Abstract
Streptococcus agalactiae (Group B Streptococcus; GBS) is a common cause of sepsis in neonates. Previous work detected GBS DNA in the placenta in ~5% of women before the onset of labour, but the clinical significance of this finding is unknown. Here we re-analysed this dataset as a case control study of neonatal unit (NNU) admission. Of 436 infants born at term (≥37 weeks of gestation), 7/30 with placental GBS and 34/406 without placental GBS were admitted to the NNU (odds ratio (OR) 3.3, 95% confidence interval (CI) 1.3–7.8). We then performed a validation study using non-overlapping subjects from the same cohort. This included a further 239 cases of term NNU admission and 686 term controls: 16/36 with placental GBS and 223/889 without GBS were admitted to the NNU (OR 2.4, 95% CI 1.2–4.6). Of the 36 infants with placental GBS, 10 were admitted to the NNU with evidence of probable but culture-negative sepsis (OR 4.8, 95% CI 2.2–10.3), 2 were admitted with proven GBS sepsis (OR 66.6, 95% CI 7.3–963.7), 6 were admitted and had chorioamnionitis (inflammation of the foetal membranes) (OR 5.3, 95% CI 2.0–13.4), and 5 were admitted and had funisitis (inflammation of the umbilical cord) (OR 6.7, 95% CI 12.5–17.7). Foetal cytokine storm (two or more pro-inflammatory cytokines >10 times median control levels in umbilical cord blood) was present in 36% of infants with placental GBS DNA and 4% of cases where the placenta was negative (OR 14.2, 95% CI 3.6–60.8). Overall, ~1 in 200 term births had GBS detected in the placenta, which was associated with infant NNU admission and morbidity.
Similar content being viewed by others
Main
Streptococcus agalactiae (Group B Streptococcus; GBS) is the most common cause of sepsis in the first week of life1, and this is referred to as early-onset disease (EOD). GBS is present in the genital tract in about 20% of women, and, in the absence of intervention, about 1% of infants born to a colonized mother develop EOD2,3. An analysis of the global burden of disease in 2020 estimated that about 20 million pregnant women were colonized with GBS, 230,000 infants exhibited EOD and GBS accounted for around 50,000 stillbirths and 50,000–100,000 infant deaths4. However, EOD remains uncommon, affecting less than 1 in 1,000 births in high income countries. The incidence is higher in low- and middle-income settings, but reliable estimates are problematic due to incomplete ascertainment. We previously used metagenomic methods to determine whether bacterial DNA was present in the placenta at term and found that the only verifiable bacterial signal before membrane rupture and the onset of labour at term was GBS5. In this Article, we employed data and biological samples from a prospective cohort of >4,000 nulliparous women to determine whether the presence of GBS DNA in the placenta was associated with the risk of neonatal morbidity.
Results
Placental GBS and the risk of neonatal morbidity
We analysed data from our previously reported dataset in which GBS had been quantified in the placenta from 537 pregnancies5. In this discovery dataset the presence of GBS DNA was defined using either deep sequencing or PCR of the bacterial 16S ribosomal RNA gene followed by amplicon sequencing, as previously described5. In the new analysis of this study, we defined cases as admission of the infant to the neonatal unit (NNU) within 48 h of birth and for 48 h or more, as previously employed6. Given the high rates of NNU admission of preterm infants, we confined the analysis to 436 births at term (41 cases and 395 controls) (Extended Data Fig. 1 and Supplementary Table 1). Controls were defined as any term birth that did not fulfil the case criteria. Of the 436 infants born at term, 7/30 (23.3%) with placental GBS DNA and 34/406 (8.4%) without placental GBS DNA were cases (odds ratio (OR) 3.3, 95% confidence interval (CI) 1.3–7.8, P = 0.007). The association was similar following adjustment for maternal characteristics (adjusted OR 3.1, 95% CI 1.2–8.0, P = 0.02).
To validate this finding we performed a case control study using non-overlapping subjects drawn from the same cohort. Cases were defined as pregnancies where the infant was admitted to the NNU without time limits for admission or duration of stay. Controls were infants who were not admitted to the NNU. We excluded preterm births and cases and controls that had already been included in the discovery study described above, leaving 239 cases and 686 controls (Extended Data Fig. 1 and Supplementary Table 2). A power calculation indicated that we had >99% power to replicate the original finding with this sample size. We determined placental GBS DNA status using an ultrasensitive polymerase chain reaction (PCR)–quantitative PCR (qPCR) assay targeted at a GBS-specific region of the 16S rRNA gene (Extended Data Figs. 2 and 3). Consistent with the results of the discovery study, 16/36 infants with placental GBS and 223/889 without GBS were admitted to the NNU (OR 2.4, 95% CI 1.2–4.6), and the association was similar following adjustment for maternal characteristics (Table 1).
Septic and non-septic phenotypes of neonatal morbidity
We hypothesized that the risk of neonatal unit admission was causally explained by the presence of GBS in the placenta. This hypothesis predicts that the association would be progressively stronger as the evidence for neonatal sepsis and inflammation was stronger. Hence, we next performed secondary analyses of the validation case control study in relation to associated evidence for sepsis. First, we classified cases of NNU admission by clinical evidence, with classification performed blind to placental GBS DNA status. The infant’s clinical record was reviewed and admissions were classified on an ordinal scale: no evidence of sepsis, possible sepsis, probable but culture-negative sepsis or proven GBS sepsis, with proven sepsis being defined on the basis of a positive postnatal culture result from a septic screen (Supplementary Table 3). Analysis of the 16 NNU admissions with placental GBS demonstrated that there was no association between placental GBS and the risk of NNU admission with no evidence of sepsis or only possible evidence (Table 1). However, there were strong associations with NNU admission with probable but culture-negative sepsis (OR 4.8, 95% CI 2.2–10.3) and proven GBS sepsis (OR 66.6, 95% CI 7.3–963.7).
