Abstract
This contemporary, international, evidence-informed guidance aims to achieve the greatest good for the greatest number of people with familial hypercholesterolaemia (FH) across different countries. FH, a family of monogenic defects in the hepatic LDL clearance pathway, is a preventable cause of premature coronary artery disease and death. Worldwide, 35 million people have FH, but most remain undiagnosed or undertreated. Current FH care is guided by a useful and diverse group of evidence-based guidelines, with some primarily directed at cholesterol management and some that are country-specific. However, none of these guidelines provides a comprehensive overview of FH care that includes both the lifelong components of clinical practice and strategies for implementation. Therefore, a group of international experts systematically developed this guidance to compile clinical strategies from existing evidence-based guidelines for the detection (screening, diagnosis, genetic testing and counselling) and management (risk stratification, treatment of adults or children with heterozygous or homozygous FH, therapy during pregnancy and use of apheresis) of patients with FH, update evidence-informed clinical recommendations, and develop and integrate consensus-based implementation strategies at the patient, provider and health-care system levels, with the aim of maximizing the potential benefit for at-risk patients and their families worldwide.
Similar content being viewed by others
Introduction
Familial hypercholesterolaemia (FH) is a co-dominant and highly penetrant monogenic disorder that markedly elevates LDL-cholesterol concentration from birth and, if untreated, leads to premature atherosclerotic cardiovascular disease (ASCVD)1,2,3. FH is a tier 1 genomic condition, meaning that it is a preventable cause of premature disease and death owing to ischaemic heart disease3,4,5,6, with substantial effects on public health7.
The public health importance of FH is also highlighted by an overall phenotypic frequency in the population of 1 in 311 (refs. 4,8). FH may affect up to 35 million people worldwide, but only 10% are currently diagnosed, and >80% of those treated do not achieve recommended LDL-cholesterol goals2,9. The persistent unmet needs in the care of patients with FH have prompted several clinical practice guidelines10,11,12,13,14,15,16,17,18, international collaborations19,20,21,22 and global calls to action9,23,24,25. Although new evidence should inform better standards of care2,26, implementation of guideline recommendations is generally overlooked27,28,29.
Implementation science offers the best approach for translating clinical recommendations into routine practice by overcoming barriers to and leveraging enablers of improved care, thereby striving to achieve maximal benefit for the population at risk29,30. This approach is highly relevant to the practice of genomics and precision medicine31. Therefore, we have promoted this methodology to develop implementation strategies to increase the impact of clinical recommendations on the care of patients with FH32.
This evidence-informed guidance article provides a systematic compendium of clinical recommendations, informed by best contemporary evidence, for the detection and management of patients with FH. These recommendations are supplemented with general and specific implementation strategies to optimize the deployment in models of care.
Methodology
The full protocol is provided in Supplementary Material 1. Briefly, development of the guidance was led by the International Expert Working Group (IEWG), selected by the board of the International Atherosclerosis Society (IAS) for having diverse expertise in FH (Supplementary Material 1 Appendices 1 and 2). The IEWG defined the scope and focus of the task, developed the evidence evaluation process, appointed a writing committee and sought stakeholder involvement. The development of the clinical guidance was based on previous guidelines that had used evidence-informed recommendations and scored highly on an AGREE-II assessment33,34 (Supplementary Material 1 Appendix 3).
Design of the guidance
The guidance was generically divided into aspects of detection, management and implementation. Detection covered screening, diagnosis, genetic testing and counselling. Management covered risk stratification, treatment of adults and children with heterozygous FH (HeFH) or homozygous FH (HoFH), management of FH during pregnancy, and use of lipoprotein apheresis. The detection and management sections included preambles, clinical recommendations and implementation recommendations. Clinical recommendations were given classes of recommendation (1 = strong, 2 = moderate and 3 = weak) and corresponding levels of evidence (A = high, B = moderate and C = low)35,36 (Supplementary Material 1 Appendix 4). Implementation recommendations were developed by consensus, based on relevant published works, and were guided by a framework provided by the Expert Recommendations for Implementing Change (ERIC)37 (Supplementary Material 1 Appendix 5).
Detection
Screening
FH meets all the criteria for screening for a health-related condition38,39. The value of early detection derives from the premise that the burden of ASCVD owing to genetically elevated plasma LDL-cholesterol concentrations in FH begins at birth and accumulates over time13,40 and that initiation of treatment in childhood can cost-effectively prevent coronary events, improve quality of life and reduce mortality2,13,40,41.
Early detection of FH is fundamental to all models of care for FH2,17,23,42. Detection strategies include opportunistic, selective, systematic and universal screening, using phenotypic and genetic testing, with many of these approaches confirmed as being cost-effective2,17,42. However, the best approach to detecting FH in primary care remains uncertain43,44,45. Newer methods have been proposed and evaluated, such as universal screening of children and subsequent child–parent testing46,47,48,49. Universal screening in the paediatric population has the specific advantage of early detection of HoFH, the most severe type of FH18. Population modelling and implementation studies show that, to identify >90% of the population with FH, combining cascade testing of family members of affected individuals with some form of universal screening at younger ages may have the highest potential42,50,51. Genomic-based population screening has also been proposed52, but experience is limited53,54,55. Genomic newborn screening is another option, but remains under investigation56,57; enhanced identification of HoFH in populations with a gene founder effect will lead to optimal treatment1,2,18.
Several barriers to effective screening for FH persist, with implementation practice remaining a major challenge2,16,24,58,59,60. All screening strategies must confer a net benefit for individuals and populations, be socially and culturally acceptable, and be undertaken in accordance with the requirements of the relevant jurisdiction2,61. Criteria for effective implementation include feasibility, fidelity, adoption, access and reach, cost–effectiveness and sustainability62. Implementation of screening strategies should be underpinned by wide public awareness, comprehensive education and training of health-care professionals, integrated programme management and effective risk-reduction models of care37. Population and community support, effective government health policy and public financing are essential, particularly for genomic-based screening programmes39,52.
The recommendations on screening for FH (Table 1) refer to clinical and public health approaches, supplemented by implementation strategies37,58,59. These should be integrated with the recommendations on the diagnosis of FH2,16,17.
Implementation recommendations on screening for FH
General screening
-
1.
Detection and diagnosis of index cases in the community should ideally use an integrated, patient-centred approach, underpinned by a multidisciplinary strategy involving community and paediatric physicians, obstetric physicians and gynaecologists, nurses and counsellors.
-
2.
Screening and detection strategies should ideally be centrally coordinated, enabling testing by all designated requestors, such as specialist practitioners and genetic counsellors, and linked to a clinical quality registry, particularly when undertaking cascade testing of family members.
-
3.
In countries or regions with limited resources, a skilled health-care professional may lead and coordinate screening and diagnostic strategies, preferably in consultation with a specialist centre and with appropriate training in the care of FH.
-
4.
Digital technologies should be used to search electronic health records to enable systematic detection of index cases, particularly in the community care setting.
-
5.
All health-care professionals involved in screening and documentation of the outcome of testing for FH should be adequately trained and fully aware of the local guidance on data protection; this training is particularly important in cascade testing of family members.
Opportunistic screening
-
6.
Opportunistic detection of FH with LDL-cholesterol testing should be performed by dermatologists (for example, on a lipid profile before commencing isotretinoin), rheumatologists and orthopaedic surgeons (for example, for patients having Achilles xanthomas and tenosynovitis), ophthalmologists and optometrists (for example, for patients having premature arcus cornealis, xanthelasma palpebrarum or planar xanthomas), occupational physicians (for example, workplace wellness programmes) and pharmacists (for example, point-of-care testing with a history that is suggestive of FH).
-
7.
Alerts and interpretive comments on laboratory reports of standard lipid profiles should be used to enable case detection, emphasizing the need to make a formal diagnosis and referral for further assessment of FH.
Universal screening
-
8.
Universal screening for FH should be integrated into routine population health surveillance strategies (for example, health checks in adults and community health screening programmes) and prevention procedures (for example, immunization in children).
-
9.
Genetic testing may be considered, if feasible and potentially implementable, for population screening for FH, provided that testing also includes other actionable Centers for Disease Control Tier 1 genetic conditions; the programme should also be equitable, cost-effective and integrated into a well-structured, risk-reduction model of care for FH.
-
10.
Patient support and professional organizations should strongly advocate for health policy to implement universal screening of FH in paediatric populations; this screening is particularly relevant to the early detection of HoFH.
See Box 1 for core implementation strategies.
Diagnosis
The most accurate way to diagnose FH is by genetic testing, which identifies the presence of pathogenic variants that impair LDL receptor function and cause hypercholesterolaemia2,63,64. However, genetic testing is currently expensive, not universally available and may not capture all pathogenic variants2,65,66,67. Accordingly, the diagnosis of FH often relies on phenotypic criteria alone2,65. A phenotypic diagnosis of FH may be used to ration genetic analyses by selectively offering testing to potential index cases who are most likely to have a variant; genetic testing may also be offered to patients for whom the presence of a variant could influence treatment recommendations (for example, those with moderately high LDL-cholesterol levels without clinical indicators of FH). Genetic and phenotypic testing are important for both assessing and managing patients with FH2,13,14,16,17.
Standardizing the phenotypic diagnosis of FH is complicated by the overlap of LDL-cholesterol concentrations between those with HoFH and those with HeFH and between those with HeFH and those with polygenic hypercholesterolaemia1,2,63. Diagnostic accuracy also depends on variations in genes unrelated to FH that influence LDL-cholesterol and lipoprotein(a) (Lp(a)) concentrations, as well as on changes in LDL-cholesterol concentrations owing to age, ancestry, menopause, coexisting acute and chronic medical conditions and the environment2,63. Adjustment for concurrent treatments that lower LDL-cholesterol concentrations is also required to make an accurate phenotypic diagnosis17,68.
In adults, the most widely used clinical diagnostic methods are the Dutch Lipid Clinic Network and the Simon Broome criteria2; other internationally used methods are the US (MED-PED or AHA), the Japanese and the Canadian criteria16,69,70 (Supplementary Material 2). However, with statin therapy, the use of clinical criteria alone is more difficult, because those treated from an early age tend not to have physical stigmata, such as tendon xanthomas, and fewer patients will have a positive family history of premature coronary artery disease2. Machine learning modelling applied to the diagnosis of FH shows promise71,72,73, but requires further evaluation in clinical practice.
In children, clinical diagnosis relies on elevated LDL-cholesterol concentrations and a positive family history of premature coronary artery disease and/or high LDL-cholesterol concentration in at least one parent13,16,17,74. In the absence of genetic testing, the diagnosis of FH during cascade testing of adults and children relies on measuring LDL-cholesterol concentrations17,75.
The clinical diagnosis of HoFH is not as problematic as that of HeFH, because HoFH presents earlier and has a more pronounced clinical phenotype18,76,77. However, LDL-cholesterol concentrations can vary in patients with HoFH according to the type of genetic defect and cannot alone establish the diagnosis18,22,78,79. Genetically confirmed HoFH can occur in patients with an LDL-cholesterol concentration <13 mmol/l (<500 mg/dl), suggesting that a lower diagnostic threshold of <10 mmol/l (<400 mg/dl) should be used clinically22,78,79. Making a phenotypic diagnosis of ‘severe FH’, on the basis of markedly elevated LDL-cholesterol concentrations and the presence of other major risk factors for ASCVD or a history of ASCVD, may have prognostic value in adults in the absence of a genetic diagnosis80,81. The term ‘phenotypic’ HoFH has also been proposed as an operational diagnosis for patients with the classic phenotype in the absence of detectable biallelic pathogenic, or likely pathogenic, gene variants18.
When making a clinical diagnosis of FH, the same recommendations as when screening for FH apply to the measurement of LDL-cholesterol concentrations in relation to elevated triglyceride levels, coexistent acute illness and concurrent use of cholesterol-lowering therapies. High Lp(a)-cholesterol concentration associated with very high Lp(a) concentrations may also affect the phenotypic diagnosis of FH in people with markedly elevated Lp(a) concentrations82,83,84. In patients with both phenotypic FH and high Lp(a) concentrations, correcting LDL-cholesterol for Lp(a)-cholesterol may refine the clinical diagnosis and avoid unnecessary genetic testing for FH82,83,85. However, how best to accurately adjust LDL-cholesterol for Lp(a)-cholesterol remains unresolved86,87.
Recommendations for the diagnosis of FH are provided in Table 2.
Implementation recommendations on the diagnosis of FH
-
1.
Cost-effective pathways for making a diagnosis of FH, including referrals to specialists, should be seamlessly integrated with all screening strategies for FH.
-
2.
The diagnosis of FH in children and adolescents should ideally be made by a paediatrician with training and expertise in lipidology, and with attention to assessing the psychological effect of the diagnosis on the family and need to follow regulations on child protection (safeguarding); in those who have difficulty fasting, a non-fasting blood sample may be considered to make a clinical diagnosis.
-
3.
All patients diagnosed with HoFH should be referred to a specialist centre for further physical and psychological assessment and careful planning of care.
-
4.
Whenever possible, all index patients with a phenotypic diagnosis of FH should be offered genetic testing, especially if cascade testing is planned.
-
5.
All health-care professionals involved in making a diagnosis of FH should be aware of the local guidance on data protection.
Genetic testing and counselling: risk notification and cascade testing
Genetic testing refers to an accredited DNA diagnostic methodology with validated bioinformatic analyses performed in a certified laboratory that issues clear reporting of results88. Genetic testing in FH increases the precision of diagnosis and counselling, accuracy of risk stratification, adherence to treatment, access to special therapies and cost–effectiveness of cascade testing1,2,63,64,89,90. The importance of genetic testing for making a diagnosis of FH is emphasized in two expert statements91,92. However, genetic testing is currently underutilized in clinical practice. This underutilization relates to the costs of genetic tests, inadequate clinical skills in genomic medicine, genetic privacy policies, concerns about restrictions on life insurance, and underavailability of genetic counselling services2,93. These barriers must be addressed for effective implementation2,63,93.
Genetic testing aims to provide precise and personalized information that helps clinicians and patients to make informed decisions about their health care63,88,94. Accordingly, genetic testing requires skilled counselling, a process that includes risk assessment, anticipatory guidance, family-based care and psychological assessment63,88,94. Patient attitudes towards genetic testing for FH are generally positive, given the minimal negative sequelae95. A pathogenic DNA variant is often found when FH is suspected clinically96, but discrepancies include patients with a variant of uncertain significance or a benign variant, patients with no detected pathogenic variant because they have polygenic hypercholesterolaemia or a truly pathogenic variant has not been molecularly identified, and normolipidaemic individuals in whom a pathogenic variant is found97. These individuals can benefit from the expertise of a genetic counsellor1,2,63,88. More comprehensive genetic testing for pathogenic or likely pathogenic variants will evidently increase the likelihood of making an accurate diagnosis of FH66,98. Genetic testing procedures should be standardized, including informed consent, pre-test and post-test genetic counselling, classification of variants, reporting and return of results, follow-up of family members for cascade testing, and shared decision-making63,94. A shared decision-making framework uniquely combines the clinical expertise of the health-care provider with the preferences of the patient, personal circumstances, goals, values and beliefs63,88,94.
