Abstract
Mammalian aryl hydrocarbon receptor (AHR) is a ligand-dependent transcription factor that belongs to the basic helix–loop–helix (bHLH)–PAS family of transcription factors, which are evolutionarily conserved environmental sensors. In the absence of ligands, AHR resides in the cytoplasm in a complex with molecular chaperones such as HSP90, XAP2 and p23. Upon ligand binding, AHR translocates into the nuclear compartment, where it dimerizes with its partner protein, AHR nuclear translocator (ARNT), an obligatory partner for the DNA-binding and functional activity. Historically, AHR had mostly been considered as a key intermediary for the detrimental effects of environmental pollutants on the body. However, following the discovery of AHR-mediated functions in various immune cells, as well as the emergence of non-toxic ‘natural’ AHR ligands, this view slowly began to change, and the study of AHR-deficient mice revealed a plethora of important beneficial functions linked to AHR activation. This Review focuses on regulation of the AHR pathway and the barrier-protective roles AHR has in haematopoietic, as well as non-haematopoietic, cells within the intestinal microenvironment. It covers the nature of AHR ligands and feedback regulation of the AHR pathway, outlining the currently known physiological functions in immune, epithelial, endothelial and neuronal cells of the intestine.
Key points
-
Aryl hydrocarbon receptor (AHR) is widely expressed in the intestinal microenvironment, and its activation by natural ligands results in barrier-protective effects.
-
In addition to well-documented functions in intestinal immune cells, AHR has important and less well-studied functions in epithelial and endothelial cells as well as in neurons of the enteric nervous system.
-
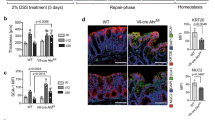
AHR involvement can appear subtle under homeostatic conditions but becomes prominent in regeneration following tissue injury.
-
AHR acts as a tumour suppressor for development of colonic malignancy.
-
New models and tools enabling the dissection of cell type-specific and tissue type-specific AHR functions in vivo are needed to understand the effect of environmental signals on inflammation and tissue repair in the gastrointestinal barrier.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Burbach, K. M., Poland, A. & Bradfield, C. A. Cloning of the Ah-receptor cDNA reveals a distinctive ligand-activated transcription factor. Proc. Natl Acad. Sci. USA 89, 8185–8189 (1992).
Schmidt, J. V. & Bradfield, C. A. Ah receptor signaling pathways. Annu. Rev. Cell Dev. Biol. 12, 55–89 (1996).
Veldhoen, M. et al. The aryl hydrocarbon receptor links TH17-cell-mediated autoimmunity to environmental toxins. Nature 453, 106–109 (2008).
Quintana, F. J. et al. Control of Treg and TH17 cell differentiation by the aryl hydrocarbon receptor. Nature 453, 65–71 (2008).
Stockinger, B., Di Meglio, P., Gialitakis, M. & Duarte, J. H. The aryl hydrocarbon receptor: multitasking in the immune system. Annu. Rev. Immunol. 32, 403–432 (2014).
Hubbard, T. D., Murray, I. A. & Perdew, G. H. Indole and tryptophan metabolism: endogenous and dietary routes to Ah receptor activation. Drug Metab. Dispos. 43, 1522–1535 (2015).
McMillan, B. J. & Bradfield, C. A. The aryl hydrocarbon receptor sans xenobiotics: endogenous function in genetic model systems. Mol. Pharmacol. 72, 487–498 (2007).
Chiaro, C. R., Patel, R. D., Marcus, C. B. & Perdew, G. H. Evidence for an aryl hydrocarbon receptor-mediated cytochrome P450 autoregulatory pathway. Mol. Pharmacol. 72, 1369–1379 (2007).
Wincent, E. et al. Inhibition of cytochrome P4501-dependent clearance of the endogenous agonist FICZ as a mechanism for activation of the aryl hydrocarbon receptor. Proc. Natl Acad. Sci. USA 109, 4479–4484 (2012). This article shows that AHR activation can be indirect via inhibition of CYP1-mediated ligand metabolism that allows response to endogenous ligands.
Bock, K. W. From TCDD-mediated toxicity to searches of physiologic AHR functions. Biochem. Pharmacol. 155, 419–424 (2018).
Giani Tagliabue, S., Faber, S. C., Motta, S., Denison, M. S. & Bonati, L. Modeling the binding of diverse ligands within the Ah receptor ligand binding domain. Sci. Rep. 9, 10693 (2019).
Agus, A., Planchais, J. & Sokol, H. Gut microbiota regulation of tryptophan metabolism in health and disease. Cell Host Microbe 23, 716–724 (2018).
