Abstract
Breast cancer is the most common invasive malignancy in the world, with millions of survivors living today. Type 2 diabetes mellitus (T2DM) is also a globally prevalent disease that is a widely studied risk factor for breast cancer. Most breast tumours express the oestrogen receptor and are treated with systemic therapies designed to disrupt oestrogen-dependent signalling. Since the advent of targeted endocrine therapy six decades ago, the mortality from breast cancer has steadily declined; however, during the past decade, an elevated risk of T2DM after breast cancer treatment has been reported, particularly for those who received endocrine therapy. In this Review, we highlight key events in the history of endocrine therapies, beginning with the development of tamoxifen. We also summarize the sequence of reported adverse metabolic effects, which include dyslipidaemia, hepatic steatosis and impaired glucose tolerance. We discuss the limitations of determining a causal role for breast cancer treatments in T2DM development from epidemiological data and describe informative preclinical studies that suggest complex mechanisms through which endocrine therapy might drive T2DM risk and progression. We also reinforce the life-saving benefits of endocrine therapy and highlight the need for better predictive biomarkers of T2DM risk and preventive strategies for the growing population of breast cancer survivors.
Key points
-
Endocrine therapies for breast cancer might increase the risk of type 2 diabetes mellitus (T2DM) development in some patients.
-
Oestrogens and oestrogen receptor activation protect against metabolic disease and are disrupted with breast cancer treatment.
-
Tamoxifen treatment promotes dyslipidaemia and hepatic steatosis in some people and also has adipose-specific effects in preclinical and clinical studies.
-
One paradigm of T2DM development centres on dysfunctional adipose tissue expansion.
-
Preclinical studies indicate that adipose tissue might be an early target of endocrine therapies for breast cancer.
-
Endocrine therapies save lives, so an urgent need exists to understand any associated T2DM risk and offer interventions for patients with breast cancer.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
World Health Organization. Breast cancer. WHO https://www.who.int/news-room/fact-sheets/detail/breast-cancer (2023).
Pan, H. et al. 20-Year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N. Engl. J. Med. 377, 1836–1846 (2017).
Mouridsen, H., Palshof, T., Patterson, J. & Battersby, L. Tamoxifen in advanced breast cancer. Cancer Treat. Rev. 5, 131–141 (1978).
Meisel, J. L., Venur, V. A., Gnant, M. & Carey, L. Evolution of targeted therapy in breast cancer: where precision medicine began. Am. Soc. Clin. Oncol. Educ. Book 38, 78–86 (2018).
Early Breast Cancer Trialists’ Collaborative Group. Effects of adjuvant tamoxifen and of cytotoxic therapy on mortality in early breast cancer. An overview of 61 randomized trials among 28,896 women. N. Engl. J. Med. 319, 1681–1692 (1988).
Fisher, B. et al. A randomized clinical trial evaluating tamoxifen in the treatment of patients with node-negative breast cancer who have estrogen-receptor-positive tumors. N. Engl. J. Med. 320, 479–484 (1989).
Rutqvist, L. E., Johansson, H., Stockholm Breast Cancer Study Group. Long-term follow-up of the randomized Stockholm trial on adjuvant tamoxifen among postmenopausal patients with early stage breast cancer. Acta Oncol. 46, 133–145 (2007).
Nayfield, S. G., Karp, J. E., Ford, L. G., Dorr, F. A. & Kramer, B. S. Potential role of tamoxifen in prevention of breast cancer. J. Natl Cancer Inst. 83, 1450–1459 (1991).
Fisher, B. et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J. Natl Cancer Inst. 90, 1371–1388 (1998).
Vogel, V. G. et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA 295, 2727–2741 (2006).
Santen, R. J., Brodie, H., Simpson, E. R., Siiteri, P. K. & Brodie, A. History of aromatase: saga of an important biological mediator and therapeutic target. Endocr. Rev. 30, 343–375 (2009).
Coombes, R. C., Goss, P., Dowsett, M., Gazet, J. C. & Brodie, A. 4-Hydroxyandrostenedione in treatment of postmenopausal patients with advanced breast cancer. Lancet 2, 1237–1239 (1984).
