Abstract
Vector-borne diseases are transmitted by haematophagous arthropods (for example, mosquitoes, ticks and sandflies) to humans and wild and domestic animals, with the largest burden on global public health disproportionately affecting people in tropical and subtropical areas. Because vectors are ectothermic, climate and weather alterations (for example, temperature, rainfall and humidity) can affect their reproduction, survival, geographic distribution and, consequently, ability to transmit pathogens. However, the effects of climate change on vector-borne diseases can be multifaceted and complex, sometimes with ambiguous consequences. In this Review, we discuss the potential effects of climate change, weather and other anthropogenic factors, including land use, human mobility and behaviour, as possible contributors to the redistribution of vectors and spread of vector-borne diseases worldwide.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
World Health Organization. Global vector control response 2017–2030. WHO https://www.who.int/publications/i/item/9789241512978 (2017).
Messina, J. P. et al. The current and future global distribution and population at risk of dengue. Nat. Microbiol. 4, 1508–1515 (2019).
Weaver, S. C., Charlier, C., Vasilakis, N. & Lecuit, M. Zika, chikungunya, and other emerging vector-borne viral diseases. Annu. Rev. Med. 69, 395–408 (2018).
The Intergovernmental Panel on Climate Change. Climate change 2022: impacts, adaptation and vulnerability. IPCC Sixth Assessment. IPCC https://www.ipcc.ch/report/ar6/wg2/ (2022).
Armstrong McKay, D. I. et al. Exceeding 1.5 °C global warming could trigger multiple climate tipping points. Science 377, eabn7950 (2022).
Rose, N. H. et al. Dating the origin and spread of specialization on human hosts in. eLife 12, e83524 (2023).
Eigenbrode, S. D., Bosque-Pérez, N. A. & Davis, T. S. Insect-borne plant pathogens and their vectors: ecology, evolution, and complex interactions. Annu. Rev. Entomol. 63, 169–191 (2018).
Singh, B. K. et al. Climate change impacts on plant pathogens, food security and paths forward. Nat. Rev. Microbiol. 21, 640–656 (2023).
Delatte, H., Gimonneau, G., Triboire, A. & Fontenille, D. Influence of temperature on immature development, survival, longevity, fecundity, and gonotrophic cycles of Aedes albopictus, vector of chikungunya and dengue in the Indian Ocean. J. Med. Entomol. 46, 33–41 (2009).
Shocket, M. S. et al. Transmission of West Nile and five other temperate mosquito-borne viruses peaks at temperatures between 23 °C and 26 °C. eLife 9, e58511 (2020).
Shapiro, L. L. M., Whitehead, S. A. & Thomas, M. B. Quantifying the effects of temperature on mosquito and parasite traits that determine the transmission potential of human malaria. PLoS Biol. 15, e2003489 (2017).
Lambrechts, L. et al. Impact of daily temperature fluctuations on dengue virus transmission by Aedes aegypti. Proc. Natl Acad. Sci. USA 108, 7460–7465 (2011).
Ogden, N. H. & Lindsay, L. R. Effects of climate and climate change on vectors and vector-borne diseases: ticks are different. Trends Parasitol. 32, 646–656 (2016).
Ogden, N. H., Ben Beard, C., Ginsberg, H. S. & Tsao, J. I. Possible effects of climate change on ixodid ticks and the pathogens they transmit: predictions and observations. J. Med. Entomol. 58, 1536–1545 (2020).
Wang, B. et al. Historical change of El Niño properties sheds light on future changes of extreme El Niño. Proc. Natl Acad. Sci. USA 116, 22512–22517 (2019).
Lawman, A. E. et al. Unraveling forced responses of extreme El Niño variability over the Holocene. Sci. Adv. 8, eabm4313 (2022).
Wengel, C. et al. Future high-resolution El Niño/Southern Oscillation dynamics. Nat. Clim. Change 11, 758–765 (2021).
Linthicum, K. J. et al. Climate and satellite indicators to forecast Rift Valley fever epidemics in Kenya. Science 285, 397–400 (1999).
Linthicum, K. J., Britch, S. C. & Anyamba, A. Rift valley fever: an emerging mosquito-borne disease. Annu. Rev. Entomol. 61, 395–415 (2016).
Lindsay, S. W., Bødker, R., Malima, R., Msangeni, H. A. & Kisinza, W. Effect of 1997–98 El Niño on highland malaria in Tanzania. Lancet 355, 989–990 (2000).
Boyce, R. M. et al. Dihydroartemisinin–piperaquine chemoprevention and malaria incidence after severe flooding: evaluation of a pragmatic intervention in rural Uganda. Clin. Infect. Dis. 74, 2191–2199 (2022).