Cascade testing is the stepwise, systematic testing of at-risk biological relatives in families with a genetic condition and is strongly recommended for detecting FH1,2,17,42,63,99. Cascade testing is highly efficient for identifying additional individuals with FH, particularly younger than the age at diagnosis of the proband63. A proactive approach, based on fundamental ethical and legal principles, is most cost-effective2,17,63. Cascade testing can be performed genotypically and phenotypically2,17, but identification of a pathogenic variant (or variants) in the proband allows targeted testing of at-risk relatives with very high sensitivity and specificity1,63,64. Cascade genetic testing also identifies relatives who did not inherit the familial variant (variants) and are, therefore, highly unlikely to have FH, an outcome with high personal and clinical utility63,94. If index cases with FH are also known to have a high Lp(a) concentration, cascade testing for elevated Lp(a) concentrations should also be considered in first-degree relatives100. Reverse cascade testing of parents from a child known to have FH is also recommended17,63. Effective and ethical risk notification and cascade testing are underpinned by pre-test and post-test genetic counselling63,94,99, which may be provided by a health-care professional with expertise in FH and genetics17. There are multiple barriers and facilitators that should be addressed to optimize the detection of new cases of FH using cascade testing29,101,102,103.
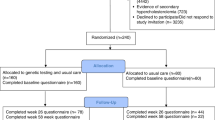
Recommendations for genetic testing and counselling for FH are provided in Table 3 and Fig. 1.
Options include using LDL-cholesterol testing alone or genetic testing together with LDL-cholesterol testing. FH, familial hypercholesterolaemia. Adapted with permission from ref. 17, Elsevier.
Implementation recommendations on genetic testing and counselling for FH
-
1.
Eligible patients should be referred to a specialized clinic or centre that offers genetic testing and supporting services; direct-to-consumer genetic tests are not recommended or appropriate for clinical use in making a diagnosis of FH.
-
2.
A standardized process for obtaining informed consent for genetic testing should be used, ensuring:
-
a.
Informed consent considers literacy and level of comprehension and sociocultural and psychological background of the patient, includes a lay explanation of risk, addresses the possible impact of either a positive or negative result and allows the patient to withdraw consent.
-
b.
Modifications to the process for paediatric patients, specifying appropriate assent be given by a custodial parent or guardian.
-
3.
Sample collection, testing, analyses and reporting of findings should use a standardized process, as follows:
-
a.
Standardize collection procedures for blood and/or saliva samples.
-
b.
Carry out testing using a centralized service in a fully accredited laboratory.
-
c.
Apply validated bioinformatics to interpret results of genetic testing and establish a process to manage variants of uncertain significance.
-
d.
Use a standardized reporting format, with the option of providing both a hard and an electronic copy of results to the patient.
-
a.
-
4.
Return of genetic test results to patients should follow a standardized process, as follows:
-
a.
First assess overall literacy and understanding and then clarify objectives and expectations before discussing results with the patient.
-
b.
Tailor disclosure of results to the level of comprehension of the patient.
-
c.
Gauge patient attitudes towards benefits and threats, consider sociocultural and psychological factors and recognize their intentions for the future.
-
d.
Communicate in everyday, jargon-free language and provide written and/or pictorial information according to the level of comprehension of the individual.
-
e.
Restrict reporting of variants in general to those with clear pathogenic or likely pathogenic impact; refrain from reporting results based on benign variants or common polymorphisms.
-
f.
Variants of uncertain significance may be reported, conditional on communication of the result and its implications to the patient being undertaken by a genetic counsellor, or a clinician with expertise in genetics.
-
a.
-
5.
Follow-up and re-assessment of genetic test results should involve the following:
-
a.
Establish a process for patient follow-up regarding questions or concerns that may arise at a later time.
-
b.
Assess subsequent changes in attitudes, behaviour and adherence to treatment advice of patients.
-
c.
Carry out regular performance audits to improve the quality of genetic services.
-
d.
Re-interpret genetic findings regularly, as a collaboration between the issuing laboratory and a clinician with expertise in genetics, accounting for new phenotypic findings in the patient and family and for evolving research knowledge.
-
a.
-
6.
Diagnostic genetic testing of index cases with suspected FH should be requested by a specialist clinician skilled in counselling, genomic medicine and the care of patients and families with FH. Where indicated (for example, rural centres and remote regions), diagnostic genetic testing of index cases may be requested by a general practitioner guided closely by a specialist clinician.
-
7.
Referral to a professional genetic counselling service should be considered, whenever feasible, to optimize the counselling process for all patients and families at risk of FH.
-
8.
Genetic test results (positive, negative or indeterminant) should be disclosed by an appropriate health-care provider, such as a skilled and experienced clinician, including a family doctor, or certified genetic counsellor.
-
9.
Simple and pragmatic tools for counselling, consenting and disclosure of genetic information should be developed and tested to support health-care professionals in providing genetic testing.
-
10.
Cascade testing of family members should be based on shared decision-making and a fully informed consenting process; results should be communicated in a timely manner, with appropriate risk communication and counselling offered.
-
11.
Cascade testing should ideally be centrally coordinated by a well-resourced, dedicated centre. Cascade testing may be undertaken by a general practitioner with skills in the care of patients and families with FH, under the guidance of an appropriate specialist. The organization of cascade testing may vary according to differences in health policies across and within countries at national, state and regional levels.
-
12.
Direct notification of at-risk relatives regarding their risk of FH should generally be undertaken (or pursued) only with authorization from the proband or index case.
-
13.
Probands and index cases with FH should be offered tools and resources by their health-care providers to assist them in communication about the risk of FH with their relatives.
-
14.
Digital technologies (such as chatbots and social media) should be used, with due consideration to safety and privacy issues, to increase the reach, adoption and effectiveness of family communication about FH and cascade testing of families.
-
15.
Novel family communication tools and programmes (such as technology including secure web portals, chatbots and direct contact by a clinician) should be tested for acceptability, feasibility and effectiveness before implementation.
-
16.
The process of risk notification of at-risk relatives should comply with local legislation and institutional guidelines; risk notification may be indirect (such as providing a family letter for the notifier to share with relatives) or direct (such as the clinical service directly contacting relatives after receiving consent or authorization from the proband or index case).
-
17.
At-risk relatives should be notified directly without authorization from the proband or index case only if there is specific legislative provision for breach of confidentiality; this legislative provision may vary between countries.
-
18.
Cascade testing should ideally be integrated with all strategies for the detection of index cases and be linked to a national registry and biobanking facility.
See Box 2 for core implementation strategies.
Management
Risk stratification
FH is commonly considered to be a condition associated with a high frequency of ASCVD, but the risk is widely heterogeneous1,2,16. The development of ASCVD in FH is driven predominantly by the cumulative burden of LDL-cholesterol concentrations, starting from birth and increasing with age if untreated1,3,104. The severity of the genetic defect causing FH determines the progression of ASCVD90, which is markedly greater in patients with HoFH than in those with HeFH1,2,18. However, the progression of ASCVD varies among individuals with a given FH-related gene variant, which relates to behavioural, clinical and other genetic factors2,80,81,105,106. Risk stratification can identify patients who require escalation of treatment and guide the best use of health-care resources2,106,107.
Male sex, delayed initiation of cholesterol-lowering therapy, smoking, low HDL-cholesterol concentration, obesity, diabetes mellitus, hypertension, chronic kidney disease and elevated Lp(a) concentration are all independently predictive of the risk of ASCVD in patients with FH80,81,108,109,110,111. The prevalence of hypertension and diabetes in patients with FH varies according to the world region and both increase with age21,112. Two robust risk-prediction equations, based on a wide spectrum of predictor variables, have been tested prospectively and may have clinical value in adults with HeFH105,113. However, further validation of these equations is required in different ancestries and clinical settings2,106,114,115. Elevated Lp(a) and LDL-cholesterol concentrations and the presence of hypertension can also accelerate the development and progression of aortic valve disease in patients with FH116. Elevated Lp(a) concentrations are also predictive of the presence of polyvascular disease in patients with HeFH117. Coexistent illness, such as coronavirus disease 2019 (COVID-19), increases the risk of myocardial infarction in patients with FH118.
Despite the conventional view that men have a higher incidence of ASCVD than women21,110,119, registry data suggest a relatively high standardized mortality ratio for coronary artery disease in women with severe FH120. Use of statins and attainment of LDL-cholesterol goals are less frequent in women than in men with FH121,122 and independently relate to ancestry121. There is a clear need for improved assessment of sex-specific risk factors for ASCVD, such as reproductive history, in women with FH123,124,125. Improved tools for predicting lifetime risk of ASCVD in children and younger patients with HeFH are also required2,13,17,126,127. Polygenic risk scores for hypercholesterolaemia and ASCVD128,129,130,131 may be valuable in predicting the risk of ASCVD in patients with FH132, subject to resolving analytical, interpretive and risk-communication barriers and the influence of ancestry132.
Although infrequently encountered in contemporary practice133, the presence of tendon xanthomas signifies high cumulative exposure to elevated circulating LDL-cholesterol concentrations and may indicate a high risk of ASCVD2,17,134,135,136,137. However, imaging of coronary and carotid arteries provides the most accurate and direct method to assess ASCVD in patients with FH2,17,107. In adults, coronary artery calcification is a good discriminator of the presence of ASCVD138,139 and increases the predictive value of the SAFEHEART risk equation in genetically defined patients with FH140. Use of CT coronary angiography shows promise2,17,141,142,143,144, but more evidence is required to establish its value for the management of asymptomatic patients with HeFH. No data are available to support the use of coronary imaging at any specific age in adults with HeFH, so the decision is primarily driven by clinical context and indications. However, on the basis of community studies of asymptomatic individuals without FH, cardiac imaging (including coronary artery calcium scoring) may be useful in the assessment of adults with HeFH aged <35 years144,145. Carotid ultrasonography, with measurement of intima–media thickness, has been valuable in research studies and is particularly appealing in children13,41,146. However, the methodology is not universally standardized, and accurate measurement of intima–media thickness requires considerable technical expertise107, precluding current routine use in risk assessment. Because of the extremely high risk of ASCVD in patients with HoFH, cardiovascular imaging of coronary arteries, the aortic root and other arterial territories (the aortic arch, descending aorta and carotid, subclavian, renal and ilio-femoral arteries) has a crucial role in risk stratification and management of these patients18,76,77,147,148,149. Limited access to cardiovascular imaging modalities might partly account for the worse cardiovascular prognosis of patients with HoFH from lower-income countries than those from higher-income countries22.
Recommendations are provided for risk stratification in patients with FH (Table 4).
Implementation recommendations on risk stratification of patients with FH
-
1.
Risk assessment and stratification strategies should be used to triage patients for referral to other services involved in the multidisciplinary care of FH (such as apheresis; general practice support; specialty care in paediatrics, cardiology or diabetes and nicotine cessation programmes).
-
2.
Clear and salient information in written, diagrammatic and electronic format that recognizes cultural, psychological, language and health literacy barriers should be designed and used, together with shared decision-making, to communicate the outcome of risk assessment and stratification, with the aim of developing personalized treatment plans; recognition of patient-reported experience measures and provision of psychosocial and social support are particularly important.
-
3.
Digital health technologies and decision support systems should be used to facilitate all risk assessment strategies (such as the use of FH risk equations or ASCVD imaging) and the corresponding capabilities and capacity of the workforce caring for patients; telehealth services with adequate facilities should be used to support the risk assessment of patients in rural and remote regions.
-
4.
All registries should include comprehensive, high-quality data on ASCVD risk, including assessments using validated risk equations and cardiovascular imaging, linked to patient outcomes and used to improve the cost–effectiveness of models of care for FH.
Treatment
Substantial evidence from epidemiological data, natural history studies, clinical trials of cholesterol-lowering treatment in primary prevention and basic science studies mandates that patients with FH receive aggressive cholesterol-lowering therapy and lifestyle management from an early age to maximally reduce the cumulative cholesterol burden3,150,151. Mendelian randomization data also support that earlier treatment leads to a greater reduction in ASCVD events by lowering lifetime exposure to LDL-cholesterol; the estimated number needed to treat for adolescents with FH to prevent one heart attack is, impressively, two3,24.
Given the lack of clinical trials, therapeutic goals for LDL-cholesterol concentrations in adults and children with FH are based on a synthesis of diverse evidence, including expert opinion2,17,74. The established principle of lower LDL-cholesterol goals in those at higher risk of ASCVD applies. Most patients with HeFH cannot attain very low absolute concentrations of LDL-cholesterol21,152,153,154,155, even when receiving maximal doses of potent statins and ezetimibe, necessitating the addition of proprotein convertase subtilisin/kexin type 9 (PCSK9)-targeted therapy as a third-line approach156,157,158,159,160. Treatment inertia also contributes to the inability to achieve LDL-cholesterol goals, emphasizing the need for greater education and support for practitioners9,21,161,162. Bempedoic acid may have a role in the management of FH, given evidence of longer-term safety and efficacy, but is approved for use only in adults163. Potential toxicity of medications needs careful consideration164, given that most adult patients with FH will be receiving two or more drugs and are, therefore, at risk of drug–drug interactions; judicious monitoring of clinical and laboratory safety is required. Statin intolerance should be investigated and managed according to the established guidelines165,166,167,168,169. Adherence to a healthy lifestyle benefits patients with FH170, mandating that guidelines specified for the prevention of ASCVD in the general population be followed10,11,17,40,171. Comorbidities, such as obesity, diabetes, hypertension, psychological conditions and coronary artery disease21 should be managed in patients with FH according to the relevant guidelines10,11,171. In patients with FH and established clinical ASCVD, the use of aspirin, colchicine and eicosapentaenoic acid should be implemented according to evidence-based guidelines for secondary prevention of ASCVD172,173,174,175,176,177,178.
