Abstract
The adrenal gland is a source of sex steroid precursors, and its activity is particularly relevant during fetal development and adrenarche. Following puberty, the synthesis of androgens by the adrenal gland has been considered of little physiologic importance. Dehydroepiandrosterone (DHEA) and its sulfate, DHEAS, are the major adrenal androgen precursors, but they are biologically inactive. The second most abundant unconjugated androgen produced by the human adrenals is 11β-hydroxyandrostenedione (11OHA4). 11-Ketotestosterone, a downstream metabolite of 11OHA4 (which is mostly produced in peripheral tissues), and its 5α-reduced product, 11-ketodihydrotestosterone, are bioactive androgens, with potencies equivalent to those of testosterone and dihydrotestosterone. These adrenal-derived androgens all share an oxygen atom on carbon 11, so we have collectively termed them 11-oxyandrogens. Over the past decade, these androgens have emerged as major components of several disorders of androgen excess, such as congenital adrenal hyperplasia, premature adrenarche and polycystic ovary syndrome, as well as in androgen-dependent tumours, such as castration-resistant prostate cancer. Moreover, in contrast to the more extensively studied, traditional androgens, circulating concentrations of 11-oxyandrogens do not demonstrate an age-dependent decline. This Review focuses on the rapidly expanding knowledge regarding the implications of 11-oxyandrogens in human physiology and disease.
Key points
Dehydroepiandrosterone (DHEA) and its sulfate, DHEAS, are the most abundant adrenal androgen precursors, but they are biologically inactive as androgens.
The adrenal gland is the primary source of a set of 11-oxygenated 19-carbon steroids, also termed 11-oxyandrogens, which have several roles in human physiology and disease.
11-Ketotestosterone is a bioactive 11-oxyandrogen, with a potency similar to that of testosterone, and its concentrations exceed those of testosterone in prepubertal children and in postmenopausal women.
Concentrations of 11-oxyandrogens are elevated in several disorders of androgen excess, including premature adrenarche, congenital adrenal hyperplasia and polycystic ovary syndrome, and they can contribute to the progression of castration-resistant prostate cancer.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
White, P. C. & Speiser, P. W. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Endocr. Rev. 21, 245–291 (2000).
Doberne, Y., Levine, L. S. & New, M. I. Elevated urinary testosterone and androstanediol in precocious adrenarche. Pediatric Res. 9, 794–797 (1975).
Korth-Schutz, S., Levine, L. S. & New, M. I. Evidence for the adrenal source of androgens in precocious adrenarche. Acta Endocrinol. 82, 342–352 (1976).
Azziz, R., Black, V., Hines, G. A., Fox, L. M. & Boots, L. R. Adrenal androgen excess in the polycystic ovary syndrome: sensitivity and responsivity of the hypothalamic–pituitary–adrenal axis. J. Clin. Endocrinol. Metab. 83, 2317–2323 (1998).
Else, T. et al. Adrenocortical carcinoma. Endocr. Rev. 35, 282–326 (2014).
Sharifi, N. Minireview: androgen metabolism in castration-resistant prostate cancer. Mol. Endocrinol. 27, 708–714 (2013).
Rege, J. et al. Liquid chromatography–tandem mass spectrometry analysis of human adrenal vein 19-carbon steroids before and after ACTH stimulation. J. Clin. Endocrinol. Metab. 98, 1182–1188 (2013).
Turcu, A. F. et al. Adrenal-derived 11-oxygenated 19-carbon steroids are the dominant androgens in classic 21-hydroxylase deficiency. Eur. J. Endocrinol. 174, 601–609 (2016).
Miller, W. L. & Auchus, R. J. The molecular biology, biochemistry, and physiology of human steroidogenesis and its disorders. Endocr. Rev. 32, 81–151 (2011).
Clark, B. J., Wells, J., King, S. R. & Stocco, D. M. The purification, cloning and expression of a novel luteinizing hormone-induced mitochondrial protein in MA-10 mouse Leydig tumor cells. Characterization of the steroidogenic acute regulatory protein (StAR). J. Biol. Chem. 269, 28314–28322 (1994).
Stocco, D. M. & Clark, B. J. Regulation of the acute production of steroids in steroidogenic cells. Endocr. Rev. 17, 221–244 (1996).
Sugawara, T. et al. Human steroidogenic acute regulatory protein: functional activity in COS-1 cells, tissue-specific expression, and mapping of the structural gene to 8p11.2 and a pseudogene to chromosome 13. Proc. Natl Acad. Sci. USA 92, 4778–4782 (1995).
Granot, Z. et al. Proteolysis of normal and mutated steroidogenic acute regulatory proteins in the mitochondria: the fate of unwanted proteins. Mol. Endocrinol. 17, 2461–2476 (2003).
Artemenko, I. P., Zhao, D., Hales, D. B., Hales, K. H. & Jefcoate, C. R. Mitochondrial processing of newly synthesized steroidogenic acute regulatory protein (StAR), but not total StAR, mediates cholesterol transfer to cytochrome P450 side chain cleavage enzyme in adrenal cells. J. Biol. Chem. 276, 46583–46596 (2001).
Tsujishita, Y. & Hurley, J. H. Structure and lipid transport mechanism of a StAR-related domain. Nat. Struct. Biol. 7, 408–414 (2000).
Anuka, E., Gal, M., Stocco, D. M. & Orly, J. Expression and roles of steroidogenic acute regulatory (StAR) protein in ‘non-classical’, extra-adrenal and extra-gonadal cells and tissues. Mol. Cell. Endocrinol. 371, 47–61 (2013).
Koritz, S. B. & Kumar, A. M. On the mechanism of action of the adrenocorticotrophic hormone. The stimulation of the activity of enzymes involved in pregnenolone synthesis. J. Biol. Chem. 245, 152–159 (1970).
Shikita, M. & Hall, P. F. The stoichiometry of the conversion of cholesterol and hydroxycholesterols to pregnenolone (3β-hydroxypregn-5-en-20-one) catalysed by adrenal cytochrome P-450. Proc. Natl Acad. Sci. USA 71, 1441–1445 (1974).
Shimizu, K., Hayano, M., Gut, M. & Dorfman, R. I. The transformation of 20α-hydroxcholesterol to isocaproic acid and C21 steroids. J. Biol. Chem. 236, 695–699 (1961).
John, M. E., John, M. C., Boggaram, V., Simpson, E. R. & Waterman, M. R. Transcriptional regulation of steroid hydroxylase genes by corticotropin. Proc. Natl Acad. Sci. USA 83, 4715–4719 (1986).