Roiz, D., Boussès, P., Simard, F., Paupy, C. & Fontenille, D. Autochthonous chikungunya transmission and extreme climate events in southern France. PLoS Negl. Trop. Dis. 9, e0003854 (2015).
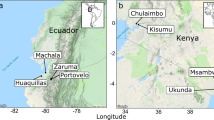
Grossi-Soyster, E. N. et al. Serological and spatial analysis of alphavirus and flavivirus prevalence and risk factors in a rural community in western Kenya. PLoS Negl. Trop. Dis. 11, e0005998 (2017).
Diniz, D. F. A., de Albuquerque, C. M. R., Oliva, L. O., de Melo-Santos, M. A. V. & Ayres, C. F. J. Diapause and quiescence: dormancy mechanisms that contribute to the geographical expansion of mosquitoes and their evolutionary success. Parasit. Vectors 10, 310 (2017).
Barrera, R. et al. Impacts of hurricanes Irma and Maria on. Am. J. Trop. Med. Hyg. 100, 1413–1420 (2019).
Caillouët, K. A. & Robertson, S. L. Temporal and spatial impacts of hurricane damage on West Nile virus transmission and human risk. J. Am. Mosq. Control. Assoc. 36, 106–119 (2020).
Paull, S. H. et al. Drought and immunity determine the intensity of West Nile virus epidemics and climate change impacts. Proc. Biol. Sci. 284, 20162078 (2017).
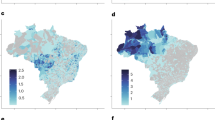
Lowe, R. et al. Combined effects of hydrometeorological hazards and urbanisation on dengue risk in Brazil: a spatiotemporal modelling study. Lancet Planet. Health 5, e209–e219 (2021).
Forero-Becerra, E., Acosta, A., Benavides, E., Martínez-Díaz, H. C. & Hidalgo, M. Amblyomma mixtum free-living stages: inferences on dry and wet seasons use, preference, and niche width in an agroecosystem (Yopal, Casanare, Colombia). PLoS ONE 17, e0245109 (2022).
Weiler, M., Duscher, G. G., Wetscher, M. & Walochnik, J. Tick abundance: a one year study on the impact of flood events along the banks of the River Danube, Austria. Exp. Appl. Acarol. 71, 151–157 (2017).
Stafford, K. C. Survival of immature Ixodes scapularis (Acari: Ixodidae) at different relative humidities. J. Med. Entomol. 31, 310–314 (1994).
Mordecai, E. A. et al. Thermal biology of mosquito-borne disease. Ecol. Lett. 22, 1690–1708 (2019).
Brady, O. J. et al. Vectorial capacity and vector control: reconsidering sensitivity to parameters for malaria elimination. Trans. R. Soc. Trop. Med. Hyg. 110, 107–117 (2016).
Samuel, G. H., Adelman, Z. N. & Myles, K. M. Temperature-dependent effects on the replication and transmission of arthropod-borne viruses in their insect hosts. Curr. Opin. Insect Sci. 16, 108–113 (2016).
Reisen, W. K., Fang, Y. & Martinez, V. M. Effects of temperature on the transmission of west nile virus by Culex tarsalis (Diptera: Culicidae). J. Med. Entomol. 43, 309–317 (2006).
Mullens, B. A., Tabachnick, W. J., Holbrook, F. R. & Thompson, L. H. Effects of temperature on virogenesis of bluetongue virus serotype 11 in Culicoides variipennis sonorensis. Med. Vet. Entomol. 9, 71–76 (1995).
Jacquot, M., Nomikou, K., Palmarini, M., Mertens, P. & Biek, R. Bluetongue virus spread in Europe is a consequence of climatic, landscape and vertebrate host factors as revealed by phylogeographic inference. Proc. Biol. Sci. 284, 20170919 (2017).
Reisen, W. K., Meyer, R. P., Presser, S. B. & Hardy, J. L. Effect of temperature on the transmission of western equine encephalomyelitis and St. Louis encephalitis viruses by Culex tarsalis (Diptera: Culicidae). J. Med. Entomol. 30, 151–160 (1993).
Kramer, L. D., Hardy, J. L. & Presser, S. B. Effect of temperature of extrinsic incubation on the vector competence of Culex tarsalis for western equine encephalomyelitis virus. Am. J. Trop. Med. Hyg. 32, 1130–1139 (1983).
Paaijmans, K. P. et al. Influence of climate on malaria transmission depends on daily temperature variation. Proc. Natl Acad. Sci. USA 107, 15135–15139 (2010).
Liu-Helmersson, J., Stenlund, H., Wilder-Smith, A. & Rocklov, J. Vectorial capacity of Aedes aegypti: effects of temperature and implications for global dengue epidemic potential. PLoS ONE 9, e89783 (2014).
