Abstract
Prion diseases are progressive, incurable and fatal neurodegenerative conditions. The term ‘prion’ was first nominated to express the revolutionary concept that a protein could be infectious. We now know that prions consist of PrPSc, the pathological aggregated form of the cellular prion protein PrPC. Over the years, the term has been semantically broadened to describe aggregates irrespective of their infectivity, and the prion concept is now being applied, perhaps overenthusiastically, to all neurodegenerative diseases that involve protein aggregation. Indeed, recent studies suggest that prion diseases (PrDs) and protein misfolding disorders (PMDs) share some common disease mechanisms, which could have implications for potential treatments. Nevertheless, the transmissibility of bona fide prions is unique, and PrDs should be considered as distinct from other PMDs.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Brown, P., Cathala, F., Castaigne, P. & Gajdusek, D. C. Creutzfeldt-Jakob disease: clinical analysis of a consecutive series of 230 neuropathologically verified cases. Ann. Neurol. 20, 597–602 (1986).
Prusiner, S. B. Novel proteinaceous infectious particles cause scrapie. Science 216, 136–144 (1982). This paper introduces the term ‘prion’ to describe the revolutionary concept of protein-mediated transmissibility.
Bolton, D. C., McKinley, M. P. & Prusiner, S. B. Identification of a protein that purifies with the scrapie prion. Science 218, 1309–1311 (1982). This study demonstrates that prions contain an aggregated form of a cellular protein.
Büeler, H. et al. Mice devoid of PrP are resistant to scrapie. Cell 73, 1339–1347 (1993). This paper provides confirmation that PrP C is required for prion propagation and disease manifestation.
Jarrett, J. T. & Lansbury, P. T. Seeding ‘one-dimensional crystallization’ of amyloid: a pathogenic mechanism in Alzheimer’s disease and scrapie? Cell 73, 1055–1058 (1993).
Knowles, T. P. J. et al. An analytical solution to the kinetics of breakable filament assembly. Science 326, 1533–1537 (2009). This analytical approach describes how fragmentation-nucleation cycles contribute to aggregate propagation.
Cox, B., Ness, F. & Tuite, M. Analysis of the generation and segregation of propagons: entities that propagate the [PSI+] prion in yeast. Genetics 165, 23–33 (2003).
Aguzzi, A. & Lakkaraju, A. K. K. Cell biology of prions and prionoids: a status report. Trends Cell Biol. 26, 40–51 (2016).
Saborio, G. P., Permanne, B. & Soto, C. Sensitive detection of pathological prion protein by cyclic amplification of protein misfolding. Nature 411, 810–813 (2001).
Sailer, A., Büeler, H., Fischer, M., Aguzzi, A. & Weissmann, C. No propagation of prions in mice devoid of PrP. Cell 77, 967–968 (1994).
Brandner, S. et al. Normal host prion protein necessary for scrapie-induced neurotoxicity. Nature 379, 339–343 (1996). This paper demonstrates that aggregation and aggregation-induced toxicity can be uncoupled by chronically exposing PrP-deficient mice to prions.
Hu, P. P. et al. Role of prion replication in the strain-dependent brain regional distribution of prions. J. Biol. Chem. 291, 12880–12887 (2016).
Glatzel, M., Abela, E., Maissen, M. & Aguzzi, A. Extraneural pathologic prion protein in sporadic Creutzfeldt-Jakob disease. N. Engl. J. Med. 349, 1812–1820 (2003).
Aguzzi, A. Cell biology: beyond the prion principle. Nature 459, 924–925 (2009). This paper introduces the term ‘prionoid’ to describe aggregates that can spread between cells but for which transmissibility between individuals has not yet been demonstrated.
Aguzzi, A. & Rajendran, L. The transcellular spread of cytosolic amyloids, prions, and prionoids. Neuron 64, 783–790 (2009).
Bruce, M. E. et al. Transmissions to mice indicate that ‘new variant’ CJD is caused by the BSE agent. Nature 389, 498–501 (1997).
Wells, G. A. et al. A novel progressive spongiform encephalopathy in cattle. Vet. Rec. 121, 419–420 (1987).
Williams, E. S. & Young, S. Chronic wasting disease of captive mule deer: a spongiform encephalopathy. J. Wildl. Dis. 16, 89–98 (1980).
Aguzzi, A., Heikenwalder, M. & Polymenidou, M. Insights into prion strains and neurotoxicity. Nat. Rev. Mol. Cell. Biol. 8, 552–561 (2007).
Kretzschmar, H. A. et al. Molecular cloning of a human prion protein cDNA. DNA 5, 315–324 (1986).
Riek, R. et al. NMR structure of the mouse prion protein domain PrP(121–231). Nature 382, 180–182 (1996).
Wulf, M.-A., Senatore, A. & Aguzzi, A. The biological function of the cellular prion protein: an update. BMC Biol. 15, 34 (2017).
Nuvolone, M. et al. Strictly co-isogenic C57BL/6 J-Prnp−/− mice: a rigorous resource for prion science. J. Exp. Med. 213, 313–327 (2016).
Nuvolone, M. et al. SIRPα polymorphisms, but not the prion protein, control phagocytosis of apoptotic cells. J. Exp. Med. 210, 2539–2552 (2013).
Bremer, J. et al. Axonal prion protein is required for peripheral myelin maintenance. Nat. Neurosci. 13, 310–318 (2010).