Buzdar, A. U. et al. Anastrozole versus megestrol acetate in the treatment of postmenopausal women with advanced breast carcinoma: results of a survival update based on a combined analysis of data from two mature phase III trials. Arimidex Study Group. Cancer 83, 1142–1152 (1998).
Nabholtz, J. M. et al. Anastrozole is superior to tamoxifen as first-line therapy for advanced breast cancer in postmenopausal women: results of a North American multicenter randomized trial. Arimidex Study Group. J. Clin. Oncol. 18, 3758–3767 (2000).
Brown, K. A. et al. Menopause is a determinant of breast aromatase expression and its associations with BMI, inflammation, and systemic markers. J. Clin. Endocrinol. Metab. 102, 1692–1701 (2017).
Coombes, R. C. et al. A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N. Engl. J. Med. 350, 1081–1092 (2004).
Baum, M. et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomised trial. Lancet 359, 2131–2139 (2002).
Mouridsen, H. et al. Superior efficacy of letrozole versus tamoxifen as first-line therapy for postmenopausal women with advanced breast cancer: results of a phase III study of the International Letrozole Breast Cancer Group. J. Clin. Oncol. 19, 2596–2606 (2001).
Mouridsen, H. et al. Phase III study of letrozole versus tamoxifen as first-line therapy of advanced breast cancer in postmenopausal women: analysis of survival and update of efficacy from the International Letrozole Breast Cancer Group. J. Clin. Oncol. 21, 2101–2109 (2003).
Goss, P. E. & Strasser, K. Aromatase inhibitors in the treatment and prevention of breast cancer. J. Clin. Oncol. 19, 881–894 (2001).
Davies, C. et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet 381, 805–816 (2013).
Mamounas, E. P. et al. Ten-year update: NRG Oncology/NSABP B-42 randomized trial: extended letrozole therapy in early-stage breast cancer. J. Natl Cancer Inst. https://doi.org/10.1093/jnci/djad078 (2023).
Vergote, I. & Robertson, J. F. Fulvestrant is an effective and well-tolerated endocrine therapy for postmenopausal women with advanced breast cancer: results from clinical trials. Br. J. Cancer 90, S11–S14 (2004).
Bidard, F. C. et al. Elacestrant (oral selective estrogen receptor degrader) versus standard endocrine therapy for estrogen receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: results from the randomized phase III EMERALD trial. J. Clin. Oncol. 40, 3246–3256 (2022).
Pagani, O. et al. Adjuvant exemestane with ovarian suppression in premenopausal breast cancer: long-term follow-up of the combined TEXT and SOFT trials. J. Clin. Oncol. 41, 1376–1382 (2023).
Early Breast Cancer Trialists’ Collaborative Group. Aromatase inhibitors versus tamoxifen in premenopausal women with oestrogen receptor-positive early-stage breast cancer treated with ovarian suppression: a patient-level meta-analysis of 7030 women from four randomised trials. Lancet Oncol. 23, 382–392 (2022).
Bertelli, G. et al. Adjuvant tamoxifen in primary breast cancer: influence on plasma lipids and antithrombin III levels. Breast cancer Res. Treat. 12, 307–310 (1988).
Bruning, P. F. et al. Tamoxifen, serum lipoproteins and cardiovascular risk. Br. J. Cancer 58, 497–499 (1988).
Love, R. R. et al. Effects of tamoxifen therapy on lipid and lipoprotein levels in postmenopausal patients with node-negative breast cancer. J. Natl Cancer Inst. 82, 1327–1332 (1990).
Rossner, S. & Wallgren, A. Serum lipoproteins and proteins after breast cancer surgery and effects of tamoxifen. Atherosclerosis 52, 339–346 (1984).
Thangaraju, M., Kumar, K., Gandhirajan, R. & Sachdanandam, P. Effect of tamoxifen on plasma lipids and lipoproteins in postmenopausal women with breast cancer. Cancer 73, 659–663 (1994).
Montagnani, A. et al. The effects on lipid serum levels of a 2-year adjuvant treatment with exemestane after tamoxifen in postmenopausal women with early breast cancer. Eur. J. Intern. Med. 19, 592–597 (2008).