We next classified admissions on the basis of histopathological examination of the foetal membranes and a cross section of the umbilical cord (Fig. 1), again assessed blind to placental GBS DNA status. Inflammation was defined on the basis of a previously described ordinal scale (stage 0, 1, 2 or 3) for chorioamnionitis and funisitis, respectively, and in both cases samples with stage 2 or 3 findings were defined as positive7. There was no association between placental GBS and the risk of NNU admission without evidence of chorioamnionitis or funisitis (Table 1). However, there were strong associations between GBS DNA in the placenta and NNU admission with chorioamnionitis (OR 5.3, 95% CI 2.0–13.4) and funisitis (OR 6.7, 95% CI 12.5–17.7). All associations were similar following adjustment for maternal characteristics (Table 1).
a–j, Representative H&E-stained sections of umbilical cords and foetal membranes were scanned using the Zeiss Axio Scan. Histopathological examination included n = 314 umbilical cord and n = 312 foetal membrane sections. a, Low power magnification of a healthy cord. b, Medium power magnification of a healthy umbilical artery. c, High power magnification of a healthy umbilical vein. d, Low power magnification of funisitis. e, Medium power magnification of an umbilical artery in funisitis (black arrows indicate extensive infiltration of neutrophils). f, High power magnification of an umbilical vein in funisitis (black arrows indicate neutrophils infiltrating between layers of smooth muscle and yellow arrow indicates microabscess). g, Low power magnification of a healthy membrane roll. h, Medium power magnification of a healthy membrane roll. i, Low power magnification of chorioamnionitis. j, Medium power magnification of chorioamnionitis (black arrows indicate extensive infiltration of neutrophils).
Rates of placental GBS by genital tract colonization
Of the 925 participants in the second case control study, 467 (50%) had a report of a high vaginal swab (HVS) during the pregnancy. GBS DNA was detected in the placenta in 7/57 (12%) of participants with a positive HVS culture for GBS and 8/410 (2%) of those with a negative HVS culture for GBS. Of those who had no HVS culture performed during the pregnancy, 21/458 (5%) had placental GBS DNA detected. There was an excess of GBS-positive placentas in the first group when compared with the second and third (P < 0.0001 and 0.02, respectively; Fig. 2a).
a, Proportion of pregnancies with GBS-positive placentas in relation to maternal genital tract colonization assessed by high vaginal swab (HVS), corresponding to 7/57 patients with positive HVS culture, 8/410 patients with negative HVS culture and 21/458 patients with no HVS culture performed. Data are presented as percentage with 95% CI. Two-sided chi-squared test P values are reported. b, Cytokines were measured in cord serum samples from term pregnancies with GBS-positive (n = 11) and negative (n = 129) placentas, using the Ella platform (Bio-Techne). Cytokine levels are expressed as the MoM of control samples analysed in the same batch. For graphical purposes, samples with MoM of 0 for IL-1β (n = 24) have been plotted using a value of MoM of 0.0126 (the lowest MoM in the dataset). The dotted line represents an elevation of MoM >10. Median cytokine levels in the controls were: 0.18 pg ml−1 for IL-1β (n = 116), 16.6 pg ml−1 for IL-6 (n = 140), 13.6 pg ml−1 for IL-8 (n = 140) and 16.6 pg ml−1 for TNF-α (n = 140). c, Proportion of pregnancies with foetal cytokine storm in relation to GBS detection in the placenta, corresponding to 4/11 GBS positives and 5/129 GBS negatives. Data are presented as percentage with 95% CI. Two-sided chi-squared test P value is reported. d, Cytokines were measured as described above in 58 term placental samples from term pregnancies with GBS-positive (n = 26) and negative (n = 32) placentas. For graphical purposes, samples with MoM of 0 for IL-1β (n = 1) and TNF-α (n = 9) have been plotted using a value of MoM of 0.256 and MoM of 0.493, respectively (the lowest MoM in the dataset). e, Cytokines were measured as described above in 55 maternal serum samples at 36-week gestation from term pregnancies with GBS-positive (n = 25) and negative (n = 30) placentas. Samples with MoM of 0 for IL-1β (n = 49) have been plotted using a value of MoM of 0.914 (the lowest MoM in the dataset).
Validating the GBS DNA signal
We tested the possibility that GBS DNA was detected in the placenta due to contamination. The design and results of the no-template controls from the discovery case control study are reported in our previous paper5. In relation to the validation case control study, there was no temporal relationship between the presence of GBS DNA in the placenta and the week of delivery and there were no clusters of positive cases (Extended Data Fig. 4 and Supplementary Table 4). We compared the proportion of infants delivered by caesarean section, where the placenta is delivered abdominally precluding contamination during vaginal birth. A greater proportion of participants with a GBS DNA-positive placenta were delivered by caesarean section compared with those who were GBS DNA negative (47% versus 28%, respectively, P = 0.01) (Supplementary Table 5). The proportion of caesarean delivery was even higher (63%) in the GBS DNA-positive cases where the infant experienced neonatal morbidity related to sepsis (Table 2). This pattern is the opposite of what would have been predicted if GBS DNA was present in the placenta due to contamination at the time of vaginal birth. We also compared the strength of association between having a positive high vaginal swab in the antenatal period and the risk of the outcomes of interest. There were either no statistically significant associations or the associations were weaker than observed with the presence of GBS DNA in the placenta (Supplementary Table 6). Hence confounding by contamination of the placenta with GBS during vaginal birth is not a plausible explanation for our findings. This interpretation is consistent with the fact that the biopsy was taken from the interior of the placenta and was washed to remove surface contamination (Methods).
