N. TauIQ: a canonical image based algorithm to quantify tau PET scans. J. Nucl. Med. 62, 1292–1300 (2021).
Jovalekic, A. et al. Validation of quantitative assessment of florbetaben PET scans as an adjunct to the visual assessment across 15 software methods. Eur. J. Nucl. Med. Mol. Imaging 50, 3276–3289 (2023).
Gebre, R. K. et al. Advancing Tau-PET quantification in Alzheimer’s disease with machine learning: introducing THETA, a novel tau summary measure. Preprint at Res. Sq. https://doi.org/10.21203/rs.3.rs-3290598/v1 (2023).
Brand, A. L. et al. The performance of plasma amyloid beta measurements in identifying amyloid plaques in Alzheimer’s disease: a literature review. Alzheimers Res. Ther. 14, 195 (2022).
Patterson, B. W. et al. Age and amyloid effects on human central nervous system amyloid-beta kinetics. Ann. Neurol. 78, 439–453 (2015).
Palmqvist, S., Mattsson, N. & Hansson, O. Cerebrospinal fluid analysis detects cerebral amyloid-β accumulation earlier than positron emission tomography. Brain 139, 1226–1236 (2016).
Schindler, S. E. et al. High-precision plasma β-amyloid 42/40 predicts current and future brain amyloidosis. Neurology 93, E1647–E1659 (2019).
Barthélemy, N. R. et al. A soluble phosphorylated tau signature links tau, amyloid and the evolution of stages of dominantly inherited Alzheimer’s disease. Nat. Med. 26, 398–407 (2020).
Milà-Alomà, M. et al. Plasma p-tau231 and p-tau217 as state markers of amyloid-β pathology in preclinical Alzheimer’s disease. Nat. Med. 28, 1797–1801 (2022).
Ashton, N. J. et al. Differential roles of Aβ42/40, p-tau231 and p-tau217 for Alzheimer’s trial selection and disease monitoring. Nat. Med. 28, 2555–2562 (2022).
Therriault, J. et al. Association of phosphorylated tau biomarkers with amyloid positron emission tomography vs tau positron emission tomography. JAMA Neurol. 80, 188–199 (2023).
Salvadó, G. et al. Specific associations between plasma biomarkers and postmortem amyloid plaque and tau tangle loads. EMBO Mol. Med. 46, e17123 (2023).
Ashton, N. J. et al. Cerebrospinal fluid p-tau231 as an early indicator of emerging pathology in Alzheimer’s disease. eBioMedicine 76, 103836 (2022).
Murray, M. E. et al. Global neuropathologic severity of Alzheimer’s disease and locus coeruleus vulnerability influences plasma phosphorylated tau levels. Mol. Neurodegener. 17, 85 (2022).
Mattsson‐Carlgren, N. et al. Soluble P‐tau217 reflects amyloid and tau pathology and mediates the association of amyloid with tau. EMBO Mol. Med. 13, e14022 (2021).
Palmqvist, S. et al. Discriminative accuracy of plasma phospho-tau217 for Alzheimer disease vs other neurodegenerative disorders. JAMA 324, 772–781 (2020).
Janelidze, S. et al. Associations of plasma phospho-tau217 levels with tau positron emission tomography in early Alzheimer disease. JAMA Neurol. 78, 149–156 (2021).
Suárez‐Calvet, M. et al. Novel tau biomarkers phosphorylated at T181, T217 or T231 rise in the initial stages of the preclinical Alzheimer’s continuum when only subtle changes in Aβ pathology are detected. EMBO Mol. Med. 12, e12921 (2020).
Jonaitis, E. M. et al. Plasma phosphorylated tau 217 in preclinical Alzheimer’s disease. Brain Commun. 5, fcad057 (2023).
Mielke, M. M. et al. Comparison of plasma phosphorylated tau species with amyloid and tau positron emission tomography, neurodegeneration, vascular pathology, and cognitive outcomes. JAMA Neurol. 78, 1108–1117 (2021).
Ossenkoppele, R. et al. Tau PET correlates with different Alzheimer’s disease‐related features compared to CSF and plasma p‐tau biomarkers. EMBO Mol. Med. 13, e14398 (2021).
Therriault, J. et al. Comparison of immunoassay- with mass spectrometry-derived p-tau quantification for the detection of Alzheimer’s disease pathology. Mol. Neurodegener. 19, 2 (2024).