Reiter, E. O., Fuldauer, V. G. & Root, A. W. Secretion of the adrenal androgen, dehydroepiandrosterone sulfate, during normal infancy, childhood, and adolescence, in sick infants, and in children with endocrinologic abnormalities. J. Pediatr. 90, 766–770 (1977).
Zuber, M. X., Simpson, E. R. & Waterman, M. R. Expression of bovine 17α-hydroxylase cytochrome P450 cDNA in non-steroidogenic (COS-1) cells. Science 234, 1258–1261 (1986).
Chung, B. C. et al. Cytochrome P450c17 (steroid 17α-hydroxylase/17,20 lyase): cloning of human adrenal and testis cDNAs indicates the same gene is expressed in both tissues. Proc. Natl Acad. Sci. USA 84, 407–411 (1987).
Kagimoto, M., Winter, J. S., Kagimoto, K., Simpson, E. R. & Waterman, M. R. Structural characterization of normal and mutant human steroid 17α-hydroxylase genes: molecular basis of one example of combined 17α-hydroxylase/17,20 lyase deficiency. Mol. Endocrinol. 2, 564–570 (1988).
Yasukochi, Y. & Masters, B. S. Some properties of a detergent-solubilized NADPH-cytochrome c (cytochrome P-450) reductase purified by biospecific affinity chromatography. J. Biol. Chem. 251, 5337–5344 (1976).
Flück, C. E., Miller, W. L. & Auchus, R. J. The 17,20-lyase activity of cytochrome P450c17 from human fetal testis favors the Δ5 steroidogenic pathway. J. Clin. Endocrinol. Metab. 88, 3762–3766 (2003).
Imai, T., Globerman, H., Gertner, J. M., Kagawa, N. & Waterman, M. R. Expression and purification of functional human 17α-hydroxylase/17,20-lyase (P450c17) in Escherichia coli. Use of this system for study of a novel form of combined 17α-hydroxylase/17,20-lyase deficiency. J. Biol. Chem. 268, 19681–19689 (1993).
Onoda, M. & Hall, P. F. Cytochrome b 5 stimulates purified testicular microsomal cytochrome P450 (C21 side-chain cleavage). Biochem. Biophys. Res. Commun. 108, 454–460 (1982).
Auchus, R. J., Lee, T. C. & Miller, W. L. Cytochrome b 5 augments the 17,20 lyase activity of human P450c17 without direct electron transfer. J. Biol. Chem. 273, 3158–3165 (1998).
Katagiri, M., Kagawa, N. & Waterman, M. R. The role of cytochrome b 5 in the biosynthesis of androgens by human P450c17. Arch. Biochem. Biophys. 317, 343–347 (1995).
Lee-Robichaud, P., Wright, J. N., Akhtar, M. E. & Akhtar, M. Modulation of the activity of human 17α-hydroxylase-17,20-lyase (CYP17) by cytochrome b 5: endocrinological and mechanistic implications. Biochem. J. 308, 901–908 (1995).
Peng, H. M. et al. Cytochrome b5 activates the 17,20-lyase activity of human cytochrome P450 17A1 by increasing the coupling of NADPH consumption to androgen production. Biochemistry 55, 4356–4365 (2016).
Simpson, E. R. et al. Regulation of the biosynthesis of steroidogenic enzymes. J. Steroid Biochem. 27, 801–805 (1987).
Zuber, M. X., John, M. E., Okamura, T., Simpson, E. R. & Waterman, M. R. Bovine adrenocortical cytochrome P-450(17α). Regulation of gene expression by ACTH and elucidation of primary sequence. J. Biol. Chem. 261, 2475–2482 (1986).
Kristiansen, S. B., Endoh, A., Casson, P. R., Buster, J. E. & Hornsby, P. J. Induction of steroidogenic enzyme genes by insulin and IGF-I in cultured adult human adrenocortical cells. Steroids 62, 258–265 (1997).
Lebrethon, M. C., Jaillard, C., Naville, D., Begeot, M. & Saez, J. M. Effects of transforming growth factor-β1 on human adrenocortical fasciculata–reticularis cell differentiated functions. J. Clin. Endocrinol. Metab. 79, 1033–1039 (1994).
Penhoat, A., Rainey, W. E., Viard, I. & Saez, J. M. Regulation of adrenal cell-differentiated functions by growth factors. Hormone Res. 42, 39–43 (1994).
Mapes, S., Corbin, C. J., Tarantal, A. & Conley, A. The primate adrenal zona reticularis is defined by expression of cytochrome b 5, 17α-hydroxylase/17,20-lyase cytochrome P450 (P450c17) and NADPH-cytochrome P450 reductase (reductase) but not 3β-hydroxysteroid dehydrogenase/Δ5–4 isomerase (3β-HSD). J. Clin. Endocrinol. Metab. 84, 3382–3385 (1999).
Suzuki, T. et al. Developmental changes in steroidogenic enzymes in human postnatal adrenal cortex: immunohistochemical studies. Clin. Endocrinol. 53, 739–747 (2000).
Rege, J. et al. Age-dependent increases in adrenal cytochrome b 5 and serum 5-androstenediol-3-sulfate. J. Clin. Endocrinol. Metab. 101, 4585–4593 (2016).
Otterness, D. M. et al. Human dehydroepiandrosterone sulfotransferase gene: molecular cloning and structural characterization. DNA Cell Biol. 14, 331–341 (1995).
Rainey, W. E., Rehman, K. S. & Carr, B. R. The human fetal adrenal: making adrenal androgens for placental estrogens. Semin. Reprod. Med. 22, 327–336 (2004).
Nakamura, Y., Gang, H. X., Suzuki, T., Sasano, H. & Rainey, W. E. Adrenal changes associated with adrenarche. Rev. Endocr. Metab. Disord. 10, 19–26 (2009).
Noordam, C. et al. Inactivating PAPSS2 mutations in a patient with premature pubarche. N. Engl. J. Med. 360, 2310–2318 (2009).
Weinshilboum, R. M. et al. Sulfation and sulfotransferases 1: sulfotransferase molecular biology: cDNAs and genes. FASEB J. 11, 3–14 (1997).
Strott, C. A. Sulfonation and molecular action. Endocr. Rev. 23, 703–732 (2002).
Rege, J. et al. Adrenocorticotropin acutely regulates pregnenolone sulfate production by the human adrenal in vivo and in vitro. J. Clin. Endocrinol. Metab. 103, 320–327 (2018).
Rege, J. et al. Transcriptome profiling reveals differentially expressed transcripts between the human adrenal zona fasciculata and zona reticularis. J. Clin. Endocrinol. Metab. 99, E518–E527 (2014).