Küffer, A. et al. The prion protein is an agonistic ligand of the G protein-coupled receptor Adgrg6. Nature 536, 464–468 (2016).
Hsiao, K. et al. Linkage of a prion protein missense variant to Gerstmann-Sträussler syndrome. Nature 338, 342–345 (1989).
Medori, R. et al. Fatal familial insomnia, a prion disease with a mutation at codon 178 of the prion protein gene. N. Engl. J. Med. 326, 444–449 (1992).
Kretzschmar, H. A., Neumann, M. & Stavrou, D. Codon 178 mutation of the human prion protein gene in a German family (Backer family): sequencing data from 72-year-old celloidin-embedded brain tissue. Acta Neuropathol. 89, 96–98 (1995).
Apetri, A. C., Vanik, D. L. & Surewicz, W. K. Polymorphism at residue 129 modulates the conformational conversion of the D178N variant of human prion protein 90–231. Biochemistry 44, 15880–15888 (2005).
Hsiao, K. et al. Mutation of the prion protein in Libyan Jews with Creutzfeldt-Jakob disease. N. Engl. J. Med. 324, 1091–1097 (1991).
Pocchiari, M. et al. A new point mutation of the prion protein gene in Creutzfeldt-Jakob disease. Ann. Neurol. 34, 802–807 (1993).
Capellari, S., Strammiello, R., Saverioni, D., Kretzschmar, H. & Parchi, P. Genetic Creutzfeldt-Jakob disease and fatal familial insomnia: insights into phenotypic variability and disease pathogenesis. Acta Neuropathol. 121, 21–37 (2011).
Parchi, P. et al. Molecular basis of phenotypic variability in sporadic Creutzfeldt-Jakob disease. Ann. Neurol. 39, 767–778 (1996).
Palmer, M. S., Dryden, A. J., Hughes, J. T. & Collinge, J. Homozygous prion protein genotype predisposes to sporadic Creutzfeldt-Jakob disease. Nature 352, 340–342 (1991).
Nurmi, M. H. et al. The normal population distribution of PRNP codon 129 polymorphism. Acta Neurol. Scand. 108, 374–378 (2003).
Pocchiari, M. et al. Predictors of survival in sporadic Creutzfeldt-Jakob disease and other human transmissible spongiform encephalopathies. Brain 127, 2348–2359 (2004).
Mok, T. et al. Variant Creutzfeldt-Jakob disease in a patient with heterozygosity at PRNP codon 129. N. Engl. J. Med. 376, 292–294 (2017).
Llewelyn, C. A. et al. Possible transmission of variant Creutzfeldt-Jakob disease by blood transfusion. Lancet 363, 417–421 (2004).
Wroe, S. J. et al. Clinical presentation and pre-mortem diagnosis of variant Creutzfeldt-Jakob disease associated with blood transfusion: a case report. Lancet 368, 2061–2067 (2006).
Peden, A. H., Head, M. W., Ritchie, D. L., Bell, J. E. & Ironside, J. W. Preclinical vCJD after blood transfusion in a PRNP codon 129 heterozygous patient. Lancet 364, 527–529 (2004).
Mead, S. et al. A novel protective prion protein variant that colocalizes with kuru exposure. N. Engl. J. Med. 361, 2056–2065 (2009).
Shibuya, S., Higuchi, J., Shin, R. W., Tateishi, J. & Kitamoto, T. Protective prion protein polymorphisms against sporadic Creutzfeldt-Jakob disease. Lancet 351, 419 (1998).
Asante, E. A. et al. A naturally occurring variant of the human prion protein completely prevents prion disease. Nature 522, 478–481 (2015).
Mead, S. et al. Genetic risk factors for variant Creutzfeldt-Jakob disease: a genome-wide association study. Lancet Neurol. 8, 57–66 (2009).
Mead, S. et al. Genome-wide association study in multiple human prion diseases suggests genetic risk factors additional to PRNP. Hum. Mol. Genet. 21, 1897–1906 (2012).
Sanchez-Juan, P. et al. A genome wide association study links glutamate receptor pathway to sporadic Creutzfeldt-Jakob disease risk. PLoS ONE 10, e0123654 (2014).
Minikel, E. V. et al. Quantifying prion disease penetrance using large population control cohorts. Sci. Transl Med. 8, 322ra9 (2016).
Xu, J. et al. Gain of function of mutant p53 by coaggregation with multiple tumor suppressors. Nat. Chem. Biol. 7, 285–295 (2011).
Levy, C. B. et al. Co-localization of mutant p53 and amyloid-like protein aggregates in breast tumors. Int. J. Biochem. Cell Biol. 43, 60–64 (2011).
Forget, K. J., Tremblay, G. & Roucou, X. p53 aggregates penetrate cells and induce the co-aggregation of intracellular p53. PLoS ONE 8, e69242 (2013).
Ghosh, S. et al. p53 amyloid formation leading to its loss of function: implications in cancer pathogenesis. Cell Death Differ. 24, 1784–1798 (2017).
Alexandrova, E. M. et al. Improving survival by exploiting tumour dependence on stabilized mutant p53 for treatment. Nature 523, 352–356 (2015).
Mukherjee, A. et al. Induction of IAPP amyloid deposition and associated diabetic abnormalities by a prion-like mechanism. J. Exp. Med. 214, 2591–2610 (2017).