Samuel, G. H., Adelman, Z. N. & Myles, K. M. Antiviral immunity and virus-mediated antagonism in disease vector mosquitoes. Trends Microbiol. 26, 447–461 (2018).
Schnettler, E. et al. Noncoding flavivirus RNA displays RNA interference suppressor activity in insect and mammalian cells. J. Virol. 86, 13486–13500 (2012).
Adelman, Z. N. et al. Cooler temperatures destabilize RNA interference and increase susceptibility of disease vector mosquitoes to viral infection. PLoS Negl. Trop. Dis. 7, e2239 (2013).
Macdonald, G. The Epidemiology and Control of Malaria (Oxford Univ. Press, 1957).
Ribeiro Dos Santos, G. et al. Estimating the effect of the wMel release programme on the incidence of dengue and chikungunya in Rio de Janeiro, Brazil: a spatiotemporal modelling study. Lancet Infect. Dis. 22, 1587–1595 (2022).
Utarini, A. et al. Efficacy of Wolbachia-infected mosquito deployments for the control of dengue. N. Engl. J. Med. 384, 2177–2186 (2021).
Vásquez, V. N., Kueppers, L. M., Rašić, G. & Marshall, J. M. Mel replacement of dengue-competent mosquitoes is robust to near-term change. Nat. Clim. Change 13, 848–855 (2023).
Olmo, R. P. et al. Mosquito vector competence for dengue is modulated by insect-specific viruses. Nat. Microbiol. 8, 135–149 (2023).
Franklinos, L. H. V., Jones, K. E., Redding, D. W. & Abubakar, I. The effect of global change on mosquito-borne disease. Lancet Infect. Dis. 19, e302–e312 (2019).
Messina, J. P. et al. Mapping global environmental suitability for Zika virus. eLife 5, e15272 (2016).
Kraemer, M. U. G. et al. Past and future spread of the arbovirus vectors Aedes aegypti and Aedes albopictus. Nat. Microbiol. 4, 854–863 (2019).
Mordecai, E. A. et al. Detecting the impact of temperature on transmission of Zika, dengue, and chikungunya using mechanistic models. PloS Negl. Trop. Dis. 11, e0005568 (2017).
Iwamura, T., Guzman-Holst, A. & Murray, K. A. Accelerating invasion potential of disease vector Aedes aegypti under climate change. Nat. Commun. 11, 2130 (2020).
Ryan, S. J., Carlson, C. J., Mordecai, E. A. & Johnson, L. R. Global expansion and redistribution of Aedes-borne virus transmission risk with climate change. PLoS Negl. Trop. Dis. 13, e0007213 (2019).
Santos-Vega, M. et al. The neglected role of relative humidity in the interannual variability of urban malaria in Indian cities. Nat. Commun. 13, 533 (2022).
Smith, M. W. et al. Incorporating hydrology into climate suitability models changes projections of malaria transmission in Africa. Nat. Commun. 11, 4353 (2020).
Colón-González, F. J. et al. Projecting the risk of mosquito-borne diseases in a warmer and more populated world: a multi-model, multi-scenario intercomparison modelling study. Lancet Planet. Health 5, e404–e414 (2021).
Tjaden, N. B. et al. Modelling the effects of global climate change on Chikungunya transmission in the 21st century. Sci. Rep. 7, 3813 (2017).
Gaythorpe, K. A., Hamlet, A., Cibrelus, L., Garske, T. & Ferguson, N. M. The effect of climate change on yellow fever disease burden in Africa. eLife 9, e55619 (2020).
Kraemer, M. U. et al. The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. eLife 4, e08347 (2015).
Estrada-Peña, A. & Fernández-Ruiz, N. A retrospective assessment of temperature trends in Northern Europe reveals a deep impact on the life cycle of Ixodes ricinus (Acari: Ixodidae). Pathogens 9, 345 (2020).
Minigan, J. N., Hager, H. A., Peregrine, A. S. & Newman, J. A. Current and potential future distribution of the American dog tick (Dermacentor variabilis, Say) in North America. Ticks Tick. Borne Dis. 9, 354–362 (2018).
Shocket, M. S., Ryan, S. J. & Mordecai, E. A. Temperature explains broad patterns of Ross River virus transmission. eLife 7, e37762 (2018).
Samy, A. M. et al. Climate change influences on the global potential distribution of the mosquito Culex quinquefasciatus, vector of West Nile virus and lymphatic filariasis. PLoS ONE 11, e0163863 (2016).
Mordecai, E. A., Ryan, S. J., Caldwell, J. M., Shah, M. M. & LaBeaud, A. D. Climate change could shift disease burden from malaria to arboviruses in Africa. Lancet Planet. Health 4, e416–e423 (2020).