Hu, W., Sorrentino, C., Denison, M. S., Kolaja, K. & Fielden, M. R. Induction of Cyp1a1 is a nonspecific biomarker of aryl hydrocarbon receptor activation: results of large scale screening of pharmaceuticals and toxicants in vivo and in vitro. Mol. Pharmacol. 71, 1475–1486 (2007).
Avilla, M. N., Malecki, K. M. C., Hahn, M. E., Wilson, R. H. & Bradfield, C. A. The Ah receptor: adaptive metabolism, ligand diversity, and the xenokine model. Chem. Res. Toxicol. 33, 860–879 (2020).
Lamas, B., Natividad, J. M. & Sokol, H. Aryl hydrocarbon receptor and intestinal immunity. Mucosal Immunol. 11, 1024–1038 (2018).
Costantini, C. et al. Tryptophan Co-metabolism at the host-pathogen interface. Front. Immunol. 11, 67 (2020).
Hestermann, E. V., Stegeman, J. J. & Hahn, M. E. Relative contributions of affinity and intrinsic efficacy to aryl hydrocarbon receptor ligand potency. Toxicol. Appl. Pharmacol. 168, 160–172 (2000).
Schiering, C., Vonk, A., Das, S., Stockinger, B. & Wincent, E. Cytochrome P4501-inhibiting chemicals amplify aryl hydrocarbon receptor activation and IL-22 production in T helper 17 cells. Biochem. Pharmacol. 151, 47–58 (2018).
Schiering, C. et al. Feedback control of AHR signalling regulates intestinal immunity. Nature 542, 242–245 (2017). This study demonstrates a key role for the intestinal epithelial barrier in regulating both local and systemic distribution of luminal-derived AHR ligands. Constitutive expression of Cyp1a1 in IECs leads to systemic AHR ligand deficiency in mice, recapitulating hallmarks of AHR deficiency.
Seok, S. H. et al. Trace derivatives of kynurenine potently activate the aryl hydrocarbon receptor (AHR). J. Biol. Chem. 293, 1994–2005 (2018). This study provides evidence that kynurenine is not an AHR ligand per se but acts as an AHR proligand, which requires novel chemical conversions for it to act as a receptor agonist.
Rannug, A. How the AHR became important in intestinal homeostasis — a diurnal FICZ/AHR/CYP1A1 feedback controls both immunity and immunopathology. Int. J. Mol. Sci. 21, 5681 (2020).
Bjeldanes, L. F., Kim, J. Y., Grose, K. R., Bartholomew, J. C. & Bradfield, C. A. Aromatic hydrocarbon responsiveness-receptor agonists generated from indole-3-carbinol in vitro and in vivo: comparisons with 2,3,7,8-tetrachlorodibenzo-p-dioxin. Proc. Natl Acad. Sci. USA 88, 9543–9547 (1991).
Hubbard, T. D. et al. Adaptation of the human aryl hydrocarbon receptor to sense microbiota-derived indoles. Sci. Rep. 5, 12689 (2015).
Murray, I. A. & Perdew, G. H. Ligand activation of the Ah receptor contributes to gastrointestinal homeostasis. Curr. Opin. Toxicol. 2, 15–23 (2017).
Scott, S. A., Fu, J. & Chang, P. V. Microbial tryptophan metabolites regulate gut barrier function via the aryl hydrocarbon receptor. Proc. Natl Acad. Sci. USA 117, 19376–19387 (2020).
Zelante, T. et al. Tryptophan catabolites from microbiota engage aryl hydrocarbon receptor and balance mucosal reactivity via interleukin-22. Immunity 39, 372–385 (2013).
Rannug, A. & Rannug, U. The tryptophan derivative 6-formylindolo[3,2-b]carbazole, FICZ, a dynamic mediator of endogenous aryl hydrocarbon receptor signaling, balances cell growth and differentiation. Crit. Rev. Toxicol. 48, 555–574 (2018).
Flaveny, C. A., Murray, I. A., Chiaro, C. R. & Perdew, G. H. Ligand selectivity and gene regulation by the human aryl hydrocarbon receptor in transgenic mice. Mol. Pharmacol. 75, 1412–1420 (2009).
Naganuma, M. et al. Efficacy of indigo naturalis in a multicenter randomized controlled trial of patients with ulcerative colitis. Gastroenterology 154, 935–947 (2018).
Marafini, I. et al. NPD-0414-2 and NPD-0414-24, two chemical entities designed as aryl hydrocarbon receptor (AhR) ligands, inhibit gut inflammatory signals. Front. Pharmacol. 10, 380 (2019).
