Abstract
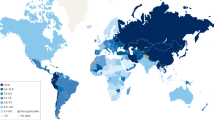
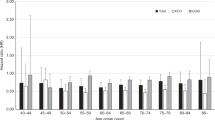
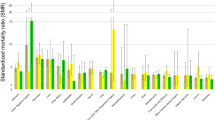
Globally, gastrointestinal cancers represent more than one-fourth of all cancer incidence and one-third of cancer-related mortality. Although there has been much progress in screening colorectal cancer, the prognosis of other gastrointestinal cancers tends to be poor. The highest burden of gastrointestinal cancers, including stomach, liver, oesophageal and gallbladder cancers, was observed in regions in East Asia. The increasing burden of gastrointestinal cancers in East Asian regions is related to population growth, ageing and the westernization of lifestyle habits in this region. Furthermore, the rising incidence of young-onset colorectal cancer is an emerging trend in East Asia. This Review provides a comprehensive and updated summary of the epidemiology of gastrointestinal cancers in East Asia, with emphasis on comparing their epidemiology in East Asia with that in Western regions, and highlights the major risk factors and implications for prevention. Overall, to optimally reduce the disease burden incurred by gastrointestinal cancers in East Asian regions, a concerted effort will be needed to modify unhealthy lifestyles, promote vaccination against the hepatitis virus, control Helicobacter pylori, liver fluke and hepatitis virus infections, increase the uptake rate of colorectal cancer screening, enhance detection of early cancers and their precursors, and improve cancer survivorship through an organized rehabilitation programme.
Key points
-
There is a substantial burden of gastrointestinal cancers in East Asia, with the highest incidence observed in colorectal and stomach cancer and the highest mortality in liver and stomach cancer.
-
Compared with Western regions, East Asia has a higher burden of stomach, liver, oesophageal and gallbladder cancer, but the burden of colorectal and pancreatic cancer is increasing.
-
There is an increasing trend in young-onset colorectal, pancreatic and gallbladder cancer in East Asia attributed to the bigger increase in risk factors among the younger population.
-
Common modifiable risk factors for gastrointestinal cancers in East Asia include smoking, alcohol intake, diet, sedentary lifestyle, obesity and metabolic diseases.
-
East Asian regions have a higher prevalence of Helicobacter pylori, liver fluke, and hepatitis B and C virus infections, hot beverage consumption and biliary cyst development, which might have increased the risk of gastrointestinal cancers.
-
Key preventive strategies for gastrointestinal cancers in the East Asian population include lifestyle modifications, hepatitis vaccination, H. pylori infection control, cancer screening, early diagnosis and improving cancer survivorship.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The geographical definition of the regions follows the rules as defined by the United Nations (https://unstats.un.org/sdgs/indicators/regional-groups). Data were retrieved from international publicly available databases such as GLOBOCAN 2020 and GBD 2019 and are available upon request. Literature regarding the epidemiology of colorectal cancer, stomach cancer, liver cancer, oesophageal cancer, pancreatic cancer and gallbladder cancer in East Asian regions were comprehensively reviewed.
References
Arnold, M. et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 159, 335–349.e15 (2020).
Allemani, C. et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 391, 1023–1075 (2018).
Arnold, M. et al. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995–2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol. 20, 1493–1505 (2019).
Huang, J. et al. Worldwide burden of, risk factors for, and trends in pancreatic cancer. Gastroenterology 160, 744–754 (2021).
Huang, J. et al. Worldwide distribution, associated factors, and trends of gallbladder cancer: a global country-level analysis. Cancer Lett. 521, 238–251 (2021).
Pourhoseingholi, M. A., Vahedi, M. & Baghestani, A. R. Burden of gastrointestinal cancer in Asia; an overview. Gastroenterol. Hepatol. Bed Bench 8, 19–27 (2015).
International Agency for Research on Cancer. Cancer tomorrow. The Global Cancer Observatory https://gco.iarc.fr/tomorrow (2020).
Xie, Y., Shi, L., He, X. & Luo, Y. Gastrointestinal cancers in China, the USA, and Europe. Gastroenterol. Rep. 9, 91–104 (2021).
United Nations. World population ageing. United Nations https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Highlights.pdf (2017).
Ezzati, M. & Riboli, E. Behavioral and dietary risk factors for noncommunicable diseases. N. Engl. J. Med. 369, 954–964 (2013).
Akimoto, N. et al. Rising incidence of early-onset colorectal cancer-a call to action. Nat. Rev. Clin. Oncol. 18, 230–243 (2021).
Wong, M. C. S. et al. Differences in incidence and mortality trends of colorectal cancer worldwide based on sex, age, and anatomic location. Clin. Gastroenterol. Hepatol. 19, 955–966.e61 (2021).
Wolf, A. M. D. et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J. Clin. 68, 250–281 (2018).
US Preventive Services Task Force. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA 325, 1965–1977 (2021).
Sung, J. J. Y. et al. Increasing trend in young-onset colorectal cancer in Asia: more cancers in men and more rectal cancers. Am. J. Gastroenterol. 114, 322–329 (2019).
Patel, S. G., Karlitz, J. J., Yen, T., Lieu, C. H. & Boland, C. R. The rising tide of early-onset colorectal cancer: a comprehensive review of epidemiology, clinical features, biology, risk factors, prevention, and early detection. Lancet Gastroenterol. Hepatol. 7, 262–274 (2022).
International Agency for Research on Cancer. Cancer today. The Global Cancer Observatory https://gco.iarc.fr/today/home (2020).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Sunkara, V. & Hébert, J. R. The colorectal cancer mortality-to-incidence ratio as an indicator of global cancer screening and care. Cancer 121, 1563–1569 (2015).
Adams, S. A. et al. Decreased cancer mortality-to-incidence ratios with increased accessibility of federally qualified health centers. J. Community Health 40, 633–641 (2015).
Choi, E. et al. Cancer mortality-to-incidence ratio as an indicator of cancer management outcomes in Organization for Economic Cooperation and Development countries. Epidemiol. Health 39, e2017006 (2017).