Primary evidence supporting the treatment of HeFH in children derives from clinical trials of statins, ezetimibe, colesevelam and PCSK9 inhibitors, with end points related to reductions in LDL-cholesterol concentration and to safety. Systematic reviews, registry data and cohort studies have confirmed the efficacy, tolerability and safety of statins for lowering LDL-cholesterol levels (32% mean reduction in LDL-cholesterol concentration in children with HeFH receiving statin therapy between baseline and up to 48 weeks of treatment compared with placebo179), with increased efficacy for higher doses of more potent statins179,180,181,182,183,184,185,186. Trials of statins as first-line therapy also show improvements in carotid intima–media thickness146. The efficacy in lowering LDL-cholesterol concentrations has also been reported for colesevelam (12% mean reduction)187, ezetimibe (27% mean reduction)188 and PCSK9 inhibitors (44% mean reduction)189,190,191. A systematic review of unbiased studies showed a small but significant effect of diet in lowering LDL-cholesterol levels192. There are new recommendations on how best to change lifestyle-related behaviour to reduce the risk of ASCVD in children104,193. Poor adherence to treatment194, inertia to initiation of treatment among paediatric specialists195 and other barriers196 need to be addressed. Genetic testing may increase the use of statins in children197. A family history of ASCVD and past personal experiences can influence treatment preferences in adolescents and young adults198.
A landmark study of patients with HeFH and statin therapy beginning in youth, with follow up to age 40 years, showed substantially lower rates of ASCVD and death compared with their affected parents (1% versus 26% for ASCVD; 0% versus 7% for mortality); the achieved mean LDL-cholesterol concentration was 4.16 mmol/l (161 mg/dl), and the long-term safety of treatment was confirmed41. Carotid intima–media thickness in those treated with statins was similar to that in unaffected siblings, with evidence of a dose–response effect41. Longer-term observational studies (over 3–9 years), combined with clinical experience, also suggest minimal adverse effects of statins, without evidence of muscle injury, liver dysfunction or incident diabetes181,182,183,184,185,186.
Severe FH, particularly HoFH, remains difficult to treat18,22. As a result of markedly elevated LDL-cholesterol concentrations from conception, patients with severe FH have marked acceleration of ASCVD and aortic stenosis, impairing quality of life199,200 and leading to premature death18,22,201,202,203,204,205. The past three decades have seen major advances in treatment104,157,160,206 that have led to improvements in ASCVD outcomes205. The early use of combination cholesterol-lowering therapies, including high-intensity statins, ezetimibe and PCSK9-directed therapies (which act mainly by augmenting LDL receptor (LDLR) function), forms the mainstay of treatment for HoFH18,156,207,208,209,210,211, but the response is dependent on residual LDLR function. The use of probucol has been promoted in Japan to lower LDL-cholesterol concentrations in patients with HoFH212. With the availability of therapies that work independently of LDLR function, such as lomitapide (which inhibits microsomal triglyceride transfer protein) and angiopoietin-like protein 3 (ANGPTL3) inhibitors18,157,213,214,215, lower therapeutic goals for LDL-cholesterol are now achievable. Clinical trials confirm the efficacy of ANGPTL3 inhibitors in patients with HoFH214, including children216. PCSK9 inhibitors are effective in patients with residual LDLR function, but longer-term safety data are required157. Evinacumab (an ANGPTL3 monoclonal antibody) has fewer adverse effects than lomitapide, but its long-term efficacy and safety remain to be confirmed214,215. Lipoprotein apheresis is effective in treating HoFH217,218,219,220,221,222,223 (see specific section discussed subsequently). The use of lipoprotein apheresis in patients with HoFH before, after or in combination with the new LDLR-independent therapies will depend on availability, expertise, costs and patient preference18. Lipoprotein apheresis should, for example, be first used in countries without access to the new therapies. Emerging therapies for HoFH include liver-directed gene transfer of LDLR and CRISPR-based gene editing directed at ANGPTL3 or PCSK9 (refs. 221,224,225). Preliminary studies indicate their potential therapeutic value, but clinical trials of safety and efficacy are required.
Liver transplantation may be offered as a therapeutic option in the context of shared decision-making, particularly in young patients with severe HoFH (caused by biallelic null variants) who are refractory to current therapies and in whom the use of lipoprotein apheresis is not feasible18,104,221,226,227. Liver transplantation can lead to sustained normalization of LDL-cholesterol concentrations228,229,230 and lowering of Lp(a) concentrations. Regression of coronary atherosclerosis has been reported231,232, but effects on aortic stenosis are less clear230,231. Combined liver and heart transplantations from a common donor should be considered in patients with poor cardiac prognosis233. The benefits and risks of liver transplantation in patients with HoFH need to be carefully considered18,221,226,228,229,230,231,232,233,234.
The use of cardiovascular imaging modalities has been advocated for risk stratification and for monitoring of ASCVD during treatment of patients with FH13,16,17,18,76,77,80,147,202,235,236. CT coronary angiography has potential clinical utility because it integrates the effect of LDL-cholesterol burden on ASCVD and can guide therapy, improve patient adherence and assist in prioritizing cardiac investigations (such as invasive coronary angiography and exercise stress testing) in adult patients with HeFH2,17. However, the precise clinical and economical value of this approach remains to be demonstrated. As clinical ASCVD and aortic stenosis are common in patients with HoFH, the use of imaging is integral to management protocols17,18,104,107 for escalating LDL-cholesterol-lowering and other medical treatments and for considering cardiac interventions, such as aortic valve (or root) and coronary artery bypass graft surgery.
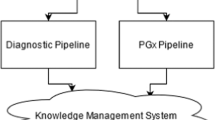
In summary, earlier initiation of treatment, improved adherence to medications, cost minimization and better access to novel therapies are needed to maximize health outcomes for patients with FH. Treatment of FH should fundamentally be patient-centred and underpinned by the core principles of shared decision-making across the continuum of care2,17,198,237,238,239,240. Recommendations are provided for the treatment of adults with HeFH (Table 5 and Fig. 2), children with HeFH (Table 6 and Fig. 2) and patients with HoFH (Table 7 and Fig. 3).
Implementation recommendations on the treatment of patients with FH
-
1.
A personalized treatment plan should be developed for all patients using shared decision-making, considering age, additional risk factors for ASCVD, psychological and sociocultural factors, economic status, barriers to adherence, and personal and family values and preferences.
-
2.
Clear and salient information (in written, diagrammatic and electronic format) that addresses age-related, sociocultural, psychological, language and health literacy barriers should be designed and used to develop personalized treatment plans.
-
3.
Personalized treatment plans for children and adolescents should be designed on the basis of shared decision-making with parents and, in the case of adolescents, using a developmentally appropriate approach.
-
4.
Care pathways should be clearly defined between general practice and paediatric centres: well-controlled and lower-complexity patients should be managed in general practice; less well-controlled (such as those who are not achieving LDL-cholesterol goals or who have several cardiovascular risk factors) and higher-complexity patients (such as those with HoFH) should be managed in specialist centres, with the option of shared care with general practice.
-
5.
Children and adolescents with HoFH should ideally be managed by a multidisciplinary team in centres with paediatric expertise in lipidology, cardiology and apheresis.
-
6.
Management of children and adolescents should ideally focus on the nuclear or immediate family, with (at a minimum) annual reviews in general practice and/or paediatric services to assess well-being, mental health issues, the safety of medication and adherence to therapy.
-
7.
Transition of care of adolescents to adult services should be planned well in advance, and support should be given to facilitate and sustain self-management and involvement in shared management into adulthood.
-
8.
Before prescribing medication and other interventions in children or adolescents with FH, clinicians should engage in a patient-centred and family-centred discussion that uses shared decision-making and covers risk stratification, expected ASCVD risk-reduction benefit, potential adverse effects and drug interactions, sociocultural and economic factors, and values and preferences. At subsequent reviews, clinicians should use, as clinically indicated, a behavioural counselling approach (such as the 5A model of assess, advise, agree, assist and arrange) to address and promote adherence to medication and other treatments.
-
9.
Multifactorial barriers (for example, those related to patients, clinicians, drugs, health-care systems and sociocultural, psychological and financial circumstances) to medication adherence in adult patients with FH should be systematically identified and addressed using appropriate resources by all health service providers; this approach should extend beyond medical care to include a more holistic approach for meeting the emotional, psychological and self-management needs of patients.
-
10.
Clinicians, health systems and health-care plans should identify patients who are not receiving guideline-directed medical therapy and facilitate the initiation of corresponding treatment using multifaceted strategies.
-
11.
Multiple interventions for improving adherence to medication should be used, with appropriate resources, for managing patients with FH; these interventions should include provision of free or subsidized medication, thereby ensuring affordability of established drugs and special access to new drugs; telephone, mobile text, e-mail and calendar reminders; use of single-pill combination drug therapies; expanded role of allied health-care provider interventions, such as simplified dosing by pharmacists and motivational counselling by skilled nurses and pharmacists, and comprehensive multidisciplinary education programmes; patient tools for improving knowledge and understanding of medication and self-care; decision support aids to empower patients and improve the patient–provider relationship; clinical decision support system-based interventions to improve the quality and safety of prescribing; and financial incentives and rewards for treatment goals attained. These strategies should be used in addition to adaptive, complex interventions shown to be effective in the care of other chronic conditions.
-
12.
Iterative strategies, based on key performance indicators (such as adherence to treatment guidelines, attainment of therapeutic goals and patient-reported outcomes and experience measures, notably quality of life in patients with HoFH), should be used regularly or as clinically indicated. These approaches should ideally be part of an audit cycle every 12 months and aim to improve the reach, effectiveness, adoption, implementation and sustainability of service delivery. Multifaceted strategies should be used to improve implementation of treatments.
-
13.
Services for FH should host regular multidisciplinary case discussions, provide local guidance on the best standards of treatment and develop strategies for implementing these recommendations.
-
14.
Paediatric and adult services for FH should participate in a national and international network of FH clinical centres to share educational, clinical and research experience and develop a comprehensive and high-quality registry of patients. Real-world registry data from these collaborations should be regularly used to assess the safety and effectiveness of conventional and new drug therapies, to advocate for policy change to close treatment gaps, to educate registrants and health-care providers and to provide a resource of potential participants for clinical trials of new interventions.
-
15.
Multidisciplinary preoperative and postoperative care, with shared decision-making (involving patients and close relatives), should be prioritized in all management plans for patients with severe HoFH undergoing liver transplantation; as a fundamental principle of quality health care, this radical treatment should be undertaken only in highly experienced paediatric or adult liver transplantation centres.
-
16.
The long-term cardiovascular and lipid outcomes and the complications of liver transplantation, as well as patient-reported outcome measures (including mental health issues), should be audited regularly and recorded in a dedicated registry, and this should be used to promote the best standard of care across all centres.
-
17.
The principles underpinning the concept of rare genetic (or intractable) diseases should be used to seek government funding for comprehensive care of all patients with HoFH, which may include developing a dedicated, specialist centre, as well as special access schemes for new therapies for all patients with HoFH.
See Box 3 for core implementation strategies and Fig. 4 for a summary of recommendations for addressing barriers to adherence.
Factors related to patients, therapy and health-care systems that can be barriers to treatment adherence and potential solutions to overcome these barriers. Adapted with permission from ref. 291, Wiley.
Pregnancy
Fertility rates are unchanged in women with FH. Safe, effective and acceptable methods of contraception are, therefore, of utmost importance in avoiding unplanned pregnancies, especially in women with HoFH18,241. Family planning should be addressed early in both women and men and should involve LDL-cholesterol testing of the partner and counselling; pre-conception counselling and prenatal and pre-implantation genetic testing with counselling of couples known to have FH is particularly important. Pregnancy and lactation in women with FH results in a prolonged exposure to elevated LDL-cholesterol concentrations owing to both the discontinuation of cholesterol-lowering therapy and the physiological changes associated with pregnancy itself242,243,244. This exposure may have effects on the cardiovascular outcomes of mothers and their progeny123,245.
Women with FH should have pre-conception counselling about the risks of pregnancy and have their level of ASCVD risk evaluated, with a full cardiovascular assessment, if clinically indicated246,247. Lifestyle and non-cholesterol risk factors should be optimized, and management options including contraception up to and during pregnancy and lactation should be discussed243,248,249. An individualized approach depending on the severity of the disease, extent of hypercholesterolaemia and the presence or absence of ASCVD should be adopted, weighing the risks and benefits of therapies246,250. Cumulative loss of years on statin treatment during pregnancy and breastfeeding may have a bearing on ASCVD outcomes in women with FH123; early detection and treatment of FH and judicious family planning advice will minimize this potential risk. Children born to a parent with HoFH and a parent without FH are obligate heterozygotes and should be formally diagnosed and offered treatment by the age of 8 years13,14,17.
The need for specific guidelines on the management of dyslipidaemia in pregnancy has been emphasized251. First-generation bile acid sequestrants have been used in pregnancy and are not associated with an increased risk of congenital abnormalities251, but are poorly tolerated252. Colesevelam, a more selective bile acid sequestrant, is the best-tolerated agent, but experience in pregnancy is limited. Women with HoFH at high risk of ASCVD, or with established ASCVD or aortic valve disease, should be offered weekly or fortnightly lipoprotein apheresis, if available, during pregnancy253,254. The risks and benefits of statin and other lipid-lowering therapies during pregnancy should be discussed160,251, and the continued use of statin therapy, or the introduction of statin and other lipid-lowering therapies during the second and third trimesters, considered carefully123,160,241,254,255,256,257,258,259,260,261,262,263. No safety data are available on the use of bempedoic acid, PCSK9 monoclonal antibodies, inclisiran, lomitapide or evinacumab in patients with FH during pregnancy160. The FDA has acknowledged the net benefits of statins during pregnancy in women at very high risk of ASCVD264,265, such as those with HoFH.
Recommendations are provided for the treatment of FH during pregnancy (Table 8).
Implementation recommendations on the treatment of FH during pregnancy
-
1.
The care of pregnant women with FH should be designed to meet the needs of local, regional and remote communities; services should be multidisciplinary, involve the general practitioner of the patient, and ideally be coordinated by a clinician with expertise in FH and obstetric medicine.
-
2.
All women with FH who are planning a pregnancy should ideally be referred for further advice to a specialist centre that provides a dedicated multidisciplinary service and holistic care. Such a service should include care of medical conditions (such as depression, hypertension and gestational diabetes) and counselling (such as psychological and mental health issues) and take account of sociocultural background and preferences and values of patients.
-
3.
Clear and relevant information (in written, diagrammatic, pictorial and electronic formats) that addresses sociocultural, language and health literacy barriers should be designed and offered to women during pregnancy-related counselling sessions. This information should include shared decision-making, choice of contraception, importance of heart-healthy behaviours, risks of pregnancy, drug safety and teratogenicity, risk of ASCVD from cessation of drug therapy, and care during lactation.
-
4.
Iterative strategies should be used, based on key performance clinical indicators, such as maternal-reported outcome and experience measures, fetal outcomes and quality of life of patients to improve the implementation of care.
-
5.