Chen, J. et al. Modulation of lymphocyte-mediated tissue repair by rational design of heterocyclic aryl hydrocarbon receptor agonists. Sci. Adv. 6, eaay8230 (2020).
Suzuki, T., Hidaka, T., Kumagai, Y. & Yamamoto, M. Environmental pollutants and the immune response. Nat. Immunol. 21, 1486–1495 (2020).
Murray, I. A., Patterson, A. D. & Perdew, G. H. Aryl hydrocarbon receptor ligands in cancer: friend and foe. Nat. Rev. Cancer 14, 801–814 (2014).
Safe, S., Han, H., Goldsby, J., Mohankumar, K. & Chapkin, R. S. Aryl hydrocarbon receptor (AhR) ligands as selective AhR modulators: genomic studies. Curr. Opin. Toxicol. 11-12, 10–20 (2018).
Vogel, C. F. A. & Haarmann-Stemmann, T. The aryl hydrocarbon receptor repressor - More than a simple feedback inhibitor of AhR signaling: clues for its role in inflammation and cancer. Curr. Opin. Toxicol. 2, 109–119 (2017).
Davarinos, N. A. & Pollenz, R. S. Aryl hydrocarbon receptor imported into the nucleus following ligand binding is rapidly degraded via the cytosplasmic proteasome following nuclear export. J. Biol. Chem. 274, 28708–28715 (1999).
MacPherson, L. et al. 2,3,7,8-Tetrachlorodibenzo-p-dioxin poly(ADP-ribose) polymerase (TiPARP, ARTD14) is a mono-ADP-ribosyltransferase and repressor of aryl hydrocarbon receptor transactivation. Nucleic Acids Res. 41, 1604–1621 (2013).
Inouye, K., Shinkyo, R., Takita, T., Ohta, M. & Sakaki, T. Metabolism of polychlorinated dibenzo-p-dioxins (PCDDs) by human cytochrome P450-dependent monooxygenase systems. J. Agric. Food Chem. 50, 5496–5502 (2002).
Wincent, E. et al. The suggested physiologic aryl hydrocarbon receptor activator and cytochrome P4501 substrate 6-formylindolo[3,2-b]carbazole is present in humans. J. Biol. Chem. 284, 2690–2696 (2009).
Ehrlich, A. K. & Kerkvliet, N. I. Is chronic AhR activation by rapidly metabolized ligands safe for the treatment of immune-mediated diseases? Curr. Opin. Toxicol. 2, 72–78 (2017).
Uno, S. et al. Oral exposure to benzo[a]pyrene in the mouse: detoxication by inducible cytochrome P450 is more important than metabolic activation. Mol. Pharmacol. 65, 1225–1237 (2004).
Nebert, D. W., Dalton, T. P., Okey, A. B. & Gonzalez, F. J. Role of aryl hydrocarbon receptor-mediated induction of the CYP1 enzymes in environmental toxicity and cancer. J. Biol. Chem. 279, 23847–23850 (2004).
Metidji, A. et al. The environmental sensor AHR protects from inflammatory damage by maintaining intestinal stem cell homeostasis and barrier integrity. Immunity 49, 353–362.e5 (2018). This study elucidates the mechanisms underlying AHR-mediated CRC protection, demonstrating an epithelial-intrinsic role for AHR in restraining dysregulated stem cell activity through transcriptional activation of the E3 ubiquitin ligases RNF43 and ZNRF3, which inhibit WNT–β-catenin.
Evans, B. R. et al. Repression of aryl hydrocarbon receptor (AHR) signaling by AHR repressor: role of DNA binding and competition for AHR nuclear translocator. Mol. Pharmacol. 73, 387–398 (2008).
Mimura, J., Ema, M., Sogawa, K. & Fujii-Kuriyama, Y. Identification of a novel mechanism of regulation of Ah (dioxin) receptor function. Genes Dev. 13, 20–25 (1999).
Brandstatter, O. et al. Balancing intestinal and systemic inflammation through cell type-specific expression of the aryl hydrocarbon receptor repressor. Sci. Rep. 6, 26091 (2016).
Dey, A., Jones, J. E. & Nebert, D. W. Tissue- and cell type-specific expression of cytochrome P450 1A1 and cytochrome P450 1A2 mRNA in the mouse localized in situ hybridization. Biochem. Pharmacol. 58, 525–537 (1999).
Uno, S. et al. Basal and inducible CYP1 mRNA quantitation and protein localization throughout the mouse gastrointestinal tract. Free Radic. Biol. Med. 44, 570–583 (2008).