Institute for Health Metrics and Evaluation. GBD results. Institute for Health Metrics and Evaluation https://vizhub.healthdata.org/gbd-results/ (2021).
GBD 2019 Colorectal Cancer Collaborators. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 7, 627–647 (2022).
GBD 2017 Pancreatic Cancer Collaborators. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 4, 934–947 (2019).
Popkin, B. M., Adair, L. S. & Ng, S. W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 70, 3–21 (2012).
Faruque, S. et al. The dose makes the poison: sugar and obesity in the United States–a review. Pol. J. Food Nutr. Sci. 69, 219–233 (2019).
World Health Organization. Obesity and overweight. WHO https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (2020).
Mills, K. T. et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 134, 441–450 (2016).
Navarro, M., Nicolas, A., Ferrandez, A. & Lanas, A. Colorectal cancer population screening programs worldwide in 2016: an update. World J. Gastroenterol. 23, 3632–3642 (2017).
Levin, T. R. et al. Effects of organized colorectal cancer screening on cancer incidence and mortality in a large community-based population. Gastroenterology 155, 1383–1391.e5 (2018).
Siegel, R. L. et al. Colorectal cancer incidence patterns in the United States, 1974–2013. J. Natl Cancer Inst. 109, djw322 (2017).
Murphy, C. C. et al. Decrease in incidence of colorectal cancer among individuals 50 years or older after recommendations for population-based screening. Clin. Gastroenterol. Hepatol. 15, 903–909.e6 (2017).
Gu, M. & Thapa, S. Colorectal cancer in the United States and a review of its heterogeneity among Asian American subgroups. Asia Pac. J. Clin. Oncol. 16, 193–200 (2020).
European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut 67, 789–804 (2018).
Mukewar, S. & Chari, S. T. in The Pancreas: an Integrated Textbook of Basic Science, Medicine, and Surgery 3rd edn (eds Beger, H. G. et al.) 565–572 (Wiley, 2018).
Wu, H. et al. Advances in biomarkers and techniques for pancreatic cancer diagnosis. Cancer Cell Int. 22, 220 (2022).
Huang, J. et al. Disease burden, risk factors, and recent trends of liver cancer: a global country-level analysis. Liver Cancer 10, 330–345 (2021).
Codipilly, D. C. et al. Epidemiology and outcomes of young-onset esophageal adenocarcinoma: an analysis from a population-based database. Cancer Epidemiol. Biomark. Prev. 30, 142–149 (2021).
Huang, J. et al. Global burden, risk factors, and trends of esophageal cancer: an analysis of cancer registries from 48 countries. Cancers (Basel) 13, 141 (2021).
Global Burden of Disease Liver Cancer Collaboration. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the Global Burden of Disease Study 2015. JAMA Oncol. 3, 1683–1691 (2017).
GBD 2017 Oesophageal Cancer Collaborators. The global, regional, and national burden of oesophageal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 5, 582–597 (2020).
Polaris Observatory HCV Collaborators. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol. Hepatol. 2, 161–176 (2017).
Petrick, J. L. & McGlynn, K. A. The changing epidemiology of primary liver cancer. Curr. Epidemiol. Rep. 6, 104–111 (2019).
Wong, M. C. S. et al. The changing epidemiology of liver diseases in the Asia-Pacific region. Nat. Rev. Gastroenterol. Hepatol. 16, 57–73 (2019).
Wong, V. W. et al. Metabolic and adipokine profile of Chinese patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 4, 1154–1161 (2006).
Ong, J. P., Pitts, A. & Younossi, Z. M. Increased overall mortality and liver-related mortality in non-alcoholic fatty liver disease. J. Hepatol. 49, 608–612 (2008).
Wong, V. W. et al. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut 59, 969–974 (2010).
Lin, L. et al. The burden and trends of primary liver cancer caused by specific etiologies from 1990 to 2017 at the global, regional, national, age, and sex level results from the Global Burden of Disease Study 2017. Liver Cancer 9, 563–582 (2020).
Lin, Y., Wang, H. L., Fang, K., Zheng, Y. & Wu, J. International trends in esophageal cancer incidence rates by histological subtype (1990–2012) and prediction of the rates to 2030. Esophagus https://doi.org/10.1007/s10388-022-00927-4 (2022).
Arnold, M., Laversanne, M., Brown, L. M., Devesa, S. S. & Bray, F. Predicting the future burden of esophageal cancer by histological subtype: international trends in incidence up to 2030. Am. J. Gastroenterol. 112, 1247–1255 (2017).
Wang, Q. L., Xie, S. H., Wahlin, K. & Lagergren, J. Global time trends in the incidence of esophageal squamous cell carcinoma. Clin. Epidemiol. 10, 717–728 (2018).
Wong, M. C. S. et al. Global incidence and mortality of oesophageal cancer and their correlation with socioeconomic indicators temporal patterns and trends in 41 countries. Sci. Rep. 8, 4522 (2018).
Wong, M. C. S. et al. Global, regional and time-trend prevalence of central obesity: a systematic review and meta-analysis of 13.2 million subjects. Eur. J. Epidemiol. 35, 673–683 (2020).
Renehan, A. G., Tyson, M., Egger, M., Heller, R. F. & Zwahlen, M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371, 569–578 (2008).
Steffen, A. et al. Anthropometry and esophageal cancer risk in the European Prospective Investigation into Cancer and Nutrition. Cancer Epidemiol. Biomark. Prev. 18, 2079–2089 (2009).
Lahmann, P. H., Pandeya, N., Webb, P. M., Green, A. C. & Whiteman, D. C. Body mass index, long-term weight change, and esophageal squamous cell carcinoma: is the inverse association modified by smoking status? Cancer 118, 1901–1909 (2012).
Wong, M. C. et al. Worldwide incidence and prevalence of metabolic syndrome: a systematic review and meta-analysis of 14.6 million individuals [abstract TU1007]. Gastroenterology 158(6 Suppl. 1), S-1003 (2020).