Barthélemy, N. R. et al. CSF tau phosphorylation occupancies at T217 and T205 represent improved biomarkers of amyloid and tau pathology in Alzheimer’s disease. Nat. Aging 3, 391–401 (2023).
Salvadó, G., Horie, K., Barthélemy, N. R. & Vogel, J. W. Novel CSF tau biomarkers can be used for disease staging of sporadic Alzheimer’s disease. Nat. Aging (in the press).
Lantero-Rodríguez, J. et al. CSF p-tau205: a biomarker of tau pathology in Alzheimer’s disease. Acta Neuropathol. 147, 12 (2024).
Horie, K., Barthélemy, N. R., Sato, C. & Bateman, R. J. CSF tau microtubule binding region identifies tau tangle and clinical stages of Alzheimer’s disease. Brain 144, 515–527 (2021).
Horie, K. et al. CSF MTBR-tau243 is a specific biomarker of tau pathology in Alzheimer’s disease. Nat. Med. 29, 1954–1963 (2023).
Simrén, J. et al. CSF tau368/total-tau ratio reflects cognitive performance and neocortical tau better compared to p-tau181 and p-tau217 in cognitively impaired individuals. Alzheimers Res. Ther. 14, 192 (2022).
Blennow, K. et al. Cerebrospinal fluid tau fragment correlates with tau PET: a candidate biomarker for tangle pathology. Brain 143, 650–660 (2020).
Lantero‐Rodriguez, J. et al. P‐tau235: a novel biomarker for staging preclinical Alzheimer’s disease. EMBO Mol. Med. 13, e15098 (2021).
Lantero-Rodriguez, J. et al. Plasma and CSF concentrations of N-terminal tau fragments associate with in vivo neurofibrillary tangle burden. Alzheimers Dement. 19, 5343–5354 (2023).
Snellman, A. et al. N-Terminal and mid-region tau fragments as fluid biomarkers in neurological diseases. Brain 145, 2834–2848 (2022).
Chhatwal, J. P. et al. Plasma N-terminal tau fragment levels predict future cognitive decline and neurodegeneration in healthy elderly individuals. Nat. Commun. 11, 6024 (2020).
Mengel, D. et al. Plasma NT1 Tau is a specific and early marker of Alzheimer’s disease. Ann. Neurol. 88, 878–892 (2020).
Mattsson-Carlgren, N. et al. Aβ deposition is associated with increases in soluble and phosphorylated tau that precede a positive Tau PET in Alzheimer’s disease. Sci. Adv. 6, eaaz2387 (2020).
Hanger, D. P. et al. Novel phosphorylation sites in tau from Alzheimer brain support a role for casein kinase 1 in disease pathogenesis. J. Biol. Chem. 282, 23645–23654 (2007).
Augustinack, J. C., Schneider, A., Mandelkow, E. M. & Hyman, B. T. Specific tau phosphorylation sites correlate with severity of neuronal cytopathology in Alzheimer’s disease. Acta Neuropathol. 103, 26–35 (2002).
Jack, C. R. et al. Predicting amyloid PET and tau PET stages with plasma biomarkers. Brain 146, 2029–2044 (2023).
Leuzy, A. et al. Comparing the clinical utility and diagnostic performance of CSF p-tau181, p-tau217, and p-tau231 assays. Neurology 97, e1681–e1694 (2021).
Janelidze, S. et al. Head-to-head comparison of 8 plasma amyloid-β 42/40 assays in Alzheimer disease. JAMA Neurol. 78, 1375–1382 (2021).
Janelidze, S. et al. Head-to-head comparison of 10 plasma phospho-tau assays in prodromal Alzheimer’s disease. Brain 146, 1592–1601 (2023).
Ashton, N. J. et al. Plasma and CSF biomarkers in a memory clinic: head-to-head comparison of phosphorylated tau immunoassays. Alzheimers Dement. 19, 1913–1924 (2023).
Pichet Binette, A. et al. Confounding factors of Alzheimer’s disease plasma biomarkers and their impact on clinical performance. Alzheimers Dement. 19, 1403–1414 (2023).
Syrjanen, J. A. et al. Associations of amyloid and neurodegeneration plasma biomarkers with comorbidities. Alzheimers Dement. 18, 1128–1140 (2022).
Mielke, M. M. et al. Performance of plasma phosphorylated tau 181 and 217 in the community. Nat. Med. 28, 1398–1405 (2022).