Schanz, O. et al. Dietary AhR ligands regulate ahrr expression in intestinal immune cells and intestinal microbiota composition. Int. J. Mol. Sci. 21, 3189 (2020).
Bernshausen, T., Jux, B., Esser, C., Abel, J. & Fritsche, E. Tissue distribution and function of the aryl hydrocarbon receptor repressor (AhRR) in C57BL/6 and aryl hydrocarbon receptor deficient mice. Arch. Toxicol. 80, 206–211 (2006).
Hosoya, T. et al. Inducibility of cytochrome P450 1A1 and chemical carcinogenesis by benzo[a]pyrene in AhR repressor-deficient mice. Biochem. Biophys. Res. Commun. 365, 562–567 (2008).
Tigges, J. et al. Aryl hydrocarbon receptor repressor (AhRR) function revisited: repression of CYP1 activity in human skin fibroblasts is not related to AhRR expression. J. Invest. Dermatol. 133, 87–96 (2013).
Ahmed, S. et al. Loss of the mono-ADP-ribosyltransferase, Tiparp, increases sensitivity to dioxin-induced steatohepatitis and lethality. J. Biol. Chem. 290, 16824–16840 (2015).
Hutin, D. et al. Hepatocyte-specific deletion of TIPARP, a negative regulator of the aryl hydrocarbon receptor, is sufficient to increase sensitivity to dioxin-induced wasting syndrome. Toxicol. Sci. 165, 347–360 (2018).
Yamada, T. et al. Constitutive aryl hydrocarbon receptor signaling constrains type I interferon-mediated antiviral innate defense. Nat. Immunol. 17, 687–694 (2016).
Mowat, A. M. Anatomical basis of tolerance and immunity to intestinal antigens. Nat. Rev. Immunol. 3, 331–341 (2003).
Li, Y. et al. Exogenous stimuli maintain intraepithelial lymphocytes via aryl hydrocarbon receptor activation. Cell 147, 629–640 (2011).
Cervantes-Barragan, L. et al. Lactobacillus reuteri induces gut intraepithelial CD4+CD8alphaalpha+ T cells. Science 357, 806–810 (2017).
Aoki, R., Aoki-Yoshida, A., Suzuki, C. & Takayama, Y. Indole-3-pyruvic acid, an aryl hydrocarbon receptor activator, suppresses experimental colitis in mice. J. Immunol. 201, 3683–3693 (2018).
Li, S., Bostick, J. W. & Zhou, L. Regulation of innate lymphoid cells by aryl hydrocarbon receptor. Front. Immunol. 8, 1909 (2017).
Seillet, C. & Jacquelot, N. Sensing of physiological regulators by innate lymphoid cells. Cell Mol. Immunol. 16, 442–451 (2019).
Gomez de Aguero, M. et al. The maternal microbiota drives early postnatal innate immune development. Science 351, 1296–1302 (2016).
Lamas, B. et al. CARD9 impacts colitis by altering gut microbiota metabolism of tryptophan into aryl hydrocarbon receptor ligands. Nat. Med. 22, 598–605 (2016).
Li, J., Doty, A. & Glover, S. C. Aryl hydrocarbon receptor signaling involves in the human intestinal ILC3/ILC1 conversion in the inflamed terminal ileum of Crohn’s disease patients. Inflamm. Cell Signal. 3, e1404 (2016).
Cella, M. et al. Subsets of ILC3-ILC1-like cells generate a diversity spectrum of innate lymphoid cells in human mucosal tissues. Nat. Immunol. 20, 980–991 (2019).
Zhao, Y. et al. MicroRNA-124 promotes intestinal inflammation by targeting aryl hydrocarbon receptor in Crohn’s disease. J. Crohns Colitis 10, 703–712 (2016).
Li, S. et al. Aryl hydrocarbon receptor signaling cell intrinsically inhibits intestinal group 2 innate lymphoid cell function. Immunity 49, 915–928.e5 (2018). This article reveals a cell-intrinsic role for AHR in balancing intestinal ILC3 and ILC2 populations through repression of the IL-33–ST2 axis, thereby limiting TH2 cell-mediated immunity in favour of ILC3 effector function.
Liang, S. C. et al. Interleukin (IL)-22 and IL-17 are coexpressed by Th17 cells and cooperatively enhance expression of antimicrobial peptides. J. Exp. Med. 203, 2271–2279 (2006).
Basu, R. et al. Th22 cells are an important source of IL-22 for host protection against enteropathogenic bacteria. Immunity 37, 1061–1075 (2012).