Murakami, T., Ishiguro, N. & Higuchi, K. Transmission of systemic AA amyloidosis in animals. Vet. Pathol. 51, 363–371 (2014).
Watts, J. C. et al. Transmission of multiple system atrophy prions to transgenic mice. Proc. Natl Acad. Sci. USA 110, 19555–19560 (2013). This study demonstrates that α-synuclein aggregates are transmissible to mice expressing a human aggregation-prone form of α-synuclein.
Prusiner, S. B. et al. Evidence for α-synuclein prions causing multiple system atrophy in humans with parkinsonism. Proc. Natl Acad. Sci. USA 112, E5308–E5317 (2015).
Sigurdson, C. J. et al. A molecular switch controls interspecies prion disease transmission in mice. J. Clin. Invest. 120, 2590–2599 (2010).
Sacino, A. N. et al. Non-prion-type transmission in A53T α-synuclein transgenic mice: a normal component of spinal homogenates from naïve non-transgenic mice induces robust α-synuclein pathology. Acta Neuropathol. 131, 151–154 (2016).
Kurowska, Z. et al. Signs of degeneration in 12-22-year old grafts of mesencephalic dopamine neurons in patients with Parkinson’s disease. J. Parkinsons Dis. 1, 83–92 (2011).
Kordower, J. H., Chu, Y., Hauser, R. A., Freeman, T. B. & Olanow, C. W. Lewy body-like pathology in long-term embryonic nigral transplants in Parkinson’s disease. Nat. Med. 14, 504–506 (2008).
Kordower, J. H., Chu, Y., Hauser, R. A., Olanow, C. W. & Freeman, T. B. Transplanted dopaminergic neurons develop PD pathologic changes: a second case report. Mov. Disord. 23, 2303–2306 (2008).
Li, W. et al. Extensive graft-derived dopaminergic innervation is maintained 24 years after transplantation in the degenerating parkinsonian brain. Proc. Natl Acad. Sci. USA 113, 6544–6549 (2016).
Li, J.-Y. et al. Lewy bodies in grafted neurons in subjects with Parkinson’s disease suggest host-to-graft disease propagation. Nat. Med. 14, 501–503 (2008).
Thal, D. R., Rüb, U., Orantes, M. & Braak, H. Phases of Aβ-deposition in the human brain and its relevance for the development of AD. Neurology 58, 1791–1800 (2002).
Meyer-Luehmann, M. et al. Exogenous induction of cerebral beta-amyloidogenesis is governed by agent and host. Science 313, 1781–1784 (2006).
Stöhr, J. et al. Purified and synthetic Alzheimer’s amyloid beta (Aβ) prions. Proc. Natl Acad. Sci. USA 109, 11025–11030 (2012).
Jaunmuktane, Z. et al. Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy. Nature 525, 247–250 (2015).
Ritchie, D. L. et al. Amyloid-β accumulation in the CNS in human growth hormone recipients in the UK. Acta Neuropathol. 134, 221–240 (2017).
Frontzek, K., Lutz, M. I., Aguzzi, A., Kovacs, G. G. & Budka, H. Amyloid-β pathology and cerebral amyloid angiopathy are frequent in iatrogenic Creutzfeldt-Jakob disease after dural grafting. Swiss Med. Wkly 146, w14287 (2016).
Arnold, S. E. et al. Comparative survey of the topographical distribution of signature molecular lesions in major neurodegenerative diseases. J. Comp. Neurol. 521, 4339–4355 (2013).
Audouard, E. et al. High-molecular-weight paired helical filaments from Alzheimer brain induces seeding of wild-type mouse tau into an argyrophilic 4R tau pathology in vivo. Am. J. Pathol. 186, 2709–2722 (2016).
Duyckaerts, C. et al. Neuropathology of iatrogenic Creutzfeldt-Jakob disease and immunoassay of French cadaver-sourced growth hormone batches suggest possible transmission of tauopathy and long incubation periods for the transmission of Aβ pathology. Acta Neuropathol. 135, 201–212 (2018).
Malinovska, L., Kroschwald, S. & Alberti, S. Protein disorder, prion propensities, and self-organizing macromolecular collectives. Biochim. Biophys. Acta 1834, 918–931 (2013).
Hyman, A. A., Weber, C. A. & Jülicher, F. Liquid-liquid phase separation in biology. Annu. Rev. Cell Dev. Biol. 30, 39–58 (2014).
Sonati, T. et al. The toxicity of antiprion antibodies is mediated by the flexible tail of the prion protein. Nature 501, 102–106 (2013). This study demonstrates that antibodies can be protective or toxic, depending on the recognized epitope.
Heppner, F. L. et al. Prevention of scrapie pathogenesis by transgenic expression of anti-prion protein antibodies. Science 294, 178–182 (2001). This paper introduces the novel concept that prion disease pathogenesis can be inhibited by protective PrP antibodies.
Polymenidou, M. et al. The POM monoclonals: a comprehensive set of antibodies to non-overlapping prion protein epitopes. PLoS ONE 3, e3872 (2008).
Herrmann, U. S. et al. Prion infections and anti-PrP antibodies trigger converging neurotoxic pathways. PLoS Pathog. 11, e1004662 (2015).
Falsig, J. et al. Prion pathogenesis is faithfully reproduced in cerebellar organotypic slice cultures. PLoS Pathog. 8, e1002985 (2012).