Existing clinical resources (such as obstetric and gynaecological medicine, lipidology, dietetics, nursing, mental health care, family planning, genetic counselling, imaging facilities, cardiology and diabetes services) should be adapted to provide an integrated model of care for women with FH planning and undergoing pregnancy241,251,266,267.
-
6.
A clinical quality registry of pregnant women with FH, linked to patient-reported and experience measures, should be used to improve pregnancy and family care.
Lipoprotein apheresis and related pharmacotherapies
Extracorporeal removal of cholesterol-carrying lipoproteins to treat hyperlipidaemia initially involved plasma exchange. This approach was subsequently replaced by lipoprotein apheresis using adsorption, differential filtration or precipitation to selectively remove the apolipoprotein B-containing lipoproteins — LDL and Lp(a) — from plasma or whole blood217. Lipoprotein apheresis is a safe and effective means of treating patients with HoFH on a lifelong basis, especially in combination with statins and ezetimibe. Treating 1.5–2.0 times the blood or plasma volumes weekly plus optimal cholesterol-lowering drug therapy reduces interval mean values of LDL-cholesterol by 64–77%218,219,220. Retrospective surveys of patients with HoFH have shown that the lower the LDL-cholesterol concentration when receiving lipoprotein apheresis combined with drug treatment, the greater the reduction in mortality203,204. Effectively lowering LDL-cholesterol concentrations with lipoprotein apheresis has also been associated with a reduction in supravalvular aortic stenosis148 and regression of tendon xanthomas221,222. Despite its therapeutic value, for logistical and economic reasons, lipoprotein apheresis is not universally available or used18,22.
Lipoprotein apheresis robustly reduces elevated concentrations of both Lp(a) and LDL-cholesterol, unlike all currently available cholesterol-lowering drugs, and is a safe means of treating children aged <12 years and pregnant women with HoFH77,254. However, its use in other forms of severe hyperlipidaemia, such as statin-refractory HeFH, is diminishing because of the efficacy of PCSK9 inhibitors223,268. The future use of lipoprotein apheresis in patients with HoFH may also decrease because of the effectiveness of lomitapide215,269,270 and the ANGPTL3 inhibitor evinacumab214. However, lipoprotein apheresis will continue to be the last resort in patients ineligible for, refractory to or intolerant of cholesterol-lowering drugs271; lipoprotein apheresis might also be the best option in countries without access to newer pharmacotherapies221. Liver transplantation was referred to earlier as a last resort for patients with HoFH who cannot tolerate lipoprotein apheresis and are refractory to all other therapies221,230,272. More studies addressing the experiences and health-related quality of life of patients with HoFH receiving lipoprotein apheresis are needed199,273. The following recommendations (Table 9) are updated from existing guidelines on the role of lipoprotein apheresis and novel cholesterol-lowering drugs in managing patients with FH or raised Lp(a) concentrations15,16,18,69,77,80,202,274,275.
Implementation recommendations on the treatment of FH by lipoprotein apheresis
-
1.
All patients being considered for lipoprotein apheresis should be assessed for physical and psychological suitability for treatment by a specialist with training in lipidology and experience in apheresis, supported by other specialists where indicated.
-
2.
If lipoprotein apheresis is not available or feasible (for example, because of a lack of resources or in children with HoFH who have a small blood volume), the use of therapeutic plasma exchange (which is more widely available) should be considered as an alternative.
-
3.
Facilities and resources for apheresis services should be regularly reviewed and cost analyses submitted to the relevant organization to obtain adequate financial support for the service.
-
4.
Apheresis services should be designed to meet local needs and be centralized in a dedicated unit, headed by a director who should be the lead of a multidisciplinary team of accredited personnel.
-
5.
Existing clinical infrastructure (for example, haemodialysis, transfusion medicine and vascular surgery services) should be adapted to improve the availability of lipoprotein apheresis and to increase the quality of the service.
-
6.
Given the varied expertise required to provide a quality apheresis service, a coalition of specialties (including lipidology, cardiology, vascular surgery, paediatrics, mental health care, nephrology, transfusion medicine, pharmacy and nursing) should be established; this coalition should hold regular multidisciplinary case meetings, plan implementation strategies for improving service delivery and develop local guidance on the best evidence-based standard of care.
-
7.
Key performance indicators, such as the efficacy, tolerability and safety of lipoprotein apheresis, as well as the effect on patient-reported outcomes and experiences (including quality of life) should be reviewed as clinically indicated and as part of a regular audit cycle every 12 months.
-
8.
Apheresis units should participate in a national or international network of similar centres to share educational, clinical and research experience and to establish and consolidate a comprehensive clinical quality registry of patients receiving treatment.
See Box 4 for core implementation strategies.
General strategies for the implementation of care
Despite the development of several international and country-specific guidelines for the care of FH, substantial gaps remain in their implementation into practice23,28. Accordingly, <10% of the estimated 35 million people with FH worldwide have been diagnosed, with <1% of cases identified in most countries201. Furthermore, many patients with FH receiving treatment are not attaining LDL-cholesterol goals, with substantial gaps in the care of those with severe FH or HoFH. Major knowledge gaps among patients, clinicians and health-care systems further hinder implementation29,276,277. Action is required to alter processes, structures and health-care teams to improve the organization and delivery of care52,278. Implementation evidence is essential to effectively manage the changes in health care29,32.
Design and assessment of implementation recommendations
The use of implementation science to improve clinical practice guidelines has been reviewed previously29,279. A five-step process should be followed29:
-
1.
Define the evidence-based practice or intervention.
-
2.
Choose an implementation theory, model or framework.
-
3.
Assess determinants, barriers, enablers and context in respect of the practice or intervention.
-
4.
Select implementation strategies.
-
5.
Select options for assessing the outcomes of implementation.
Implementation science entails the design of processes, termed ‘implementation strategies’, to overcome barriers to and leverage enablers of improved care280,281. Implementation science is fundamentally an operational tool to change practice on the basis of the best evidence-informed guidance (step 1), such as clinical practice recommendations provided in this guidance article. Informed by an appropriate implementation model (step 2) and knowledge of barriers and enablers (step 3), implementation strategies can be used to implement clinical guidelines. We have used the ERIC taxonomy37 (Supplementary Material 1 Appendix 5) to develop general and specific implementation recommendations in this guidance (step 4).
The development of new guidance on FH provides an opportunity to identify potential strategies that could be used to implement recommendations into policy and practice and research their effect on patient outcomes32,282. Researching implementation requires the selection of processes for monitoring and evaluating implementation strategies (step 5)29. The value of tailored implementation strategies for improving the care of patients with FH is well supported by several studies58,101,283,284,285,286.
A pathway for the iterative development and implementation of cardiovascular guidelines to improve their translation into practice has been recommended32. This guidance article on FH proposes both clinical and implementation recommendations to enable translation into policy and practice29,32. Local implementation requires an initial assessment of barriers to and facilitators of change, paired with the tailoring of strategies to implement a change in practice32. Similar to clinical quality improvement, successful implementation practice relies on monitoring, evaluation and ongoing efforts to ensure the sustainability of changes287. This cyclical and iterative process builds new evidence for the implementation of future clinical practice recommendations. The success of implementation in addressing gaps in clinical practice relies on implementing behavioural change at multiple levels of the adaptive health-care system2,32,288.
General implementation recommendations
-
1.
The design and implementation of health services for FH should deliver quality care that is patient-centred, safe, effective, efficient, equitable, well led and integrated, and sustainably resourced.
-
2.
Care and support processes for FH should be widely based on evidence from public health and prevention and precision medicine; these should be adapted to local, regional and national needs, guided by contextual barriers and facilitators, and subjected to regular evaluation.
-
3.
Implementation of improvements in the detection and care of FH should be underpinned by an integrated national cholesterol awareness campaign targeted at young people, high-risk individuals and all health-care professionals.
-
4.
National and regional centres with expertise in lipidology, genetics and ASCVD prevention should be established to accept referrals and give advice, as indicated. All patients with suspected FH should be referred to, or discussed with, a relevant specialist to plan further management and care; a key priority is to establish specialized centres for managing patients with severe FH or HoFH.
-
5.
General practice and primary care should be actively involved in the care of all individuals and families with FH and provide support for screening, diagnosing, managing cholesterol-lowering therapy and addressing comorbidities; regular review and evaluation of health and patient-reported outcomes data are essential.
-
6.
A multidisciplinary team with expertise in caring for individuals with FH should partner with primary care and include representation from appropriate specialty disciplines, including mental health care.
-
7.
Models of care should ideally consider the entire family as a patient unit. Appropriate strategies for paediatric patients to transition to adult care should be used.
-
8.
Individuals with FH should be active participants in their care and work with their primary care and multidisciplinary team to discuss care pathways.
-
9.
Patient-reported outcome and experience measures form the bedrock of value-based health care and should accordingly be used to improve implementation practice across the continuum of care for FH.
-
10.
The implementation of all clinical recommendations for FH should account, as a priority, for the access to and the acceptability of health services for patients and families of diverse ancestries, including minority groups.
-
11.
Health services should partner with academic and professional organizations and foundations to improve teaching, training and research.
-
12.
When planning and designing treatment protocols across the continuum of care for FH, service providers should seek the collaboration of another clinical centre that provides excellence of care and arrange for relevant staff to visit and train there.
-
13.
All health professionals involved in the care of individuals with FH, including those at the primary care level, should have appropriate accreditation, in addition to ongoing education, training and skills in lipidology, cardiovascular disease prevention, family communication, interpretation of test results, local guidance on data protection, and genomic medicine. Clinical practice guidelines for managing FH should be simplified to improve accessibility and use by all health-care professionals.
-
14.
Digital technologies (telehealth, adherence applications and decision support systems in electronic health records) that target both patients and clinicians should be developed to improve the precision, accuracy and communication of the detection and management of FH.
-
15.
Awareness, advocacy and educational campaigns including social media, website banner advertisements, billboards and/or celebrity endorsements should be conducted to increase public awareness of FH and the importance of genetic testing.
-
16.
Advocacy and peer groups of patients, family members and other stakeholders should be established to support patients with FH and their care, particularly across different sociocultural communities, levels of health literacy and economic circumstances; advocacy for patients with HoFH is crucial for ensuring that health policy addresses all aspects of the care of this most severe form of FH (Supplementary Material 5).
-
17.
Sustainable financing and sharing of existing resources should be used, enabled by key opinion leaders and stakeholder organizations, to deliver an impactful and cost-effective clinical service.
-
18.
The national coding systems for FH should be used in primary and specialist care to improve the precision of data acquisition and linkage and their use for audit, research and development of health policy.
-
19.
A national registry for FH should be established and used for linking patient outcomes, raising awareness, improving advocacy efforts and iteratively auditing key performance indicators, and for international collaborations for improving care.
-
20.
Comprehensive research strategies and programmes, based on the core principles of implementation science, should be developed for evaluating and improving all models of care for FH. This process should focus on the acceptability, adoption, appropriateness, cost, feasibility, fidelity and sustainability of all interventions.
See Box 5 for core general implementation strategies.
Conclusions
Updating models of care meets international calls to action on FH9,24,25. This guidance aims to provide comprehensive recommendations for providing the best clinical care for the greatest number of people with FH worldwide. The recommendations inform both broad and narrow areas of practice across the continuum of care2,17. Strong recommendations, mostly informed by high-quality evidence, as well as by common sense, should be followed as best practice, whereas the weaker recommendations are optional and provide a basis for further research2,16,17,36,289 (for references supporting recommendations, see Supplementary Material 6). Because of economic, political, cultural and social differences among countries, the recommendations we make might not be universally applicable or adopted.
Nevertheless, exponential growth in new knowledge on the diagnosis and effective therapies for FH2 has set a precedence for countries to aspire to developing high-quality, integrated health-care systems for FH2,9,23,24,25. A challenge for health-care organizations is adapting to the demands of the complexities of changes required2. Implementation science provides the best methodology to address this challenge and was, therefore, used to support the clinical recommendations29,30,32,280.
However, evaluating implementation practice, including patient-reported outcomes and experiences, is an ongoing challenge for evolving models of care for patients with FH29,32,37,280. Beyond observational investigations, future implementation research on FH should involve interventional studies, ideally based on randomized, stepped-wedge, hybrid, counterbalanced and adaptive designs32,279,287. Researchers should make particular efforts to include subjects from diverse socioeconomic strata, ancestries and geographical location. These studies would increase generalizability and allow replication of findings across different real-world settings. The development and utilization of integrated care systems to improve the health outcomes of all patients with FH remains a global challenge for implementation programmes290.
References
Defesche, J. C. et al. Familial hypercholesterolaemia. Nat. Rev. Dis. Prim. 3, 17093 (2017).
Watts, G. F. et al. Familial hypercholesterolaemia: evolving knowledge for designing adaptive models of care. Nat. Rev. Cardiol. 17, 360–377 (2020).
Ference, B. A. et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 38, 2459–2472 (2017).
Beheshti, S. O., Madsen, C. M., Varbo, A. & Nordestgaard, B. G. Worldwide prevalence of familial hypercholesterolemia: meta-analyses of 11 million subjects. J. Am. Coll. Cardiol. 75, 2553–2566 (2020).
Beheshti, S., Madsen, C. M., Varbo, A., Benn, M. & Nordestgaard, B. G. Relationship of familial hypercholesterolemia and high LDL cholesterol to ischemic stroke: the Copenhagen General Population Study. Circulation 138, 578–589 (2018).
Svendsen, K. et al. Risk of stroke in genetically verified familial hypercholesterolemia: a prospective matched cohort study. Atherosclerosis 358, 34–40 (2022).
Centers for Disease Control and Prevention. Tier 1 Genomic Applications Toolkit for Public Health Departments. CDC https://www.cdc.gov/genomics/implementation/toolkit/index.htm (2014).
Hu, P. et al. Prevalence of familial hypercholesterolemia among the general population and patients with atherosclerotic cardiovascular disease: a systematic review and meta-analysis. Circulation 141, 1742–1759 (2020).
Ray, K. et al. World Heart Federation Cholesterol Roadmap 2022. Glob. Heart 17, 75 (2022).
Grundy, S. M. et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 73, e285–e350 (2019).
Mach, F. et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the Management of Dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 41, 111–188 (2020).
National Institute for Health and Clinical Excellence. NICE Clinical Guideline 71: Familial hypercholesterolaemia: identification and management. NICE https://www.nice.org.uk/guidance/cg71/chapter/recommendations (2019).
Wiegman, A. et al. Familial hypercholesterolaemia in children and adolescents: gaining decades of life by optimizing detection and treatment. Eur. Heart J. 36, 2425–2437 (2015).
Ramaswami, U. et al. Current management of children and young people with heterozygous familial hypercholesterolaemia — HEART UK statement of care. Atherosclerosis 290, 1–8 (2019).
de Ferranti, S. D. et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association. Circulation 139, e603–e634 (2019).