Wang, Z. et al. The relationship between rising temperatures and malaria incidence in Hainan, China, from 1984 to 2010: a longitudinal cohort study. Lancet Planet. Health 6, e350–e358 (2022).
Recht, J. et al. Malaria in Brazil, Colombia, Peru and Venezuela: current challenges in malaria control and elimination. Malar. J. 16, 273 (2017).
Wilder-Smith, A. et al. Epidemic arboviral diseases: priorities for research and public health. Lancet Infect. Dis. 17, e101–e106 (2017).
Cohen, J. A chikungunya vaccine is likely to get approved. Who will get it? Science 382, 503–504 (2023).
Thomas, S. J. Is new dengue vaccine efficacy data a relief or cause for concern? NPJ Vaccines 8, 55 (2023).
Nash, D. et al. The outbreak of West Nile virus infection in the New York City area in 1999. N. Engl. J. Med. 344, 1807–1814 (2001).
Nunes, M. R. et al. Emergence and potential for spread of Chikungunya virus in Brazil. BMC Med. 13, 102 (2015).
Faria, N. R. et al. Zika virus in the Americas: early epidemiological and genetic findings. Science 352, 345–349 (2016).
Jones, K. E. et al. Global trends in emerging infectious diseases. Nature 451, 990–993 (2008).
Gibb, R. et al. Zoonotic host diversity increases in human-dominated ecosystems. Nature 584, 398–402 (2020).
Song, X. P. et al. Global land change from 1982 to 2016. Nature 560, 639–643 (2018).
Santos, C. V. B. D., Sevá, A. D. P. & Werneck, G. L. Does deforestation drive visceral leishmaniasis transmission? A causal analysis. Proc. Biol. Sci. 288, 20211537 (2021).
MacDonald, A. J. & Mordecai, E. A. Amazon deforestation drives malaria transmission, and malaria burden reduces forest clearing. Proc. Natl Acad. Sci. USA 116, 22212–22218 (2019).
Walsh, J. F., Molyneux, D. H. & Birley, M. H. Deforestation: effects on vector-borne disease. Parasitology 106, S55–S75 (1993).
Russell, M. C. et al. Both consumptive and non-consumptive effects of predators impact mosquito populations and have implications for disease transmission. eLife 11, e71503 (2022).
Ducheyne, E. et al. The impact of habitat fragmentation on tsetse abundance on the plateau of eastern Zambia. Prev. Vet. Med. 91, 11–18 (2009).
Van den Bossche, P., Shumba, W. & Makhambera, P. The distribution and epidemiology of bovine trypanosomosis in Malawi. Vet. Parasitol. 88, 163–176 (2000).
Estrada-Peña, A. & Jongejan, F. Ticks feeding on humans: a review of records on human-biting Ixodoidea with special reference to pathogen transmission. Exp. Appl. Acarol. 23, 685–715 (1999).
Kurokawa, C. et al. Interactions between Borrelia burgdorferi and ticks. Nat. Rev. Microbiol. 18, 587–600 (2020).
Levi, T., Keesing, F., Holt, R. D., Barfield, M. & Ostfeld, R. S. Quantifying dilution and amplification in a community of hosts for tick-borne pathogens. Ecol. Appl. 26, 484–498 (2016).
Occhibove, F., Kenobi, K., Swain, M. & Risley, C. An eco-epidemiological modeling approach to investigate dilution effect in two different tick-borne pathosystems. Ecol. Appl. 32, e2550 (2022).
Ogden, N. H. & Tsao, J. I. Biodiversity and Lyme disease: dilution or amplification? Epidemics 1, 196–206 (2009).
Li, S. L. et al. Mapping environmental suitability of Haemagogus and Sabethes spp.mosquitoes to understand sylvatic transmission risk of yellow fever virus in Brazil. PLoS Negl. Trop. Dis. 16, e0010019 (2022).
Faria, N. R. et al. Genomic and epidemiological monitoring of yellow fever virus transmission potential. Science 361, 894–899 (2018).
MacDonald, A. J. Abiotic and habitat drivers of tick vector abundance, diversity, phenology and human encounter risk in southern California. PLoS ONE 13, e0201665 (2018).
Kweka, E. J., Kimaro, E. E. & Munga, S. Effect of deforestation and land use changes on mosquito productivity and development in western Kenya highlands: implication for malaria risk. Front. Public Health 4, 238 (2016).
Burkett-Cadena, N. D. & Vittor, A. Y. Deforestation and vector-borne disease: forest conversion favors important mosquito vectors of human pathogens. Basic. Appl. Ecol. 26, 101–110 (2018).
Plowright, R. K. et al. Pathways to zoonotic spillover. Nat. Rev. Microbiol. 15, 502–510 (2017).