We next considered the potential for contamination during sample analysis. There was also no evidence of batch effects in relation to the conduct of the PCR–qPCR assay for placental GBS (Extended Data Fig. 5 and Supplementary Table 7). Moreover, all of the qPCR plates contained multiple negative controls, which were included at every step of the experimental workflow, and none of these (0/129 wells) were positive for GBS. To test the validity of the GBS DNA signal further, we analysed additional samples from the 36 placentas that were positive for GBS DNA and from 36 GBS DNA-negative placentas using a novel reverse transcriptase (RT)–qPCR assay for GBS 16S ribosomal RNA (Extended Data Fig. 6). RNA, unlike DNA, is highly prone to degradation and is much less likely to be an environmental contaminant. Moreover, this assay did not require to be nested because of the greater amount of template (that is, rRNA versus DNA) per organism. Despite the fact that the majority of samples had not been collected using a protocol optimized for RNA preservation, the level of agreement in classification of GBS by the presence of 16S RNA and DNA was 87%, and this was highly statistically significant (κ = 0.72, P = 3.5 × 10−10). Moreover, when we re-analysed the case control study and re-defined GBS status based on the presence of both GBS 16S DNA and rRNA, all of the previously identified associations remained highly statistically significant and the associations with sepsis- and inflammation-related outcomes became stronger (Supplementary Table 8).
Placental GBS and foetal cytokine storm
Umbilical cord serum was available from 11 samples from term births across both studies where the placenta was positive for GBS DNA. We analysed levels of four pro-inflammatory cytokines that have previously been associated with GBS8, namely interleukin (IL)-1β, IL-6, IL-8 and tumour necrosis factor (TNF)-α and compared the 11 GBS-positive cases with 129 cord serum samples from infants with GBS-negative placentas where the infants were not admitted to the NNU. Umbilical cord blood levels of IL-1β, IL-6 and IL-8, but not TNF-α, were more likely to be elevated in the group where GBS had been detected in the placenta (Fig. 2b). We defined a foetal cytokine storm as two or more pro-inflammatory cytokines that were elevated >10 times the median level in controls. Cytokine storm was observed in 4/11 (36%) cases where the placenta was GBS positive and 5/129 (4%) placentas were negative for GBS DNA (OR 14.2, 95% CI 3.6–69.8, P = 0.002) (Fig. 2c). There was no association between the presence of GBS DNA in the placenta and levels of pro-inflammatory cytokines in placental protein lysates obtained from the same biopsies (Fig. 2d) or in maternal blood before the onset of labour and near term (Fig. 2e).
Clinical features of cases of proven and probable GBS sepsis
There was a total of 3,689 term births where placental sampling had been performed. Among this group there were three cases of proven GBS sepsis (8.1 (95% CI 1.7–23.7) per 10,000 births), which were all admitted to the NNU. In addition, there were 13 cases of NNU admission with strong clinical or histopathological evidence of sepsis, where GBS DNA was detected in the placenta but not postnatal culture of the infant (35.2 (95% CI 18.8–60.2) per 10,000 births), and we refer to this as probable but culture-negative sepsis. Hence, approximately one birth in 200 had either proven GBS sepsis or probable but culture-negative sepsis plus GBS DNA in the placenta. This is approximately ten times greater than the currently estimated rate of early neonatal GBS disease following term birth9. Clinical characteristics for the 16 cases are tabulated separately by whether there was proven GBS sepsis or probable but culture-negative sepsis plus the presence of GBS DNA in the placenta (Table 2). Key observations were that only 3 of the 16 cases had GBS colonization detected in the antenatal period and only three had antibiotics in labour. The majority of the cases were delivered by caesarean section for foetal distress. Interestingly, none of the three cases of proven GBS sepsis had histopathological evidence of inflammation, whereas this was present in the majority of cases of probable but culture-negative sepsis plus the presence of GBS DNA in the placenta.
Discussion
We performed discovery and validation studies and show that the presence of GBS DNA in the placenta is associated with an increased risk of neonatal morbidity, as evidenced by NNU admission. When analysed by the cause, we found that the association was explained by increased rates of admission with probable but culture-negative sepsis and with culture-positive proven GBS sepsis. Although the number of patients was limited, the validity of these findings was further supported by the fact that there were similar associations when NNU admission was classified on the basis of blinded histopathological examination of the foetal membranes and umbilical cord. Furthermore, the likely mechanism of the observed morbidity in a proportion of these infants is a cytokine storm, which was evident in utero. We believe that it is plausible that the presence of a pathogen in a normally sterile site10 would be causally associated with symptoms, signs and biomarkers of sepsis. The associations were similar when we detected GBS by the presence of GBS rRNA and the presence of GBS RNA suggests the presence of live, albeit rare, bacteria. Moreover, we observed that 10–15% of infants who were born with symptoms, signs or laboratory tests suggestive of sepsis had GBS DNA present in the placenta even though the organism was not cultured from the neonate. We conclude that GBS causes about ten times the number of cases of neonatal morbidity than is currently recognized and that this morbidity is associated with bacterial invasion of the placenta and extreme activation of the foetal innate immune system before birth.
Among women who are colonized by GBS, the risk of EOD is reduced by more than 80% by the use of intrapartum antibiotic prophylaxis (IAP)11. Many countries, including the United States, routinely screen all pregnant women for GBS and administer IAP to those who screen positive. A substantial minority of countries (40%), including the United Kingdom, do not perform universal screening and IAP is only given to women who have a positive culture following a clinically indicated swab12. The decision not to screen in the United Kingdom is based on multiple facets of the problem, including the fact that detection of genital tract colonization is temporally variable in a given woman, only a small minority of babies exposed to GBS develop a clinical infection, a very large number of women need to be treated to prevent each case of EOD, there is an absence of level 1 evidence that universal screening improves outcomes, and the rates of EOD in the United Kingdom are comparable with other countries where screening takes place13. However, the current analysis demonstrated that only 3/16 cases affected by GBS (that is, proven GBS sepsis or probable but culture-negative sepsis where GBS DNA was present in the placenta) received antibiotics in labour. Given the efficacy of IAP to prevent neonatal sepsis, these results suggest that identification of these cases and treatment with antibiotics in labour may have prevented a number of the adverse outcomes.