Endoh, A., Kristiansen, S. B., Casson, P. R., Buster, J. E. & Hornsby, P. J. The zona reticularis is the site of biosynthesis of dehydroepiandrosterone and dehydroepiandrosterone sulfate in the adult human adrenal cortex resulting from its low expression of 3β-hydroxysteroid dehydrogenase. J. Clin. Endocrinol. Metab. 81, 3558–3565 (1996).
Baulieu, E. E. Dehydroepiandrosterone (DHEA): a fountain of youth? J. Clin. Endocrinol. Metab. 81, 3147–3151 (1996).
Buster, J. E., Abraham, G. E., Kyle, F. W. & Marshall, J. R. Serum steroid levels following a large intravenous dose of a steroid sulfate precursor during the second trimester of human pregnancy. II. Pregnenolone sulfate. J. Clin. Endocrinol. Metab. 38, 1038–1045 (1974).
Longcope, C. Dehydroepiandrosterone metabolism. J. Endocrinol. 150, S125–S127 (1996).
Fischli, S. et al. Dehydroepiandrosterone sulfate in the assessment of the hypothalamic–pituitary–adrenal axis. J. Clin. Endocrinol. Metab. 93, 539–542 (2008).
Nasrallah, M. P. & Arafah, B. M. The value of dehydroepiandrosterone sulfate measurements in the assessment of adrenal function. J. Clin. Endocrinol. Metab. 88, 5293–5298 (2003).
Sayyed Kassem, L., El Sibai, K., Chaiban, J., Abdelmannan, D. & Arafah, B. M. Measurements of serum DHEA and DHEA sulphate levels improve the accuracy of the low-dose cosyntropin test in the diagnosis of central adrenal insufficiency. J. Clin. Endocrinol. Metab. 97, 3655–3662 (2012).
Dennedy, M. C. et al. Low DHEAS: a sensitive and specific test for detection of subclinical hypercortisolism in adrenal incidentalomas. J. Clin. Endocrinol. Metab. 102, 786–792 (2017).
Yener, S., Yilmaz, H., Demir, T., Secil, M. & Comlekci, A. DHEAS for the prediction of subclinical Cushing’s syndrome: perplexing or advantageous? Endocrine 48, 669–676 (2015).
Vaiani, E. et al. Central adrenal insufficiency could not be confirmed by measurement of basal serum DHEAS levels in pubertal children. Horm. Res. Paediatr. 82, 332–337 (2014).
Bencsik, Z. et al. Low dehydroepiandrosterone sulfate (DHEA-S) level is not a good predictor of hormonal activity in nonselected patients with incidentally detected adrenal tumors. J. Clin. Endocrinol. Metab. 81, 1726–1729 (1996).
Thomas, J. L., Myers, R. P. & Strickler, R. C. Human placental 3β-hydroxy-5-ene-steroid dehydrogenase and steroid 5–4-ene-isomerase: purification from mitochondria and kinetic profiles, biophysical characterization of the purified mitochondrial and microsomal enzymes. J. Steroid Biochem. 33, 209–217 (1989).
Lachance, Y. et al. Characterization of human 3β-hydroxysteroid dehydrogenase/Δ5–Δ4-isomerase gene and its expression in mammalian cells. J. Biol. Chem. 265, 20469–20475 (1990).
Lorence, M. C., Murry, B. A., Trant, J. M. & Mason, J. I. Human 3β-hydroxysteroid dehydrogenase/Δ5–4 isomerase from placenta: expression in nonsteroidogenic cells of a protein that catalyzes the dehydrogenation/isomerization of C21 and C19 steroids. Endocrinology 126, 2493–2498 (1990).
Thomas, J. L., Myers, R. P. & Strickler, R. C. Human placental 3β-hydroxy-5-ene-steroid dehydrogenase and steroid 5/4-ene-isomerase: purification from mitochondria and kinetic profiles, biophysical characterization of the purified mitochondrial and microsomal enzymes. J. Steroid Biochem. 33, 209–217 (1989).
Lee, T. C., Miller, W. L. & Auchus, R. J. Medroxyprogesterone acetate and dexamethasone are competitive inhibitors of different human steroidogenic enzymes. J. Clin. Endocrinol. Metab. 84, 2104–2110 (1999).
Labrie, F., Simard, J., Luu-The, V., Belanger, A. & Pelletier, G. Structure, function and tissue-specific gene expression of 3β-hydroxysteroid dehydrogenase/5-ene-4-ene isomerase enzymes in classical and peripheral intracrine steroidogenic tissues. J. Steroid Biochem. Mol. Biol. 43, 805–826 (1992).
Lachance, Y. et al. Structure of the human type II 3β-hydroxysteroid dehydrogenase/Δ5–Δ4 isomerase (3β-HSD) gene: adrenal and gonadal specificity. DNA Cell Biol. 10, 701–711 (1991).
Luu The, V. et al. Full length cDNA structure and deduced amino acid sequence of human 3β-hydroxy-5-ene steroid dehydrogenase. Mol. Endocrinol. 3, 1310–1312 (1989).
Nakamura, Y. et al. 3βHSD and CYB5A double positive adrenocortical cells during adrenal development/aging. Endocr. Res. 40, 8–13 (2015).
Geissler, W. M. et al. Male pseudohermaphroditism caused by mutations of testicular 17β-hydroxysteroid dehydrogenase 3. Nat. Genet. 7, 34–39 (1994).
Nakamura, Y. et al. Type 5 17β-hydroxysteroid dehydrogenase (AKR1C3) contributes to testosterone production in the adrenal reticularis. J. Clin. Endocrinol. Metab. 94, 2192–2198 (2009).
Dufort, I., Rheault, P., Huang, X. F., Soucy, P. & Luu-The, V. Characteristics of a highly labile human type 5 17β-hydroxysteroid dehydrogenase. Endocrinology 140, 568–574 (1999).
Deyashiki, Y. et al. Molecular cloning of two human liver 3α-hydroxysteroid/dihydrodiol dehydrogenase isoenzymes that are identical with chlordecone reductase and bile-acid binder. Biochem. J. 299, 545–552 (1994).
Lin, H. K. et al. Expression and characterization of recombinant type 2 3α-hydroxysteroid dehydrogenase (HSD) from human prostate: demonstration of bifunctional 3α/17β-HSD activity and cellular distribution. Mol. Endocrinol. 11, 1971–1984 (1997).
Qin, K., Ehrmann, D. A., Cox, N., Refetoff, S. & Rosenfield, R. L. Identification of a functional polymorphism of the human type 5 17β-hydroxysteroid dehydrogenase gene associated with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 91, 270–276 (2006).