Weaver, S. C. Urbanization and geographic expansion of zoonotic arboviral diseases: mechanisms and potential strategies for prevention. Trends Microbiol. 21, 360–363 (2013).
Hurtt, G. C. et al. Harmonization of land-use scenarios for the period 1500–2100: 600 years of global gridded annual land-use transitions, wood harvest, and resulting secondary lands. Clim. Change 109, 117 (2011).
Waage, J. et al. Changing food systems and infectious disease risks in low-income and middle-income countries. Lancet Planet. Health 6, e760–e768 (2022).
Chan, K. et al. Malaria transmission and prevalence in rice-growing versus non-rice-growing villages in Africa: a systematic review and meta-analysis. Lancet Planet. Health 6, e257–e269 (2022).
Sarfraz, M. S. et al. Analyzing the spatio-temporal relationship between dengue vector larval density and land-use using factor analysis and spatial ring mapping. BMC Public Health 12, 853 (2012).
Franklinos, L. H. V. et al. Joint spatiotemporal modelling reveals seasonally dynamic patterns of Japanese encephalitis vector abundance across India. PLoS Negl. Trop. Dis. 16, e0010218 (2022).
Jones, B. A. et al. Zoonosis emergence linked to agricultural intensification and environmental change. Proc. Natl Acad. Sci. USA 110, 8399–8404 (2013).
Shah, H. A., Huxley, P., Elmes, J. & Murray, K. A. Agricultural land-uses consistently exacerbate infectious disease risks in Southeast Asia. Nat. Commun. 10, 4299 (2019).
Sinka, M. E. et al. The dominant Anopheles vectors of human malaria in the Asia–Pacific region: occurrence data, distribution maps and bionomic précis. Parasit. Vectors 4, 89 (2011).
Trung, H. D. et al. Malaria transmission and major malaria vectors in different geographical areas of Southeast Asia. Trop. Med. Int. Health 9, 230–237 (2004).
Boccolini, D. et al. Impact of environmental changes and human-related factors on the potential malaria vector, Anopheles labranchiae (Diptera: Culicidae), in Maremma, Central Italy. J. Med. Entomol. 49, 833–842 (2012).
Gregory, N., Ewers, R. M., Chung, A. Y. C. & Cator, L. J. Oil palm expansion increases the vectorial capacity of dengue vectors in Malaysian Borneo. PLoS Negl. Trop. Dis. 16, e0009525 (2022).
Le Flohic, G., Porphyre, V., Barbazan, P. & Gonzalez, J. P. Review of climate, landscape, and viral genetics as drivers of the Japanese encephalitis virus ecology. PLoS Negl. Trop. Dis. 7, e2208 (2013).
Tchouassi, D. P. et al. Mosquito host choices on livestock amplifiers of Rift Valley fever virus in Kenya. Parasit. Vectors 9, 184 (2016).
Kumar Pant, D., Tenzin, T., Chand, R., Kumar Sharma, B. & Raj Bist, P. Spatio-temporal epidemiology of Japanese encephalitis in Nepal, 2007–2015. PLoS ONE 12, e0180591 (2017).
Yakob, L. et al. Japanese encephalitis emergence in Australia: the potential population at risk. Clin. Infect. Dis. 76, 335–337 (2022).
Lord, J. S., Gurley, E. S. & Pulliam, J. R. Rethinking Japanese encephalitis virus transmission: a framework for implicating host and vector species. PLoS Negl. Trop. Dis. 9, e0004074 (2015).
Morgan, C. E. et al. Association between domesticated animal ownership and Plasmodium falciparum parasite prevalence in the Democratic Republic of the Congo: a national cross-sectional study. Lancet Microbe 4, e516–e523 (2023).
Kuhn, K. G., Campbell-Lendrum, D. H., Armstrong, B. & Davies, C. R. Malaria in Britain: past, present, and future. Proc. Natl Acad. Sci. USA 100, 9997–10001 (2003).
Hayek, M. N. The infectious disease trap of animal agriculture. Sci. Adv. 8, eadd6681 (2022).
He, C. et al. Future global urban water scarcity and potential solutions. Nat. Commun. 12, 4667 (2021).
Kache, P. A. et al. Bridging landscape ecology and urban science to respond to the rising threat of mosquito-borne diseases. Nat. Ecol. Evol. 6, 1601–1616 (2022).
Wilke, A. B. B. et al. Urbanization favors the proliferation of Aedes aegypti and Culex quinquefasciatus in urban areas of Miami-Dade County, Florida. Sci. Rep. 11, 22989 (2021).
Allan, R., Budge, S. & Sauskojus, H. What sounds like Aedes, acts like Aedes, but is not Aedes? Lessons from dengue virus control for the management of invasive Anopheles. Lancet Glob. Health 11, e165–e169 (2023).