Van Westen, D. et al. Cerebral white matter lesions — associations with Aβ isoforms and amyloid PET. Sci. Rep. 6, 20709 (2016).
Janelidze, S., Barthélemy, N. R., He, Y., Bateman, R. J. & Hansson, O. Mitigating the associations of kidney dysfunction with blood biomarkers of Alzheimer disease by using phosphorylated tau to total tau ratios. JAMA Neurol. 80, 516–522 (2023).
Schindler, S. E. Fluid biomarkers in dementia diagnosis. Contin. Lifelong Learn. Neurol. 28, 822–833 (2022).
Verberk, I. M. W. et al. Characterization of pre-analytical sample handling effects on a panel of Alzheimer’s disease-related blood-based biomarkers: results from the Standardization of Alzheimer’s Blood Biomarkers (SABB) working group. Alzheimers Dement. 18, 1484–1497 (2022).
Hansson, O. et al. Pre-analytical protocol for measuring Alzheimer’s disease biomarkers in fresh CSF. Alzheimers Dement. 12, e12137 (2020).
Therriault, J. et al. Equivalence of plasma p-tau217 with cerebrospinal fluid in the diagnosis of Alzheimer’s disease. Alzheimers Dement. 19, 4967–4977 (2023).
Karikari, T. K. et al. Blood phospho-tau in Alzheimer disease: analysis, interpretation, and clinical utility. Nat. Rev. Neurol. 18, 400–418 (2022).
Ashton, N. J. et al. Diagnostic accuracy of a plasma phosphorylated tau 217 immunoassay for Alzheimer disease pathology. JAMA Neurol. e235319, https://doi.org/10.1001/jamaneurol.2023.5319 (2024).
Mundada, N. S. et al. Head-to-head comparison between plasma p-tau217 and flortaucipir-PET in amyloid-positive patients with cognitive impairment. Alzheimers Res. Ther. 15, 157 (2023).
Coomans, E. M. et al. A head-to-head comparison between plasma ptau181 and tau PET along the Alzheimer’s disease continuum. J. Nucl. Med. 64, 437–443 (2023).
McKhann, G., Drachman, D., Folstein, M. & Katzman, R. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34, 939–944 (1984).
Alladi, S. et al. Focal cortical presentations of Alzheimer’s disease. Brain 130, 2636–2645 (2007).
Graff-Radford, J. et al. New insights into atypical Alzheimer’s disease in the era of biomarkers. Lancet Neurol. 20, 222–234 (2021).
Murray, M. E. et al. Neuropathologically defined subtypes of Alzheimer’s disease with distinct clinical characteristics: a retrospective study. Lancet Neurol. 10, 785–796 (2011).
Ossenkoppele, R. et al. Tau PET patterns mirror clinical and neuroanatomical variability in Alzheimer’s disease. Brain 139, 1551–1567 (2016).
Xia, C. et al. Association of in vivo [18F]AV-1451 tau PET imaging results with cortical atrophy and symptoms in typical and atypical Alzheimer disease. JAMA Neurol. 74, 427–436 (2017).
Townley, R. A. et al. Progressive dysexecutive syndrome due to Alzheimer’s disease: a description of 55 cases and comparison to other phenotypes. Brain Commun. 2, fcaa068 (2020).
Therriault, J. et al. Topographical distribution of amyloid-β, tau and atrophy in behavioral/dysexecutive AD patients. Neurology 96, e81–e92 (2020).
Phillips, J. S. et al. Tau PET imaging predicts cognition in atypical variants of Alzheimer’s disease. Hum. Brain Mapp. 39, 691–708 (2018).
Therriault, J. et al. Intrinsic connectivity of the human brain provides scaffold for tau aggregation in clinical variants of Alzheimer’s disease. Sci. Transl. Med. 14, eabc8693 (2022).
Corriveau-Lecavalier, N. et al. Deciphering the clinico-radiological heterogeneity of dysexecutive Alzheimer’s disease. Cereb. Cortex 33, 7026–7043 (2023).
La Joie, R. et al. Association of APOE4 and clinical variability in Alzheimer disease with the pattern of tau- and amyloid-PET. Neurology 96, e650–e661 (2021).
Petersen, C. et al. Alzheimer’s disease clinical variants show distinct regional patterns of neurofibrillary tangle accumulation. Acta Neuropathol. 138, 597–612 (2019).