Mornet, E., Dupont, J., Vitek, A. & White, P. C. Characterization of two genes encoding human steroid 11β-hydroxylase (P-450(11)β). J. Biol. Chem. 264, 20961–20967 (1989).
Imamichi, Y. et al. 11-Ketotestosterone is a major androgen produced in human gonads. J. Clin. Endocrinol. Metab. 101, 3582–3591 (2016).
Axelrod, L. R., Kraemer, D. C., Burdett, J. Jr. & Goldzieher, J. W. Biosynthesis of 11-hydroxyandrostenedione by human and baboon adrenals. Acta Endocrinol. 72, 545–550 (1973).
Penning, T. M., Wangtrakuldee, P. & Auchus, R. J. Structural and functional biology of aldo-keto reductase steroid-transforming enzymes. Endocr. Rev. 40, 447–475 (2019).
Barnard, M. et al. 11-Oxygenated androgen precursors are the preferred substrates for aldo-keto reductase 1C3 (AKR1C3): implications for castration resistant prostate cancer. J. Steroid Biochem. Mol. Biol. 183, 192–201 (2018).
Storbeck, K. H. et al. 11β-Hydroxydihydrotestosterone and 11-ketodihydrotestosterone, novel C19 steroids with androgenic activity: a putative role in castration resistant prostate cancer? Mol. Cell. Endocrinol. 377, 135–146 (2013).
Andersson, S. & Russell, D. W. Structural and biochemical properties of cloned and expressed human and rat steroid 5α-reductases. Proc. Natl Acad. Sci. USA 87, 3640–3644 (1990).
Rosemberg, E. & Dorfman, R. I. Biological activity of 9α-fluoro-11β-hydroxy-Δ4-androstene-3,17-dione. Proc. Soc. Exp. Biol. Med. 99, 336–338 (1958).
Dorfman, R. I., Rooks, W. H. II, Jones, J. B. & Leman, J. D. Androgenic activity of highly purified 5α-androstane and 5α-androstan-17β-ol. J. Med. Chem. 9, 930–931 (1966).
Campana, C. et al. Development of a novel cell based androgen screening model. J. Steroid Biochem. Mol. Biol. 156, 17–22 (2016).
Rege, J. et al. 11-Ketotestosterone is the dominant circulating bioactive androgen during normal and premature adrenarche. J. Clin. Endocrinol. Metab. 103, 4589–4598 (2018).
Pretorius, E. et al. 11-Ketotestosterone and 11-ketodihydrotestosterone in castration resistant prostate cancer: potent androgens which can no longer be ignored. PLoS One 11, e0159867 (2016).
Rainey, W. E., Carr, B. R., Sasano, H., Suzuki, T. & Mason, J. I. Dissecting human adrenal androgen production. Trends Endocrinol. Metab. 13, 234–239 (2002).
Cutler, G. B. Jr. & Loriaux, D. L. Andrenarche and its relationship to the onset of puberty. Fed. Proc. 39, 2384–2390 (1980).
Havelock, J. C., Auchus, R. J. & Rainey, W. E. The rise in adrenal androgen biosynthesis: adrenarche. Semin. Reprod. Med. 22, 337–347 (2004).
Hui, X. G. et al. Development of the human adrenal zona reticularis: morphometric and immunohistochemical studies from birth to adolescence. J. Endocrinol. 203, 241–252 (2009).
Remer, T., Boye, K. R., Hartmann, M. F. & Wudy, S. A. Urinary markers of adrenarche: reference values in healthy subjects, aged 3–18 years. J. Clin. Endocrinol. Metab. 90, 2015–2021 (2005).
Korth-Schutz, S., Levine, L. S. & New, M. I. Dehydroepiandrosterone sulfate (DS) levels, a rapid test for abnormal adrenal androgen secretion. J. Clin. Endocrinol. Metab. 42, 1005–1013 (1976).
Korth-Schutz, S., Levine, L. S. & New, M. I. Serum androgens in normal prepubertal and pubertal children and in children with precocious adrenarche. J. Clin. Endocrinol. Metab. 42, 117–124 (1976).
Guran, T. et al. Reference values for serum dehydroepiandrosterone-sulphate in healthy children and adolescents with emphasis on the age of adrenarche and pubarche. Clin. Endocrinol. 82, 712–718 (2015).
Rosenfield, R. L. & Lucky, A. W. Acne, hirsutism, and alopecia in adolescent girls. Clinical expressions of androgen excess. Endocrinol. Metab. Clin. North Am. 22, 507–532 (1993).
Arlt, W. et al. Dehydroepiandrosterone replacement in women with adrenal insufficiency. N. Engl. J. Med. 341, 1013–1020 (1999).
Arlt, W. et al. Oral dehydroepiandrosterone for adrenal androgen replacement: pharmacokinetics and peripheral conversion to androgens and estrogens in young healthy females after dexamethasone suppression. J. Clin. Endocrinol. Metab. 83, 1928–1934 (1998).
Ke, Y. et al. Serum levels of sex steroids and metabolites following 12 weeks of intravaginal 0.50% DHEA administration. J. Steroid Biochem. Mol. Biol. 154, 186–196 (2015).
Labrie, F. et al. Effect of intravaginal DHEA on serum DHEA and eleven of its metabolites in postmenopausal women. J. Steroid Biochem. Mol. Biol. 111, 178–194 (2008).
O’Reilly, M. W. et al. AKR1C3-mediated adipose androgen generation drives lipotoxicity in women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 102, 3327–3339 (2017).
Swart, A. C. & Storbeck, K. H. 11β-Hydroxyandrostenedione: downstream metabolism by 11βHSD, 17βHSD and SRD5A produces novel substrates in familiar pathways. Mol. Cell. Endocrinol. 408, 114–123 (2015).
Kroboth, P. D., Salek, F. S., Pittenger, A. L., Fabian, T. J. & Frye, R. F. DHEA and DHEA-S: a review. J. Clin. Pharmacol. 39, 327–348 (1999).
Kirschner, M. A. & Bardin, C. W. Androgen production and metabolism in normal and virilized women. Metabolism 21, 667–688 (1972).
Abraham, G. E. Ovarian and adrenal contribution to peripheral androgens during the menstrual cycle. J. Clin. Endocrinol. Metab. 39, 340–346 (1974).
Longcope, C. Adrenal and gonadal androgen secretion in normal females. Clin. Endocrinol. Metab. 15, 213–228 (1986).