Francini, G. et al. Exemestane after tamoxifen as adjuvant hormonal therapy in postmenopausal women with breast cancer: effects on body composition and lipids. Br. J. Cancer 95, 153–158 (2006).
Cigler, T. et al. A randomized, placebo-controlled trial (NCIC CTG MAP.2) examining the effects of exemestane on mammographic breast density, bone density, markers of bone metabolism and serum lipid levels in postmenopausal women. Breast Cancer Res. Treat. 126, 453–461 (2011).
Wasan, K. M. et al. Lipid concentrations in postmenopausal women on letrozole after 5 years of tamoxifen: an NCIC CTG MA.17 sub-study. Breast Cancer Res. Treat. 136, 769–776 (2012).
Hozumi, Y. et al. The effect of exemestane, anastrozole, and tamoxifen on lipid profiles in Japanese postmenopausal early breast cancer patients: final results of National Surgical Adjuvant Study BC 04, the TEAM Japan sub-study. Ann. Oncol. 22, 1777–1782 (2011).
[No authors listed] CORRIGENDUM to ‘Steroidal aromatase inhibitors have a more favorable effect on lipid profiles than nonsteroidal aromatase inhibitors in postmenopausal women with early breast cancer: a prospective cohort study’. Ther. Adv. Med. Oncol. 12, 1758835920956880 (2020).
Wang, X. et al. Steroidal aromatase inhibitors have a more favorable effect on lipid profiles than nonsteroidal aromatase inhibitors in postmenopausal women with early breast cancer: a prospective cohort study. Ther. Adv. Med. Oncol. 12, 1758835920925991 (2020).
Boszkiewicz, K., Piwowar, A. & Petryszyn, P. Aromatase inhibitors and risk of metabolic and cardiovascular adverse effects in breast cancer patients — a systematic review and meta-analysis. J. Clin. Med. 11, 3133 (2022).
Eslam, M., Sanyal, A. J., George, J. International Consensus Panel. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology 158, 1999–2014.e1 (2020).
Pinto, H. C. et al. Tamoxifen-associated steatohepatitis — report of three cases. J. Hepatol. 23, 95–97 (1995).
Ogawa, Y., Murata, Y., Nishioka, A., Inomata, T. & Yoshida, S. Tamoxifen-induced fatty liver in patients with breast cancer. Lancet 351, 725 (1998).
Bruno, S. et al. Incidence and risk factors for non-alcoholic steatohepatitis: prospective study of 5408 women enrolled in Italian tamoxifen chemoprevention trial. Br. Med. J. 330, 932 (2005).
Nguyen, M. C., Stewart, R. B., Banerji, M. A., Gordon, D. H. & Kral, J. G. Relationships between tamoxifen use, liver fat and body fat distribution in women with breast cancer. Int. J. Obes. Relat. Metab. Disord. 25, 296–298 (2001).
Cheung, Y. M., Ramchand, S. K., Yeo, B. & Grossmann, M. Cardiometabolic effects of endocrine treatment of estrogen receptor-positive early breast cancer. J. Endocr. Soc. 3, 1283–1301 (2019).
Hong, N. et al. Different patterns in the risk of newly developed fatty liver and lipid changes with tamoxifen versus aromatase inhibitors in postmenopausal women with early breast cancer: a propensity score-matched cohort study. Eur. J. Cancer 82, 103–114 (2017).
Lin, Y. et al. A prospective, randomized study on hepatotoxicity of anastrozole compared with tamoxifen in women with breast cancer. Cancer Sci. 105, 1182–1188 (2014).
Lee, J. I. et al. Aromatase inhibitors and newly developed nonalcoholic fatty liver disease in postmenopausal patients with early breast cancer: a propensity score-matched cohort study. Oncologist 24, e653–e661 (2019).
Harborg, S. et al. Obesity and breast cancer prognosis: pre-diagnostic anthropometric measures in relation to patient, tumor, and treatment characteristics. Cancer Metab. 11, 8 (2023).