Frontzek, K. et al. Neurotoxic antibodies against the prion protein do not trigger prion replication. PLoS ONE 11, e0163601 (2016).
Yim, Y.-I. et al. The multivesicular body is the major internal site of prion conversion. J. Cell. Sci. 128, 1434–1443 (2015).
Vella, L. J., Hill, A. F. & Cheng, L. Focus on extracellular vesicles: exosomes and their role in protein trafficking and biomarker potential in Alzheimer’s and Parkinson’s disease. Int. J. Mol. Sci. 17, 173 (2016).
Gousset, K. et al. Prions hijack tunnelling nanotubes for intercellular spread. Nat. Cell Biol. 11, 328–336 (2009).
Senatore, A. et al. Mutant PrP suppresses glutamatergic neurotransmission in cerebellar granule neurons by impairing membrane delivery of VGCC α(2)δ-1 subunit. Neuron 74, 300–313 (2012).
Rodríguez, A. et al. Metabotropic glutamate receptor/phospholipase C pathway: a vulnerable target to Creutzfeldt-Jakob disease in the cerebral cortex. Neuroscience 131, 825–832 (2005).
Rodríguez, A. et al. Group I mGluR signaling in BSE-infected bovine-PrP transgenic mice. Neurosci. Lett. 410, 115–120 (2006).
Goniotaki, D. et al. Inhibition of group-I metabotropic glutamate receptors protects against prion toxicity. PLoS Pathog. 13, e1006733 (2017).
Khosravani, H. et al. Prion protein attenuates excitotoxicity by inhibiting NMDA receptors. J. Gen. Physiol. 131, i5 (2008).
Laurén, J., Gimbel, D. A., Nygaard, H. B., Gilbert, J. W. & Strittmatter, S. M. Cellular prion protein mediates impairment of synaptic plasticity by amyloid-beta oligomers. Nature 457, 1128–1132 (2009).
Gimbel, D. A. et al. Memory impairment in transgenic Alzheimer mice requires cellular prion protein. J. Neurosci. 30, 6367–6374 (2010).
Haas, L. T., Kostylev, M. A. & Strittmatter, S. M. Therapeutic molecules and endogenous ligands regulate the interaction between brain cellular prion protein (PrPC) and metabotropic glutamate receptor 5 (mGluR5). J. Biol. Chem. 289, 28460–28477 (2014).
Um, J. W. et al. Metabotropic glutamate receptor 5 is a coreceptor for Alzheimer aβ oligomer bound to cellular prion protein. Neuron 79, 887–902 (2013).
Um, J. W. et al. Alzheimer amyloid-β oligomer bound to postsynaptic prion protein activates Fyn to impair neurons. Nat. Neurosci. 15, 1227–1235 (2012).
Hu, N.-W. et al. mGlu5 receptors and cellular prion protein mediate amyloid-β-facilitated synaptic long-term depression in vivo. Nat. Commun. 5, 3374 (2014).
Ostapchenko, V. G. et al. Increased prion protein processing and expression of metabotropic glutamate receptor 1 in a mouse model of Alzheimer’s disease. J. Neurochem. 127, 415–425 (2013).
Renner, M. et al. Deleterious effects of amyloid beta oligomers acting as an extracellular scaffold for mGluR5. Neuron 66, 739–754 (2010).
Hamilton, A., Esseltine, J. L., DeVries, R. A., Cregan, S. P. & Ferguson, S. S. G. Metabotropic glutamate receptor 5 knockout reduces cognitive impairment and pathogenesis in a mouse model of Alzheimer’s disease. Mol. Brain 7, 40 (2014).
Balducci, C. et al. Synthetic amyloid-beta oligomers impair long-term memory independently of cellular prion protein. Proc. Natl Acad. Sci. USA 107, 2295–2300 (2010).
Kessels, H. W., Nguyen, L. N., Nabavi, S. & Malinow, R. The prion protein as a receptor for amyloid-beta. Nature 466, E3–E4 (2010).
Calella, A. M. et al. Prion protein and Abeta-related synaptic toxicity impairment. EMBO Mol. Med. 2, 306–314 (2010).
Cissé, M. et al. Ablation of cellular prion protein does not ameliorate abnormal neural network activity or cognitive dysfunction in the J20 line of human amyloid precursor protein transgenic mice. J. Neurosci. 31, 10427–10431 (2011).
Aulic, S. et al. α-Synuclein amyloids hijack prion protein to gain cell entry, facilitate cell-to-cell spreading and block prion replication. Sci. Rep. 7, 10050 (2017).
Ferreira, D. G. et al. α-Synuclein interacts with PrP(C) to induce cognitive impairment through mGluR5 and NMDAR2B. Nat. Neurosci. 20, 1569–1579 (2017).
Diógenes, M. J. et al. Extracellular alpha-synuclein oligomers modulate synaptic transmission and impair LTP via NMDA-receptor activation. J. Neurosci. 32, 11750–11762 (2012).
Parizek, P. et al. Similar turnover and shedding of the cellular prion protein in primary lymphoid and neuronal cells. J. Biol. Chem. 276, 44627–44632 (2001).
Yedidia, Y., Horonchik, L., Tzaban, S., Yanai, A. & Taraboulos, A. Proteasomes and ubiquitin are involved in the turnover of the wild-type prion protein. EMBO J. 20, 5383–5391 (2001).