Lagergren, J., Bergström, R., Lindgren, A. & Nyrén, O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N. Engl. J. Med. 340, 825–831 (1999).
Lagergren, J. Influence of obesity on the risk of esophageal disorders. Nat. Rev. Gastroenterol. Hepatol. 8, 340–347 (2011).
El-Serag, H. B., Sweet, S., Winchester, C. C. & Dent, J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 63, 871–880 (2014).
Wong, M. C. S. et al. Global incidence and mortality of gastric cancer, 1980–2018. JAMA Netw. Open 4, e2118457 (2021).
GBD 2017 Stomach Cancer Collaborators. The global, regional, and national burden of stomach cancer in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 5, 42–54 (2020).
Ouyang, G. et al. The global, regional, and national burden of gallbladder and biliary tract cancer and its attributable risk factors in 195 countries and territories, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study 2017. Cancer 127, 2238–2250 (2021).
Fock, K. M. & Ang, T. L. Epidemiology of Helicobacter pylori infection and gastric cancer in Asia. J. Gastroenterol. Hepatol. 25, 479–486 (2010).
Hipgrave, D. B., Chang, S., Li, X. & Wu, Y. Salt and sodium intake in China. JAMA 315, 703–705 (2016).
Inoue, M. Changing epidemiology of Helicobacter pylori in Japan. Gastric Cancer 20, 3–7 (2017).
Shimazu, T. et al. Association of vegetable and fruit intake with gastric cancer risk among Japanese: a pooled analysis of four cohort studies. Ann. Oncol. 25, 1228–1233 (2014).
Randi, G. et al. Epidemiology of biliary tract cancers: an update. Ann. Oncol. 20, 146–159 (2009).
Legorreta, A. P., Silber, J. H., Costantino, G. N., Kobylinski, R. W. & Zatz, S. L. Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy. JAMA 270, 1429–1432 (1993).
Huang, X., Feng, Y. & Huang, Z. Complications of laparoscopic cholecystectomy in China: an analysis of 39,238 cases. Chin. Med. J. 110, 704–706 (1997).
Mohandas, K. M. & Patil, P. S. Cholecystectomy for asymptomatic gallstones can reduce gall bladder cancer mortality in northern Indian women. Indian. J. Gastroenterol. 25, 147–151 (2006).
Torre, L. A., Siegel, R. L., Islami, F., Bray, F. & Jemal, A. Worldwide burden of and trends in mortality from gallbladder and other biliary tract cancers. Clin. Gastroenterol. Hepatol. 16, 427–437 (2018).
Liao, J. K. Safety and efficacy of statins in Asians. Am. J. Cardiol. 99, 410–414 (2007).
Bodmer, M., Brauchli, Y. B., Krähenbühl, S., Jick, S. S. & Meier, C. R. Statin use and risk of gallstone disease followed by cholecystectomy. JAMA 302, 2001–2007 (2009).
Feletto, E. et al. Trends in colon and rectal cancer incidence in Australia from 1982 to 2014: analysis of data on over 375,000 cases. Cancer Epidemiol. Biomark. Prev. 28, 83–90 (2019).
Patel, P. & De, P. Trends in colorectal cancer incidence and related lifestyle risk factors in 15–49-year-olds in Canada, 1969–2010. Cancer Epidemiol. 42, 90–100 (2016).
Larsen, I. K. & Bray, F. Trends in colorectal cancer incidence in Norway 1962-2006: an interpretation of the temporal patterns by anatomic subsite. Int. J. Cancer 126, 721–732 (2010).
di Martino, E. et al. Incidence trends for twelve cancers in younger adults–a rapid review. Br. J. Cancer 126, 1374–1386 (2022).
You, Y. N., Lee, L. D., Deschner, B. W. & Shibata, D. Colorectal cancer in the adolescent and young adult population. JCO Oncol. Pract. 16, 19–27 (2020).
Vuik, F. E. R. et al. Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut 68, 1820–1826 (2019).
Exarchakou, A., Donaldson, L. J., Girardi, F. & Coleman, M. P. Colorectal cancer incidence among young adults in England: trends by anatomical sub-site and deprivation. PLoS ONE 14, e0225547 (2019).
Hur, H., Oh, C. M., Won, Y. J., Oh, J. H. & Kim, N. K. Characteristics and survival of Korean patients with colorectal cancer based on data from the Korea Central Cancer Registry Data. Ann. Coloproctol. 34, 212–221 (2018).
Global Burden of Disease 2019 Cancer Collaboration. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 8, 420–444 (2022).
Alazmi, W. M., Siddique, I., Alateeqi, N. & Al-Nakib, B. Prevalence of Helicobacter pylori infection among new outpatients with dyspepsia in Kuwait. BMC Gastroenterol. 10, 14 (2010).
Yim, J. Y. et al. Seroprevalence of Helicobacter pylori in South Korea. Helicobacter 12, 333–340 (2007).
Pennathur, A., Gibson, M. K., Jobe, B. A. & Luketich, J. D. Oesophageal carcinoma. Lancet 381, 400–412 (2013).
Kingham, T. P. et al. Treatment of cancer in sub-Saharan Africa. Lancet Oncol. 14, e158–e167 (2013).
Barton, M. B., Frommer, M. & Shafiq, J. Role of radiotherapy in cancer control in low-income and middle-income countries. Lancet Oncol. 7, 584–595 (2006).
Goss, P. E. et al. Planning cancer control in Latin America and the Caribbean. Lancet Oncol. 14, 391–436 (2013).
Gini, A. et al. Impact of colorectal cancer screening on cancer-specific mortality in Europe: a systematic review. Eur. J. Cancer 127, 224–235 (2020).
Schreuders, E. H. et al. Colorectal cancer screening: a global overview of existing programmes. Gut 64, 1637 (2015).
Araghi, M. et al. Global trends in colorectal cancer mortality: projections to the year 2035. Int. J. Cancer 144, 2992–3000 (2019).
Ranganath, R. & Chu, Q. Global trends in pancreas cancer among Asia-Pacific population. J. Gastrointest. Oncol. 12, S374–S386 (2021).