Metz, H. C. et al. Evolution of a mosquito’s hatching behavior to match its human-provided habitat. Am. Nat. 201, 200–214 (2023).
Rose, N. H. et al. Climate and urbanization drive mosquito preference for humans. Curr. Biol. 30, 3570–3579.e6 (2020).
Zhao, Z. et al. Mosquito brains encode unique features of human odour to drive host seeking. Nature 605, 706–712 (2022).
Maquart, P. O., Froehlich, Y. & Boyer, S. Plastic pollution and infectious diseases. Lancet Planet. Health 6, e842–e845 (2022).
Wilke, A. B. B. et al. Urbanization creates diverse aquatic habitats for immature mosquitoes in urban areas. Sci. Rep. 9, 15335 (2019).
Carlson, J., Keating, J., Mbogo, C. M., Kahindi, S. & Beier, J. C. Ecological limitations on aquatic mosquito predator colonization in the urban environment. J. Vector Ecol. 29, 331–339 (2004).
Zhao, L., Lee, X., Smith, R. B. & Oleson, K. Strong contributions of local background climate to urban heat islands. Nature 511, 216–219 (2014).
Zhao, L. et al. Global multi-model projections of local urban climates. Nat. Clim. Change 11, 152–157 (2021).
Patz, J. A., Campbell-Lendrum, D., Holloway, T. & Foley, J. A. Impact of regional climate change on human health. Nature 438, 310–317 (2005).
Caminade, C., McIntyre, K. M. & Jones, A. E. Impact of recent and future climate change on vector-borne diseases. Ann. N. Y. Acad. Sci. 1436, 157–173 (2019).
Nieuwenhuijsen, M. J. Green infrastructure and health. Annu. Rev. Public Health 42, 317–328 (2021).
Medeiros-Sousa, A. R., Fernandes, A., Ceretti-Junior, W., Wilke, A. B. B. & Marrelli, M. T. Mosquitoes in urban green spaces: using an island biogeographic approach to identify drivers of species richness and composition. Sci. Rep. 7, 17826 (2017).
Obame-Nkoghe, J. et al. Urban green spaces and vector-borne disease risk in Africa: the case of an unclean forested park in libreville (Gabon, Central Africa). Int. J. Environ. Res. Public Health 20, 5774 (2023).
Liu, L., Zhong, Y., Ao, S. & Wu, H. Exploring the relevance of green space and epidemic diseases based on panel data in China from 2007 to 2016. Int. J. Environ. Res. Public Health 16, 2551 (2019).
Weiss, D. J. et al. Global maps of travel time to healthcare facilities. Nat. Med. 26, 1835–1838 (2020).
Plowright, R. K. et al. Land use-induced spillover: a call to action to safeguard environmental, animal, and human health. Lancet Planet. Health 5, e237–e245 (2021).
Kibret, S., McCartney, M., Lautze, J., Nhamo, L. & Yan, G. The impact of large and small dams on malaria transmission in four basins in Africa. Sci. Rep. 11, 13355 (2021).
Kibret, S., Lautze, J., McCartney, M., Nhamo, L. & Yan, G. Malaria around large dams in Africa: effect of environmental and transmission endemicity factors. Malar. J. 18, 303 (2019).
Kibret, S. Time to revisit how dams are affecting malaria transmission. Lancet Planet. Health 2, e378–e379 (2018).
De Salazar, P. M., Cox, H., Imhoff, H., Alexandre, J. S. F. & Buckee, C. O. The association between gold mining and malaria in Guyana: a statistical inference and time-series analysis. Lancet Planet. Health 5, e731–e738 (2021).
Fletcher, I. K. et al. Synergies between environmental degradation and climate variation on malaria re-emergence in southern Venezuela: a spatiotemporal modelling study. Lancet Planet. Health 6, e739–e748 (2022).
Rotureau, B., Joubert, M., Clyti, E., Djossou, F. & Carme, B. Leishmaniasis among gold miners, French Guiana. Emerg. Infect. Dis. 12, 1169–1170 (2006).
Duron, O. et al. Novel chronic anaplasmosis in splenectomized patient, Amazon rainforest. Emerg. Infect. Dis. 28, 1673–1676 (2022).
VanAcker, M. C., Little, E. A. H., Molaei, G., Bajwa, W. I. & Diuk-Wasser, M. A. Enhancement of risk for Lyme disease by landscape connectivity, New York, New York, USA. Emerg. Infect. Dis. 25, 1136–1143 (2019).
Yasuoka, J. & Levins, R. Impact of deforestation and agricultural development on anopheline ecology and malaria epidemiology. Am. J. Trop. Med. Hyg. 76, 450–460 (2007).
Stern, A. M. The public health service in the Panama Canal: a forgotten chapter of U.S. public health. Public. Health Rep. 120, 675–679 (2005).