Camoriano, J. K. et al. Weight change in women treated with adjuvant therapy or observed following mastectomy for node-positive breast cancer. J. Clin. Oncol. 8, 1327–1334 (1990).
Kohrt, W. M. & Wierman, M. E. Preventing fat gain by blocking follicle-stimulating hormone. N. Engl. J. Med. 377, 293–295 (2017).
Sestak, I. et al. Weight change associated with anastrozole and tamoxifen treatment in postmenopausal women with or at high risk of developing breast cancer. Breast Cancer Res. Treat. 134, 727–734 (2012).
Hoskin, P. J., Ashley, S. & Yarnold, J. R. Weight gain after primary surgery for breast cancer-effect of tamoxifen. Breast Cancer Res. Treat. 22, 129–132 (1992).
Kumar, N. B. et al. Weight gain associated with adjuvant tamoxifen therapy in stage I and II breast cancer: fact or artifact? Breast Cancer Res. Treat. 44, 135–143 (1997).
Fisher, B. et al. Five versus more than five years of tamoxifen therapy for breast cancer patients with negative lymph nodes and estrogen receptor-positive tumors. J. Natl Cancer Inst. 88, 1529–1542 (1996).
Day, R. National Surgical Adjuvant Breast and Bowel Projet P-1 Study. Quality of life and tamoxifen in a breast cancer prevention trial: a summary of findings from the NSABP P-1 study. Ann. NY Acad. Sci. 949, 143–150 (2001).
Sheean, P. M., Hoskins, K. & Stolley, M. Body composition changes in females treated for breast cancer: a review of the evidence. Breast Cancer Res. Treat. 135, 663–680 (2012).
Ali, P. A., al-Ghorabie, F. H., Evans, C. J., el-Sharkawi, A. M. & Hancock, D. A. Body composition measurements using DXA and other techniques in tamoxifen-treated patients. Appl. Radiat. Isot. 49, 643–645 (1998).
van Londen, G. J. et al. The impact of an aromatase inhibitor on body composition and gonadal hormone levels in women with breast cancer. Breast Cancer Res. Treat. 125, 441–446 (2011).
Gibb, F. W. et al. Higher insulin resistance and adiposity in postmenopausal women with breast cancer treated with aromatase inhibitors. J. Clin. Endocrinol. Metab. 104, 3670–3678 (2019).
Johnson, J. D. On the causal relationships between hyperinsulinaemia, insulin resistance, obesity and dysglycaemia in type 2 diabetes. Diabetologia 64, 2138–2146 (2021).
Lipscombe, L. L., Goodwin, P. J., Zinman, B., McLaughlin, J. R. & Hux, J. E. Increased prevalence of prior breast cancer in women with newly diagnosed diabetes. Breast Cancer Res. Treat. 98, 303–309 (2006).
Bordeleau, L. et al. Diabetes and breast cancer among women with BRCA1 and BRCA2 mutations. Cancer 117, 1812–1818 (2011).
Kwan, M. L. et al. Risk of cardiometabolic risk factors in women with and without a history of breast cancer: the pathways heart study. J. Clin. Oncol. 40, 1635–1646 (2022).
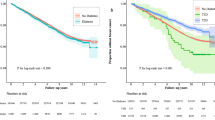
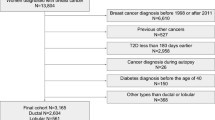
Lipscombe, L. L. et al. Association between tamoxifen treatment and diabetes: a population-based study. Cancer 118, 2615–2622 (2012).
Santorelli, M. L. et al. Hormonal therapy for breast cancer and diabetes incidence among postmenopausal women. Ann. Epidemiol. 26, 436–440 (2016).
Sun, L. M., Chen, H. J., Liang, J. A., Li, T. C. & Kao, C. H. Association of tamoxifen use and increased diabetes among Asian women diagnosed with breast cancer. Br. J. Cancer 111, 1836–1842 (2014).
Ng, H. S., Koczwara, B., Roder, D., Niyonsenga, T. & Vitry, A. Incidence of comorbidities in women with breast cancer treated with tamoxifen or an aromatase inhibitor: an Australian population-based cohort study. J. Comorb. 8, 16–24 (2018).