Dong, E., Duan, L. & Wu, B. U. Racial and ethnic minorities at increased risk for gastric cancer in a regional US population study. Clin. Gastroenterol. Hepatol. 15, 511–517 (2017).
Rawla, P. & Barsouk, A. Epidemiology of gastric cancer: global trends, risk factors and prevention. Prz. Gastroenterol. 14, 26–38 (2019).
Nguyen, M. H. et al. Role of ethnicity in risk for hepatocellular carcinoma in patients with chronic hepatitis C and cirrhosis. Clin. Gastroenterol. Hepatol. 2, 820–824 (2004).
Zhang, G., Mai, R. & Huang, B. ADH1B Arg47His polymorphism is associated with esophageal cancer risk in high-incidence Asian population: evidence from a meta-analysis. PLoS ONE 5, e13679 (2010).
Haggar, F. A. & Boushey, R. P. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin. Colon. Rectal Surg. 22, 191–197 (2009).
Chen, W. et al. Cancer incidence and mortality in China, 2014. Chin. J. Cancer Res. 30, 1–12 (2018).
Tamakoshi, A. et al. Characteristics and prognosis of Japanese colorectal cancer patients: The BioBank Japan Project. J. Epidemiol. 27, S36–S42 (2017).
Jung, K.-W., Won, Y.-J., Kong, H.-J. & Lee, E. S. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res. Treat. 50, 303–316 (2018).
Yuen, M. F., Hou, J. L. & Chutaputti, A. Hepatocellular carcinoma in the Asia pacific region. J. Gastroenterol. Hepatol. 24, 346–353 (2009).
Nguyen, S. P., Bent, S., Chen, Y.-H. & Terdiman, J. P. Gender as a risk factor for advanced neoplasia and colorectal cancer: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 7, 676–681.e3 (2009).
Newcomb, P. A. et al. Estrogen plus progestin use, microsatellite instability, and the risk of colorectal cancer in women. Cancer Res. 67, 7534–7539 (2007).
Rossouw, J. E. et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 288, 321–333 (2002).
Xie, S. H. & Lagergren, J. The male predominance in esophageal adenocarcinoma. Clin. Gastroenterol. Hepatol. 14, 338–347.e1 (2016).
Xie, S. H. et al. Circulating sex hormone levels and risk of esophageal adenocarcinoma in a prospective study in men. Am. J. Gastroenterol. 115, 216–223 (2020).
Chandanos, E. & Lagergren, J. Oestrogen and the enigmatic male predominance of gastric cancer. Eur. J. Cancer 44, 2397–2403 (2008).
Derakhshan, M. H. et al. Oesophageal and gastric intestinal-type adenocarcinomas show the same male predominance due to a 17 year delayed development in females. Gut 58, 16–23 (2009).
Piehler, J. M. & Crichlow, R. W. Primary carcinoma of the gallbladder. Surg. Gynecol. Obstet. 147, 929–942 (1978).
Bari, O. D. et al. Cholesterol cholelithiasis in pregnant women: pathogenesis, prevention and treatment. Ann. Hepatol. 13, 728–745 (2014).
Wistuba, I. I. & Gazdar, A. F. Gallbladder cancer: lessons from a rare tumour. Nat. Rev. Cancer 4, 695–706 (2004).
Ng, S. C. et al. Increased risk of advanced neoplasms among asymptomatic siblings of patients with colorectal cancer. Gastroenterology 144, 544–550 (2013).
Choi, Y. J. & Kim, N. Gastric cancer and family history. Korean J. Intern. Med. 31, 1042–1053 (2016).
Liu, X. et al. Family history of liver cancer may modify the association between HBV infection and liver cancer in a Chinese population. Liver Int. 39, 1490–1503 (2019).
Chen, T. et al. Family history of esophageal cancer increases the risk of esophageal squamous cell carcinoma. Sci. Rep. 5, 16038 (2015).
Wong, M. C. S. et al. Lower relative contribution of positive family history to colorectal cancer risk with increasing age: a systematic review and meta-analysis of 9.28 million individuals. Am. J. Gastroenterol. 113, 1819–1827 (2018).
Wong, M. C. et al. Risk of colorectal neoplasia in individuals with self-reported family history: a prospective colonoscopy study from 16 Asia-Pacific regions. Am. J. Gastroenterol. 111, 1621–1629 (2016).
Pourhoseingholi, M. A., Ashtari, S., Hajizadeh, N., Fazeli, Z. & Zali, M. R. Systematic review of pancreatic cancer epidemiology in Asia-Pacific region: major patterns in GLOBACON 2012. Gastroenterol. Hepatol. Bed Bench 10, 245–257 (2017).
Shi, C., Hruban, R. H. & Klein, A. P. Familial pancreatic cancer. Arch. Pathol. Lab. Med. 133, 365–374 (2009).
Randi, G., Franceschi, S. & La Vecchia, C. Gallbladder cancer worldwide: geographical distribution and risk factors. Int. J. Cancer 118, 1591–1602 (2006).
Gu, M. J. et al. Attributable causes of colorectal cancer in China. BMC Cancer 18, 38 (2018).
Tsong, W. H. et al. Cigarettes and alcohol in relation to colorectal cancer: the Singapore Chinese health study. Br. J. Cancer 96, 821–827 (2007).
Shimizu, N. et al. Height, weight and alcohol consumption in relation to the risk of colorectal cancer in Japan: a prospective study. Br. J. Cancer 88, 1038–1043 (2003).
Koizumi, Y. et al. Cigarette smoking and the risk of gastric cancer: a pooled analysis of two prospective studies in Japan. Int. J. Cancer 112, 1049–1055 (2004).
Koh, W. P. et al. Smoking as an independent risk factor for hepatocellular carcinoma: the Singapore Chinese Health Study. Br. J. Cancer 105, 1430–1435 (2011).
Yang, X. et al. Smoking and alcohol drinking in relation to the risk of esophageal squamous cell carcinoma: a population-based case-control study in China. Sci. Rep. 7, 17249 (2017).