Ma, J. & Lindquist, S. Conversion of PrP to a self-perpetuating PrPSc-like conformation in the cytosol. Science 298, 1785–1788 (2002).
Stewart, R. S., Drisaldi, B. & Harris, D. A. A transmembrane form of the prion protein contains an uncleaved signal peptide and is retained in the endoplasmic reticulum. Mol. Biol. Cell 12, 881–889 (2001).
Ma, J. & Lindquist, S. Wild-type PrP and a mutant associated with prion disease are subject to retrograde transport and proteasome degradation. Proc. Natl Acad. Sci. USA 98, 14955–14960 (2001).
Zanusso, G. et al. Proteasomal degradation and N-terminal protease resistance of the codon 145 mutant prion protein. J. Biol. Chem. 274, 23396–23404 (1999).
Jin, T. et al. The chaperone protein BiP binds to a mutant prion protein and mediates its degradation by the proteasome. J. Biol. Chem. 275, 38699–38704 (2000).
Drisaldi, B. et al. Mutant PrP is delayed in its exit from the endoplasmic reticulum, but neither wild-type nor mutant PrP undergoes retrotranslocation prior to proteasomal degradation. J. Biol. Chem. 278, 21732–21743 (2003).
Kristiansen, M. et al. Disease-associated prion protein oligomers inhibit the 26S proteasome. Mol. Cell 26, 175–188 (2007).
Kristiansen, M. et al. Disease-related prion protein forms aggresomes in neuronal cells leading to caspase activation and apoptosis. J. Biol. Chem. 280, 38851–38861 (2005).
Deriziotis, P. et al. Misfolded PrP impairs the UPS by interaction with the 20S proteasome and inhibition of substrate entry. EMBO J. 30, 3065–3077 (2011).
Moreno, J. A. et al. Sustained translational repression by eIF2α-P mediates prion neurodegeneration. Nature 485, 507–511 (2012).
Abisambra, J. F. et al. Tau accumulation activates the unfolded protein response by impairing endoplasmic reticulum-associated degradation. J. Neurosci. 33, 9498–9507 (2013).
Atkin, J. D. et al. Endoplasmic reticulum stress and induction of the unfolded protein response in human sporadic amyotrophic lateral sclerosis. Neurobiol. Dis. 30, 400–407 (2008).
Devi, L. & Ohno, M. PERK mediates eIF2α phosphorylation responsible for BACE1 elevation, CREB dysfunction and neurodegeneration in a mouse model of Alzheimer’s disease. Neurobiol. Aging 35, 2272–2281 (2014).
Saxena, S., Cabuy, E. & Caroni, P. A role for motoneuron subtype-selective ER stress in disease manifestations of FALS mice. Nat. Neurosci. 12, 627–636 (2009).
Hoozemans, J. J. M. et al. Activation of the unfolded protein response in Parkinson’s disease. Biochem. Biophys. Res. Commun. 354, 707–711 (2007).
Radford, H., Moreno, J. A., Verity, N., Halliday, M. & Mallucci, G. R. PERK inhibition prevents tau-mediated neurodegeneration in a mouse model of frontotemporal dementia. Acta Neuropathol. 130, 633–642 (2015).
Horiuchi, M., Yamazaki, N., Ikeda, T., Ishiguro, N. & Shinagawa, M. A cellular form of prion protein (PrPC) exists in many non-neuronal tissues of sheep. J. Gen. Virol. 76, 2583–2587 (1995).
Arai, H. et al. Expression patterns of beta-amyloid precursor protein (beta-APP) in neural and nonneural human tissues from Alzheimer’s disease and control subjects. Ann. Neurol. 30, 686–693 (1991).
Gu, Y., Oyama, F. & Ihara, Y. Tau is widely expressed in rat tissues. J. Neurochem. 67, 1235–1244 (1996).
Klein, M. A. et al. A crucial role for B cells in neuroinvasive scrapie. Nature 390, 687–690 (1997).
Raeber, A. J. et al. Ectopic expression of prion protein (PrP) in T lymphocytes or hepatocytes of PrP knockout mice is insufficient to sustain prion replication. Proc. Natl Acad. Sci. USA 96, 3987–3992 (1999).
Yang, W. & Yu, S. Synucleinopathies: common features and hippocampal manifestations. Cell. Mol. Life Sci. 74, 1485–1501 (2017).
Ferrer, I., Casas, R. & Rivera, R. Parvalbumin-immunoreactive cortical neurons in Creutzfeldt-Jakob disease. Ann. Neurol. 34, 864–866 (1993).
Guentchev, M., Groschup, M. H., Kordek, R., Liberski, P. P. & Budka, H. Severe, early and selective loss of a subpopulation of GABAergic inhibitory neurons in experimental transmissible spongiform encephalopathies. Brain Pathol. 8, 615–623 (1998).
Guentchev, M., Wanschitz, J., Voigtländer, T., Flicker, H. & Budka, H. Selective neuronal vulnerability in human prion diseases. Fatal familial insomnia differs from other types of prion diseases. Am. J. Pathol. 155, 1453–1457 (1999).
Sargent, D. et al. ‘Prion-like’ propagation of the synucleinopathy of M83 transgenic mice depends on the mouse genotype and type of inoculum. J. Neurochem. 143, 126–135 (2017).