Ye, F. et al. The influence of hormone therapy on secondary diabetes mellitus in breast cancer: a meta-analysis. Clin. Breast Cancer 22, e48–e58 (2022).
Kim, J. E. et al. Effects of endocrine therapy on cardiovascular diseases and type 2 diabetes among breast cancer survivors: the National Health Insurance Service Database of Korea. J. Am. Heart Assoc. 11, e026743 (2022).
Choi, Y. J., Bak, K., Yeo, Y., Choi, Y. & Shin, S. Incident type 2 diabetes risk of selective estrogen receptor modulators in female patients with breast cancer. Pharmaceuticals 14, 925 (2021).
Waters, E. A., McNeel, T. S., Stevens, W. M. & Freedman, A. N. Use of tamoxifen and raloxifene for breast cancer chemoprevention in 2010. Breast Cancer Res. Treat. 134, 875–880 (2012).
Francucci, C. M. et al. Effects of raloxifene on body fat distribution and lipid profile in healthy post-menopausal women. J. Endocrinol. Invest. 28, 623–631 (2005).
Tommaselli, G. A. et al. Serum leptin levels and body composition in postmenopausal women treated with tibolone and raloxifene. Menopause 13, 660–668 (2006).
Lee, C. C., Kasa-Vubu, J. Z. & Supiano, M. A. Differential effects of raloxifene and estrogen on insulin sensitivity in postmenopausal women. J. Am. Geriatr. Soc. 51, 683–688 (2003).
Fabian, C. J. et al. Effect of bazedoxifene and conjugated estrogen (Duavee) on breast cancer risk biomarkers in high-risk women: a pilot study. Cancer Prev. Res. 12, 711–720 (2019).
Xu, B., Lovre, D. & Mauvais-Jarvis, F. The effect of selective estrogen receptor modulators on type 2 diabetes onset in women: basic and clinical insights. J. Diabetes Complicat. 31, 773–779 (2017).
Lovre, D. et al. Conjugated estrogens and bazedoxifene improve beta cell function in obese menopausal women. J. Endocr. Soc. 3, 1583–1594 (2019).
Kim, J. H. et al. Tissue-selective estrogen complexes with bazedoxifene prevent metabolic dysfunction in female mice. Mol. Metab. 3, 177–190 (2014).
Rillamas-Sun, E. et al. Development of cardiometabolic risk factors following endocrine therapy in women with breast cancer. Breast Cancer Res. Treat. 201, 117–126 (2023).
Hamood, R., Hamood, H., Merhasin, I. & Keinan-Boker, L. Diabetes after hormone therapy in breast cancer survivors: a case-cohort study. J. Clin. Oncol. 36, 2061–2069 (2018).
Sun, H. et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119 (2022).
Deutsch, A. J., Ahlqvist, E. & Udler, M. S. Phenotypic and genetic classification of diabetes. Diabetologia 65, 1758–1769 (2022).
Heilbronn, L., Smith, S. R. & Ravussin, E. Failure of fat cell proliferation, mitochondrial function and fat oxidation results in ectopic fat storage, insulin resistance and type II diabetes mellitus. Int. J. Obes. Relat. Metab. Disord. 28, S12–S21 (2004).
Ravussin, E. & Smith, S. R. Increased fat intake, impaired fat oxidation, and failure of fat cell proliferation result in ectopic fat storage, insulin resistance, and type 2 diabetes mellitus. Ann. NY Acad. Sci. 967, 363–378 (2002).
Yang, X. & Smith, U. Adipose tissue distribution and risk of metabolic disease: does thiazolidinedione-induced adipose tissue redistribution provide a clue to the answer. Diabetologia 50, 1127–1139 (2007).
Elks, M. L. Fat oxidation and diabetes of obesity: the Randle hypothesis revisited. Med. Hypotheses 33, 257–260 (1990).
Iyengar, N. M. et al. Metabolic obesity, adipose inflammation and elevated breast aromatase in women with normal body mass index. Cancer Prev. Res. 10, 235–243 (2017).