Ansary-Moghaddam, A. et al. The effect of modifiable risk factors on pancreatic cancer mortality in populations of the Asia-Pacific region. Cancer Epidemiol. Biomark. Prev. 15, 2435–2440 (2006).
Lugo, A., Peveri, G. & Gallus, S. Should we consider gallbladder cancer a new smoking-related cancer? A comprehensive meta-analysis focused on dose-response relationships. Int. J. Cancer 146, 3304–3311 (2020).
Naing, C., Lai, P. K. & Mak, J. W. Immediately modifiable risk factors attributable to colorectal cancer in Malaysia. BMC Public Health 17, 637 (2017).
Choi, Y. J. et al. The relationship between drinking alcohol and esophageal, gastric or colorectal cancer: a nationwide population-based cohort study of South Korea. PLoS ONE https://doi.org/10.1371/journal.pone.0185778 (2017).
Mizoue, T. et al. Alcohol drinking and colorectal cancer in Japanese: a pooled analysis of results from five cohort studies. Am. J. Epidemiol. 167, 1397–1406 (2008).
Li, Y. et al. Alcohol consumption and risk of gastric cancer: the Japan Collaborative Cohort Study. J. Epidemiol. 31, 30–36 (2021).
Yokoyama, A. & Omori, T. Genetic polymorphisms of alcohol and aldehyde dehydrogenases and risk for esophageal and head and neck cancers. Jpn. J. Clin. Oncol. 33, 111–121 (2003).
Yokoyama, A. et al. Alcohol-related cancers and aldehyde dehydrogenase-2 in Japanese alcoholics. Carcinogenesis 19, 1383–1387 (1998).
Im, P. K. et al. Alcohol drinking and risks of total and site-specific cancers in China: a 10-year prospective study of 0.5 million adults. Int. J. Cancer 149, 522–534 (2021).
Shan, Y.-S. et al. No association between alcohol consumption and pancreatic cancer even among individuals genetically susceptible to the carcinogenicity of alcohol. Sci. Rep. 11, 14567 (2021).
Azeem, S. et al. Diet and colorectal cancer risk in Asia – a systematic review. Asian Pac. J. Cancer Prev. 16, 5389–5396 (2015).
Moore, M. A. Diverse influences of dietary factors on cancer in Asia. Asian Pac. J. Cancer Prev. 10, 981–986 (2009).
Chiu, B. C. H. et al. Dietary factors and risk of colon cancer in Shanghai, China. Cancer Epidemiol. Biomark. Prev. 12, 201–208 (2003).
Park, Y., Lee, J., Oh, J. H., Shin, A. & Kim, J. Dietary patterns and colorectal cancer risk in a Korean population: a case-control study. Medicine 95, e3759 (2016).
Lin, S. H., Li, Y. H., Leung, K., Huang, C. Y. & Wang, X. R. Salt processed food and gastric cancer in a Chinese population. Asian Pac. J. Cancer Prev. 15, 5293–5298 (2014).
Liu, Y. & Wu, F. Global burden of aflatoxin-induced hepatocellular carcinoma: a risk assessment. Env. Health Perspect. 118, 818–824 (2010).
Okada, E. et al. Dietary patterns and risk of esophageal cancer mortality: the Japan Collaborative Cohort Study. Nutr. Cancer 68, 1001–1009 (2016).
Nelson, S. M. et al. Diet and biliary tract cancer risk in Shanghai, China. PLoS ONE 12, e0173935 (2017).
Zheng, J. et al. Dietary patterns and risk of pancreatic cancer: a systematic review. Nutr. Rev. 75, 883–908 (2017).
Liu, S.-Z. et al. Dietary factors and risk of pancreatic cancer: a multi-centre case-control study in China. Asian Pac. J. Cancer Prev. 15, 7947–7950 (2014).
Arafa, A. et al. Dairy intake and the risk of pancreatic cancer: the Japan Collaborative Cohort Study (JACC Study) and meta-analysis of prospective cohort studies. Br. J. Nutr. https://doi.org/10.1017/S0007114521004232 (2021).
Mueller, N. T. et al. Soft drink and juice consumption and risk of pancreatic cancer: the Singapore Chinese Health Study. Cancer Epidemiol. Biomark. Prev. 19, 447–455 (2010).
Pham, N. M. et al. Physical activity and colorectal cancer risk: an evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn. J. Clin. Oncol. 42, 2–13 (2012).
Gunathilake, M. N. et al. Physical activity and gastric cancer risk in patients with and without Helicobacter pylori infection in a Korean population: a hospital-based case-control study. Cancers https://doi.org/10.3390/cancers10100369 (2018).
Inoue, M. et al. Daily total physical activity level and total cancer risk in men and women: results from a large-scale population-based cohort study in Japan. Am. J. Epidemiol. 168, 391–403 (2008).
Etemadi, A. et al. Large body size and sedentary lifestyle during childhood and early adulthood and esophageal squamous cell carcinoma in a high-risk population. Ann. Oncol. 23, 1593–1600 (2012).
Wu, L. et al. Physical activity and pancreatic cancer risk among urban Chinese: results from two prospective cohort studies. Cancer Epidemiol. Biomark. Prev. 27, 479–487 (2018).
Pang, Y. et al. Association of physical activity with risk of hepatobiliary diseases in China: a prospective cohort study of 0.5 million people. Br. J. Sports Med. 55, 1024–1033 (2021).
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363, 157–163 (2004).
Matsuo, K. et al. Association between body mass index and the colorectal cancer risk in Japan: pooled analysis of population-based cohort studies in Japan. Ann. Oncol. 23, 479–490 (2012).
Mafiana, R. N. et al. Association between dietary and lifestyle indices and colorectal cancer in Oman: a case-control study. Asian Pac. J. Cancer Prev. 19, 3117–3122 (2018).
Kim, H. J. et al. Relationship between body mass index and the risk of early gastric cancer and dysplasia regardless of Helicobacter pylori infection. Gastric Cancer 18, 762–773 (2015).