Bu, X.-L. et al. Blood-derived amyloid-β protein induces Alzheimer’s disease pathologies. Mol. Psychiatry https://doi.org/10.1038/mp.2017.204 (2017).
Glatzel, M., Heppner, F. L., Albers, K. M. & Aguzzi, A. Sympathetic innervation of lymphoreticular organs is rate limiting for prion neuroinvasion. Neuron 31, 25–34 (2001).
Prinz, M. et al. Positioning of follicular dendritic cells within the spleen controls prion neuroinvasion. Nature 425, 957–962 (2003).
Hill, A. F. et al. The same prion strain causes vCJD and BSE. Nature 389, 448–450 (1997).
Saido, T. C. et al. Dominant and differential deposition of distinct beta-amyloid peptide species, Aβ N3(pE), in senile plaques. Neuron 14, 457–466 (1995).
Schilling, S. et al. Glutaminyl cyclase inhibition attenuates pyroglutamate Abeta and Alzheimer’s disease-like pathology. Nat. Med. 14, 1106–1111 (2008).
Castegna, A. et al. Proteomic identification of nitrated proteins in Alzheimer’s disease brain. J. Neurochem. 85, 1394–1401 (2003).
Smith, M. A., Richey Harris, P. L., Sayre, L. M., Beckman, J. S. & Perry, G. Widespread peroxynitrite-mediated damage in Alzheimer’s disease. J. Neurosci. 17, 2653–2657 (1997).
Sweeney, P. et al. Protein misfolding in neurodegenerative diseases: implications and strategies. Transl Neurodegener. 6, 6 (2017).
Steele, A. D. et al. Heat shock factor 1 regulates lifespan as distinct from disease onset in prion disease. Proc. Natl Acad. Sci. USA 105, 13626–13631 (2008).
Baldo, B. et al. A screen for enhancers of clearance identifies huntingtin as a heat shock protein 90 (Hsp90) client protein. J. Biol. Chem. 287, 1406–1414 (2012).
Luo, W. et al. Roles of heat-shock protein 90 in maintaining and facilitating the neurodegenerative phenotype in tauopathies. Proc. Natl Acad. Sci. USA 104, 9511–9516 (2007).
Labbadia, J. et al. Altered chromatin architecture underlies progressive impairment of the heat shock response in mouse models of Huntington disease. J. Clin. Invest. 121, 3306–3319 (2011).
Putcha, P. et al. Brain-permeable small-molecule inhibitors of Hsp90 prevent alpha-synuclein oligomer formation and rescue alpha-synuclein-induced toxicity. J. Pharmacol. Exp. Ther. 332, 849–857 (2010).
Hetz, C., Russelakis-Carneiro, M., Maundrell, K., Castilla, J. & Soto, C. Caspase-12 and endoplasmic reticulum stress mediate neurotoxicity of pathological prion protein. EMBO J. 22, 5435–5445 (2003).
Yoo, B. C. et al. Overexpressed protein disulfide isomerase in brains of patients with sporadic Creutzfeldt-Jakob disease. Neurosci. Lett. 334, 196–200 (2002).
Hoshino, T. et al. Endoplasmic reticulum chaperones inhibit the production of amyloid-beta peptides. Biochem. J. 402, 581–589 (2007).
Park, K.-W. et al. The endoplasmic reticulum chaperone GRP78/BiP modulates prion propagation in vitro and in vivo. Sci. Rep. 7, 44723 (2017).
Hetz, C. et al. The disulfide isomerase Grp58 is a protective factor against prion neurotoxicity. J. Neurosci. 25, 2793–2802 (2005).
Glover, J. R. & Lindquist, S. Hsp104, Hsp70, and Hsp40: a novel chaperone system that rescues previously aggregated proteins. Cell 94, 73–82 (1998).
Shorter, J. & Lindquist, S. Hsp104 catalyzes formation and elimination of self-replicating Sup35 prion conformers. Science 304, 1793–1797 (2004).
Chernoff, Y. O., Lindquist, S. L., Ono, B., Inge-Vechtomov, S. G. & Liebman, S. W. Role of the chaperone protein Hsp104 in propagation of the yeast prion-like factor [psi+]. Science 268, 880–884 (1995).
Aguzzi, A., Lakkaraju, A. K. K. & Frontzek, K. Toward therapy of human prion diseases. Annu. Rev. Pharmacol. Toxicol. 58, 331–351 (2018).
Silva, J. L., De Moura Gallo, C. V., Costa, D. C. F. & Rangel, L. P. Prion-like aggregation of mutant p53 in cancer. Trends Biochem. Sci. 39, 260–267 (2014).
Whitesell, L. & Lindquist, S. L. HSP90 and the chaperoning of cancer. Nat. Rev. Cancer 5, 761–772 (2005).
Soragni, A. et al. A designed inhibitor of p53 aggregation rescues p53 tumor suppression in ovarian carcinomas. Cancer Cell 29, 90–103 (2016).
Wang, B. et al. A CNS-permeable Hsp90 inhibitor rescues synaptic dysfunction and memory loss in APP-overexpressing Alzheimer’s mouse model via an HSF1-mediated mechanism. Mol. Psychiatry 22, 990–1001 (2017).