Iyengar, N. M., Gucalp, A., Dannenberg, A. J. & Hudis, C. A. Obesity and cancer mechanisms: tumor microenvironment and inflammation. J. Clin. Oncol. 34, 4270–4276 (2016).
Huang, H. et al. The immunomodulatory effects of endocrine therapy in breast cancer. J. Exp. Clin. Cancer Res. 40, 19 (2021).
Akyol, M. et al. The effects of adjuvant endocrine treatment on serum leptin, serum adiponectin and body composition in patients with breast cancer: the Izmir Oncology Group (IZOG) study. Chemotherapy 61, 57–64 (2016).
Ghaben, A. L. & Scherer, P. E. Adipogenesis and metabolic health. Nat. Rev. Mol. Cell Biol. 20, 242–258 (2019).
White, U., Fitch, M. D., Beyl, R. A., Hellerstein, M. K. & Ravussin, E. Adipose depot-specific effects of 16 weeks of pioglitazone on in vivo adipogenesis in women with obesity: a randomised controlled trial. Diabetologia 64, 159–167 (2021).
Giles, E. D. & Wellberg, E. A. Preclinical models to study obesity and breast cancer in females: considerations, caveats, and tools. J. Mammary Gland. Biol. Neoplasia 25, 237–253 (2020).
Estrada-Meza, J. et al. Tamoxifen treatment in the neonatal period affects glucose homeostasis in adult mice in a sex-dependent manner. Endocrinology 162, bqab098 (2021).
Hesselbarth, N. et al. Tamoxifen affects glucose and lipid metabolism parameters, causes browning of subcutaneous adipose tissue and transient body composition changes in C57BL/6NTac mice. Biochem. Biophys. Res. Commun. 464, 724–729 (2015).
Liu, L. et al. Tamoxifen reduces fat mass by boosting reactive oxygen species. Cell Death Dis. 6, e1586 (2015).
Liu, Z. et al. Short-term tamoxifen treatment has long-term effects on metabolism in high-fat diet-fed mice with involvement of Nmnat2 in POMC neurons. FEBS Lett. 592, 3305–3316 (2018).
Ye, R. et al. Impact of tamoxifen on adipocyte lineage tracing: inducer of adipogenesis and prolonged nuclear translocation of Cre recombinase. Mol. Metab. 4, 771–778 (2015).
Zhao, L. et al. Even a low dose of tamoxifen profoundly induces adipose tissue browning in female mice. Int. J. Obes. 44, 226–234 (2020).
Pike, S. et al. In vitro effects of tamoxifen on adipose-derived stem cells. Wound Repair Regen. 23, 728–736 (2015).
Stout, M. B., Scalzo, R. L. & Wellberg, E. A. Persistent metabolic effects of tamoxifen: considerations for an experimental tool and clinical breast cancer treatment. Endocrinology 162, bqab126 (2021).
Guillaume, M. et al. Selective activation of estrogen receptor alpha activation function-1 is sufficient to prevent obesity, steatosis, and insulin resistance in mouse. Am. J. Pathol. 187, 1273–1287 (2017).
Scalzo, R. L. et al. Breast cancer endocrine therapy promotes weight gain with distinct adipose tissue effects in lean and obese female mice. Endocrinology 162, bqab174 (2021).
Johansson, H. et al. Effect of fenretinide and low-dose tamoxifen on insulin sensitivity in premenopausal women at high risk for breast cancer. Cancer Res. 68, 9512–9518 (2008).
Butera, P. C. Estradiol and the control of food intake. Physiol. Behav. 99, 175–180 (2010).
Fagerberg, L. et al. Analysis of the human tissue-specific expression by genome-wide integration of transcriptomics and antibody-based proteomics. Mol. Cell Proteom. 13, 397–406 (2014).
Heine, P. A., Taylor, J. A., Iwamoto, G. A., Lubahn, D. B. & Cooke, P. S. Increased adipose tissue in male and female estrogen receptor-alpha knockout mice. Proc. Natl Acad. Sci. USA 97, 12729–12734 (2000).
Jones, M. E. et al. Aromatase-deficient (ArKO) mice have a phenotype of increased adiposity. Proc. Natl Acad. Sci. USA 97, 12735–12740 (2000).