Eisenhofer, G. et al. Reference intervals for plasma concentrations of adrenal steroids measured by LC-MS/MS: impact of gender, age, oral contraceptives, body mass index and blood pressure status. Clin. Chim. Acta 470, 115–124 (2017).
Elmlinger, M. W., Kuhnel, W., Wormstall, H. & Doller, P. C. Reference intervals for testosterone, androstenedione and SHBG levels in healthy females and males from birth until old age. Clin. Lab. 51, 625–632 (2005).
Rothman, M. S. et al. Reexamination of testosterone, dihydrotestosterone, estradiol and estrone levels across the menstrual cycle and in postmenopausal women measured by liquid chromatography–tandem mass spectrometry. Steroids 76, 177–182 (2011).
Davison, S. L., Bell, R., Donath, S., Montalto, J. G. & Davis, S. R. Androgen levels in adult females: changes with age, menopause, and oophorectomy. J. Clin. Endocrinol. Metab. 90, 3847–3853 (2005).
Haring, R. et al. Age-specific reference ranges for serum testosterone and androstenedione concentrations in women measured by liquid chromatography–tandem mass spectrometry. J. Clin. Endocrinol. Metab. 97, 408–415 (2012).
Wu, F. C. et al. Hypothalamic–pituitary–testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European male aging study. J. Clin. Endocrinol. Metab. 93, 2737–2745 (2008).
Handelsman, D. J. et al. Age-specific population centiles for androgen status in men. Eur. J. Endocrinol. 173, 809–817 (2015).
Nanba, A. T. et al. 11-Oxygenated C19 steroids do not decline with age in women. J. Clin. Endocrinol. Metab. 104, 2615–2622 (2019).
Parker, C. R. Jr. Dehydroepiandrosterone and dehydroepiandrosterone sulfate production in the human adrenal during development and aging. Steroids 64, 640–647 (1999).
Parker, C. R. Jr. et al. Effects of aging on adrenal function in the human: responsiveness and sensitivity of adrenal androgens and cortisol to adrenocorticotropin in premenopausal and postmenopausal women. J. Clin. Endocrinol. Metab. 85, 48–54 (2000).
Xing, Y. et al. The effects of ACTH on steroid metabolomic profiles in human adrenal cells. J. Endocrinol. 209, 327–335 (2011).
Kindler, P. M., Philipp, D. P., Gross, M. R. & Bahr, J. M. Serum 11-ketotestosterone and testosterone concentrations associated with reproduction in male bluegill (Lepomis macrochirus: centrarchidae). Gen. Comp. Endocrinol. 75, 446–453 (1989).
Feist, G., Schreck, C. B., Fitzpatrick, M. S. & Redding, J. M. Sex steroid profiles of coho salmon (Oncorhynchus kisutch) during early development and sexual differentiation. Gen. Comp. Endocrinol. 80, 299–313 (1990).
Kobayashi, M. & Nakanishi, T. 11-Ketotestosterone induces male-type sexual behavior and gonadotropin secretion in gynogenetic crucian carp, Carassius auratus langsdorfii. Gen. Comp. Endocrinol. 115, 178–187 (1999).
Nagahama, Y., Miura, T. & Kobayashi, T. The onset of spermatogenesis in fish. Ciba Found. Symp. 182, 255–267 (1994).
Miura, T., Yamauchi, K., Takahashi, H. & Nagahama, Y. The role of hormones in the acquisition of sperm motility in salmonid fish. J. Exp. Zool. 261, 359–363 (1992).
Rege, J. et al. Circulating 11-oxygenated androgens across species. J. Steroid Biochem. Mol. Biol. 190, 242–249 (2019).
Polson, D. W., Reed, M. J., Franks, S., Scanlon, M. J. & James, V. H. Serum 11β-hydroxyandrostenedione as an indicator of the source of excess androgen production in women with polycystic ovaries. J. Clin. Endocrinol. Metab. 66, 946–950 (1988).
Ibrahim, F. et al. Plasma 11β-hydroxy-4-androstene-3,17-dione: comparison of a time-resolved fluoroimmunoassay using a biotinylated tracer with a radioimmunoassay using a tritiated tracer. J. Steroid Biochem. Mol. Biol. 84, 563–568 (2003).
Therrell, B. L. Newborn screening for congenital adrenal hyperplasia. Endocrinol. Metab. Clin. North. Am. 30, 15–30 (2001).
Speiser, P. W. et al. High frequency of nonclassical steroid 21-hydroxylase deficiency. Am. J. Hum. Genet. 37, 650–667 (1985).
Turcu, A. F. & Auchus, R. J. Adrenal steroidogenesis and congenital adrenal hyperplasia. Endocrinol. Metab. Clin. North. Am. 44, 275–296 (2015).
Fluck, C. E., Miller, W. L. & Auchus, R. J. The 17,20-lyase activity of cytochrome p450c17 from human fetal testis favors the Δ5 steroidogenic pathway. J. Clin. Endocrinol. Metab. 88, 3762–3766 (2003).
Speiser, P. W. et al. Disease expression and molecular genotype in congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J. Clin. Invest. 90, 584–595 (1992).
Krone, N., Braun, A., Roscher, A. A., Knorr, D. & Schwarz, H. P. Predicting phenotype in steroid 21-hydroxylase deficiency? Comprehensive genotyping in 155 unrelated, well defined patients from southern Germany. J. Clin. Endocrinol. Metab. 85, 1059–1065 (2000).
Charmandari, E., Matthews, D. R., Johnston, A., Brook, C. G. & Hindmarsh, P. C. Serum cortisol and 17-hydroxyprogesterone interrelation in classic 21-hydroxylase deficiency: is current replacement therapy satisfactory? J. Clin. Endocrinol. Metab. 86, 4679–4685 (2001).
Rezvani, I., Garibaldi, L. R., Digeorge, A. M. & Artman, H. G. Disproportionate suppression of dehydroepiandrosterone sulfate (DHEAS) in treated patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Pediatr. Res. 17, 131–134 (1983).
Carmina, E., Stanczyk, F. Z., Chang, L., Miles, R. A. & Lobo, R. A. The ratio of androstenedione:11β-hydroxyandrostenedione is an important marker of adrenal androgen excess in women. Fertil. Steril. 58, 148–152 (1992).
Huerta, R. et al. 11β-Hydroxyandrostenedione and Δ5-androstenediol as markers of adrenal androgen production in patients with 21-hydroxylase-deficient nonclassic adrenal hyperplasia. Fertil. Steril. 72, 996–1000 (1999).