Vogel, J. W. et al. Four distinct trajectories of tau deposition identified in Alzheimer’s disease. Nat. Med. 27, 871–881 (2021).
Young, C. B. et al. Divergent cortical tau positron emission tomography patterns among patients with preclinical Alzheimer disease. JAMA Neurol. 79, 592–603 (2022).
Tijms, B. M. et al. Pathophysiological subtypes of Alzheimer’s disease based on cerebrospinal fluid proteomics. Brain 143, 3776–3792 (2020).
van Dyck, C. H. et al. Lecanemab in early Alzheimer’s disease. N. Engl. J. Med. 388, 9–21 (2023).
Tian Hui Kwan, A., Arfaie, S., Therriault, J., Rosa-Neto, P. & Gauthier, S. Lessons learnt from the second generation of anti-amyloid monoclonal antibodies clinical trials. Dement. Geriatr. Cogn. Disord. 3, 334–348 (2020).
Budd Haeberlein, S. et al. Two randomized phase 3 studies of aducanumab in early Alzheimer’s disease. J. Prev. Alzheimers Dis. 9, 197–210 (2022).
Therriault, J. et al. Association of apolipoprotein e ϵ4 with medial temporal tau independent of amyloid-β. JAMA Neurol. 77, 470–479 (2020).
Plowey, E. D. et al. Alzheimer disease neuropathology in a patient previously treated with aducanumab. Acta Neuropathol. 144, 143–153 (2022).
Rafii, M. S. et al. The AHEAD 3-45 study: design of a prevention trial for Alzheimer’s disease. Alzheimers Dement. 19, 1227–1233 (2023).
Bateman, R. J. et al. The DIAN-TU Next Generation Alzheimer’s prevention trial: adaptive design and disease progression model. Alzheimers Dement. 13, 8–19 (2017).
Sperling, R. et al. Trial of solanezumab in preclinical Alzheimer’s disease. N. Engl. J. Med. 389, 1096–1107 (2023).
Leuzy, A. et al. Biomarker-based prediction of longitudinal tau positron emission tomography in Alzheimer disease. JAMA Neurol. 79, 149–158 (2022).
Hanseeuw, B. J. et al. Association of amyloid and tau with cognition in preclinical Alzheimer disease: a longitudinal study. JAMA Neurol. 76, 915–924 (2019).
Kwan, A. T. H. et al. Medial temporal tau predicts memory decline in cognitively unimpaired elderly. Brain Commun. 5, fcac325 (2023).
Groot, C. et al. Phospho-tau with subthreshold tau-PET predicts increased tau accumulation rates in amyloid-positive individuals. Brain 146, 1580–1591 (2023).
Therriault, J. et al. Association of plasma P-tau181 with memory decline in non-demented adults. Brain Commun. 3, fcab136 (2021).
Palmqvist, S. et al. Prediction of future Alzheimer’s disease dementia using plasma phospho-tau combined with other accessible measures. Nat. Med. 27, 1034–1042 (2021).
Mattsson-Carlgren, N. et al. Prediction of longitudinal cognitive decline in preclinical Alzheimer disease using plasma biomarkers. JAMA Neurol. 80, 360–369 (2023).
Moher, D., Wells, G. A. & Dulberg, C. S. Statistical power, sample size, and their reporting in randomized controlled trials. JAMA 272, 122–124 (1994).
Jack, C. R. et al. Longitudinal tau PET in ageing and Alzheimer’s disease. Brain 141, 1517–1528 (2018).
Pascoal, T. A. et al. Longitudinal 18F-MK-6240 tau tangles accumulation follows Braak stages. Brain 144, 3517–3528 (2021).
Harrison, T. M. et al. Longitudinal tau accumulation and atrophy in aging and Alzheimer disease. Ann. Neurol. 85, 229–240 (2019).
Franzmeier, N. et al. Patient-centered connectivity-based prediction of tau pathology spread in Alzheimer’s disease. Sci. Adv. 6, eabd1327 (2020).
Alafuzoff, I. et al. Staging of neurofibrillary pathology in Alzheimer’s disease: a study of the BrainNet Europe consortium. Brain Pathol. 18, 484–496 (2008).
Jack, C. R. et al. Long-term associations between amyloid positron emission tomography, sex, apolipoprotein E and incident dementia and mortality among individuals without dementia: hazard ratios and absolute risk. Brain Commun. 4, fcac017 (2022).