Stubbins, R. E., Holcomb, V. B., Hong, J. & Nunez, N. P. Estrogen modulates abdominal adiposity and protects female mice from obesity and impaired glucose tolerance. Eur. J. Nutr. 51, 861–870 (2012).
Manrique, C. et al. Loss of estrogen receptor alpha signaling leads to insulin resistance and obesity in young and adult female mice. Cardiorenal Med. 2, 200–210 (2012).
Bryzgalova, G. et al. Evidence that oestrogen receptor-alpha plays an important role in the regulation of glucose homeostasis in mice: insulin sensitivity in the liver. Diabetologia 49, 588–597 (2006).
Sharma, G. & Prossnitz, E. R. GPER/GPR30 knockout mice: effects of GPER on metabolism. Methods Mol. Biol. 1366, 489–502 (2016).
Sharma, G. & Prossnitz, E. R. G-protein-coupled estrogen receptor (GPER) and sex-specific metabolic homeostasis. Adv. Exp. Med. Biol. 1043, 427–453 (2017).
Ribas, V. et al. Skeletal muscle action of estrogen receptor alpha is critical for the maintenance of mitochondrial function and metabolic homeostasis in females. Sci. Transl Med. 8, 334ra354 (2016).
Inigo, M. R. et al. Estrogen receptor-alpha in female skeletal muscle is not required for regulation of muscle insulin sensitivity and mitochondrial regulation. Mol. Metab. 34, 1–15 (2020).
Zhou, Z. et al. Estrogen receptor α controls metabolism in white and brown adipocytes by regulating Polg1 and mitochondrial remodeling. Sci. Transl Med. 12, eaax8096 (2020).
Liu, Q. et al. Inhibitory effect of 17beta-estradiol on triglyceride synthesis in skeletal muscle cells is dependent on ESR1 and not ESR2. Mol. Med. Rep. 19, 5087–5096 (2019).
Collins, B. C. et al. Estrogen regulates the satellite cell compartment in females. Cell Rep. 28, 368–381.e6 (2019).
Kitajima, Y. & Ono, Y. Estrogens maintain skeletal muscle and satellite cell functions. J. Endocrinol. 229, 267–275 (2016).
Shao, X. et al. The asymmetrical ESR1 signaling in muscle progenitor cells determines the progression of adolescent idiopathic scoliosis. Cell Discov. 9, 44 (2023).
Barros, R. P., Machado, U. F., Warner, M. & Gustafsson, J. A. Muscle GLUT4 regulation by estrogen receptors ERbeta and ERalpha. Proc. Natl Acad. Sci. USA 103, 1605–1608 (2006).
Barros, R. P., Gabbi, C., Morani, A., Warner, M. & Gustafsson, J. A. Participation of ERalpha and ERbeta in glucose homeostasis in skeletal muscle and white adipose tissue. Am. J. Physiol. Endocrinol. Metab. 297, E124–E133 (2009).
Sharma, G. & Prossnitz, E. R. Targeting the G protein-coupled estrogen receptor (GPER) in obesity and diabetes. Endocr. Metab. Sci. 2, 100080 (2021).
Hevener, A. L., Zhou, Z., Drew, B. G. & Ribas, V. The role of skeletal muscle estrogen receptors in metabolic homeostasis and insulin sensitivity. Adv. Exp. Med. Biol. 1043, 257–284 (2017).
Alonso-Magdalena, P. et al. Pancreatic insulin content regulation by the estrogen receptor ER alpha. PLoS ONE 3, e2069 (2008).
Balhuizen, A., Kumar, R., Amisten, S., Lundquist, I. & Salehi, A. Activation of G protein-coupled receptor 30 modulates hormone secretion and counteracts cytokine-induced apoptosis in pancreatic islets of female mice. Mol. Cell. Endocrinol. 320, 16–24 (2010).
Kumar, R., Balhuizen, A., Amisten, S., Lundquist, I. & Salehi, A. Insulinotropic and antidiabetic effects of 17β-estradiol and the GPR30 agonist G-1 on human pancreatic islets. Endocrinology 152, 2568–2579 (2011).