Kamrath, C., Wettstaedt, L., Boettcher, C., Hartmann, M. F. & Wudy, S. A. Androgen excess is due to elevated 11-oxygenated androgens in treated children with congenital adrenal hyperplasia. J. Steroid Biochem. Mol. Biol. 178, 221–228 (2018).
Turcu, A. F. et al. 11-Oxygenated androgens are biomarkers of adrenal volume and testicular adrenal rest tumors in 21-hydroxylase deficiency. J. Clin. Endocrinol. Metab. 102, 2701–2710 (2017).
Claahsen-van der Grinten, H. L., Sweep, F. C., Blickman, J. G., Hermus, A. R. & Otten, B. J. Prevalence of testicular adrenal rest tumours in male children with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Eur. J. Endocrinol. 157, 339–344 (2007).
Albright, F., Smith, P. H. & Fraser, R. A syndrome characterized by primary ovarian insufficiency and decreased stature: report of 11 cases with a digression on hormonal control of axillary and pubic hair. Am. J. Med. Sci. 2014, 625–648 (1942).
Ibanez, L. et al. Postpubertal outcome in girls diagnosed of premature pubarche during childhood: increased frequency of functional ovarian hyperandrogenism. J. Clin. Endocrinol. Metab. 76, 1599–1603 (1993).
Idkowiak, J. et al. Premature adrenarche: novel lessons from early onset androgen excess. Eur. J. Endocrinol. 165, 189–207 (2011).
Talbot, N. B., Butler, A. M., Berman, R. A., Rodriguez, P. M. & Maclachlan, E. A. Excretion of 17-keto steroids by normal and abnormal children. Am. J. Dis. Child. 65, 364–375 (1943).
Voutilainen, R. & Jaaskelainen, J. Premature adrenarche: etiology, clinical findings, and consequences. J. Steroid Biochem. Mol. Biol. 145, 226–236 (2015).
Herman-Giddens, M. E. et al. Secondary sexual characteristics and menses in young girls seen in office practice: a study from the pediatric research in office settings network. Pediatrics 99, 505–512 (1997).
Voutilainen, R., Perheentupa, J. & Apter, D. Benign premature adrenarche: clinical features and serum steroid levels. Acta Paediatr. Scand. 72, 707–711 (1983).
Sopher, A. B. et al. Bone age advancement in prepubertal children with obesity and premature adrenarche: possible potentiating factors. Obesity 19, 1259–1264 (2011).
Kaplowitz, P. & Soldin, S. J. Steroid profiles in serum by liquid chromatography–tandem mass spectrometry in infants with genital hair. J. Pediatr. Endocrinol. Metab. 20, 597–605 (2007).
Novello, L. & Speiser, P. W. Premature adrenarche. Pediatr. Ann. 47, e7–e11 (2018).
Saenger, P. & Dimartino-Nardi, J. Premature adrenarche. J. Endocrinol. Invest. 24, 724–733 (2001).
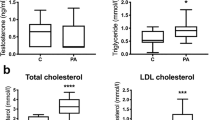
Celik, N. et al. The association between premature adrenarche and cardiovascular risk may be greater than expected. Horm. Res. Paediatr. 87, 7–14 (2017).
Ibanez, L. et al. Hyperinsulinemia and decreased insulin-like growth factor-binding protein-1 are common features in prepubertal and pubertal girls with a history of premature pubarche. J. Clin. Endocrinol. Metab. 82, 2283–2288 (1997).
Ibanez, L., Potau, N., Chacon, P., Pascual, C. & Carrascosa, A. Hyperinsulinaemia, dyslipaemia and cardiovascular risk in girls with a history of premature pubarche. Diabetologia 41, 1057–1063 (1998).
Mathew, R. P. et al. Evidence of metabolic syndrome in lean children with premature pubarche at diagnosis. Metabolism 57, 733–740 (2008).
Kaya, G., Yavas Abali, Z., Bas, F., Poyrazoglu, S. & Darendeliler, F. Body mass index at the presentation of premature adrenarche is associated with components of metabolic syndrome at puberty. Eur. J. Pediatr. 177, 1593–1601 (2018).
Ibanez, L., Potau, N. & Carrascosa, A. Insulin resistance, premature adrenarche, and a risk of the polycystic ovary syndrome (PCOS). Trends Endocrinol. Metab. 9, 72–77 (1998).
Kousta, E. Premature adrenarche leads to polycystic ovary syndrome? Long-term consequences. Ann. N. Y. Acad. Sci. 1092, 148–157 (2006).
Legro, R. S. Detection of insulin resistance and its treatment in adolescents with polycystic ovary syndrome. J. Pediatr. Endocrinol. Metab. 15, 1367–1378 (2002).
Rosenfield, R. L. Clinical review: Identifying children at risk for polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 92, 787–796 (2007).
Siklar, Z., Ocal, G., Adiyaman, P., Ergur, A. & Berberoglu, M. Functional ovarian hyperandrogenism and polycystic ovary syndrome in prepubertal girls with obesity and/or premature pubarche. J. Pediatr. Endocrinol. Metab. 20, 475–481 (2007).
Ibanez, L. et al. Hyperinsulinemia in postpubertal girls with a history of premature pubarche and functional ovarian hyperandrogenism. J. Clin. Endocrinol. Metab. 81, 1237–1243 (1996).
Ollila, M. M. et al. Weight gain and dyslipidemia in early adulthood associate with polycystic ovary syndrome: prospective cohort study. J. Clin. Endocrinol. Metab. 101, 739–747 (2016).
West, S. et al. Irregular menstruation and hyperandrogenaemia in adolescence are associated with polycystic ovary syndrome and infertility in later life: Northern Finland Birth Cohort 1986 study. Hum. Reprod. 29, 2339–2351 (2014).
Banerjee, S. et al. Hormonal findings in African-American and Caribbean Hispanic girls with premature adrenarche: implications for polycystic ovarian syndrome. Pediatrics 102, E36 (1998).
Toscano, V. et al. Changes in steroid pattern following acute and chronic adrenocorticotropin administration in premature adrenarche. J. Steroid Biochem. 32, 321–326 (1989).
Kim, S. H., Moon, J. Y., Sasano, H., Choi, M. H. & Park, M. J. Body fat mass is associated with ratio of steroid metabolites reflecting 17,20-lyase activity in prepubertal girls. J. Clin. Endocrinol. Metab. 101, 4653–4660 (2016).
Vuguin, P., Linder, B., Rosenfeld, R. G., Saenger, P. & DiMartino-Nardi, J. The roles of insulin sensitivity, insulin-like growth factor I (IGF-I), and IGF-binding protein-1 and -3 in the hyperandrogenism of African-American and Caribbean Hispanic girls with premature adrenarche. J. Clin. Endocrinol. Metab. 84, 2037–2042 (1999).