Gagliani, N. et al. Th17 cells transdifferentiate into regulatory T cells during resolution of inflammation. Nature 523, 221–225 (2015).
Coombes, J. L., Robinson, N. J., Maloy, K. J., Uhlig, H. H. & Powrie, F. Regulatory T cells and intestinal homeostasis. Immunol. Rev. 204, 184–194 (2005).
Russler-Germain, E. V., Rengarajan, S. & Hsieh, C. S. Antigen-specific regulatory T-cell responses to intestinal microbiota. Mucosal Immunol. 10, 1375–1386 (2017).
Kim, K. S. et al. Dietary antigens limit mucosal immunity by inducing regulatory T cells in the small intestine. Science 351, 858–863 (2016).
Duarte, J. H., Di Meglio, P., Hirota, K., Ahlfors, H. & Stockinger, B. Differential influences of the aryl hydrocarbon receptor on Th17 mediated responses in vitro and in vivo. PLoS ONE 8, e79819 (2013).
Ye, J. et al. The aryl hydrocarbon receptor preferentially marks and promotes gut regulatory T cells. Cell Rep. 21, 2277–2290 (2017). This article probes a cell-intrinsic role for AHR in Treg cells, demonstrating the importance of Treg cell AHR signalling in regulating intestinal homing, and its requirement for immunosuppressive function in colitis.
Xiong, L. et al. Ahr-Foxp3-RORgammat axis controls gut homing of CD4+ T cells by regulating GPR15. Sci. Immunol. 5, eaaz7277 (2020).
Goudot, C. et al. Aryl hydrocarbon receptor controls monocyte differentiation into dendritic cells versus macrophages. Immunity 47, 582–596.e6 (2017).
Chen, F. et al. mTOR mediates IL-23 induction of neutrophil IL-17 and IL-22 production. J. Immunol. 196, 4390–4399 (2016).
Ireland, H. et al. Inducible Cre-mediated control of gene expression in the murine gastrointestinal tract: effect of loss of beta-catenin. Gastroenterology 126, 1236–1246 (2004).
Ito, S., Chen, C., Satoh, J., Yim, S. & Gonzalez, F. J. Dietary phytochemicals regulate whole-body CYP1A1 expression through an arylhydrocarbon receptor nuclear translocator-dependent system in gut. J. Clin. Invest. 117, 1940–1950 (2007).
Barker, N. et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature 449, 1003–1007 (2007).
Clevers, H. The intestinal crypt, a prototype stem cell compartment. Cell 154, 274–284 (2013).
Novellasdemunt, L., Antas, P. & Li, V. S. Targeting Wnt signaling in colorectal cancer. a review in the theme: cell signaling: proteins, pathways and mechanisms. Am. J. Physiol. Cell Physiol 309, C511–C521 (2015).
Boitano, A. E. et al. Aryl hydrocarbon receptor antagonists promote the expansion of human hematopoietic stem cells. Science 329, 1345–1348 (2010).
Gialitakis, M. et al. Activation of the aryl hydrocarbon receptor interferes with early embryonic development. Stem Cell Rep. 9, 1377–1386 (2017).
Villa, M. et al. The aryl hydrocarbon receptor controls cyclin O to promote epithelial multiciliogenesis. Nat. Commun. 7, 12652 (2016).
Ly, M. et al. Diminished AHR signaling drives human acute myeloid leukemia stem cell maintenance. Cancer Res. 79, 5799–5811 (2019).
Schneider, A. J., Branam, A. M. & Peterson, R. E. Intersection of AHR and Wnt signaling in development, health, and disease. Int. J. Mol. Sci. 15, 17852–17885 (2014).
Luecke-Johansson, S. et al. A molecular mechanism to switch the aryl hydrocarbon receptor from a transcription factor to an E3 ubiquitin ligase. Mol. Cell Biol. 37, e00630-16 (2017).
Koo, B. K. et al. Tumour suppressor RNF43 is a stem-cell E3 ligase that induces endocytosis of Wnt receptors. Nature 488, 665–669 (2012).
Alvarado, D. M. et al. Epithelial indoleamine 2,3-dioxygenase 1 modulates aryl hydrocarbon receptor and Notch signaling to increase differentiation of secretory cells and alter mucus-associated microbiota. Gastroenterology 157, 1093–1108.e11 (2019).
Yu, M. et al. Aryl hydrocarbon receptor activation modulates intestinal epithelial barrier function by maintaining tight junction integrity. Int. J. Biol. Sci. 14, 69–77 (2018).