Kraemer, M. U. G. et al. Mapping global variation in human mobility. Nat. Hum. Behav. 4, 800–810 (2020).
Tatem, A. J., Hay, S. I. & Rogers, D. J. Global traffic and disease vector dispersal. Proc. Natl Acad. Sci. USA 103, 6242–6247 (2006).
Chippaux, J. P. & Chippaux, A. Yellow fever in Africa and the Americas: a historical and epidemiological perspective. J. Venom. Anim. Toxins Incl. Trop. Dis. 24, 20 (2018).
Cuthbert, R. N. et al. Invasive hematophagous arthropods and associated diseases in a changing world. Parasit. Vectors 16, 291 (2023).
Tian, H. et al. Increasing airline travel may facilitate co-circulation of multiple dengue virus serotypes in Asia. PLoS Negl. Trop. Dis. 11, e0005694 (2017).
Nunes, M. R. et al. Air travel is associated with intracontinental spread of dengue virus serotypes 1–3 in Brazil. PLoS Negl. Trop. Dis. 8, e2769 (2014).
Baker, R. E. et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 20, 193–205 (2022).
Costard, S. et al. African swine fever: how can global spread be prevented? Philos. Trans. R. Soc. Lond. B Biol. Sci. 364, 2683–2696 (2009).
Rodriguez, M., Hooghuis, H. & Castaño, M. African horse sickness in Spain. Vet. Microbiol. 33, 129–142 (1992).
Diagne, C. et al. High and rising economic costs of biological invasions worldwide. Nature 592, 571–576 (2021).
Juliano, S. A. & Lounibos, L. P. Ecology of invasive mosquitoes: effects on resident species and on human health. Ecol. Lett. 8, 558–574 (2005).
Backus, L. H., Pascoe, E. L. & Foley, J. Will new ticks invade North America? How to identify future invaders. Trends Parasitol. 38, 805–814 (2022).
The Bureau of Transportation Statistics, part of the U.S. Department of Transportation. Air transport, passengers carried. BTS https://www.bts.gov/newsroom/full-year-2022-us-airline-traffic-data (2022).
International Organization for Migration. World Migration Report 2022 https://publications.iom.int/books/world-migration-report-2022 (2021).
McMichael, C. Human mobility, climate change, and health: unpacking the connections. Lancet Planet. Health 4, e217–e218 (2020).
Schütte, S., Gemenne, F., Zaman, M., Flahault, A. & Depoux, A. Connecting planetary health, climate change, and migration. Lancet Planet. Health 2, e58–e59 (2018).
Bharti, N. Linking human behaviors and infectious diseases. Proc. Natl Acad. Sci. USA 118, e2101345118 (2021).
Nsoesie, E. O. et al. Global distribution and environmental suitability for chikungunya virus, 1952 to 2015. Euro Surveill. https://doi.org/10.2807/1560-7917.ES.2016.21.20.30234 (2016).
Reiter, P. et al. Texas lifestyle limits transmission of dengue virus. Emerg. Infect. Dis. 9, 86–89 (2003).
Davis, L. W. & Gertler, P. J. Contribution of air conditioning adoption to future energy use under global warming. Proc. Natl Acad. Sci. USA 112, 5962–5967 (2015).
Centers for Disase Control and Prevention (CDC). Knowledge, attitudes, and behaviors about West Nile virus — Connecticut, 2002. MMWR Morb. Mortal. Wkly. Rep. 52, 886–888 (2003).
McCarthy, T. A. et al. West Nile virus serosurvey and assessment of personal prevention efforts in an area with intense epizootic activity: Connecticut, 2000. Ann. N. Y. Acad. Sci. 951, 307–316 (2001).
Haenchen, S. D. et al. Mosquito avoidance practices and knowledge of arboviral diseases in cities with differing recent history of disease. Am. J. Trop. Med. Hyg. 95, 945–953 (2016).
Adams, L. E. et al. Epidemiology of dengue, chikungunya, and Zika virus disease in U.S. states and territories, 2017. Am. J. Trop. Med. Hyg. 101, 884–890 (2019).
Salje, H. et al. How social structures, space, and behaviors shape the spread of infectious diseases using chikungunya as a case study. Proc. Natl Acad. Sci. USA 113, 13420–13425 (2016).
Slatculescu, A. M. et al. Rurality, socioeconomic status, and residence in environmental risk areas associated with increased lyme disease incidence in Ontario, Canada: a case–control study. Vector Borne Zoonotic Dis. 22, 572–581 (2022).
Aenishaenslin, C. et al. Behavioral risk factors associated with reported tick exposure in a Lyme disease high incidence region in Canada. BMC Public Health 22, 807 (2022).