Paterson, W. F. et al. Exaggerated adrenarche in a cohort of Scottish children: clinical features and biochemistry. Clin. Endocrinol. 72, 496–501 (2010).
Jamieson, A. et al. Apparent cortisone reductase deficiency: a functional defect in 11β-hydroxysteroid dehydrogenase type 1. J. Clin. Endocrinol. Metab. 84, 3570–3574 (1999).
Malunowicz, E. M., Romer, T. E., Urban, M. & Bossowski, A. 11β-Hydroxysteroid dehydrogenase type 1 deficiency (‘apparent cortisone reductase deficiency’) in a 6-year-old boy. Horm. Res. 59, 205–210 (2003).
Charmandari, E., Kino, T. & Chrousos, G. P. Primary generalized familial and sporadic glucocorticoid resistance (Chrousos syndrome) and hypersensitivity. Endocr. Dev. 24, 67–85 (2013).
Lappalainen, S., Utriainen, P., Kuulasmaa, T., Voutilainen, R. & Jaaskelainen, J. Androgen receptor gene CAG repeat polymorphism and X-chromosome inactivation in children with premature adrenarche. J. Clin. Endocrinol. Metab. 93, 1304–1309 (2008).
Likitmaskul, S. et al. ‘Exaggerated adrenarche’ in children presenting with premature adrenarche. Clin. Endocrinol. 42, 265–272 (1995).
Utriainen, P., Laakso, S., Liimatta, J., Jaaskelainen, J. & Voutilainen, R. Premature adrenarche — a common condition with variable presentation. Horm. Res. Paediatr. 83, 221–231 (2015).
Kaufman, F. R. et al. Dehydroepiandrosterone and dehydroepiandrosterone sulfate metabolism in human genital skin. Fertil. Steril. 54, 251–254 (1990).
Pelletier, G. Expression of steroidogenic enzymes and sex-steroid receptors in human prostate. Best. Pract. Res. Clin. Endocrinol. Metab. 22, 223–228 (2008).
Rosenfield, R. L. Hirsutism and the variable response of the pilosebaceous unit to androgen. J. Investig. Dermatol. Symp. Proc. 10, 205–208 (2005).
Liimatta, J. et al. Serum androgen bioactivity is low in children with premature adrenarche. Pediatr. Res. 75, 645–650 (2014).
Azziz, R. et al. The prevalence and features of the polycystic ovary syndrome in an unselected population. J. Clin. Endocrinol. Metab. 89, 2745–2749 (2004).
Fauser, B. C. et al. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-sponsored 3rd PCOS Consensus Workshop Group. Fertil. Steril. 97, 28–38 (2012).
Lauritsen, M. P. et al. The prevalence of polycystic ovary syndrome in a normal population according to the Rotterdam criteria versus revised criteria including anti-Mullerian hormone. Hum. Reprod. 29, 791–801 (2014).
Goodman, N. F. et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome — part 1. Endocr. Pract. 21, 1291–1300 (2015).
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil. Steril. 81, 19–25 (2004).
Azziz, R. et al. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil. Steril. 91, 456–488 (2009).
Randeva, H. S. et al. Cardiometabolic aspects of the polycystic ovary syndrome. Endocr. Rev. 33, 812–841 (2012).
Legro, R. S. Polycystic ovary syndrome and cardiovascular disease: a premature association? Endocr. Rev. 24, 302–312 (2003).
Wild, R. A. Long-term health consequences of PCOS. Hum. Reprod. Update 8, 231–241 (2002).
Han, T. S., Walker, B. R., Arlt, W. & Ross, R. J. Treatment and health outcomes in adults with congenital adrenal hyperplasia. Nat. Rev. Endocrinol. 10, 115–124 (2014).
Stahl, N. L., Teeslink, C. R., Beauchamps, G. & Greenblatt, R. B. Serum testosterone levels in hirsute women: a comparison of adrenal, ovarian and peripheral vein values. Obstet. Gynecol. 41, 650–654 (1973).
Stahl, N. L., Teeslink, C. R. & Greenblatt, R. B. Ovarian, adrenal, and peripheral testosterone levels in the polycystic ovary syndrome. Am. J. Obstet. Gynecol. 117, 194–200 (1973).
Barnes, R. B., Rosenfield, R. L., Burstein, S. & Ehrmann, D. A. Pituitary–ovarian responses to nafarelin testing in the polycystic ovary syndrome. N. Engl. J. Med. 320, 559–565 (1989).
Ehrmann, D. A., Rosenfield, R. L., Barnes, R. B., Brigell, D. F. & Sheikh, Z. Detection of functional ovarian hyperandrogenism in women with androgen excess. N. Engl. J. Med. 327, 157–162 (1992).
Lachelin, G. C. et al. Long term effects of nightly dexamethasone administration in patients with polycystic ovarian disease. J. Clin. Endocrinol. Metab. 55, 768–773 (1982).
O’Reilly, M. W. et al. Hyperandrogenemia predicts metabolic phenotype in polycystic ovary syndrome: the utility of serum androstenedione. J. Clin. Endocrinol. Metab. 99, 1027–1036 (2014).
Conway, G. et al. The polycystic ovary syndrome: a position statement from the European Society of Endocrinology. Eur. J. Endocrinol. 171, 1–29 (2014).
Pasquali, R. et al. Defining hyperandrogenism in women with polycystic ovary syndrome: a challenging perspective. J. Clin. Endocrinol. Metab. 101, 2013–2022 (2016).
Hoffman, D. I., Klove, K. & Lobo, R. A. The prevalence and significance of elevated dehydroepiandrosterone sulfate levels in anovulatory women. Fertil. Steril. 42, 76–81 (1984).
Lucky, A. W., Rosenfield, R. L., McGuire, J., Rudy, S. & Helke, J. Adrenal androgen hyperresponsiveness to adrenocorticotropin in women with acne and/or hirsutism: adrenal enzyme defects and exaggerated adrenarche. J. Clin. Endocrinol. Metab. 62, 840–848 (1986).
Azziz, R., Boots, L. R., Parker, C. R. Jr., Bradley, E. Jr. & Zacur, H. A. 11β-Hydroxylase deficiency in hyperandrogenism. Fertil. Steril. 55, 733–741 (1991).
Stanczyk, F. Z., Chang, L., Carmina, E., Putz, Z. & Lobo, R. A. Is 11β-hydroxyandrostenedione a better marker of adrenal androgen excess than dehydroepiandrosterone sulfate? Am. J. Obstet. Gynecol. 165, 1837–1842 (1991).