Sohn, W. et al. Obesity and the risk of primary liver cancer: a systematic review and meta-analysis. Clin. Mol. Hepatol. 27, 157–174 (2021).
Cho, J. H. et al. Abdominal obesity increases risk for esophageal cancer: a nationwide population-based cohort study of South Korea. J. Gastroenterol. 55, 307–316 (2020).
Hsing, A. W. et al. Body size and the risk of biliary tract cancer: a population-based study in China. Br. J. Cancer 99, 811–815 (2008).
Shin, C. M. et al. Association among obesity, metabolic health, and the risk for colorectal cancer in the general population in Korea using the National Health Insurance Service–National Sample Cohort. Dis. Colon Rectum 60, 1192–1200 (2017).
Li, F., Du, H., Li, S. & Liu, J. The association between metabolic syndrome and gastric cancer in Chinese. Front. Oncol. https://doi.org/10.3389/fonc.2018.00326 (2018).
Yu, M.-W. et al. Influence of metabolic risk factors on risk of hepatocellular carcinoma and liver-related death in men with chronic hepatitis B: a large cohort study. Gastroenterology 153, 1006–1017.e5 (2017).
Zhang, J., Wu, H. & Wang, R. Metabolic syndrome and esophageal cancer risk: a systematic review and meta-analysis. Diabetol. Metab. Syndr. 13, 8 (2021).
Ko, S. et al. Metabolic risk profile and cancer in Korean men and women. J. Prev. Med. Public. Health 49, 143–152 (2016).
[No authors listed] Schistosomes, liver flukes and Helicobacter pylori. IARC Monogr. Eval. Carcinog. Risks Hum. 61, 1–241 (1994).
Eslick, G. D., Lim, L. L.-Y., Byles, J. E., Xia, H. H.-X. & Talley, N. J. Association of Helicobacter pylori infection with gastric carcinoma: a meta-analysis. Am. J. Gastroenterol. 94, 2373–2379 (1999).
Yang, L. et al. The relative and attributable risks of cardia and non-cardia gastric cancer associated with Helicobacter pylori infection in China: a case-cohort study. Lancet Public Health 6, e888–e896 (2021).
Ren, S. et al. Prevalence of Helicobacter pylori infection in China: a systematic review and meta-analysis. J. Gastroenterol. Hepatol. 37, 464–470 (2022).
Fujisawa, T., Kumagai, T., Akamatsu, T., Kiyosawa, K. & Matsunaga, Y. Changes in seroepidemiological pattern of Helicobacter pylori and hepatitis A virus over the last 20 years in Japan. Am. J. Gastroenterol. 94, 2094–2099 (1999).
Hooi, J. K. Y. et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology 153, 420–429 (2017).
Mbulaiteye, S. M., Hisada, M. & El-Omar, E. M. Helicobacter pylori associated global gastric cancer burden. Front. Biosci. 14, 1490–1504 (2009).
Miwa, H., Go, M. F. & Sato, N. H. pylori and gastric cancer: the Asian enigma. Am. J. Gastroenterol. 97, 1106–1112 (2002).
Zuo, Y. et al. Association between Helicobacter pylori infection and the risk of colorectal cancer: a systematic review and meta-analysis. Medicine 99, e21832 (2020).
Hong, S. T. & Fang, Y. Clonorchis sinensis and clonorchiasis, an update. Parasitol. Int. 61, 17–24 (2012).
Rim, H. J. Clonorchiasis: an update. J. Helminthol. 79, 269–281 (2005).
Na, B. K., Pak, J. H. & Hong, S. J. Clonorchis sinensis and clonorchiasis. Acta Trop. 203, 105309 (2020).
Bouvard, V. et al. A review of human carcinogens – Part B: biological agents. Lancet Oncol. 10, 321–322 (2009).
Qian, M. B. et al. Familial assimilation in transmission of raw-freshwater fish-eating practice leading to clonorchiasis. PLoS Negl. Trop. Dis. 14, e0008263 (2020).
Qian, M.-B. et al. Effectiveness of health education in improving knowledge, practice and belief related to clonorchiasis in children. Acta Tropica 207, 105436 (2020).
Qian, M. B., Chen, Y. D., Liang, S., Yang, G. J. & Zhou, X. N. The global epidemiology of clonorchiasis and its relation with cholangiocarcinoma. Infect. Dis. Poverty 1, 4 (2012).
Shin, H. R. et al. Descriptive epidemiology of cholangiocarcinoma and clonorchiasis in Korea. J. Korean Med. Sci. 25, 1011–1016 (2010).
Qian, M.-B. & Zhou, X.-N. Human liver flukes in China and ASEAN: time to fight together. PLoS Negl. Trop. Dis. 13, e0007214 (2019).
de Martel, C., Maucort-Boulch, D., Plummer, M. & Franceschi, S. World-wide relative contribution of hepatitis B and C viruses in hepatocellular carcinoma. Hepatology 62, 1190–1200 (2015).
World Health Organization. Global hepatitis report, 2017. WHO http://apps.who.int/iris/bitstream/10665/255017/1/WHO-HIV-2017.06-eng.pdf (2017).
Ott, J. J., Stevens, G. A., Groeger, J. & Wiersma, S. T. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine 30, 2212–2219 (2012).
Petruzziello, A., Marigliano, S., Loquercio, G., Cozzolino, A. & Cacciapuoti, C. Global epidemiology of hepatitis C virus infection: an up-date of the distribution and circulation of hepatitis C virus genotypes. World J. Gastroenterol. 22, 7824–7840 (2016).
Lin, C. L. & Kao, J. H. Hepatitis B virus genotypes and variants. Cold Spring Harb. Perspect. Med. 5, a021436 (2015).
Chen, Y. et al. Consumption of hot beverages and foods and the risk of esophageal cancer: a meta-analysis of observational studies. BMC Cancer 15, 449–449 (2015).
Hundal, R. & Shaffer, E. A. Gallbladder cancer: epidemiology and outcome. Clin. Epidemiol. 6, 99–109 (2014).