Singh, R. et al. Enhancement of the gut barrier integrity by a microbial metabolite through the Nrf2 pathway. Nat. Commun. 10, 1–18 (2019).
Lahvis, G. P. et al. Portosystemic shunting and persistent fetal vascular structures in aryl hydrocarbon receptor-deficient mice. Proc. Natl Acad. Sci. USA 97, 10442–10447 (2000). This study characterizes physiological and morphological abnormalities in AHR-deficient mice, providing early evidence for a critical function of AHR in the regulation of vascular development and patterning.
Walisser, J. A., Glover, E., Pande, K., Liss, A. L. & Bradfield, C. A. Aryl hydrocarbon receptor-dependent liver development and hepatotoxicity are mediated by different cell types. Proc. Natl Acad. Sci. USA 102, 17858–17863 (2005).
Agbor, L. N., Elased, K. M. & Walker, M. K. Endothelial cell-specific aryl hydrocarbon receptor knockout mice exhibit hypotension mediated, in part, by an attenuated angiotensin II responsiveness. Biochem. Pharmacol. 82, 514–523 (2011).
Fandriks, L. The angiotensin II type 2 receptor and the gastrointestinal tract. J. Renin Angiotensin Aldosterone Syst. 11, 43–48 (2010).
Nakajima, H. & Mochizuki, N. Flow pattern-dependent endothelial cell responses through transcriptional regulation. Cell Cycle 16, 1893–1901 (2017).
Lin, K. et al. Molecular mechanism of endothelial growth arrest by laminar shear stress. Proc. Natl Acad. Sci. USA 97, 9385–9389 (2000).
McMillan, B. J. & Bradfield, C. A. The aryl hydrocarbon receptor is activated by modified low-density lipoprotein. Proc. Natl Acad. Sci. USA 104, 1412–1417 (2007).
Han, Z. et al. Aryl hydrocarbon receptor mediates laminar fluid shear stress-induced CYP1A1 activation and cell cycle arrest in vascular endothelial cells. Cardiovasc. Res. 77, 809–818 (2008).
Conway, D. E. et al. Expression of CYP1A1 and CYP1B1 in human endothelial cells: regulation by fluid shear stress. Cardiovasc. Res. 81, 669–677 (2009).
Hanahan, D. & Folkman, J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 86, 353–364 (1996).
Lee, J. H. et al. Lung stem cell differentiation in mice directed by endothelial cells via a BMP4-NFATc1-thrombospondin-1 axis. Cell 156, 440–455 (2014).
Hsu, T., Nguyen-Tran, H. H. & Trojanowska, M. Active roles of dysfunctional vascular endothelium in fibrosis and cancer. J. Biomed. Sci. 26, 86 (2019).
Deban, L., Correale, C., Vetrano, S., Malesci, A. & Danese, S. Multiple pathogenic roles of microvasculature in inflammatory bowel disease: a jack of all trades. Am. J. Pathol. 172, 1457–1466 (2008).
Pousa, I. D., Mate, J. & Gisbert, J. P. Angiogenesis in inflammatory bowel disease. Eur. J. Clin. Invest. 38, 73–81 (2008).
Zhu, Z. et al. Aryl hydrocarbon receptor in cutaneous vascular endothelial cells restricts psoriasis development by negatively regulating neutrophil recruitment. J. Invest. Dermatol. 140, 1233–1243.e9 (2019).
Cardoso, V. et al. Neuronal regulation of type 2 innate lymphoid cells via neuromedin U. Nature 549, 277–281 (2017).
Ibiza, S. et al. Glial-cell-derived neuroregulators control type 3 innate lymphoid cells and gut defence. Nature 535, 440–443 (2016).
Juricek, L. & Coumoul, X. The aryl hydrocarbon receptor and the nervous system. Int. J. Mol. Sci. 19, 2504 (2018).
Memic, F. et al. Transcription and signaling regulators in developing neuronal subtypes of mouse and human enteric nervous system. Gastroenterology 154, 624–636 (2018).
Obata, Y. et al. Neuronal programming by microbiota regulates intestinal physiology. Nature 578, 284–289 (2020). This study identifies that enteric neurons in the colon express AHR in a manner dependent on the microbiota. Cell-intrinsic AHR activation is required for the integration of environmental cues from the microbiota in order to regulate peristalsis.
De Vadder, F. et al. Gut microbiota regulates maturation of the adult enteric nervous system via enteric serotonin networks. Proc. Natl Acad. Sci. USA 115, 6458–6463 (2018).