Costa, G. B., Smithyman, R., O’Neill, S. L. & Moreira, L. A. How to engage communities on a large scale? Lessons from World Mosquito Program in Rio de Janeiro, Brazil. Gates Open. Res. 4, 109 (2020).
de Souza, W. M. et al. Spatiotemporal dynamics and recurrence of chikungunya virus in Brazil: an epidemiological study. Lancet Microbe 4, e319–e329 (2023).
Rohat, G. et al. Intersecting vulnerabilities: climatic and demographic contributions to future population exposure to Aedes-borne viruses in the United States. Environ. Res. Lett. 15, 084046 (2020).
McDonald, E. et al. Surveillance for West Nile virus disease — United States, 2009–2018. MMWR Surveill. Summ. 70, 1–15 (2021).
de Lima, S. T. S. et al. Fatal outcome of chikungunya virus infection in Brazil. Clin. Infect. Dis. 73, e2436–e2443 (2021).
Rowe, E. K. et al. Challenges in dengue fever in the elderly: a typical presentation and risk of severe dengue and hospital-acquired infection [corrected]. PLoS Negl. Trop. Dis. 8, e2777 (2014).
Power, G. M. et al. Socioeconomic risk markers of arthropod-borne virus (arbovirus) infections: a systematic literature review and meta-analysis. BMJ Glob. Health 7, e007735 (2022).
Haakenstad, A. et al. Tracking spending on malaria by source in 106 countries, 2000–16: an economic modelling study. Lancet Infect. Dis. 19, 703–716 (2019).
Shepard, D. S., Undurraga, E. A., Halasa, Y. A. & Stanaway, J. D. The global economic burden of dengue: a systematic analysis. Lancet Infect. Dis. 16, 935–941 (2016).
Ngonghala, C. N. et al. Poverty, disease, and the ecology of complex systems. PloS Biol. 12, e1001827 (2014).
Romanello, M. et al. The 2023 report of the Lancet Countdown on health and climate change: the imperative for a health-centred response in a world facing irreversible harms. Lancet 402, 2346–2394 (2023).
Brady, O. J. et al. The cost-effectiveness of controlling dengue in Indonesia using wMel Wolbachia released at scale: a modelling study. BMC Med. 18, 186 (2020).
Nwaiwu, A. U., Musekiwa, A., Tamuzi, J. L., Sambala, E. Z. & Nyasulu, P. S. The incidence and mortality of yellow fever in Africa: a systematic review and meta-analysis. BMC Infect. Dis. 21, 1089 (2021).
Fieler, A. M. et al. Larval thermal characteristics of multiple ixodid ticks. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 257, 110939 (2021).
Li, S. et al. Lyme disease risks in Europe under multiple uncertain drivers of change. Env. Health Perspect. 127, 67010 (2019).
Acknowledgements
W.M.d.S. is supported by a Global Virus Network fellowship, Burroughs Wellcome Fund — Climate Change and Human Health Seed Grants (no. 1022448) and Wellcome Trust — Digital Technology Development Award in Climate Sensitive Infectious Disease Modelling (no. 226075/Z/22/Z). S.C.W. is supported by National Institutes of Health (NIH) grant AI120942.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Microbiology thanks Matthew Baylis, Cyril Caminade and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Anthropogenic
-
Resulting from the influence of humans on nature.
- Enzootic
-
Ancestral, often continuous cycles of zoonotic arboviruses involving wild animals serving as amplification and/or reservoir hosts.
- Epizootic
-
An outbreak of disease in non-human animal populations.
- Global warming
-
Long-term heating of the Earth’s surface observed since the pre-industrial period.
- Spillback
-
Transmission of pathogens from humans to wild animals, sometimes resulting in stable enzootic cycles.
- Spillover
-
Pathogen transmission from zoonotic wildlife hosts to humans, sometimes resulting in stable human-amplified transmission.
- Thermal performance curves
-
Effects of ambient temperature on biological rate processes of organisms, including vectors, from behaviour to biological processes, that can be used to predict the potential effects of global warming on ecological systems.
- Tipping points
-
Critical thresholds in a climate system that, when exceeded, can lead to a significant change in the climate state, often with predicted irreversible changes.
- Trans-stadial transmission
-
Sequential passage of pathogens acquired during one life stage, or stadium, through the moult to the next stage or stages, or stadium.
- Vector competence
-
The intrinsic ability of an arthropod to become infected and transmit a pathogen.
- Zoonotic
-
Infections that spill over from non-human animals to humans.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Souza, W.M., Weaver, S.C. Effects of climate change and human activities on vector-borne diseases. Nat Rev Microbiol (2024). https://doi.org/10.1038/s41579-024-01026-0
Accepted:
Published:
DOI: https://doi.org/10.1038/s41579-024-01026-0