Ourry, V. et al. How do modifiable risk factors affect Alzheimer’s disease pathology or mitigate its effect on clinical symptom expression? Biol. Psychiatry https://doi.org/10.1016/j.biopsych.2023.09.003 (2023).
Bocancea, D. I. et al. Determinants of cognitive and brain resilience to tau pathology: a longitudinal analysis. Brain 146, 3719–3734 (2023).
Ossenkoppele, R. et al. Assessment of demographic, genetic, and imaging variables associated with brain resilience and cognitive resilience to pathological tau in patients with Alzheimer disease. JAMA Neurol. 77, 632–642 (2020).
Gobom, J. et al. Antibody-free measurement of cerebrospinal fluid tau phosphorylation across the Alzheimer’s disease continuum. Mol. Neurodegener. 17, 81 (2022).
Schindler, S. E. et al. Effect of race on prediction of brain amyloidosis by plasma Aβ42/Aβ40, phosphorylated tau, and neurofilament light. Neurology 99, E245–E257 (2022).
Schindler, S. E. & Karikari, T. K. Comorbidities confound Alzheimer’s blood tests. Nat. Med. 28, 1349–1351 (2022).
Acknowledgements
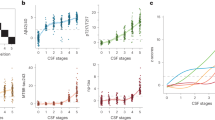
The authors thank Kelsey Caetano-Anolles for support with manuscript review. The TRIAD cohort (data in Fig. 3) is supported by the Weston Brain Institute, Canadian Institutes of Health Research (CIHR; grants MOP-11-51-31 and RFN 152985, 159815 and 162303), Canadian Consortium of Neurodegeneration and Aging (CCNA; MOP-11-51-31 team 1), the Alzheimer’s Association (grants NIRG-12-92090 and NIRP-12-259245), Brain Canada Foundation (CFI Project 34874; 33397), the Fonds de Recherche du Québec — Santé (FRQS; Chercheur Boursier, 2020-VICO-279314) and the Colin J. Adair Charitable Foundation.
Author information
Authors and Affiliations
Contributions
J.T., S.E.S., G.S., A.L.B., N.J.A., T.K.K., J.W.V., R.LJ., H.Z., C.R.J. and P.R.-N. researched the data for the article. J.T., S.E.S., G.S., T.A.P., A.L.B., N.J.A., T.K.K., L.A., I.V., J.W.V., R.LJ., C.T., G.D.R., H.Z., R.J.B., R.S., O.H., C.R.J. and P.R.-N. contributed substantially to discussion of the content. J.T., S.E.S., G.S., A.L.B., N.J.A., T.K.K., J.W.V., R.LJ., O.H., C.R.J. and P.R.-N. wrote the article. J.T., S.E.S., G.S., T.A.P., A.L.B., N.J.A., T.K.K., L.A., M.E.M., I.V., J.W.V., S.G., C.T., G.D.R., H.Z., R.J.B, P.S., K.B., R.S., O.H., C.R.J. and P.R.-N. reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
J.T. has received consultancy fees from the Neurotorium educational platform outside the scope of the present work. L.A. has received grants from the National Institute on Aging, the Alzheimer’s Association, AVID Radiopharmaceuticals, Life Molecular Imaging, and Roche Diagnostics and personal fees from Eli Lilly, Biogen, Two Labs, IQVIA, Genentech, Siemens, Corium, GE Healthcare, Eisai, Roche Diagnostics, Alnylam, the Alzheimer’s Association, and from the FDA outside the submitted work. C.T. reports non-financial support from Quanterix during the conduct of the study, has a patent pending for glial fibrillary acidic protein as a biomarker, serves as an editorial board member of Alzheimer’s Research and Therapy, Medidact Neurologie (Springer), and Neurology: Neuroimmunology & Neuroinflammation, serves as an editor of the Neuromethods book series (Springer), and reports grants from Roche Diagnostics, non-financial support from ADx Neurosciences and Eli Lilly, and compensation from AC Immune, Axon Neurosciences, Biogen, Brainstorm Cell Therapeutics, Celgene, Denali Therapeutics, EIP Pharma, Eisai, PeopleBio, Toyama Pharmaceutical Association and Vivoryon Therapeutics outside the submitted work. G.D.R. has received grants from the American College of Radiology, Avid Radiopharmaceuticals, Life Molecular Imaging (formerly Piramal Imaging) and GE Healthcare during the conduct of the study, personal fees from Alector, Eli Lilly, Merck, and the Johnson & Johnson Data and Safety Monitoring Board and grants from Genentech, the NIH, the Alzheimer’s Association, and