Kabouridis, P. S. et al. Microbiota controls the homeostasis of glial cells in the gut lamina propria. Neuron 85, 289–295 (2015).
Bielefeldt, K., Tuteja, A. & Nusrat, S. Disorders of gastrointestinal hypomotility. F1000Res 5, 1897 (2016).
Yano, J. M. et al. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell 161, 264–276 (2015).
Manzella, C. R. et al. Serotonin modulates AhR activation by interfering with CYP1A1-mediated clearance of AhR ligands. Cell. Physiol. Biochem. 54, 126–141 (2020).
Yuan, H. X. et al. Whole exome sequencing identifies a KCNJ12 mutation as a cause of familial dilated cardiomyopathy. Medicine 96, e7727 (2017).
Silver, J., Schwab, M. E. & Popovich, P. G. Central nervous system regenerative failure: role of oligodendrocytes, astrocytes, and microglia. Cold Spring Harb. Perspect. Biol. 7, a020602 (2014).
Kruger, G. M. et al. Neural crest stem cells persist in the adult gut but undergo changes in self-renewal, neuronal subtype potential, and factor responsiveness. Neuron 35, 657–669 (2002).
Heanue, T. A. & Pachnis, V. Enteric nervous system development and Hirschsprung’s disease: advances in genetic and stem cell studies. Nat. Rev. Neurosci. 8, 466–479 (2007).
Di Giaimo, R. et al. The aryl hydrocarbon receptor pathway defines the time frame for restorative neurogenesis. Cell Rep. 25, 3241–3251.e5 (2018).
Bersten, D. C., Sullivan, A. E., Peet, D. J. & Whitelaw, M. L. bHLH-PAS proteins in cancer. Nat. Rev. Cancer 13, 827–841 (2013).
Denissenko, M. F., Pao, A., Tang, M. & Pfeifer, G. P. Preferential formation of benzo[a]pyrene adducts at lung cancer mutational hotspots in P53. Science 274, 430–432 (1996).
McGuire, J., Okamoto, K., Whitelaw, M. L., Tanaka, H. & Poellinger, L. Definition of a dioxin receptor mutant that is a constitutive activator of transcription: delineation of overlapping repression and ligand binding functions within the PAS domain. J. Biol. Chem. 276, 41841–41849 (2001).
Andersson, P. et al. A constitutively active dioxin/aryl hydrocarbon receptor induces stomach tumors. Proc. Natl Acad. Sci. USA 99, 9990–9995 (2002).
Moennikes, O. et al. A constitutively active dioxin/aryl hydrocarbon receptor promotes hepatocarcinogenesis in mice. Cancer Res. 64, 4707–4710 (2004).
Diaz-Diaz, C. J. et al. The aryl hydrocarbon receptor is a repressor of inflammation-associated colorectal tumorigenesis in mouse. Ann. Surg. 264, 429–436 (2016).
Dinallo, V. et al. Protective effects of aryl hydrocarbon receptor signaling in celiac disease mucosa and in poly I:C-induced small intestinal atrophy mouse model. Front. Immunol. 10, 91 (2019).
Ikuta, T., Kurosumi, M., Yatsuoka, T. & Nishimura, Y. Tissue distribution of aryl hydrocarbon receptor in the intestine: implication of putative roles in tumor suppression. Exp. Cell Res. 343, 126–134 (2016).
Beyaz, S. et al. High-fat diet enhances stemness and tumorigenicity of intestinal progenitors. Nature 531, 53–58 (2016).
Mayne, S. T., Playdon, M. C. & Rock, C. L. Diet, nutrition, and cancer: past, present and future. Nat. Rev. Clin. Oncol. 13, 504–515 (2016).
Terry, P. et al. Fruit, vegetables, dietary fiber, and risk of colorectal cancer. J. Natl Cancer Inst. 93, 525–533 (2001).
Cunningham, D. et al. Colorectal cancer. Lancet 375, 1030–1047 (2010).
Zitvogel, L., Pietrocola, F. & Kroemer, G. Nutrition, inflammation and cancer. Nat. Immunol. 18, 843–850 (2017).
Fernandez-Salguero, P. M., Ward, J. M., Sundberg, J. P. & Gonzalez, F. J. Lesions of aryl-hydrocarbon receptor-deficient mice. Vet. Pathol. 34, 605–614 (1997).
Monteleone, I. et al. Aryl hydrocarbon receptor-induced signals up-regulate IL-22 production and inhibit inflammation in the gastrointestinal tract. Gastroenterology 141, 237–248.e1 (2011).