The current findings are of clinical relevance in a number of areas. First, the study highlights that analysis of the placenta immediately after birth may allow detection of intra-uterine invasion by GBS and thus infants who are at increased risk of neonatal morbidity could be identified. Second, as GBS was clinically undetectable in the neonate in the majority of cases of neonatal morbidity associated with the presence of GBS DNA in the placenta, and as we have previously shown that GBS DNA is present in the placenta in very small amounts5, the data indicate that some neonatal morbidity may be due to an exaggerated inflammatory response to a burden of pathogen that is too low to be detected as a clinical infection. Experiments in neonatal mice have demonstrated that administration of small numbers of GBS colony forming units results in an increased risk of neonatal death, which can be prevented by immune blockade (genetic or pharmacological)14. The current study is also highly relevant to the development of interventions to prevent GBS sepsis, such as trials of GBS vaccination in pregnancy15 and a current United Kingdom randomized controlled trial of screening for GBS and IAP (GBS3, ISRCTN49639731; https://www.gbs3trial.ac.uk/). Our findings indicate that the incidence of adverse neonatal outcome that might be prevented by such interventions is much greater than previously thought, being ~1 in 200 as opposed to ~1 per 2,000 births at term. Identifying all cases of neonatal morbidity caused by GBS could make it easier to demonstrate the clinical effectiveness of interventions. Moreover, the potential clinical impact of these interventions may be far greater than estimated on the basis of previous assessments of the burden of disease. The study is also relevant when considering whether physiological development of the foetus includes colonization with microbiota10. We found that the only organism present in the placenta before labour onset was GBS5. As we now show that the presence of this organism in the placenta is associated with an increased risk of adverse neonatal outcome, the current study provides further support for the ‘sterile womb’ model of normal foetal development.
The strong association between placental GBS and genital tract colonization is consistent with the possibility that the infection originates from the genital tract. However, only a minority of cases with placental GBS DNA had chorioamnionitis, which suggests that placental infection by GBS is not invariably due to passage of the organism through the foetal membranes. The timing of invasion is probably before the onset of labour in a large proportion of affected placentas, as we previously demonstrated that the proportion of placentas that were positive for GBS DNA did not vary between women who delivered before versus after labour onset and membrane rupture5. It is also possible that invasion precedes pregnancy as it is known that GBS can infect the non-pregnant endometrium16. Hence it is possible that the GBS detected in the placenta originated from the decidua; that is, placental infection could occur by implantation of the conceptus in GBS-infected decidua, followed by local invasion of the placenta by decidual GBS. Further studies will be required to address this point. It is of particular interest that none of the three cases of proven GBS sepsis had histopathological features, indicating that infection ascended during labour, whereas two out of the three cases had GBS present in the placenta. Although the numbers are small, these findings indicate that antenatal invasion by GBS may be a particular feature of culture-proven GBS EOD.
Strengths of the current study include the fact that it was prospective, there were hypothesis-generating and hypothesis-testing elements, and we combined extensive clinical data with comprehensive biological samples. The latter allowed objective classification of inflammation in 99% of NNU admissions using histopathology. Moreover, collection of cord blood allowed us to address the mechanisms underlying the associations. However, the study also has weaknesses. First, this is a report from a single centre with a relatively homogeneous population. Second, we did not have genital tract culture results from all participants as universal screening for GBS is not currently recommended in the United Kingdom17. However, as discussed above, the data do not support contamination during vaginal delivery as a plausible explanation of our findings. A third relative weakness is that, although we sampled four sites of the placenta, the volume of tissue used was a small fraction of the total organ and, therefore, we may have underestimated the proportion of cases with intra-uterine invasion. However, there was a high level of agreement for the detection of GBS analysing different samples from the same placentas using two different methods. Fourth, we confined the current analysis to term births only. This is because neonatal unit admission and suspected sepsis are very common among infants born preterm; hence, unlike term births, there is not a valid control group of healthy preterm infants. Finally, the immediate clinical application of these results may be limited as it is currently not feasible to test the placenta for the presence of extremely low levels of GBS DNA within a timescale that can inform immediate neonatal care. However, a battery of novel molecular methods for rapid detection of pathogens have been developed, many of which have been evaluated and refined in the coronavirus disease 2019 pandemic18. It is plausible that technological developments in this field could be applied in the perinatal setting for the detection of placental GBS.
Methods
Patient selection
We used data and samples from a prospective cohort of unselected nulliparous women with a singleton pregnancy and attending the Rosie Hospital, Cambridge UK for antenatal care between 2008 and 2013. The only clinical exclusion criterion for the study was multiple pregnancy. The rationale, design and conduct of the study have been described elsewhere6,19,20. In brief, women were recruited around the time of their dating ultrasound scan (typically at ~12 weeks) and were seen for research visits at 20, 28 and 36 weeks of gestational age. Following delivery, a team of technicians performed systematic sampling of the placenta, umbilical cord and foetal membranes, and samples were flash frozen for molecular analysis and fixed for microscopy (see below). Umbilical cord blood was collected from about a third of participants. Outcome data were obtained for all participants by individual examination of the medical record of the mother and by linkage to a range of electronic databases of clinical information, including the results of all microbial cultures performed during the pregnancy. In the whole pregnancy outcome prediction (POP) study population (n = 4,212), the median age, height and body mass index (BMI) and interquartile ranges (IQRs) were 30.3 (26.8–33.4) years, 165 (161–169) cm, and 24.1 (21.8–27.3) kg m−2, respectively, and 13% of the women were smokers at recruitment. In the current work, preterm births were excluded and detailed characteristics of women included in this study are given in Supplementary Tables 1 and 2. Participants received no compensation for taking part in the study. Ethical approval for the study was given by the Cambridgeshire 2 Research Ethics Committee (reference number 07/H0308/163), and all women gave written informed consent. This study is in compliance with all relevant ethical regulations.