Ansar, S. et al. A non-toxic Hsp90 inhibitor protects neurons from Aβ-induced toxicity. Bioorg. Med. Chem. Lett. 17, 1984–1990 (2007).
Diaz-Espinoza, R. et al. Treatment with a non-toxic, self-replicating anti-prion delays or prevents prion disease in vivo. Mol. Psychiatry 23, 777–788 (2018).
Abeliovich, A. et al. Mice lacking alpha-synuclein display functional deficits in the nigrostriatal dopamine system. Neuron 25, 239–252 (2000).
Zheng, H. et al. β-Amyloid precursor protein-deficient mice show reactive gliosis and decreased locomotor activity. Cell 81, 525–531 (1995).
Soto, C. et al. Reversion of prion protein conformational changes by synthetic beta-sheet breaker peptides. Lancet 355, 192–197 (2000).
Nilsson, K. P. R. et al. Structural typing of systemic amyloidoses by luminescent-conjugated polymer spectroscopy. Am. J. Pathol. 176, 563–574 (2010).
Margalith, I. et al. Polythiophenes inhibit prion propagation by stabilizing prion protein (PrP) aggregates. J. Biol. Chem. 287, 18872–18887 (2012).
Sigurdson, C. J. et al. Prion strain discrimination using luminescent conjugated polymers. Nat. Methods 4, 1023–1030 (2007).
Herrmann, U. S. et al. Structure-based drug design identifies polythiophenes as antiprion compounds. Sci. Transl Med. 7, 299ra123 (2015).
Frenzel, A., Schirrmann, T. & Hust, M. Phage display-derived human antibodies in clinical development and therapy. mAbs 8, 1177–1194 (2016).
Polymenidou, M. et al. Humoral immune response to native eukaryotic prion protein correlates with anti-prion protection. Proc. Natl Acad. Sci. USA 101(Suppl. 2), 14670–14676 (2004).
Falsig, J. & Aguzzi, A. The prion organotypic slice culture assay — POSCA. Nat. Protoc. 3, 555–562 (2008).
Zhu, C. et al. A neuroprotective role for microglia in prion diseases. J. Exp. Med. 213, 1047–1059 (2016).
Kranich, J. et al. Engulfment of cerebral apoptotic bodies controls the course of prion disease in a mouse strain-dependent manner. J. Exp. Med. 207, 2271–2281 (2010).
Sevigny, J. et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature 537, 50–56 (2016). This paper describes the human antibody aducanumab, the first therapeutic shown to affect the cognitive decline in AD patients.
Cummings, J. L., Morstorf, T. & Zhong, K. Alzheimer’s disease drug-development pipeline: few candidates, frequent failures. Alzheimers Res. Ther. 6, 37 (2014).
Price, J. L. & Morris, J. C. Tangles and plaques in nondemented aging and ‘preclinical’ Alzheimer’s disease. Ann. Neurol. 45, 358–368 (1999).
Jack, C. R. et al. Serial PIB and MRI in normal, mild cognitive impairment and Alzheimer’s disease: implications for sequence of pathological events in Alzheimer’s disease. Brain 132, 1355–1365 (2009).
Luk, K. C. et al. Pathological α-synuclein transmission initiates Parkinson-like neurodegeneration in nontransgenic mice. Science 338, 949–953 (2012).
Lundmark, K. et al. Transmissibility of systemic amyloidosis by a prion-like mechanism. Proc. Natl Acad. Sci. USA 99, 6979–6984 (2002).
Burns, T. C., Li, M. D., Mehta, S., Awad, A. J. & Morgan, A. A. Mouse models rarely mimic the transcriptome of human neurodegenerative diseases: A systematic bioinformatics-based critique of preclinical models. Eur. J. Pharmacol. 759, 101–117 (2015).
Zanusso, G., Monaco, S., Pocchiari, M. & Caughey, B. Advanced tests for early and accurate diagnosis of Creutzfeldt-Jakob disease. Nat. Rev. Neurol. 12, 325–333 (2016).
Edgeworth, J. A. et al. Detection of prion infection in variant Creutzfeldt-Jakob disease: a blood-based assay. Lancet 377, 487–493 (2011).
Jackson, G. S. et al. A highly specific blood test for vCJD. Blood 123, 452–453 (2014).
Saá, P., Castilla, J. & Soto, C. Presymptomatic detection of prions in blood. Science 313, 92–94 (2006).
Colby, D. W. et al. Prion detection by an amyloid seeding assay. Proc. Natl Acad. Sci. USA 104, 20914–20919 (2007).
Atarashi, R. et al. Simplified ultrasensitive prion detection by recombinant PrP conversion with shaking. Nat. Methods 5, 211–212 (2008).
Atarashi, R. et al. Ultrasensitive human prion detection in cerebrospinal fluid by real-time quaking-induced conversion. Nat. Med. 17, 175–178 (2011).
Orrú, C. D. et al. Rapid and sensitive RT-QuIC detection of human Creutzfeldt-Jakob disease using cerebrospinal fluid. mBio 6, e02451–14 (2015).
Concha-Marambio, L. et al. Detection of prions in blood from patients with variant Creutzfeldt-Jakob disease. Sci. Transl Med. 8, 370ra183 (2016).
Bougard, D. et al. Detection of prions in the plasma of presymptomatic and symptomatic patients with variant Creutzfeldt-Jakob disease. Sci. Transl Med. 8, 370ra182 (2016).