Gidding, S. S. et al. The agenda for familial hypercholesterolemia — a scientific statement from the American Heart Association. Circulation 132, 2167–2192 (2015).
Watts, G. F. et al. Integrated guidance for enhancing the care of familial hypercholesterolaemia in Australia. Heart Lung Circ. 30, 324–349 (2021).
Cuchel, M. et al. 2023 Update on European Atherosclerosis Society Consensus Statement on Homozygous Familial Hypercholesterolaemia: new treatments and clinical guidance. Eur. Heart J. https://doi.org/10.1093/eurheartj/ehad197 (2023).
Santos, R. D. et al. Clinical and molecular aspects of familial hypercholesterolemia in Ibero-American countries. J. Clin. Lipidol. 11, 160–166 (2017).
Pang, J. et al. Comparative aspects of the care of familial hypercholesterolemia in the ‘Ten Countries Study’. J. Clin. Lipidol. 13, 287–300 (2019).
Vallejo-Vaz, A. J. et al. Global perspective of familial hypercholesterolaemia: a cross-sectional study from the EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). Lancet 398, 1713–1725 (2021).
Tromp, T. R. et al. Worldwide experience of homozygous familial hypercholesterolaemia: retrospective cohort study. Lancet 399, 719–728 (2022).
Representatives of the Global Familial Hypercholesterolemia Community. Reducing the clinical and public health burden of familial hypercholesterolemia — a global call to action. JAMA Cardiol. 5, 217–229 (2020).
Groselj, U., Wiegman, A. & Gidding, S. S. Screening in children for familial hypercholesterolaemia: start now. Eur. Heart J. 43, 3209–3212 (2022).
Vallejo-Vaz, A. J. et al. Familial hypercholesterolaemia: a global call to arms. Atherosclerosis 243, 257–259 (2015).
Wei, N. et al. A bibliometric analysis of familial hypercholesterolemia from 2011 to 2021. Curr. Probl. Cardiol. https://doi.org/10.1016/j.cpcardiol.2022.101151 (2022).
Nieuwlaat, R., Schwalm, J.-D., Khatib, R. & Yusuf, S. Why are we failing to implement effective therapies in cardiovascular disease? Eur. Heart J. 34, 1262–1269 (2013).
Uchmanowicz, I. et al. Optimising implementation of European guidelines on cardiovascular disease prevention in clinical practice: what is needed? Eur. J. Prev. Cardiol. 28, 426–431 (2021).
Jones, L. K., Brownson, R. C. & Williams, M. S. Applying implementation science to improve care for familial hypercholesterolemia. Curr. Opin. Endocrinol. Diabetes Obes. 29, 141–151 (2022).
Bauer, M. S. & Kirchner, J. Implementation science: what is it and why should I care? Psychiatry Res. 283, 112376 (2020).
O’Shea, R., Ma, A. S., Jamieson, R. V. & Rankin, N. M. Precision medicine in Australia: now is the time to get it right. Med. J. Aust. 217, 559–563 (2022).
Sarkies, M. N., Jones, L. K., Gidding, S. S. & Watts, G. F. Improving clinical practice guidelines with implementation science. Nat. Rev. Cardiol. 19, 3–4 (2022).
Migliara, G. et al. Familial hypercholesterolemia: a systematic review of guidelines on genetic testing and patient management. Front. Public Health 5, 252 (2017).
Brouwers, M. C. et al. Development and validation of a tool to assess the quality of clinical practice guideline recommendations. JAMA Netw. Open 3, e205535 (2020).
Jacobson, T. A. et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 1 — full report. J. Clin. Lipidol. 9, 129–169 (2015).
Guyatt, G. H. et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br. Med. J. 336, 924–926 (2008).
Powell, B. J. et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement. Sci. 10, 21 (2015).
Wilson, J. M. G. & Jungner, G. Principles and practice of screening for disease. WHO Chron. 22, 473 (1968).
Andermann, A., Blancquaert, I., Beauchamp, S. & Déry, V. Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bull. World Health Organ. 86, 317–319 (2008).
Falkner, B. & Gidding, S. Life-course implications of pediatric risk factors for cardiovascular disease. Can. J. Cardiol. 37, 766–775 (2021).
Luirink, I. et al. 20-Year follow-up of statins in children with familial hypercholesterolaemia. N. Engl. J. Med. 381, 1547–1556 (2019).
Ibrahim, S., Reeskamp, L. F., Stroes, E. S. & Watts, G. F. Advances, gaps and opportunities in the detection of familial hypercholesterolemia: overview of current and future screening and detection methods. Curr. Opin. Lipidol. 31, 347–355 (2020).
Qureshi, N. et al. Strategies for screening for familial hypercholesterolaemia in primary care and other community settings. Cochrane Database Syst. Rev. 10, CD012985 (2021).
Jahn, B. et al. Familial hypercholesterolemia: a systematic review of modeling studies on screening interventions. Atherosclerosis 355, 15–29 (2022).
Carvalho, C. et al. Application of a risk stratification tool for familial hypercholesterolaemia in primary care: an observational cross-sectional study in an unselected urban population. Heart 107, 1220–1225 (2021).
Wald, D. S. et al. Child–parent familial hypercholesterolemia screening in primary care. N. Engl. J. Med. 375, 1628–1637 (2016).
McKay, A. J. et al. Universal screening at age 1–2 years as an adjunct to cascade testing for familial hypercholesterolaemia in the UK: a cost–utility analysis. Atherosclerosis 275, 434–443 (2018).
Klančar, G. et al. Universal screening for familial hypercholesterolemia in children. J. Am. Coll. Cardiol. 66, 1250–1257 (2015).
Matsunaga, K. et al. Universal screening for familial hypercholesterolemia in children in Kagawa, Japan. J. Atheroscler. Thromb. 29, 839–849 (2022).
Morris, J. K., Wald, D. S. & Wald, N. J. The evaluation of cascade testing for familial hypercholesterolemia. Am. J. Med. Genet. A 158, 78–84 (2012).
Wald, D. S. & Bestwick, J. P. Reaching detection targets in familial hypercholesterolaemia: comparison of identification strategies. Atherosclerosis 293, 57–61 (2020).
Murray, M. F. et al. DNA-based screening and population health: a points to consider statement for programs and sponsoring organizations from the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 23, 989–995 (2021).
Grzymski, J. et al. Population genetic screening efficiently identifies carriers of autosomal dominant diseases. Nat. Med. 26, 1235–1239 (2020).
Buchanan, A. H. et al. Clinical outcomes of a genomic screening program for actionable genetic conditions. Genet. Med. 22, 1874–1882 (2020).
Khoury, M. J. & Dotson, W. D. From genes to public health: are we ready for DNA-based population screening? Genet. Med. 23, 996–998 (2021).
Held, P. K. et al. Analytical validation of familial hypercholesterolemia biomarkers in dried blood spots. Int. J. Neonatal Screen. 8, 14 (2022).
Downie, L., Halliday, J., Lewis, S. & Amor, D. J. Principles of genomic newborn screening programs: a systematic review. JAMA Netw. Open 4, e2114336 (2021).
Jones, L. K. et al. Evaluation of a multidisciplinary lipid clinic to improve the care of individuals with severe lipid conditions: a RE-AIM framework analysis. Implement. Sci. Commun. 2, 32 (2021).
Jones, L. K. et al. Barriers, facilitators, and solutions to familial hypercholesterolemia treatment. PLoS ONE 15, e0244193 (2020).
Gidding, S. S. Familial hypercholesterolemia: the Atlantic Divide. J. Pediatr. https://doi.org/10.1016/j.jpeds.2022.09.021 (2022).
Public Health England. Familial hypercholesterolaemia implementing a systems approach to detection and management. Public Health England https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/731873/familial_hypercholesterolaemia_implementation_guide.pdf (2018).
Peters, D. H., Tran, N. T. & Adam, T. Implementation research in health: a practical guide. WHO https://www.who.int/iris/bitstream/10665/91758/1/9789241506212_eng.pdf (2013).
Sturm, A. C. et al. Clinical genetic testing for familial hypercholesterolemia: JACC Scientific Expert Panel. J. Am. Coll. Cardiol. 72, 662–680 (2018).
Ibrahim, S., Defesche, J. & Kastelein, J. J. P. Beyond the usual suspects: expanding on mutations and detection for familial hypercholesterolemia. Expert. Rev. Mol. Diagn. 21, 887–895 (2021).
Sniderman, A. D., Glavinovic, T. & Thanassoulis, G. Key questions about familial hypercholesterolemia: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 79, 1023–1031 (2022).
Sturm, A. C. et al. Limited-variant screening vs comprehensive genetic testing for familial hypercholesterolemia diagnosis. JAMA Cardiol. 6, 902–909 (2021).
Gandhi, G. D. et al. Assessing the genetic burden of familial hypercholesterolemia in a large middle eastern biobank. J. Transl. Med. 20, 502 (2022).
Haralambos, K. et al. Clinical experience of scoring criteria for familial hypercholesterolaemia (FH) genetic testing in Wales. Atherosclerosis 240, 190–196 (2015).
Brunham, L. R. et al. Canadian cardiovascular society position statement on familial hypercholesterolemia: update 2018. Can. J. Cardiol. 34, 1553–1563 (2018).
Harada-Shiba, M. et al. Guidelines for the diagnosis and treatment of adult familial hypercholesterolemia 2022. J. Atheroscler. Thromb. https://doi.org/10.5551/jat.CR005 (2023).
Pina, A. et al. Virtual genetic diagnosis for familial hypercholesterolemia powered by machine learning. Eur. J. Prev. Cardiol. 27, 1639–1646 (2020).
Correia, M., Kagenaar, E., van Schalkwijk, D. B., Bourbon, M. & Gama-Carvalho, M. Machine learning modelling of blood lipid biomarkers in familial hypercholesterolaemia versus polygenic/environmental dyslipidaemia. Sci. Rep. 11, 801 (2021).
Hesse, R., Raal, F. J., Endo, C., Blom, D. & George, J. A. Familial hypercholesterolemia identification by machine learning using lipid profile data performs as well as clinical diagnostic criteria. Circ. Genom. Precis. Med. 15, e003324 (2022).
Khoury, M. et al. The detection, evaluation, and management of dyslipidemia in children and adolescents: a Canadian Cardiovascular Society/Canadian Pediatric Cardiology Association Clinical Practice Update. Can. J. Cardiol. 38, 1168–1179 (2022).
Starr, B. et al. Development of sensitive and specific age- and gender-specific low-density lipoprotein cholesterol cutoffs for diagnosis of first-degree relatives with familial hypercholesterolaemia in cascade testing. Clin. Chem. Lab. Med. 46, 791–803 (2008).
Nohara, A. et al. Homozygous familial hypercholesterolemia. J. Atheroscler. Thromb. 28, 665–678 (2021).
France, M. et al. HEART UK statement on the management of homozygous familial hypercholesterolaemia in the United Kingdom. Atherosclerosis 255, 128–139 (2016).
Sjouke, B. et al. Homozygous autosomal dominant hypercholesterolaemia in the Netherlands: prevalence, genotype–phenotype relationship, and clinical outcome. Eur. Heart J. 36, 560–565 (2015).
Bertolini, S. et al. Homozygous familial hypercholesterolemia in Italy: clinical and molecular features. Atherosclerosis 312, 72–78 (2020).
Santos, R. D. et al. Defining severe familial hypercholesterolaemia and the implications for clinical management: a consensus statement from the International Atherosclerosis Society Severe Familial Hypercholesterolemia Panel. Lancet Diabetes Endocrinol. 4, 850–861 (2016).
Funabashi, S. et al. Substantially elevated atherosclerotic risks in Japanese severe familial hypercholesterolemia defined by the International Atherosclerosis Society. JACC Asia 1, 245–255 (2021).
Langsted, A., Kamstrup, P. R., Benn, M., Tybjærg-Hansen, A. & Nordestgaard, B. G. High lipoprotein(a) as a possible cause of clinical familial hypercholesterolaemia: a prospective cohort study. Lancet Diabetes Endocrinol. 4, 577–587 (2016).
Chan, D. C. et al. Effect of lipoprotein(a) on the diagnosis of familial hypercholesterolemia: does it make a difference in the clinic? Clin. Chem. 65, 1258–1266 (2019).
Tromp, T. R. et al. Use of lipoprotein(a) to improve diagnosis and management in clinical familial hypercholesterolemia. Atherosclerosis 365, 27–33 (2023).
Yeang, C., Witztum, J. L. & Tsimikas, S. Novel method for quantification of lipoprotein(a)-cholesterol: implications for improving accuracy of LDL-C measurements. J. Lipid Res. 62, 100053 (2021).
Kronenberg, F. et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement. Eur. Heart J. 43, 3925–3946 (2022).
Yeang, C. et al. Effect of pelacarsen on lipoprotein(a) cholesterol and corrected low-density lipoprotein cholesterol. J. Am. Coll. Cardiol. 79, 1035–1046 (2022).
Brown, E. E. et al. Genetic testing in dyslipidemia: a scientific statement from the National Lipid Association. J. Clin. Lipidol. 14, 398–413 (2020).
Khera, A. V. et al. Diagnostic yield and clinical utility of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. J. Am. Coll. Cardiol. 67, 2578–2589 (2016).
Paquette, M. et al. Effect of the LDL receptor mutation type on incident major adverse cardiovascular events in familial hypercholesterolaemia. Eur. J. Prev. Cardiol. 29, 2125–2131 (2022).
Landstrom, A. P. et al. Genetic testing for heritable cardiovascular diseases in pediatric patients: a scientific statement from the American Heart Association. Circ. Genom. Precis. Med. 14, e000086 (2021).
Musunuru, K. et al. Genetic testing for inherited cardiovascular diseases: a scientific statement from the American Heart Association. Circ. Genom. Precis. Med. 13, e000067 (2020).
Berberich, A. J. & Hegele, R. A. The advantages and pitfalls of genetic analysis in the diagnosis and management of lipid disorders. Best. Pract. Res. Clin. Endocrinol. Metab. 37, 101719 (2023).
Brown, E. E. The genetic counselor’s role in management of patients with dyslipidemia. Curr. Opin. Lipidol. 32, 83–88 (2021).
Marchand, M., Chen, V., Trinder, M., Cermakova, L. & Brunham, L. Patient perspectives regarding genetic testing for familial hypercholesterolemia. CJC Open 3, 557–564 (2020).
Berberich, A. J. & Hegele, R. A. The complex molecular genetics of familial hypercholesterolaemia. Nat. Rev. Cardiol. 16, 9–20 (2019).
Khera, A. V. & Hegele, R. A. What is familial hypercholesterolemia, and why does it matter? Circulation 141, 1760–1763 (2020).