Discovery case control study
Participants eligible for the first case control study were those included in a previous paper5. In brief, these participants included two subgroups: (1) participants delivered by planned caesarean section where GBS was detected in the placenta using deep sequencing, and (2) participants where the presence of GBS DNA was determined by 16S rRNA amplicon sequencing, using DNA obtained from the same placenta using two different DNA extraction kits. The participants in subgroup 1 were all delivered by planned caesarean section and consisted of 20 women with a diagnosis of preeclampsia, 20 women delivering a small infant for gestational age and 40 controls. The participants in the second subgroup consisted of 100 women with a diagnosis of preeclampsia, 100 women delivering a small infant for gestational age, 100 preterm births and 200 controls. The women in the second subgroup were not selected in relation to mode of delivery. As there was overlap between the two groups, the two subgroups combined had data on placental GBS status of 537 participants. We excluded preterm births and one sample failed analysis, resulting in a study group of 436 births at term. Case status was defined as admission of the infant to the neonatal unit (NNU) within 48 h of birth and for 48 h or more, which had previously been defined and employed as a marker of significant and immediate neonatal morbidity6. Admissions were confined to episodes following delivery (that is, the definition did not include infants who were discharged from hospital following delivery and subsequently readmitted). Controls were pregnancies where this did not occur. The characteristics of the cases and controls are tabulated (Supplementary Table 1). Briefly, the median maternal age varied between 31 and 30 years between cases (n = 41) and controls (n = 395), respectively. The median BMI was similar between the groups (24 kg m−2 in cases and 25 kg m−2 in controls). The prevalence of smoking at booking was 15% in cases and 6% among the controls and the prevalence of alcohol consumption was 0% in cases and 5% among the controls. Patient selection for the current work is presented in a flow diagram (Extended Data Fig. 1).
Validation case control study
Participants eligible for the second case control study were pregnancies where delivery occurred at term, the placenta had been biopsied after the birth and the baby was live born. Cases were defined as any eligible participant where the infant was admitted to the neonatal unit without limit of timing or duration. The scope of neonatal admission was broadened as further analyses to define sepsis phenotypes was planned (see below) but, again, cases related solely to the delivery admission. Controls were selected in a ratio of two controls for each case. After selection of cases and controls, we excluded any participants included in the first case control study. The characteristics of the cases and controls are tabulated (Supplementary Table 2). Briefly, the median maternal age varied between 31 and 30 years between cases (n = 239) and controls (n = 686). The median BMI was similar between the groups (25 kg m−2 in cases and 24 kg m−2 in controls). The prevalence of smoking at booking was 5% in both groups and the prevalence of alcohol consumption was 5% in cases and 4% among the controls. Patient selection is presented in a flow diagram (Extended Data Fig. 1).
The cause of neonatal unit admission was defined on the basis of clinical assessment of the infant’s medical record and by histopathology of the foetal membranes and umbilical cord. Both forms of assessment were performed blind to placental GBS DNA status. Clinical assessment was performed by an experienced consultant neonatologist (H.S.W.) and admissions were categorized as being unrelated to sepsis (no clinical signs or laboratory tests suggestive of sepsis), possible sepsis (clinical signs of sepsis but no laboratory tests supportive of sepsis), probable sepsis (clinical signs of sepsis plus laboratory tests supportive of sepsis but with a negative septic screen) and proven sepsis (GBS cultured from a normally sterile site) (Supplementary Table 3). Histopathological examination was performed by an experienced consultant perinatal pathologist (F.J.). Membranes (n = 312) were prepared as a roll and cut in cross section, and umbilical cord (n = 314) was also cut in a cross section where all cord vessels were included. Sections were stained using haematoxylin and eosin (H&E) and reported blind to placental GBS DNA status, on the basis of a previously described classification system7, where stage 2 or stage 3 evidence was regarded as positive for chorioamnionitis or funisitis, and stage 1 or no evidence was regarded as negative.
Placental biopsy
Placentas were collected after delivery and the procedure has previously been described in detail19. Placental sampling was confined to the placental terminal villi (foetal tissue). Villous tissue was obtained from four separate lobules of the placenta after trimming to remove adhering decidua from the basal plate, that is samples were from the interior of the placenta. Areas of the placenta to be biopsied were selected on the basis of no visible damage, haematomas or infarctions. To remove blood and surface contamination the samples were rinsed in chilled sterile phosphate-buffered saline (Oxoid Phosphate Buffered Saline Tablets, Dulbecco A; Thermo Fisher Scientific dissolved in ultrapure water (ELGA Purelab Classic 18 MΩ cm)). After collection, all placental samples were frozen in liquid nitrogen and stored at −80 °C until further processing. For DNA isolation, approximately 25 mg of villous tissue (combined weight obtained from fragments from all four biopsy collection points) was cut from the stored tissue. Tissue processing was carried out in a class 2 biological safety cabinet.