Le May, C. et al. Estrogens protect pancreatic beta-cells from apoptosis and prevent insulin-deficient diabetes mellitus in mice. Proc. Natl Acad. Sci. USA 103, 9232–9237 (2006).
Sharma, G. & Prossnitz, E. R. Mechanisms of estradiol-induced insulin secretion by the G protein-coupled estrogen receptor GPR30/GPER in pancreatic beta-cells. Endocrinology 152, 3030–3039 (2011).
Tiano, J. & Mauvais-Jarvis, F. Selective estrogen receptor modulation in pancreatic β-cells and the prevention of type 2 diabetes. Islets 4, 173–176 (2012).
Tiano, J. P. et al. Estrogen receptor activation reduces lipid synthesis in pancreatic islets and prevents β cell failure in rodent models of type 2 diabetes. J. Clin. Invest. 121, 3331–3342 (2011).
Musatov, S. et al. Silencing of estrogen receptor alpha in the ventromedial nucleus of hypothalamus leads to metabolic syndrome. Proc. Natl Acad. Sci. USA 104, 2501–2506 (2007).
Correa, S. M. et al. An estrogen-responsive module in the ventromedial hypothalamus selectively drives sex-specific activity in females. Cell Rep. 10, 62–74 (2015).
Zhang, Z. et al. Estrogen receptor alpha in the brain mediates tamoxifen-induced changes in physiology in mice. eLife 10, e63333 (2021).
Lopez, M. et al. Tamoxifen-induced anorexia is associated with fatty acid synthase inhibition in the ventromedial nucleus of the hypothalamus and accumulation of malonyl-CoA. Diabetes 55, 1327–1336 (2006).
Wade, G. N. & Heller, H. W. Tamoxifen mimics the effects of estradiol on food intake, body weight, and body composition in rats. Am. J. Physiol. 264, R1219–R1223 (1993).
Palmisano, B. T., Zhu, L. & Stafford, J. M. Role of estrogens in the regulation of liver lipid metabolism. Adv. Exp. Med. Biol. 1043, 227–256 (2017).
Zhu, L. et al. Estrogen treatment after ovariectomy protects against fatty liver and may improve pathway-selective insulin resistance. Diabetes 62, 424–434 (2013).
Hart-Unger, S. et al. Hormone signaling and fatty liver in females: analysis of estrogen receptor alpha mutant mice. Int. J. Obes. 41, 945–954 (2017).
Cole, L. K., Jacobs, R. L. & Vance, D. E. Tamoxifen induces triacylglycerol accumulation in the mouse liver by activation of fatty acid synthesis. Hepatology 52, 1258–1265 (2010).
Larosche, I. et al. Tamoxifen inhibits topoisomerases, depletes mitochondrial DNA, and triggers steatosis in mouse liver. J. Pharmacol. Exp. Ther. 321, 526–535 (2007).
Saavedra-Pena, R. D. M., Taylor, N., Flannery, C. & Rodeheffer, M. S. Estradiol cycling drives female obesogenic adipocyte hyperplasia. Cell Rep. 42, 112390 (2023).
Jeffery, E. et al. The adipose tissue microenvironment regulates depot-specific adipogenesis in obesity. Cell Metab. 24, 142–150 (2016).
Acknowledgements
The authors are grateful for the guidance of S. Wright-Hobart, a breast cancer survivor and patient advocate. Her experience with breast cancer therapy and that of her fellow survivors provide a critical perspective and inspired this line of work in our laboratories. N.S.T. acknowledges the support of the Harold Hamm Diabetes Center and Stephenson Cancer Center postdoctoral fellowship, and E.A.W. acknowledges the support of the Human Environmental Sciences Institute THRIVE grant.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks Emily Gallagher and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ArrayExpress: www.ebi.ac.uk/arrayexpress/
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thomas, N.S., Scalzo, R.L. & Wellberg, E.A. Diabetes mellitus in breast cancer survivors: metabolic effects of endocrine therapy. Nat Rev Endocrinol 20, 16–26 (2024). https://doi.org/10.1038/s41574-023-00899-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-023-00899-0