Cao, Y.-X. et al. Improvement of definite diagnosis of familial hypercholesterolemia using an expanding genetic analysis. JACC Asia 1, 82–89 (2021).
Leren, T. P. & Bogsrud, M. P. The importance of cascade genetic screening for diagnosing autosomal dominant hypercholesterolemia: results from twenty years of a national screening program in Norway. J. Clin. Lipidol. 15, 674–681 (2021).
Loh, W. J., Chan, D. C., Mata, P. & Watts, G. F. Familial hypercholesterolemia and elevated lipoprotein(a): cascade testing and other implications for contextual models of care. Front. Genet. 13, 905941 (2022).
Jones, L. K. et al. Acceptability, appropriateness, and feasibility of automated screening approaches and family communication methods for identification of familial hypercholesterolemia: stakeholder engagement results from the IMPACT-FH study. J. Pers. Med. 11, 587 (2021).
Campbell-Salome, G. et al. Motivating cascade testing for familial hypercholesterolemia: applying the extended parallel process model for clinician communication. Transl. Behav. Med. 12, 800–809 (2022).
Leonardi-Bee, J. et al. Effectiveness of cascade testing strategies in relatives for familial hypercholesterolemia: a systematic review and meta-analysis. Atherosclerosis 338, 7–14 (2021).
Reijman, M. D., Kusters, D. M. & Wiegman, A. Advances in familial hypercholesterolaemia in children. Lancet Child. Adolesc. Health 5, 652–661 (2021).
Pérez de Isla, L. et al. Predicting cardiovascular events in familial hypercholesterolemia: the SAFEHEART registry. Circulation 135, 2133–2144 (2017).
Bianconi, V., Banach, M. & Pirro, M. Why patients with familial hypercholesterolemia are at high cardiovascular risk? Beyond LDL-C levels. Trends Cardiovasc. Med. 31, 205–215 (2021).
Gallo, A., Mszar, R. & Miname, M. H. Updates on the use of subclinical atherosclerosis to predict risk of cardiovascular events in heterozygous familial hypercholesterolemia. Curr. Atheroscler. Rep. 24, 407–418 (2022).
Alonso, R. et al. Lipoprotein(a) levels in familial hypercholesterolaemia: an important predictor for cardiovascular disease independent of the type of LDL-receptor mutation. J. Am. Coll. Cardiol. 63, 1982–1989 (2014).
Ellis, K. L. et al. Value of measuring lipoprotein(a) during cascade testing for familial hypercholesterolemia. J. Am. Coll. Cardiol. 73, 1029–1039 (2019).
Pérez de Isla, L. et al. A resilient type of familial hypercholesterolaemia: case–control follow-up of genetically characterized older patients in the SAFEHEART cohort. Eur. J. Prev. Cardiol. 29, 795–801 (2021).
Hedegaard, B. S. et al. Equivalent impact of elevated lipoprotein(a) and familial hypercholesterolemia in patients with atherosclerotic cardiovascular disease. J. Am. Coll. Cardiol. 80, 1998–2010 (2022).
Nazli, S. A. et al. Familial hypercholesterolaemia and coronary risk factors among patients with angiogram-proven premature coronary artery disease in an Asian cohort. PLoS ONE 17, e0273896 (2022).
Paquette, M. et al. Familial hypercholesterolemia-risk-score: a new score predicting cardiovascular events and cardiovascular mortality in familial hypercholesterolemia. Arterioscler. Thromb. Vasc. Biol. 41, 2632–2640 (2021).
McKay, A. J., Gunn, L. H. & Ray, K. K. Assessing the external validity of the SAFEHEART risk prediction model in patients with familial hypercholesterolaemia in an English routine care cohort. Atherosclerosis 358, 68–74 (2022).
Agarwala, A. et al. Racial disparities in modifiable risk factors and statin usage in Black patients with familial hypercholesterolemia. J. Am. Heart Assoc. 10, e020890 (2021).
Pérez de Isla, L. et al. Lipoprotein(a), LDL-cholesterol, and hypertension: predictors of the need for aortic valve replacement in familial hypercholesterolaemia. Eur. Heart J. 42, 2201–2211 (2021).
Funabashi, S. et al. Characterization of polyvascular disease in heterozygous familial hypercholesterolemia: its association with circulating lipoprotein(a) levels. J. Am. Heart Assoc. 11, e025232 (2022).
Myers, K. D. et al. COVID-19 associated risks of myocardial infarction in persons with familial hypercholesterolemia with or without ASCVD. Am. J. Prev. Cardiol. 7, 100197 (2021).
Coutinho, E. R. et al. Familial hypercholesterolemia and cardiovascular disease in older individuals. Atherosclerosis 318, 32–37 (2021).
Iyen, B. et al. Sex differences in cardiovascular morbidity associated with familial hypercholesterolaemia: a retrospective cohort study of the UK Simon Broome register linked to national hospital records. Atherosclerosis 315, 131–137 (2020).
Amrock, S. M. et al. Health disparities among adult patients with a phenotypic diagnosis of familial hypercholesterolemia in the CASCADE-FH™ patient registry. Atherosclerosis 267, 19–26 (2017).
Zamora, A. et al. Women with familial hypercholesterolemia phenotype are undertreated and poorly controlled compared to men. Sci. Rep. 13, 1492 (2023).
Klevmoen, M. et al. Loss of statin treatment years during pregnancy and breastfeeding periods in women with familial hypercholesterolemia. Atherosclerosis 335, 8–15 (2021).
Cho, L. et al. Summary of updated recommendations for primary prevention of cardiovascular disease in women: JACC state-of-the-art review. J. Am. Coll. Cardiol. 75, 2602–2618 (2020).
Okoth, K. et al. Association between the reproductive health of young women and cardiovascular disease in later life: umbrella review. Br. Med. J. 371, m3502 (2020).
Bjelakovic, B. et al. Risk assessment and clinical management of children and adolescents with heterozygous familial hypercholesterolaemia. A position paper of the associations of preventive pediatrics of Serbia, mighty medic and international lipid expert panel. J. Clin. Med. 10, 4930 (2021).
Ramaswami, U. & Humphries, S. E. Management of familial hypercholesterolaemia in childhood. Curr. Opin. Pediatr. 32, 633–640 (2020).
Trinder, M. et al. Polygenic contribution to low-density lipoprotein cholesterol levels and cardiovascular risk in monogenic familial hypercholesterolemia. Circ. Genom. Precis. Med. 13, 515–523 (2020).
Fahed, A. C. et al. Polygenic background modifies penetrance of monogenic variants for tier 1 genomic conditions. Nat. Commun. 11, 3635 (2020).
Aragam, K. G. et al. Limitations of contemporary guidelines for managing patients at high genetic risk of coronary artery disease. J. Am. Coll. Cardiol. 75, 2769–2780 (2020).
Bolli, A., Di Domenico, P., Pastorino, R., Busby, G. B. & Bottà, G. Risk of coronary artery disease conferred by low-density lipoprotein cholesterol depends on polygenic background. Circulation 143, 1452–1454 (2021).
Christoffersen, M. & Tybjærg-Hansen, A. Polygenic risk scores: how much do they add? Curr. Opin. Lipidol. 32, 157–162 (2021).
Pérez de Isla, L. et al. Coronary heart disease, peripheral arterial disease, and stroke in familial hypercholesterolaemia. Arterioscler. Thromb. Vasc. Biol. 36, 2004–2010 (2016).
Kitahara, H. et al. Extent of lipid core plaque in patients with Achilles tendon xanthoma undergoing percutaneous coronary intervention for coronary artery disease. J. Cardiol. 79, 559–563 (2022).
Mangili, L. C. et al. Achilles tendon xanthomas are associated with the presence and burden of subclinical coronary atherosclerosis in heterozygous familial hypercholesterolemia: a pilot study. Atherosclerosis 263, 393–397 (2017).
Tada, H. et al. Impact of clinical signs and genetic diagnosis of familial hypercholesterolaemia on the prevalence of coronary artery disease in patients with severe hypercholesterolaemia. Eur. Heart J. 38, 1573–1579 (2017).
Michikura, M. et al. Association between Achilles tendon softness and atherosclerotic cardiovascular disease in patients with familial hypercholesterolemia. J. Atheroscler. Thromb. 29, 1603–1612 (2022).
Miname, M. H. et al. Vascular age derived from coronary artery calcium score on the risk stratification of individuals with heterozygous familial hypercholesterolaemia. Eur. Heart J. Cardiovasc. Imaging 21, 251–257 (2020).
Miname, M. H. et al. Coronary artery calcium and cardiovascular events in patients with familial hypercholesterolemia receiving standard lipid-lowering therapy. JACC Cardiovasc. Imaging 12, 1797–1804 (2019).
Gallo, A. et al. The added value of coronary calcium score in predicting cardiovascular events in familial hypercholesterolemia. JACC Cardiovasc. Imaging 14, 2414–2424 (2021).
Miname, M. H. et al. Evaluation of subclinical atherosclerosis by computed tomography coronary angiography and its association with risk factors in familial hypercholesterolemia. Atherosclerosis 213, 486–491 (2010).
Pérez de Isla, L. et al. Coronary computed tomographic angiography findings and their therapeutic implications in asymptomatic patients with familial hypercholesterolemia. Lessons from the SAFEHEART study. J. Clin. Lipidol. 12, 948–957 (2018).
Pérez de Isla, L. et al. Coronary plaque burden, plaque characterization and their prognostic implications in familial hypercholesterolemia: a computed tomographic angiography study. Atherosclerosis 317, 52–58 (2021).
Fuchs, A. et al. Subclinical coronary atherosclerosis and risk for myocardial infarction in a Danish cohort: a prospective observational cohort study. Ann. Intern. Med. 176, 433–442 (2023).
Javaid, A. et al. Distribution of coronary artery calcium by age, sex, and race among patients 30–45 years old. J. Am. Coll. Cardiol. 79, 1873–1886 (2022).
Kusters, D. M., Wiegman, A., Kastelein, J. J. & Hutten, B. A. Carotid intima–media thickness in children with familial hypercholesterolemia. Circ. Res. 114, 307–310 (2014).
Stefanutti, C. et al. Toward an international consensus — integrating lipoprotein apheresis and new lipid-lowering drugs. J. Clin. Lipidol. 11, 858–871.e3 (2017).
Bélanger, A. M., Akioyamen, L. E., Ruel, I., Hales, L. & Genest, J. Aortic stenosis in homozygous familial hypercholesterolaemia: a paradigm shift over a century. Eur. Heart J. 43, 3227–3239 (2022).
Zhang, R. et al. Supravalvular aortic stenosis and the risk of premature death among patients with homozygous familial hypercholesterolemia. Am. J. Cardiol. 145, 58–63 (2021).
Zhang, Y. et al. Association between cumulative low-density lipoprotein cholesterol exposure during young adulthood and middle age and risk of cardiovascular events. JAMA Cardiol. 6, 1406–1413 (2021).
Masson, W. et al. Reduction of cardiovascular events with the use of lipid-lowering medication in patients with familial hypercholesterolemia or severe primary hypercholesterolemia: a systematic review. J. Clin. Lipidol. 16, 562–573 (2022).
Iyen, B., Akyea, R. K., Weng, S., Kai, J. & Qureshi, N. Statin treatment and LDL-cholesterol treatment goal attainment among individuals with familial hypercholesterolaemia in primary care. Open Heart 8, e001817 (2021).
Perez de Isla, L. et al. Attainment of LDL-cholesterol treatment goals in patients with familial hypercholesterolemia: 5-Year SAFEHEART registry follow-up. J. Am. Coll. Cardiol. 67, 1278–1285 (2016).
Schwarz, A. et al. Low-density lipoprotein cholesterol goal attainment in patients with clinical evidence of familial hypercholesterolemia and elevated Lp(a). Lipids Health Dis. 21, 114 (2022).
Chua, Y.-A. et al. Attainment of low-density lipoprotein cholesterol targets and prescribing pattern of lipid-lowering medications among patients with familial hypercholesterolemia attending specialist clinics. J. Atheroscler. Thromb. https://doi.org/10.5551/jat.63389 (2022).
Raal, F. J., Hovingh, G. K. & Catapano, A. L. Familial hypercholesterolemia treatments: guidelines and new therapies. Atherosclerosis 277, 483–492 (2018).
Brandts, J. & Ray, K. K. Familial hypercholesterolemia. J. Am. Coll. Cardiol. 78, 1831–1843 (2021).
Rosenson, R. S. Existing and emerging therapies for the treatment of familial hypercholesterolemia. J. Lipid Res. 62, 100060 (2021).
Ray, K. K. et al. Inclisiran and cardiovascular events: a patient-level analysis of phase III trials. Eur. Heart J. 44, 129–138 (2022).
Lloyd-Jones, D. M. et al. 2022 ACC Expert Consensus Decision Pathway on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 80, 1366–1418 (2022).
Wong, N. D., Bang, M., Block, R. C., Peterson, A. L. & Karalis, D. G. Perceptions and barriers on the use of proprotein subtilisin/kexin type 9 inhibitors in heterozygous familial hypercholesterolemia (from a Survey of Primary Care Physicians and Cardiologists). Am. J. Cardiol. 152, 57–62 (2021).
Langer, A. et al. Treatment inertia in patients with familial hypercholesterolemia. J. Am. Heart Assoc. 10, e020126 (2021).
Ballantyne, C. M. et al. Long-term safety and efficacy of bempedoic acid in patients with atherosclerotic cardiovascular disease and/or heterozygous familial hypercholesterolemia (from the CLEAR Harmony Open-label Extension Study). Am. J. Cardiol. 41, 1–11 (2022).
Newman, C. B. Safety of statins and nonstatins for treatment of dyslipidemia. Endocrinol. Metab. Clin. North Am. 51, 655–679 (2022).
Stroes, E. S. et al. Statin-associated muscle symptoms: impact on statin therapy — European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. Eur. Heart J. 36, 1012–1022 (2015).
Rosenson, R. S. et al. Optimizing cholesterol treatment in patients with muscle complaints. J. Am. Coll. Cardiol. 70, 1290–1301 (2017).
Mach, F. et al. Adverse effects of statin therapy: perception vs. the evidence — focus on glucose homeostasis, cognitive, renal and hepatic function, haemorrhagic stroke and cataract. Eur. Heart J. 39, 2526–2539 (2018).
Newman, C. B. et al. Statin safety and associated adverse events: a scientific statement from the American Heart Association. Arterioscler. Thromb. Vasc. Biol. 39, e38–e81 (2019).
Nissen, S. E. et al. Bempedoic acid and cardiovascular outcomes in statin-intolerant patients. N. Engl. J. Med. 388, 1353–1364 (2023).