DNA analysis in the discovery case control study
DNA isolation and the methods for detecting the presence of GBS DNA in the first case control study were described in detail in the original publication5. In brief, DNA was extracted using an MP Biomedical kit. Deep sequencing was performed using the Illumina XTen platform, with 150 base pair paired-end sequencing with an average of 424 million reads per sample. A sample was defined as positive for GBS if there was ≥1 read aligned to the GBS genome. The 16S rRNA PCR was performed using degenerate primers and amplified the V1–V2 region of the gene. Amplicons were sequenced on the Illumina MiSeq platform using 250 base pair paired-end sequencing. Samples were defined as GBS DNA positive if >1% of amplicons were derived from GBS. Analyses were replicated using the threshold >0.1%. The previous study reported a high level of agreement between deep sequencing and 16S rRNA amplicon sequencing (P = 1.5 × 10−8). There were no cases where a sample was positive by 16S rRNA and negative by deep sequencing but there were 4 samples out of 79 that were positive by deep sequencing but negative by 16S rRNA amplicon sequencing. This could either indicate greater sensitivity or more false positives using deep sequencing.
DNA analysis in validation case control study
DNA was isolated from placental tissue using the QIAamp 96 DNA QIAcube HT Kit (Qiagen; 51331) and the QIAcube HT instrument for automated high-throughput nucleic acid purification in 96-well format (Qiagen). The DNA isolation was carried out according to the manufacturer’s instructions with the following initial steps. Placental biopsies were lysed in 200 µl of lysis buffer, containing 20 mM Tris–HCl (pH 8) with 2 mM ethylenediaminetetraacetic acid (EDTA) (Sigma; T9285), 1.2% Triton X-100 (Sigma; T8787), lysozyme 10 mg ml−1 (Sigma; 10837059001), mutanolysin 300 U ml−1 (Sigma; SAE0092), and incubated at 37 °C for 30 min with 400 rpm shaking. After addition of 20 µl of proteinase K per sample (provided by the QIAamp 96 DNA QIAcube HT Kit), samples were incubated at 56 °C overnight with 600 rpm shaking. The following day the samples were transferred to the 96-well plate and 4 µl of RNase A (100 mg ml−1) was added to each sample (Qiagen; 19101). After an incubation at room temperature for 5 min, the plate was loaded on the QIAcube HT instrument and run using the protocol for DNA isolation with the final elution in 200 µl of elution buffer performed twice. Negative controls performed at this stage had tissue lysis buffer carried through the entire experimental workflow (n = 17 DNA extraction blanks; Extended Data Fig. 5). DNA concentrations were determined by Nanodrop Lite (Thermo Fisher Scientific) and samples were diluted to a concentration of 12.5 ng µl−1 with IDTE (10 mM Tris and 0.1 mM EDTA, pH 8) (Integrated DNA Technologies; 11-05-01-05), using the PIPETMAX Liquid Handler (Gilson).
The presence of GBS DNA in placental samples was assessed using a nested multiplex PCR–qPCR assay targeting the GBS sip and 16S rRNA genes, and the human RNaseP gene (RPPH1). Briefly, the first round (outer) of PCR was performed using the Multiplex PCR 5X Master Mix (New England Biolabs; M0284S). The sip primers and probe were as previously described5. The PCR–qPCR assay for the 16S rRNA gene utilized a GBS-specific region of the gene (Extended Data Fig. 2). The following primers were employed for detection of the GBS 16S rRNA gene: forward (outer F) 5′-TAAAAGGAGCAATTGCTTCACTGTG-3′ and reverse (outer R) 5′-TCCTCCAGTTTCCAAAGCGT-3′; amplification was performed in 50 μl with primers at a final concentration of 0.2 μM and 500 ng of placental DNA per reaction. Negative and positive controls performed at this stage had H2O (n = 25 reactions) or GBS genomic DNA (n = 100 reactions with different GBS gDNA quantities, that is, 4,000, 400, 40 or 4 copies per well; ATCC; BAA-611DQ) as the reaction substrates, respectively (Extended Data Fig. 5). The PCR amplification profile had an initial step of 95 °C for 3 min followed by 15 cycles of 95 °C (20 s), 48 °C (60 s) and 68 °C (60 s) and a final incubation at 68 °C for 3 min. The second round (nested) of qPCR was performed using the TaqMan Multiplex Master Mix (Thermo Fisher Scientific; 4461882); the sip TaqMan assay as previously described with FAM dye/MGB probe at a final 1× concentration (Thermo Fisher Scientific, Assay ID: Ba04646276_s1); a custom-made TaqMan assay for the GBS 16S rRNA gene at a final 1× concentration with forward primer (inner F) 5′-AATGGACGGAAGTCTGAC-3′, reverse primer (inner R) 5′-GTTAGTTACCGTCACTTGGTA-3′ and JUN dye/QSY probe 5′-AGAGAAGAACGTTGGTAGGAGTGGA-3′ (primers and probe by Thermo Fisher Scientific); and a human RNaseP TaqMan assay with VIC dye/MGB probe (gene symbol: RPPH1, Thermo Fisher Scientific, Assay ID: Hs04930436_g1) at a final 0.5× concentration. In each well, 6.1 μl of the first round of PCR (or water in the no-template control/blank wells) was used as the reaction substrate in a total volume of 10 μl. Negative and positive controls performed at this stage had H2O (n = 28 wells) or GBS gDNA (n = 112 wells with different GBS gDNA quantities, that is, 4,000, 400, 40 or 4 copies per well) as the reaction substrates, respectively (Extended Data Fig. 5). The qPCR amplification profile had an initial step of 95 °C for 20 s followed by 50 cycles of 95 °C (5 s), 50 °C (10 s) and 60 °C (20 s). Samples were excluded from the PCR–qPCR analysis if the RNaseP signal was not detectable, indicating absence of gDNA in the PCR assay or a technical failure. The specificity of this assay was tested by amplifying GBS (Streptococcus agalactiae) DNA in presence of genomic DNA from Streptococcus pyogenes (ATCC; 700294DQ) and Streptococcus pneumoniae (ATCC; 700669DQ) (Supplementary Table 9). qPCR data were collected using the instrument software (QuantStudio 6 Flex system version 1.3, Thermo Fisher Scientific).