Singham, J., Schaeffer, D., Yoshida, E. & Scudamore, C. Choledochal cysts: analysis of disease pattern and optimal treatment in adult and paediatric patients. HPB 9, 383–387 (2007).
Stinton, L. M. & Shaffer, E. A. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver 6, 172–187 (2012).
Rawla, P., Sunkara, T., Thandra, K. C. & Barsouk, A. Epidemiology of gallbladder cancer. Clin. Exp. Hepatol. 5, 93–102 (2019).
Jabłońska, B. Biliary cysts: etiology, diagnosis and management. World J. Gastroenterol. 18, 4801–4810 (2012).
Kamisawa, T. et al. Japanese clinical practice guidelines for pancreaticobiliary maljunction. J. Gastroenterol. 47, 731–759 (2012).
Roa, I. et al. Clinicopathological features of gallbladder polyps and adenomas [Spanish]. Rev. Med. Chil. 132, 673–679 (2004).
Luu, H. N. et al. Quality diet index and risk of pancreatic cancer: findings from the Singapore Chinese Health Study. Cancer Epidemiol. Biomark. Prev. 30, 2068–2078 (2021).
Steck, S. E. & Murphy, E. A. Dietary patterns and cancer risk. Nat. Rev. Cancer 20, 125–138 (2020).
Yun, Y. H. et al. Dietary preference, physical activity, and cancer risk in men: National Health Insurance Corporation Study. BMC Cancer 8, 366 (2008).
Wang, J. et al. Physically active individuals have a 23% lower risk of any colorectal neoplasia and a 27% lower risk of advanced colorectal neoplasia than their non-active counterparts: systematic review and meta-analysis of observational studies. Br. J. Sports Med. 54, 582 (2020).
Li, L., Assanangkornchai, S., Duo, L., McNeil, E. & Li, J. Risk behaviors, prevalence of HIV and hepatitis C virus infection and population size of current injection drug users in a China-Myanmar border city: results from a Respondent-Driven Sampling Survey in 2012. PLoS ONE 9, e106899 (2014).
Strosnider, H. et al. Workgroup report: public health strategies for reducing aflatoxin exposure in developing countries. Env. Health Perspect. 114, 1898–1903 (2006).
Wang, Q.-L., Xie, S.-H., Li, W.-T. & Lagergren, J. Smoking cessation and risk of esophageal cancer by histological type: systematic review and meta-analysis. J. Natl Cancer Inst. 109, djx115 (2017).
United Nations. Transforming our world: the 2030 agenda for sustainable development. United Nations https://sustainabledevelopment.un.org/content/documents/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf (2015).
La Torre, G. et al. Economic evaluation of HBV vaccination: a systematic review of recent publications (2000–2013). Hum. Vaccin. Immunother. 12, 2299–2311 (2016).
Luo, Z., Li, L. & Ruan, B. Impact of the implementation of a vaccination strategy on hepatitis B virus infections in China over a 20-year period. Int. J. Infect. Dis. 16, e82–e88 (2012).
Sandhu, H. S., Roesel, S., Sharifuzzaman, M., Chunsuttiwat, S. & Tohme, R. A. Progress toward hepatitis B control–South-East Asia region, 2016-2019. MMWR Morb. Mortal. Wkly. Rep. 69, 988–992 (2020).
Shan, S., Cui, F. & Jia, J. How to control highly endemic hepatitis B in Asia. Liver Int. 38 (Suppl 1), 122–125 (2018).
Zhu, D. et al. Socioeconomic inequality in hepatitis B vaccination of rural adults in China. Hum. Vaccin. Immunother. 14, 464–470 (2018).
Ayers, J. W., Juon, H.-S., Lee, S. & Park, E. Hepatitis B vaccination prevalence and its predictors among Asian, Pacific Islander, Native American, and multiracial adults in the National Health and Nutrition Examination Survey. J. Immigr. Minor. Health 12, 847–852 (2010).
Beste, L. A., Green, P., Berry, K., Belperio, P. & Ioannou, G. N. Hepatitis C-related hepatocellular carcinoma incidence in the Veterans Health Administration after introduction of direct-acting antivirals. JAMA 324, 1003–1005 (2020).
Chang, L.-J. et al. Factors associated with the refusal of direct-acting antiviral agents for the treatment of hepatitis C in Taiwan. Medicina 58, 121 (2022).
Lee, Y. C. et al. Association between Helicobacter pylori eradication and gastric cancer incidence: a systematic review and meta-analysis. Gastroenterology 150, 1113–1124.e5 (2016).
Yan, L. et al. Effect of Helicobacter pylori eradication on gastric cancer prevention: updated report from a randomized controlled trial with 26.5 years of follow-up. Gastroenterology https://doi.org/10.1053/j.gastro.2022.03.039 (2022).
Tshibangu-Kabamba, E. & Yamaoka, Y. Helicobacter pylori infection and antibiotic resistance–from biology to clinical implications. Nat. Rev. Gastroenterol. Hepatol. 18, 613–629 (2021).
Sung, J. J. et al. Asia Pacific consensus recommendations for colorectal cancer screening. Gut 57, 1166–1176 (2008).
Sung, J. J. Y., Ng, S. C. & Chan, F. K. L. An updated Asia Pacific consensus recommendations on colorectal cancer screening. Gut 64, 121–132 (2015).
Ng, S. C. & Wong, S. H. Colorectal cancer screening in Asia. Br. Med. Bull. 105, 29–42 (2013).
Yeoh, K. G. et al. The Asia-Pacific colorectal screening score: a validated tool that stratifies risk for colorectal advanced neoplasia in asymptomatic Asian subjects. Gut 60, 1236–1241 (2011).
Lee, B. I. et al. Korean guidelines for colorectal cancer screening and polyp detection. J. Korean Soc. Radiol. 66, 385 (2012).
Cancer Expert Working Group on Cancer Prevention and Screening. Recommendations on Prevention and Screening for Colorectal Cancer For Health Professionals. https://www.chp.gov.hk/files/pdf/cewg_crc_professional_hp.pdf (2022).