Lanis, J. M. et al. Tryptophan metabolite activation of the aryl hydrocarbon receptor regulates IL-10 receptor expression on intestinal epithelia. Mucosal Immunol. 10, 1133–1144 (2017).
Hernandez, P., Gronke, K. & Diefenbach, A. A catch-22: interleukin-22 and cancer. Eur. J. Immunol. 48, 15–31 (2018).
Gronke, K. et al. Interleukin-22 protects intestinal stem cells against genotoxic stress. Nature 566, 249–253 (2019).
Kirchberger, S. et al. Innate lymphoid cells sustain colon cancer through production of interleukin-22 in a mouse model. J. Exp. Med. 210, 917–931 (2013).
Thompson, C. L., Plummer, S. J., Tucker, T. C., Casey, G. & Li, L. Interleukin-22 genetic polymorphisms and risk of colon cancer. Cancer Causes Control. 21, 1165–1170 (2010).
Rothhammer, V. et al. Microglial control of astrocytes in response to microbial metabolites. Nature 557, 724–728 (2018).
Shinde, R. & McGaha, T. L. The aryl hydrocarbon receptor: connecting immunity to the microenvironment. Trends Immunol. 39, 1005–1020 (2018).
Fatkhullina, A. R. et al. An interleukin-23-interleukin-22 axis regulates intestinal microbial homeostasis to protect from diet-induced atherosclerosis. Immunity 49, 943–957.e9 (2018).
Rosser, E. C. et al. Microbiota-Derived metabolites suppress arthritis by amplifying aryl-hydrocarbon receptor activation in regulatory B cells. Cell Metab. 31, 837–851.e10 (2020).
Natividad, J. M. et al. Impaired aryl hydrocarbon receptor ligand production by the gut microbiota is a key factor in metabolic syndrome. Cell Metab. 28, 737–749.e4 (2018). This article links metabolic syndrome with reduced capacity for generation of AHR ligands via microbiota metabolism of tryptophan.
Lavelle, A. & Sokol, H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 17, 223–237 (2020).
Busbee, P. B. et al. Indole-3-carbinol prevents colitis and associated microbial dysbiosis in an IL-22-dependent manner. JCI Insight 5, e127551 (2020).
Kim, Y. S. & Milner, J. A. Targets for indole-3-carbinol in cancer prevention. J. Nutr. Biochem. 16, 65–73 (2005).
Weng, J. R., Tsai, C. H., Kulp, S. K. & Chen, C. S. Indole-3-carbinol as a chemopreventive and anti-cancer agent. Cancer Lett. 262, 153–163 (2008).
Acknowledgements
B.S. and K.S. are supported by the Francis Crick Institute, which receives its core funding from Cancer Research UK, the UK Medical Research Council and the Wellcome Trust (FC001159). E.W. is supported by the Swedish research councils FORMAS (216-2013-1966) and VR (2020-03418).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks C. Bradfield, who co-reviewed with R. Wilson and P. Carney, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Ligands
-
Molecules or compounds exhibiting specific binding to a receptor.
- ‘Natural’ AHR ligands
-
Ligands derived from the diet or the gut microbiota or formed endogenously.
- Efficacy
-
Biological effectiveness of the ligand; that is, its ability to induce an active form of the receptor and the degree to which it produces a biological response.
- Potency
-
The concentration or amount of the ligand needed to produce a specific biological effect; that is, the sum of a ligand’s affinity and efficacy.
- Affinity
-
The strength with which a ligand binds to its receptor; that is, how well it fits into the ligand-binding pocket.
Rights and permissions
About this article
Cite this article
Stockinger, B., Shah, K. & Wincent, E. AHR in the intestinal microenvironment: safeguarding barrier function. Nat Rev Gastroenterol Hepatol 18, 559–570 (2021). https://doi.org/10.1038/s41575-021-00430-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41575-021-00430-8
This article is cited by
-
Porphyromonas gingivalis aggravates colitis via a gut microbiota-linoleic acid metabolism-Th17/Treg cell balance axis
Nature Communications (2024)
-
Bioluminescence imaging of Cyp1a1-luciferase reporter mice demonstrates prolonged activation of the aryl hydrocarbon receptor in the lung
Communications Biology (2024)
-
Microbiota–gut–brain axis and its therapeutic applications in neurodegenerative diseases
Signal Transduction and Targeted Therapy (2024)
-
Modulating AHR function offers exciting therapeutic potential in gut immunity and inflammation
Cell & Bioscience (2023)
-
Immune regulation through tryptophan metabolism
Experimental & Molecular Medicine (2023)