Rainwater Charitable Foundation outside the submitted work, and is an Associate Editor for JAMA Neurology. R.J.B. declares research funding from Avid Radiopharmaceuticals, Janssen, Roche/Genentech, Eli Lilly, Eisai, Biogen, AbbVie, Bristol Myers Squibb and Novartis, equity ownership interest in C2N Diagnostics and income from C2N Diagnostics for serving on the scientific advisory board, serves on the Roche gantenerumab steering committee as an unpaid member, has income based on technology (blood plasma assay and methods of diagnosing Alzheimer disease with phosphorylation changes) licensed by Washington University to C2N Diagnostics, and also declares involvement with the Alzheimer’s Association, Duke Margolis Alzheimer’s, BrightFocus Foundation and Tau Consortium Investigators’ Meeting. H.Z. has served on scientific advisory boards and/or as a consultant for Abbvie, Acumen, Alector, Alzinova, ALZPath, Annexon, Apellis, Artery Therapeutics, AZTherapies, Cognito Therapeutics, CogRx, Denali, Eisai, Nervgen, Novo Nordisk, Optoceutics, Passage Bio, Pinteon Therapeutics, Prothena, Red Abbey Labs, reMYND, Roche, Samumed, Siemens Healthineers, Triplet Therapeutics, and Wave, has given lectures in symposia sponsored by Cellectricon, Fujirebio, Alzecure, Biogen and Roche, and is a co-founder of Brain Biomarker Solutions in Gothenburg AB (BBS), which is a part of the GU Ventures Incubator Program (outside the submitted work). P.S. is a full-time employee of EQT Life Sciences (formerly LSP) and Professor Emeritus at Amsterdam University Medical Centers. He has received consultancy fees (paid to the university) from Alzheon, Brainstorm Cell and Green Valley. Within his university affiliation, he was the global Principal Investigator of a phase Ib study for AC Immune, a phase IIb study for FUJI-film/Toyama and a phase II study for UCB. He is past chair of the European Union steering committee of the Vivoryon phase IIb programme and a phase IIb study for Novartis Cardiology, and is currently co-chair of a phase III study for Novo Nordisk. K.B. has served as a consultant and on advisory boards for Acumen, ALZPath, BioArctic, Biogen, Eisai, Julius Clinical, Lilly, Novartis, Ono Pharma, Prothena, Roche Diagnostics and Siemens Healthineers, has served on data monitoring committees for Julius Clinical and Novartis, has given lectures, produced educational materials and participated in educational programmes for Biogen, Eisai and Roche Diagnostics, and is a co-founder of BBS, which is part of the GU Ventures Incubator Program, outside the work presented in this paper. R.S. reports grant support from the NIH, Eli Lilly, the Alzheimer’s Association, GHR Foundation, Fidelity, and Gates Ventures, non-financial support from CogState and Mount Sinai, grants and personal fees from Janssen, and personal fees from AC Immune, Biogen, Neurocentria, Eisai, Roche, Takeda and Novartis. O.H. has acquired research support (for the institution) from ADx, AVID Radiopharmaceuticals, Biogen, Eli Lilly, Eisai, Fujirebio, GE Healthcare, Pfizer and Roche. In the past 2 years, he has received consultancy or speaker fees from AC Immune, Amylyx, Alzpath, BioArctic, Biogen, Cerveau, Eisai, Eli Lilly, Fujirebio, Merck, Novartis, Novo Nordisk, Roche, Sanofi and Siemens. P.R.-N. has served on scientific advisory boards and/or as a consultant for Roche, Novo Nordisk, Eisai and Cerveau Technologies. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks J. Quinn, M. Malpetti and M. Grothe for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Therriault, J., Schindler, S.E., Salvadó, G. et al. Biomarker-based staging of Alzheimer disease: rationale and clinical applications. Nat Rev Neurol 20, 232–244 (2024). https://doi.org/10.1038/s41582-024-00942-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-024-00942-2
This article is cited by
-
Disease staging of Alzheimerâs disease using a CSF-based biomarker model
Nature Aging (2024)