Ito, D., Hatano, M. & Suzuki, N. RNA binding proteins and the pathological cascade in ALS/FTD neurodegeneration. Sci. Transl Med. 9, eaah5436 (2017).
Jackson, W. S. Selective vulnerability to neurodegenerative disease: the curious case of Prion Protein. Dis. Model. Mech. 7, 21–29 (2014).
Pettersen, E. F. et al. UCSF Chimera — a visualization system for exploratory research and analysis. J. Comput. Chem. 25, 1605–1612 (2004).
Aguzzi, A., Baumann, F. & Bremer, J. The prion’s elusive reason for being. Annu. Rev. Neurosci. 31, 439–477 (2008).
Acknowledgements
C.S. is the recipient of a Marie Curie Individual Fellowship. A.A. is the recipient of an advanced grant of the European Research Council and grants from the Swiss National Research Foundation, the Clinical Research Priority Programs ‘Small RNAs’ and ‘Human Haemato-Lymphatic Diseases’ of the University of Zurich and SystemsX.ch. Molecular graphics and analyses were performed with the University of California, San Francisco (UCSF) Chimaera package. Chimaera is developed by the Resource for Biocomputing, Visualization and Informatics at UCSF (supported by NIGMS P41-GM103311).
Reviewer information
Nature Reviews Genetics thanks E. Biasini, C. Soto and the other, anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
Both authors contributed to researching, discussing, writing and editing this Review.
Corresponding author
Ethics declarations
Competing interests
Adriano Aguzzi is a founder and director of Mabylon Inc., a company devoted to the development of human antibodies for treating intractable diseases, including neurodegeneration. The authors are not aware of any other affiliations, memberships, funding or financial holdings that might be perceived as affecting the objectivity of this Review.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Prion diseases
-
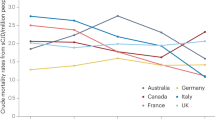
(PrDs). A group of diseases caused by an infectious protein, which includes genetic, acquired and sporadic forms. PrDs have an overall incidence of one to two cases per million individuals per year.
- Prion
-
The agent causing transmissible spongiform encephalopathies. As originally defined, the term does not have structural implications other than that a protein is an essential component. Although it is now generally accepted that the prion consists largely of the pathological aggregate of the prion protein, PrPSc, prions are defined as a biological activity rather than a physical entity. Hence, they can be measured by activity assays rather than by quantitating PrPSc.
- Aggregates
-
In the context of this Review, the term ‘aggregate’ is used to denote the coalescence of misfolded proteins into highly ordered structures, typically resulting in the formation of fibrils.
- Protein misfolding disorders
-
(PMDs). Disorders that are characterized by protein aggregates, which induce neurodegeneration if present in the brain.
- Propagon
-
The minimal propagating unit of a misfolded protein, defined by its capacity to self-replicate in vitro and/or in vivo. A propagon that can transmit from a host individual to another individual is called a prion.
- Prionoids
-
Protein aggregates that can propagate and spread between cells but for which transmissibility between individuals has not yet been demonstrated.
- Polymorphisms
-
Any sites in the DNA sequence that are present in the general population in more than one state.
- Penetrance
-
The percentage of individuals with a mutation who exhibit clinical symptoms. Most PRNP mutations are highly penetrant, meaning that most individuals with PRNP mutations develop prion disease.
- Prion strains
-
Entities associated with distinct biochemical and neuropathological profiles, translating into a spectrum of incubation periods and clinical signs. Crucially, strain-specific traits are stable across serial transmission between isogenic hosts, indicating that they are encoded by the prion itself. Distinct structural assemblies of chemically identical pathological aggregates of the prion protein, PrPSc, are thought to underlie strain-ness.
- Phase demixing
-
Process of membrane-less compartmentalization. Spontaneous demixing of two coexisting phases is driven by intermolecular interactions, a propensity that seems to be particularly high for proteins with low-complexity domains.
- Excitotoxicity
-
Neuronal overstimulation caused by increased levels of the excitatory neurotransmitter glutamate leading to calcium overload and mitochondrial dysfunction and ultimately to neuronal cell death and memory loss.
- Parabiosis
-
Surgical technique to anatomically connect two individuals. The shared circulatory system between the individuals allows specific factors to be assessed for their involvement in regulating physiological functions, behaviour and disease pathogenesis.
Rights and permissions
About this article
Cite this article
Scheckel, C., Aguzzi, A. Prions, prionoids and protein misfolding disorders. Nat Rev Genet 19, 405–418 (2018). https://doi.org/10.1038/s41576-018-0011-4
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41576-018-0011-4
This article is cited by
-
Amyloid aggregates induced by the p53-R280T mutation lead to loss of p53 function in nasopharyngeal carcinoma
Cell Death & Disease (2024)
-
Decoding the Cellular Trafficking of Prion-like Proteins in Neurodegenerative Diseases
Neuroscience Bulletin (2024)
-
Excess PrPC inhibits muscle cell differentiation via miRNA-enhanced liquid–liquid phase separation implicated in myopathy
Nature Communications (2023)
-
Mechanisms and pathology of protein misfolding and aggregation
Nature Reviews Molecular Cell Biology (2023)
-
Bi-Directional Relationship Between Autophagy and Inflammasomes in Neurodegenerative Disorders
Cellular and Molecular Neurobiology (2023)