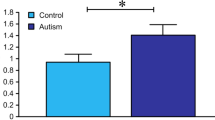
O’Reilly, M. W. et al. 11-Oxygenated C19 steroids are the predominant androgens in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 102, 840–848 (2017).
Heidenreich, A. et al. EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur. Urol. 65, 467–479 (2014).
Montgomery, R. B. et al. Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res. 68, 4447–4454 (2008).
Titus, M. A., Schell, M. J., Lih, F. B., Tomer, K. B. & Mohler, J. L. Testosterone and dihydrotestosterone tissue levels in recurrent prostate cancer. Clin. Cancer Res. 11, 4653–4657 (2005).
de Bono, J. S. et al. Abiraterone and increased survival in metastatic prostate cancer. N. Engl. J. Med. 364, 1995–2005 (2011).
Ryan, C. J. et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N. Engl. J. Med. 368, 138–148 (2013).
Scher, H. I. et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N. Engl. J. Med. 367, 1187–1197 (2012).
Pfeiffer, M. J., Smit, F. P., Sedelaar, J. P. & Schalken, J. A. Steroidogenic enzymes and stem cell markers are upregulated during androgen deprivation in prostate cancer. Mol. Med. 17, 657–664 (2011).
Hamid, A. R. et al. Aldo-keto reductase family 1 member C3 (AKR1C3) is a biomarker and therapeutic target for castration-resistant prostate cancer. Mol. Med. 18, 1449–1455 (2013).
Chang, K. H. et al. A gain-of-function mutation in DHT synthesis in castration-resistant prostate cancer. Cell 154, 1074–1084 (2013).
Mitsiades, N. et al. Distinct patterns of dysregulated expression of enzymes involved in androgen synthesis and metabolism in metastatic prostate cancer tumors. Cancer Res. 72, 6142–6152 (2012).
Titus, M. A. et al. Steroid 5α-reductase isozymes I and II in recurrent prostate cancer. Clin. Cancer Res. 11, 4365–4371 (2005).
Chang, K. H. et al. Dihydrotestosterone synthesis bypasses testosterone to drive castration-resistant prostate cancer. Proc. Natl Acad. Sci. USA 108, 13728–13733 (2011).
Gent, R., du Toit, T., Bloem, L. M. & Swart, A. C. The 11β-hydroxysteroid dehydrogenase isoforms: pivotal catalytic activities yield potent C11-oxy C19 steroids with 11βHSD2 favouring 11-ketotestosterone, 11-ketoandrostenedione and 11-ketoprogesterone biosynthesis. J. Steroid Biochem. Mol. Biol. 189, 116–126 (2019).
Dovio, A. et al. Differential expression of determinants of glucocorticoid sensitivity in androgen-dependent and androgen-independent human prostate cancer cell lines. J. Steroid Biochem. Mol. Biol. 116, 29–36 (2009).
Page, N., Warriar, N. & Govindan, M. V. 11β-Hydroxysteroid dehydrogenase and tissue specificity of androgen action in human prostate cancer cell LNCaP. J. Steroid Biochem. Mol. Biol. 49, 173–181 (1994).
Gao, X. et al. Functional silencing of HSD17B2 in prostate cancer promotes disease progression. Clin. Cancer Res. 25, 1291–1301 (2019).
du Toit, T. et al. Profiling adrenal 11β-hydroxyandrostenedione metabolites in prostate cancer cells, tissue and plasma: UPC2-MS/MS quantification of 11β-hydroxytestosterone, 11keto-testosterone and 11keto-dihydrotestosterone. J. Steroid Biochem. Mol. Biol. 166, 54–67 (2017).
du Toit, T. & Swart, A. C. Inefficient UGT-conjugation of adrenal 11β-hydroxyandrostenedione metabolites highlights C11-oxy C19 steroids as the predominant androgens in prostate cancer. Mol. Cell. Endocrinol. 461, 265–276 (2018).
Acknowledgements
The authors acknowledge the support of grants from the NIH (1K08DK109116 to A.F.T., R01DK069950 and R01DK43140 to W.E.R., R01GM086596 to R.J.A.) and the University of Michigan (MCubed U064177 to A.F.T. and W.E.R.).
Author information
Authors and Affiliations
Contributions
A.F.T. researched data for the article, contributed to discussion of the content, wrote the article and reviewed and/or edited the manuscript before submission. J.R. contributed to discussion of the content, wrote the article and reviewed and/or edited the manuscript before submission. R.J.A. and W.E.R. contributed to discussion of the content and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Endocrinology thanks V. Papadopoulos, S. Wudy and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Adrenarche
-
An early stage in sexual maturation specific to humans and other primates that is caused by androgen synthesis from the adrenal glands and is associated with the development of pubic hair, body odour, skin oiliness and acne.
- Steroidogenesis
-
The process of steroid synthesis.
- Tropic
-
Related to hormones that stimulate the growth and activity of target glands.
- Second messengers
-
Small intracellular molecules that mediate the effects of first messengers, that is, neurotransmitters and hormones.
- Pubarche
-
The first appearance of pubic hair at puberty.
- Sulfonation
-
The transfer of a sulfonate group (SO3−1) from the universal sulfonate donor 3′-phosphoadenosine 5′-phosphosulfate (PAPS) to an appropriate acceptor molecule.
- Glucuronidation
-
A process of steroid metabolism that consists of transfer of the glucuronic acid component of uridine diphosphate glucuronic acid to a substrate by any of several types of UDP-glucuronosyltransferase.
Rights and permissions
About this article
Cite this article
Turcu, A.F., Rege, J., Auchus, R.J. et al. 11-Oxygenated androgens in health and disease. Nat Rev Endocrinol 16, 284–296 (2020). https://doi.org/10.1038/s41574-020-0336-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-020-0336-x
This article is cited by
-
Impact of dehydroepiandrosterone sulfate and free androgen index on pregnancy and neonatal outcomes in PCOS patients
Reproductive Biology and Endocrinology (2024)
-
In situ fabrication of covalent organic frameworks on solid-phase microextraction probes coupled with electrospray ionization mass spectrometry for enrichment and determination of androgens in biosamples
Microchimica Acta (2024)
-
Longitudinal assessment of classic and 11-oxygenated androgen concentrations and their association with type 2 diabetes mellitus development: the Tromsø study
Acta Diabetologica (2024)
-
Targeting sex steroid biosynthesis for breast and prostate cancer therapy
Nature Reviews Cancer (2023)
-
Management challenges and therapeutic advances in congenital adrenal hyperplasia
Nature Reviews Endocrinology (2022)