Fahed, A. C. et al. Association of the interaction between familial hypercholesterolemia variants and adherence to a healthy lifestyle with risk of coronary artery disease. JAMA Netw. Open 5, e222687 (2022).
Stone, N. J. et al. Managing atherosclerotic cardiovascular risk in young adults: JACC state-of-the-art review. J. Am. Coll. Cardiol. 79, 819–836 (2022).
Bhatt, D. L. et al. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N. Engl. J. Med. 380, 11–22 (2019).
Orringer, C. E., Jacobson, T. A. & Maki, K. C. National Lipid Association Scientific Statement on the use of icosapent ethyl in statin-treated patients with elevated triglycerides and high or very-high ASCVD risk. J. Clin. Lipidol. 13, 860–872 (2019).
Budoff, M. J. et al. Effect of icosapent ethyl on progression of coronary atherosclerosis in patients with elevated triglycerides on statin therapy: final results of the EVAPORATE trial. Eur. Heart J. 41, 3925–3932 (2020).
Skulas-Ray, A. C. et al. Omega-3 fatty acids for the management of hypertriglyceridemia: a science advisory from the American Heart Association. Circulation 140, e673–e691 (2019).
Visseren, F. L. et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 42, 3227–3337 (2021).
Nidorf, S. M. et al. Colchicine in patients with chronic coronary disease. N. Engl. J. Med. 383, 1838–1847 (2020).
Tardif, J.-C. et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N. Engl. J. Med. 381, 2497–2505 (2019).
Vuorio, A. et al. Statins for children with familial hypercholesterolemia. Cochrane Database Syst. Rev. 11, CD006401 (2019).
Anagnostis, P. et al. Efficacy and safety of statin use in children and adolescents with familial hypercholesterolaemia: a systematic review and meta-analysis of randomized-controlled trials. Endocrine 69, 249–261 (2020).
Mamann, N. et al. Intermediate-term efficacy and tolerance of statins in children. J. Pediatr. 210, 161–165 (2019).
Benekos, T., Kosmeri, C., Vlahos, A. & Milionis, H. Nine-year overview of dyslipidemia management in children with heterozygous familial hypercholesterolemia: a university hospital outpatient lipid clinic project in Northwestern Greece. J. Pediatr. Endocrinol. Metab. 33, 533–538 (2020).
Desai, N. K. et al. Hepatotoxicity of statins as determined by serum alanine aminotransferase in a pediatric cohort with dyslipidemia. J. Pediatr. Gastroenterol. Nutr. 68, 175 (2019).
Johnson, P. K. et al. Statin-associated myopathy in a pediatric preventive cardiology practice. J. Pediatr. 185, 94–98.e1 (2017).
Joyce, N. R., Zachariah, J. P., Eaton, C. B., Trivedi, A. N. & Wellenius, G. A. Statin use and the risk of type 2 diabetes mellitus in children and adolescents. Acad. Pediatr. 17, 515–522 (2017).
Kavey, R.-E. W. et al. Effectiveness and safety of statin therapy in children: a real-world clinical practice experience. CJC Open 2, 473–482 (2020).
Stein, E. A. et al. Colesevelam hydrochloride: efficacy and safety in pediatric subjects with heterozygous familial hypercholesterolemia. J. Pediatr. 156, 231–236.e1–3 (2010).
Kusters, D. M. et al. Efficacy and safety of ezetimibe monotherapy in children with heterozygous familial or nonfamilial hypercholesterolemia. J. Pediatr. 166, 1377–1384.e1–3 (2015).
Santos, R. D. et al. Evolocumab in pediatric heterozygous familial hypercholesterolemia. N. Engl. J. Med. 383, 1317–1327 (2020).
Daniels, S. et al. PCSK9 inhibition with alirocumab in pediatric patients with heterozygous familial hypercholesterolemia: the ODYSSEY KIDS study. J. Clin. Lipidol. 14, 322–330.e5 (2020).
Santos, R. D. et al. Paediatric patients with heterozygous familial hypercholesterolaemia treated with evolocumab for 80 weeks (HAUSER-OLE): a single-arm, multicentre, open-label extension of HAUSER-RCT. Lancet Diabetes Endocrinol. 10, 732–740 (2022).
Roy, G., Boucher, A., Couture, P. & Drouin-Chartier, J.-P. Impact of diet on plasma lipids in individuals with heterozygous familial hypercholesterolemia: a systematic review of randomized controlled nutritional studies. Nutrients 13, 235 (2021).
Kris-Etherton, P. M. et al. Strategies for promotion of a healthy lifestyle in clinical settings: pillars of ideal cardiovascular health: a science advisory from the American Heart Association. Circulation 144, e495–e514 (2021).
Langslet, G. et al. Thirty percent of children and young adults with familial hypercholesterolemia treated with statins have adherence issues. Am. J. Prev. Cardiol. 6, 100180 (2021).
Hokanson, J. S. et al. Preventive medicine in pediatric cardiology practice. J. Pediatr. 253, 14–17.e3 (2022).
Kinnear, F. J. et al. Enablers and barriers to treatment adherence in heterozygous familial hypercholesterolaemia: a qualitative evidence synthesis. BMJ Open 9, e030290 (2019).
Svendsen, K. et al. Genetic testing is essential for initiating statin therapy in children with familial hypercholesterolemia: examples from Scandinavia. Atherosclerosis 316, 48–52 (2021).
Mackie, T. I., Tse, L. L., de Ferranti, S. D., Ryan, H. R. & Leslie, L. K. Treatment decision making for adolescents with familial hypercholesterolemia: role of family history and past experiences. J. Clin. Lipidol. 9, 583–593.e1–3 (2015).
Alothman, L. et al. Health-related quality of life in homozygous familial hypercholesterolemia: a systematic review and meta-analysis. J. Clin. Lipidol. 16, 52–65 (2022).
Tunçel, Ö. K. et al. Mental status and physical activity in patients with homozygous familial hypercholesterolemia: a subgroup analysis of a nationwide survey (A-HIT1 registry). J. Clin. Lipidol. 14, 361–370. e2 (2020).
Nordestgaard, B. et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease (Consensus Statement of the European Atherosclerosis Society). Eur. Heart J. 34, 3478–3490 (2013).
Cuchel, M. et al. Homozygous familial hypercholesterolaemia: new insights and guidance for clinicians to improve detection and clinical management. A position paper from the consensus panel on familial hypercholesterolaemia of the European Atherosclerosis Society. Eur. Heart J. 35, 2146–2157 (2014).
Stefanutti, C. et al. A cross-national investigation of cardiovascular survival in homozygous familial hypercholesterolemia: the Sino-Roman Study. J. Clin. Lipidol. 13, 608–617 (2019).
Thompson, G. R. et al. Survival in homozygous familial hypercholesterolaemia is determined by the on-treatment level of serum cholesterol. Eur. Heart J. 39, 1162–1168 (2018).
Kramer, A. I. et al. Major adverse cardiovascular events in homozygous familial hypercholesterolaemia: a systematic review and meta-analysis. Eur. J. Prev. Cardiol. 29, 817–828 (2021).
Nurmohamed, N. S., Navar, A. M. & Kastelein, J. J. P. New and emerging therapies for reduction of LDL-cholesterol and apolipoprotein B. J. Am. Coll. Cardiol. 77, 1564–1575 (2021).
Ray, K. K. et al. Combination lipid-lowering therapy as first-line strategy in very high-risk patients. Eur. Heart J. 43, 830–833 (2021).
Raal, F. J. et al. Inhibition of PCSK9 with evolocumab in homozygous familial hypercholesterolaemia (TESLA Part B): a randomised, double-blind, placebo-controlled trial. Lancet 385, 341–350 (2015).
Bansal, S. et al. Evolocumab in patients with homozygous familial hypercholesterolemia in India. J. Clin. Lipidol. 15, 814–821 (2021).
Santos, R. D. et al. Long-term evolocumab in patients with familial hypercholesterolemia. J. Am. Coll. Cardiol. 75, 565–574 (2020).
Bruckert, E. et al. Efficacy and safety of alirocumab in children and adolescents with homozygous familial hypercholesterolemia: phase 3, multinational open-label study. Arterioscler. Thromb. Vasc. Biol. 42, 1447–1457 (2022).
Harada-Shiba, M. et al. Guidelines for the diagnosis and treatment of pediatric familial hypercholesterolemia 2022. J. Atheroscler. Thromb. https://doi.org/10.5551/jat.CR006 (2023).
Sunil, B., Foster, C., Wilson, D. P. & Ashraf, A. P. Novel therapeutic targets and agents for pediatric dyslipidemia. Ther. Adv. Endocrinol. Metab. 12, 20420188211058323 (2021).
Raal, F. J. et al. Evinacumab for homozygous familial hypercholesterolemia. N. Engl. J. Med. 383, 711–720 (2020).
Blom, D. J. et al. Long-term efficacy and safety of the microsomal triglyceride transfer protein inhibitor lomitapide in patients with homozygous familial hypercholesterolemia. Circulation 136, 332–335 (2017).
Reeskamp, L. F. et al. Marked plaque regression in homozygous familial hypercholesterolemia. Atherosclerosis 327, 13–17 (2021).
Stefanutti, C. & Thompson, G. R. Lipoprotein apheresis in the management of familial hypercholesterolaemia: historical perspective and recent advances. Curr. Atheroscler. Rep. 17, 465 (2015).
Palcoux, J.-B. et al. Low-density lipoprotein apheresis in children with familial hypercholesterolemia: follow-up to 21 years. Ther. Apher. Dial. 12, 195–201 (2008).
Hudgins, L. C., Kleinman, B., Scheuer, A., White, S. & Gordon, B. R. Long-term safety and efficacy of low-density lipoprotein apheresis in childhood for homozygous familial hypercholesterolemia. Am. J. Cardiol. 102, 1199–1204 (2008).
Græsdal, A. et al. Apheresis in homozygous familial hypercholesterolemia: the results of a follow-up of all Norwegian patients with homozygous familial hypercholesterolemia. J. Clin. Lipidol. 6, 331–339 (2012).
Bajaj, A. & Cuchel, M. Advancements in the treatment of homozygous familial hypercholesterolemia. J. Atheroscler. Thromb. 29, 1125–1135 (2022).
Luirink, I. K. et al. Efficacy and safety of lipoprotein apheresis in children with homozygous familial hypercholesterolemia: a systematic review. J. Clin. Lipidol. 13, 31–39 (2019).
Kawashiri, M.-a et al. Impact of evolocumab treatment on low-density lipoprotein cholesterol levels in heterozygous familial hypercholesterolemic patients withdrawing from regular apheresis. Atherosclerosis 265, 225–230 (2017).
Chadwick, A. C., Evitt, N. H., Lv, W. & Musunuru, K. Reduced blood lipid levels with in vivo CRISPR-Cas9 base editing of ANGPTL3. Circulation 137, 975–977 (2018).
Musunuru, K. et al. In vivo CRISPR base editing of PCSK9 durably lowers cholesterol in primates. Nature 593, 429–434 (2021).
Al Dubayee, M., Kayikcioglu, M., van Lennep, J. R., Hergli, N. & Mata, P. Is liver transplant curative in homozygous familial hypercholesterolemia? A review of nine global cases. Adv. Ther. 39, 3042–3057 (2022).
Kazimi, M. et al. Concurrent living donor liver transplantation and off-pump coronary artery bypass in a five-year-old child with homozygous familial hypercholesterolemia: a case report. Transplant. Proc. https://doi.org/10.1016/j.transproceed.2023.02.024 (2023).
El-Rassi, I., Chehab, G., Saliba, Z., Alawe, A. & Jebara, V. Fatal cardiac atherosclerosis in a child 10 years after liver transplantation: a case report and a review. J. Clin. Lipidol. 5, 329–332 (2011).
Ishigaki, Y. et al. Liver transplantation for homozygous familial hypercholesterolemia. J. Atheroscler. Thromb. 26, 121–127 (2019).
Martinez, M. et al. Effects of liver transplantation on lipids and cardiovascular disease in children with homozygous familial hypercholesterolemia. Am. J. Cardiol. 118, 504–510 (2016).
Cephus, C. E., Qureshi, A. M., Tejtel, S. K. S., Alam, M. & Moodie, D. S. Coronary artery disease in a child with homozygous familial hypercholesterolemia: regression after liver transplantation. J. Clin. Lipidol. 13, 880–886 (2019).
Mlinaric, M. et al. Case report: liver transplantation in homozygous familial hypercholesterolemia (HoFH) — long-term follow-up of a patient and literature review. Front. Pediatr. 8, 567895 (2020).
Ibrahim, M., El-Hamamsy, I., Barbir, M. & Yacoub, M. H. Translational lessons from a case of combined heart and liver transplantation for familial hypercholesterolemia 20 years post-operatively. J. Cardiovasc. Transl. Res. 5, 351–358 (2012).
Squires, J. E. et al. Factors associated with improved patient and graft survival beyond 1 year in pediatric liver transplantation. Liver Transpl. 28, 1899–1910 (2022).
Cohen, H. & Stefanutti, C. Current approach to the diagnosis and treatment of heterozygote and homozygous FH children and adolescents. Curr. Atheroscler. Rep. 23, 30 (2021).
Perez de Isla, L. et al. Alicrocumab and coronary atherosclerosis in asymptomatic patients with familial hypercholesterolaemia: the ARCHITECT study. Circulation https://doi.org/10.1161/CIRCULATIONAHA.122.062557 (2023).
Sepucha, K. R. & Scholl, I. Measuring shared decision making: a review of constructs, measures, and opportunities for cardiovascular care. Circ. Cardiovasc. Qual. Outcomes 7, 620–626 (2014).
Barrett, B., Ricco, J., Wallace, M., Kiefer, D. & Rakel, D. Communicating statin evidence to support shared decision-making. BMC Fam. Pract. 17, 41 (2016).
Spatz, E. S. & Spertus, J. A. Shared decision making: a path toward improved patient-centered outcomes. Circ. Cardiovasc. Qual. Outcomes 5, e75–e77 (2012).
Birtcher, K. K. et al. 2022 ACC expert consensus decision pathway for integrating atherosclerotic cardiovascular disease and multimorbidity treatment: a framework for pragmatic, patient-centered care. J. Am. Coll. Cardiol. 81, 292–317 (2023).
Graham, D. F. & Raal, F. J. Management of familial hypercholesterolemia in pregnancy. Curr. Opin. Lipidol. 32, 370–377 (2021).
Amundsen, Å. L. et al. Marked changes in plasma lipids and lipoproteins during pregnancy in women with familial hypercholesterolemia. Atherosclerosis 189, 451–457 (2006).