When we compared samples that had a detectable signal for GBS, there was a very strong correlation between the signals for 16S and sip when the cycle threshold (Ct) count was <30 and no correlation was observed with higher values (Extended Data Fig. 7). There were eight placental biopsies that were positive using the 16S PCR–qPCR assay but negative with sip, and no samples were positive by sip but negative by 16S. Moreover, where a sample was positive using both methods, the Ct count was higher (that is, a weaker signal) for the sip than for the 16S assay (mean difference 2.4, 95% CI 1.0–3.7, P = 0.0009). Extended Data Fig. 8 illustrates a representative example. Given that the GBS genome has seven copies of the 16S rRNA gene but only one copy of sip, we assume that there is more template for the 16S assay for a given number of colony forming units than for the sip assay. We concluded that the 16S PCR–qPCR assay was more sensitive and defined a positive sample simply on the basis of being positive by 16S PCR–qPCR.
Analysis of GBS 16S rRNA
Placental RNA was isolated from 72 samples (36 GBS DNA-positive and 36 GBS-negative placentas from the validation study) using the RNeasy Plus Mini Kit (Qiagen; 74134) according to the manufacturer’s instructions with the following additional steps. Placental biopsies (approximately 15 mg per sample, including fragments from all four biopsy collection points) were lysed in 600 µl of Buffer RTL Plus and homogenized by bead-beating (Lysing Matrix A tubes, 2 × 30 s, speed of 6.0 m s−1 on a FastPrep-24, MP Biomedical). The subsequent steps were performed following the manufacturer’s instructions and RNA was eluted from the spin columns with 30 μl of RNase-free H2O. RT reactions were performed using 1 μg RNA per sample, 0.1 μM specific primer (outer reverse primer for GBS 16S rRNA described above) and Superscript IV (Invitrogen; 18090050) in a total volume of 25 μl. Incubations were carried according to the instructions provided in the Superscript IV datasheet (65 °C for 5 min, ice incubation for 2 min, 53 °C for 5 min and 80 °C for 10 min). The RT setup included two types of negative control (omitting the enzyme or the template RNA from the reaction) and three positive controls with decreasing concentrations of GBS RNA (100, 20 and 4 fg per well). The qPCR was performed using 3.6 μl of cDNA, the custom-made GBS 16S TaqMan assay described above and the TaqMan Multiplex Master Mix in a total volume of 12 μl. The qPCR amplification profile had an initial step of 95 °C for 20 s, followed by 50 cycles of 95 °C (5 s) and 60 °C (25 s). Samples were run in duplicate and were considered GBS positive if both wells had 16S signal. The qPCR setup included negative and positive controls with H2O or GBS gDNA (4000, 400, 40 or 4 copies per well, as described above) as the reaction substrates, respectively (Extended Data Fig. 5). Analysis of the controls performed at the various steps of the experimental workflow revealed the expected results: no 16S signal in the 20 wells corresponding to the negative controls and signal in 26/28 positive controls (signal was not detected in 2/4 wells corresponding to the RT positive controls obtained from the lowest GBS RNA quantity, that is, 4 fg per well).
Assessment of contamination
Assessment of contamination in the discovery case control study is described in detail in the original publication5. In the validation study we performed an extensive series of control experiments to determine whether the results might be affected by contamination, given that PCR–qPCR assays are highly sensitive and prone to contaminant dependent signals. First, we compared rates of GBS DNA in the placenta in relation to mode of delivery and found that it was less common among infants delivered vaginally (Supplementary Table 5). This is the opposite pattern to what would be expected if the placenta was usually positive due to contamination from the mother’s genital tract. Second, we compared rates of GBS DNA in the placenta in relation to week of delivery. The number of GBS-positive placentas demonstrated no temporal association with the week of sampling (Extended Data Fig. 4 and Supplementary Table 4), whereas we previously demonstrated a temporal association with the contaminant signal Deinococcus geothermalis5. Third, all qPCR plates included analysis of positive and negative controls performed throughout the experimental workflow and each plate was designed to have similar numbers of cases and controls (Extended Data Fig. 5 and Supplementary Table 7). Analysis of signals by plate demonstrated no pattern in the distribution of positive results. Moreover, the signals from positive and negative controls demonstrated 100% agreement with the expected results. Finally, we re-tested all of the GBS DNA-positive placentas plus the same number of controls using different biopsies and detected GBS by RT–qPCR of 16S ribosomal RNA, and then assessed the level of agreement between the two assays and the associations with the clinical outcomes of interest (Supplementary Table 8).
Cytokine ELISAs
Cytokine levels were measured using targeted enzyme-linked immunosorbent assays (ELISAs) in umbilical cord and maternal serum samples, and were measured in placental protein lysates using the Ella platform (Bio-Techne) and cartridges for the analysis of IL-1β, IL-6, IL-8 and TNF-α (Simple Plex Cartridge Kit for 32 samples, containing IL-1β/IL-1F2, IL-6 second generation, IL-8, TNF-α second generation; SPCKC-PS-003229, Bio-Techne). Positive controls (human IL-1β; 894962, human IL-6; 894968, human IL-8/CXCL8; 894950, and human TNF-α; 894977, Bio-Techne) were prepared according to the manufacturer’s instructions. We ran 145 unique cord serum samples from term pregnancies in two batches and cytokine levels were expressed as the multiple of the median (MoM) of GBS-negative samples analysed in the same batch. In cases where the median was zero, the lowest detected value was used instead of the median in the calculation. GBS positives were defined as samples with 16S signal using the nested PCR–qPCR assay and/or with one or more GBS read identified by deep sequencing and/or GBS 16S rRNA amplicons >1% in the placenta. Positive samples that were weakly positive (that is, GBS 16S rRNA amplicons >0% and <1%; n = 5) were excluded from the primary analysis. However, we performed a sensitivity analysis where the process was repeated defining GBS positivity as GBS 16S amplicons >0.1% of all reads (Extended Data Fig. 9). Controls were pregnancies with GBS-negative placentas on all tests completed and with infants not admitted to NNU. Therefore, the current analysis included 140 samples, 11 cases and 129 controls.