Huang, J. J. & Huang, J. L. Challenges to the adoption of risk algorithms for colorectal cancer screening programmes: perspectives for future research. Hong. Kong Med. J. 23, 661–663 (2017).
Wong, M. C. et al. A validated tool to predict colorectal neoplasia and inform screening choice for asymptomatic subjects. Gut 63, 1130–1136 (2014).
Sung, J. J. Y. et al. A modified colorectal screening score for prediction of advanced neoplasia: a prospective study of 5744 subjects. J. Gastroenterol. Hepatol. 33, 187–194 (2018).
Hatamian, S., Hadavandsiri, F., Momenimovahed, Z. & Salehiniya, H. Barriers and facilitators of colorectal cancer screening in Asia. Ecancermedicalscience 15, 1285 (2021).
Wong, M. C. S. et al. Association of interactive reminders and automated messages with persistent adherence to colorectal cancer screening: a randomized clinical trial. JAMA Oncol. 3, 1281–1283 (2017).
Wong, M. C. et al. Effectiveness of reminder strategies on cancer screening adherence: a randomised controlled trial. Br. J. Gen. Pract. 68, e604–e611 (2018).
Kim, J. Y. et al. Development and validation of a scoring system for advanced colorectal neoplasm in young Korean subjects less than age 50 years. Intest. Res. https://doi.org/10.5217/ir.2018.00062 (2018).
Noh, C.-K. et al. Association of intensive endoscopic screening burden with gastric cancer detection. JAMA Netw. Open 4, e2032542 (2021).
Mabe, K. et al. Endoscopic screening for gastric cancer in Japan: current status and future perspectives. Dig. Endosc. 34, 412–419 (2022).
Chen, R. et al. Effectiveness of one-time endoscopic screening programme in prevention of upper gastrointestinal cancer in China: a multicentre population-based cohort study. Gut 70, 251 (2021).
Hamashima, C. Benefits and harms of endoscopic screening for gastric cancer. World J. Gastroenterol. 22, 6385–6392 (2016).
Leung, C. Y. et al. Benefits and harms of gastric cancer screening and prevention in Japan: a microsimulation modeling analysis [abstract]. J. Glob. Oncol. 4 (Suppl. 2), 42s (2018).
World Health Organization. Cancer – Screening and early detection. WHO https://www.who.int/europe/news-room/fact-sheets/item/cancer-screening-and-early-detection-of-cancer#:~:text=Early%20diagnosis%20focuses%20on%20detecting,cancers%20before%20any%20symptoms%20appear (2010).
Leung, W. K. et al. Screening for gastric cancer in Asia: current evidence and practice. Lancet Oncol. 9, 279–287 (2008).
Wong, M. C. S. et al. Performance of screening tests for oesophageal squamous cell carcinoma: a systematic review and meta-analysis. Gastrointest. Endosc. https://doi.org/10.1016/j.gie.2022.04.005 (2022).
Wong, M. C. S. & Huang, J. The growing burden of liver cirrhosis: implications for preventive measures. Hepatol. Int. 12, 201–203 (2018).
Zhang, L., Sanagapalli, S. & Stoita, A. Challenges in diagnosis of pancreatic cancer. World J. Gastroenterol. 24, 2047–2060 (2018).
Kongkam, P. et al. Pancreatic cancer in an Asian population. Endosc. Ultrasound 4, 56–62 (2015).
Dutta, U., Bush, N., Kalsi, D., Popli, P. & Kapoor, V. K. Epidemiology of gallbladder cancer in India. Chin. Clin. Oncol. 8, 33 (2019).
Jefford, M. et al. Improved models of care for cancer survivors. Lancet 399, 1551–1560 (2022).
Yoon, S. et al. Living with long-term consequences: experience of follow-up care and support needs among Asian long-term colorectal cancer survivors. Psychooncology 29, 1557–1563 (2020).
Kim, H. & Yoo, Y.-S. Factors influencing supportive care needs of colorectal cancer survivors. Asian Nurs. Res. 15, 60–66 (2021).
Jover, R. Surveillance after colonic neoplasia: to die of success. Endoscopy 45, 511–512 (2013).
Thinh, D. H. Q. et al. Analgesic prescription patterns and pain outcomes in Southeast Asia: findings from the analgesic treatment of cancer pain in Southeast Asia study. J. Glob. Oncol. 4, 1–10 (2018).
Emery, J. et al. Management of common clinical problems experienced by survivors of cancer. Lancet 399, 1537–1550 (2022).
Kline, R. M. et al. Long-term survivorship care after cancer treatment–summary of a 2017 National Cancer Policy Forum Workshop. J. Natl Cancer Inst. 110, 1300–1310 (2018).
Author information
Authors and Affiliations
Contributions
J.H. researched data for the article. M.C.S.W., J.H., S.H.W. and S.C.N. contributed substantially to discussion of the content. J.H. wrote the article. M.C.S.W., D.E.L.-P., L.Z., W.X., S.H.W. and S.C.N. reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks Eishi Baba, Jianguang Ji and the other, anonymous, reviewer for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
GBD 2019: https://vizhub.healthdata.org/gbd-results/
GLOBOCAN 2020: https://gco.iarc.fr/
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, J., Lucero-Prisno, D.E., Zhang, L. et al. Updated epidemiology of gastrointestinal cancers in East Asia. Nat Rev Gastroenterol Hepatol 20, 271–287 (2023). https://doi.org/10.1038/s41575-022-00726-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41575-022-00726-3
This article is cited by
-
Editorial: Comparisons of COVID-19-related disturbance in diagnosis of esophagogastric cancer between the Netherlands and Japan
Journal of Gastroenterology (2024)
-
Influence of Circumferential Extension on Friction of Small Intestine
Tribology Letters (2024)
-
Global burden of young-onset gastric cancer: a systematic trend analysis of the global burden of disease study 2019
Gastric Cancer (2024)
-
Non-coding RNAs/DNMT3B axis in human cancers: from pathogenesis to clinical significance
Journal of Translational Medicine (2023)