Nangrahary, M., Graham, D. F., Pang, J., Barnett, W. & Watts, G. F. Familial hypercholesterolaemia in pregnancy: Australian case series and review. Aust. N. Z. J. Obstet. Gynaecol. https://doi.org/10.1111/ajo.13657 (2023).
Johansen, A. K. et al. Young women with familial hypercholesterolemia have higher LDL-cholesterol burden than men: novel data using repeated measurements during 12-years follow-up. Atheroscler 51, 28–34 (2023).
Cacciatore, F. et al. Maternal hypercholesterolaemia during pregnancy affects severity of myocardial infarction in young adults. Eur. J. Prev. Cardiol. 29, 758–765 (2022).
Balla, S., Ekpo, E. P., Wilemon, K. A., Knowles, J. W. & Rodriguez, F. Women living with familial hypercholesterolemia: challenges and considerations surrounding their care. Curr. Atheroscler. Rep. 22, 60 (2020).
Thorogood, M., Seed, M. & De Mott, K., Guideline Development Group. Management of fertility in women with familial hypercholesterolaemia: summary of NICE guidance. Br. J. Obstet. Gynaecol. 116, 478–479 (2009).
Regitz-Zagrosek, V. et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur. Heart J. 39, 3165–3241 (2018).
Lawesson, S. S. et al. Association between history of adverse pregnancy outcomes and coronary artery disease assessed by coronary computed tomography angiography. J. Am. Med. Assoc. 329, 393–404 (2023).
Agarwala, A., Michos, E. D., Samad, Z., Ballantyne, C. M. & Virani, S. S. The use of sex-specific factors in the Assessment of Women’s Cardiovascular Risk. Circulation 141, 592–599 (2020).
Lewek, J. & Banach, M. Dyslipidemia management in pregnancy: why is it not covered in the guidelines? Curr. Atheroscler. Rep. 24, 547–556 (2022).
Pieper, P. G. Use of medication for cardiovascular disease during pregnancy. Nat. Rev. Cardiol. 12, 718 (2015).
Blaha, M., Lanska, M., Blaha, V., Boudys, L. & Zak, P. Pregnancy in homozygous familial hypercholesterolemia — importance of LDL-apheresis. Atheroscler. Suppl. 18, 134–139 (2015).
Ogura, M. et al. Lipoprotein apheresis is essential for managing pregnancies in patients with homozygous familial hypercholesterolemia: seven case series and discussion. Atherosclerosis 254, 179–183 (2016).
Kusters, D. M. et al. Statin use during pregnancy: a systematic review and meta-analysis. Expert. Rev. Cardiovasc. Ther. 10, 363–378 (2012).
Zarek, J., Delano, K. E., Nickel, C., Laskin, C. A. & Koren, G. Are statins teratogenic in humans? Addressing the safety of statins in light of potential benefits during pregnancy. Exp. Rev. Obstet. Gynecol. 8, 513–524 (2013).
Winterfeld, U. et al. Pregnancy outcome following maternal exposure to statins: a multicentre prospective study. Br. J. Obstet. Gynaecol. 120, 463–471 (2013).
Karalis, D. G., Hill, A. N., Clifton, S. & Wild, R. A. The risks of statin use in pregnancy: a systematic review. J. Clin. Lipidol. 10, 1081–1090 (2016).
Vahedian-Azimi, A. et al. A systematic review and meta-analysis on the effects of statins on pregnancy outcomes. Atherosclerosis 336, 1–11 (2021).
Botha, T. C., Pilcher, G. J., Wolmarans, K., Blom, D. J. & Raal, F. J. Statins and other lipid-lowering therapy and pregnancy outcomes in homozygous familial hypercholesterolaemia: a retrospective review of 39 pregnancies. Atherosclerosis 277, 502–507 (2018).
Thobani, A., Hassen, L., Mehta, L. S. & Agarwala, A. Management of hypercholesterolemia in pregnant women with atherosclerotic cardiovascular disease. Curr. Atheroscler. Rep. 23, 58 (2021).
Toleikyte, I., Retterstøl, K., Leren, T. P. & Iversen, P. O. Pregnancy outcomes in familial hypercholesterolemia — a registry-based study. Circulation 124, 1606–1614 (2011).
Chang, J.-C. et al. Perinatal outcomes after statin exposure during pregnancy. JAMA Netw. Open 4, e2141321 (2021).
Poornima, I. G., Pulipati, V. P., Brinton, E. A. & Wild, R. A. Update on statin use in pregnancy. Am. J. Med. 136, 12–14 (2022).
Mauricio, R. & Khera, A. Statin use in pregnancy: is it time for a paradigm shift? Circulation 145, 496–498 (2022).
Lundberg, G. P. et al. Heart centers for women: historical perspective on formation and future strategies to reduce cardiovascular disease. Circulation 138, 1155–1165 (2018).
Geraghty, L. et al. Cardiovascular disease in women: from pathophysiology to novel and emerging risk factors. Heart Lung Circ. 30, 9–17 (2021).
Baum, S. J. et al. Effect of evolocumab on lipoprotein apheresis requirement and lipid levels: results of the randomized, controlled, open-label DE LAVAL study. J. Clin. Lipidol. 13, 901–909 (2019).
Cuchel, M. et al. Efficacy and safety of a microsomal triglyceride transfer protein inhibitor in patients with homozygous familial hypercholesterolaemia: a single-arm, open-label, phase 3 study. Lancet 381, 40–46 (2013).
D’Erasmo, L. et al. Efficacy and safety of lomitapide in homozygous familial hypercholesterolaemia: the pan-European retrospective observational study. Eur. J. Prev. Cardiol. 29, 832–841 (2022).
Thompson, G. R. The scientific basis and future of lipoprotein apheresis. Ther. Apher. Dial. 26, 32–36 (2022).
Thompson, G. R. et al. Improved cardiovascular outcomes following temporal advances in lipid-lowering therapy in a genetically-characterised cohort of familial hypercholesterolaemia homozygotes. Atherosclerosis 243, 328–333 (2015).
Kayikcioglu, M. et al. Clinical management, psychosocial characteristics, and quality of life in patients with homozygous familial hypercholesterolemia undergoing LDL-apheresis in Turkey: results of a nationwide survey (A-HIT1 registry). J. Clin. Lipidol. 13, 455–467 (2019).
Watts, G. F. et al. Familial hypercholesterolaemia: a model of care for Australasia. Atheroscler. Suppl. 12, 221–263 (2011).
Padmanabhan, A. et al. Guidelines on the use of therapeutic apheresis in clinical practice — evidence‐based approach from the writing committee of the American Society for Apheresis: the eighth special issue. J. Clin. Apher. 34, 171–354 (2019).
McIntosh, S. et al. Patient voice and health education for familial hypercholesterolaemia. Health Educ. J. 8, 123–133 (2022).
Bulsara, C. et al. Awareness of familial hypercholesterolaemia in Australian primary care: a qualitative descriptive study. Aust. J. Gen. Pract. 50, 634–640 (2021).
Bean, L. J. et al. DNA-based screening and personal health: a points to consider statement for individuals and health-care providers from the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 23, 979–988 (2021).
Jones, L. K., Sturm, A. C. & Gionfriddo, M. R. Translating guidelines into practice via implementation science: an update in lipidology. Curr. Opin. Lipidol. 33, 336–341 (2022).
Bauer, M. S., Damschroder, L., Hagedorn, H., Smith, J. & Kilbourne, A. M. An introduction to implementation science for the non-specialist. BMC Psychol. 3, 32 (2015).
Sarkies, M. et al. Avoiding unnecessary hospitalisation for patients with chronic conditions: a systematic review of implementation determinants for hospital avoidance programmes. Implement. Sci. 15, 91 (2020).
Andermann, A., Blancquaert, I., Beauchamp, S. & Costea, I. Guiding policy decisions for genetic screening: developing a systematic and transparent approach. Public Health Genom. 14, 9–16 (2011).
Jones, L. K. et al. Developing implementation strategies to improve uptake of guideline-recommended treatments for individuals with familial hypercholesterolemia: a protocol. Res. Soc. Adm. Pharm. 16, 390–395 (2019).
Bangash, H. et al. An implementation science framework to develop a clinical decision support tool for familial hypercholesterolemia. J. Pers. Med. 10, 67 (2020).
Lindell, O. P. et al. Clinical decision support for familial hypercholesterolemia (CDS-FH): rationale and design of a cluster randomized trial in primary care. Am. Heart J. 247, 132–148 (2022).
Jones, L. K. et al. Implementation strategies to improve statin utilization in individuals with hypercholesterolemia: a systematic review and meta-analysis. Implement. Sci. 16, 40 (2021).
Proctor, E. K. et al. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm. Policy Ment. Health 36, 24–34 (2009).
Michie, S., Van Stralen, M. M. & West, R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 6, 42 (2011).
Martin, A. C., Gidding, S. S., Wiegman, A. & Watts, G. F. Known and unknowns in the care of paediatric familial hypercholesterolaemia. J. Lipid Res. 58, 1765–1776 (2017).
National Audit Office. Introducing Integrated Care Systems: joining up local services to improve health outcomes. NAO https://www.nao.org.uk/reports/introducing-integrated-care-systems-joining-up-local-services-to-improve-health-outcomes (2022).
Desai, N. R., Farbaniec, M. & Karalis, D. G. Nonadherence to lipid‐lowering therapy and strategies to improve adherence in patients with atherosclerotic cardiovascular disease. Clin. Cardiol. 46, 13–21 (2022).
Acknowledgements
The authors are grateful to J. Stock for editorial assistance with the manuscript before submission. J.P. has received grants from the National Health and Medical Research Council (Australia), the Medical Research Future Fund (Australia), the Department of Health of Western Australia and the Royal Perth Hospital Research Foundation.
Author information
Authors and Affiliations
Contributions
G.F.W., S.S.G., R.A.H., F.J.R., A.C.S., L.K.J., M.N.S., J.P. and G.R.T. researched data for the article. All the authors contributed to discussion of content. G.F.W., S.S.G., R.A.H., F.J.R., A.C.S. and G.R.T. wrote the manuscript. All the authors reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors have received no financial support for the research, authorship and/or publication of this article. The pharmaceutical industry was not involved and did not contribute financially to the development of this guidance. G.F.W. has received honoraria related to consulting, research and/or speaker activities from Amgen, Arrowhead, AstraZeneca, CRISPR Therapeutics, Esperion, Novartis and Sanofi. S.S.G. is a consultant for Esperion and is on a scientific advisory panel for Silence Therapeutics. R.A.H. has received honoraria related to consulting, research and/or speaker activities from Acasti, Akcea-Ionis, Amgen, Arrowhead, HLS Therapeutics, Pfizer, Novartis and Sanofi/Regeneron. F.J.R. has received personal fees from Amgen, LIB Therapeutics, Novartis, Regeneron and Sanofi-Aventis. A.C.S. is an employee and stockholder of 23andMe, an adviser to Nest Genomics and a consultant on the NHLBI IMPACT-FH grant. L.K.J. is a consultant for Novartis. M.N.S. has received personal fees from Amgen. K.A.-R. has received grants and personal fees from Sanofi and personal fees from Abbott and Novartis. D.J.B. has received grants for clinical trials and/or personal fees from Abbott, Akcea, Amgen, Amryt, AstraZeneca, Ionis, LIB Therapeutics, Novartis, Sanofi and Silence Therapeutics. S.D.d.F. has received personal fees from UpToDate. P.L. has received research funding from Novartis; is on the Board of Directors of XBiotech; has a financial interest in Soley Therapeutics, TenSixteen Bio and XBiotech; is an unpaid consultant to, or involved in clinical trials for, Amgen, AstraZeneca, Baim Institute, Beren Therapeutics, Esperion Therapeutics, Genentech, Kancera, Kowa Pharmaceuticals, Medimmune, Merck, Norvo Nordisk, Novartis, Pfizer and Sanofi-Regeneron; is a member of the scientific advisory board for Amgen, Caristo Diagnostics, Cartesian Therapeutics, CSL Behring, DalCor Pharmaceuticals, Dewpoint Therapeutics, Eulicid Bioimaging, Kancera, Kowa Pharmaceuticals, Medimmune, Moderna, Novartis, Olatec Therapeutics, PlaqueTec, Soley Therapeutics, TenSixteen Bio and XBiotech. P.M. has received grants from Amgen and Sanofi. K.K.R. has received grants from Amgen, Daiichi Sankyo, Regeneron and Sanofi; personal fees for serving on steering committees, executive committees or advisory boards from Abbott, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Cargene, CRISPR Therapeutics, CSL Behring, Daiichi Sankyo, Eli Lilly, Esperion, Kowa, New Amsterdam Pharma, Novartis, Novo Nordisk, Sanofi, Scribe, Silence Therapeutics and Vaxxinity; personal fees for CME and non-CME lectures from Amgen, AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, Sanofi and Viatris. C.S. has consulted and received research grants from Aegerion, Amgen, B. Braun Avitum, Cerenis Therapeutics, Difass, Fresenius Medical Care, Isis (Ionis) Pharmaceuticals, Kaneka NV, Kowa Company, Merck Sharp & Dohme, Regeneron-Sanofi and Ultragenyx. S.Y. has received personal fees from Amgen, Kowa Company, Merck Sharp & Dohme, Novartis and Otsuka Pharmaceutical Company. R.D.S. has received honoraria related to consulting, research and/or speaker activities from Abbott, Ache, Amgen, AstraZeneca, EMS, Esperion, GETZ Pharma, Kowa, Libbs, Novartis, Novo-Nordisk, Merck, Merck Sharp & Dohme, Pfizer, PTC Therapeutics and Sanofi/Regeneron. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Rodrigo Alonso, Maria Cristina de Oliveira Izar and Atsushi Nohara for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Watts, G.F., Gidding, S.S., Hegele, R.A. et al. International Atherosclerosis Society guidance for implementing best practice in the care of familial hypercholesterolaemia. Nat Rev Cardiol 20, 845–869 (2023). https://doi.org/10.1038/s41569-023-00892-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-023-00892-0
This article is cited by
-
Prevalence, clinical features and prognosis of familial hypercholesterolemia in Chinese Han patients with acute coronary syndrome after a coronary event: a retrospective observational study
BMC Cardiovascular Disorders (2024)
-
Cost-Effectiveness of Screening Strategies for Familial Hypercholesterolaemia: An Updated Systematic Review
PharmacoEconomics (2024)
-
Unexpected gaps in knowledge of familial hypercholesterolaemia among Dutch general practitioners
Netherlands Heart Journal (2024)
-
Whether and Why Do We Need a Vaccine Against Atherosclerosis? Can We Expect It Anytime Soon?
Current Atherosclerosis Reports (2024)
-
Familiäre Hypercholesterinämie
CardioVasc (2023)