Cytokines were also assayed in maternal plasma and in placental biopsies from patients included in the current analysis using the targeted ELISAs described above. A total of 55 maternal serum samples obtained at 36 weeks gestation were assayed, which were randomly selected among patients with GBS-positive (n = 25) and negative (n = 30) placentas. Cytokines were also measured in protein lysates obtained from 58 term placental samples, which were randomly selected among patients with GBS-positive (n = 26) and negative (n = 32) placentas. GBS positives and negatives were defined as in the cord serum analysis described above.
Serum samples were diluted 1:2 with sample diluent (SD13) and run according to the manufacturer’s instructions. Placental protein lysates were prepared from the same placental biopsies used for the detection of GBS DNA (5–10 mg from each placenta). Tissues were homogenized in 400 μl of lysis buffer (Phosphate Buffered Saline with 0.1% Triton X-100 and protease inhibitors (cOmplete Mini EDTA-free Protease Inhibitor Tablet; Roche; 04693159001)) by bead-beating in Lysing Matrix D tubes (MP Biomedical; 116913050-CF) for 10 s at a speed of 4 m s−1 on a FastPrep-24 (MP Biomedical). Lysates were centrifuged twice at 10,000g for 10 min at 4 °C and the supernatants were quantified using the Pierce BCA Protein Assay Kit (ThermoFisher; 23227). Placental lysates were not diluted with SD13 before loading them on the cartridges.
Statistics
All the aspects of the POP study, including the results of the research ultrasound scans, were conducted blind, and data were unblinded only at the statistical analysis stage. Participants were allocated into groups based on pregnancy outcome and during the experiments analysis batches contained samples from both cases and controls. Outcome data were ascertained by review of each woman’s paper case record by an academic clinical fellow (K.S.) and a neonatologist (H.S.W.), and by record linkage to clinical electronic databases20. Proportions were compared using the chi-squared test or Fisher’s exact test, as appropriate, and Wilson 95% CIs were calculated21. Ninety-five percent CI for unadjusted odds ratios were calculated using the combination of the Baptista–Pike method and the mid-P approach22. Odds ratios adjusted for maternal characteristics (age, BMI, smoking and marital status) were estimated using multivariable logistic regression. The sample size for the POP study cohort was pre-determined by the total recruitment achieved. Power calculations were performed for all analyses using the available sample size to estimate the statistical power to detect a given strength of association based on two-sided α = 0.05. The power calculation for the primary outcome (admission of the infant to the neonatal unit) was based on observing the same relative risk and proportions of exposure and outcome in the validation study as observed in the development study. Power calculations for all the secondary outcomes (foetal cytokine storm, probable and proven sepsis, chorioamnionitis and funisitis) were based on the observed numbers of GBS-positive and GBS-negative placentas in the validation study, the observed proportion of the given outcome in the GBS-negative group of the validation study, and a range of possible odds ratios. The results were plotted for each of the secondary outcomes (Extended Data Fig. 10). All P values were two sided, and all analyses were performed using Stata version 17 (StataCorp LLC) and GraphPad Prism version 9.2.0 (GraphPad Software LLC).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Any additional data are available from the corresponding authors on reasonable request and subject to a Data Transfer Agreement, as they include clinical information and in compliance with the ethical permission for the POP study. No participant identifiable information will be disclosed. Requests can be addressed to G.C.S.S. (gcss2@cam.ac.uk) and D.S.C.-J. (dscj1@cam.ac.uk) and will be answered within 1 month. Previously described datasets5 are: the 16S rRNA gene sequencing datasets, which are publicly available under European Nucleotide Archive (ENA) accession number ERP109246 and the metagenomics datasets, which are available with managed access in the European Genome-phenome Archive (EGA) accession number EGAD00001004198. Source data are provided with this paper.
References
Prevention of group B streptococcal early-onset disease in newborns: ACOG committee opinion, number 797. Obstet. Gynecol. https://doi.org/10.1097/AOG.0000000000003668 (2020).
Russell, N. J. et al. Maternal colonization with group B Streptococcus and serotype distribution worldwide: systematic review and meta-analyses. Clin. Infect. Dis. 65, S100–S111 (2017).
Russell, N. J. et al. Risk of early-onset neonatal group B streptococcal disease with maternal colonization worldwide: systematic review and meta-analyses. Clin. Infect. Dis. 65, S152–S159 (2017).
Goncalves, B. P. et al. Group B Streptococcus infection during pregnancy and infancy: estimates of regional and global burden. Lancet Glob. Health 10, e807–e819 (2022).
de Goffau, M. C. et al. Human placenta has no microbiome but can contain potential pathogens. Nature 572, 329–334 (2019).
Sovio, U., White, I. R., Dacey, A., Pasupathy, D. & Smith, G. C. Screening for fetal growth restriction with universal third trimester ultrasonography in nulliparous women in the Pregnancy Outcome Prediction (POP) study: a prospective cohort study. Lancet 386, 2089–2097 (2015).
Khong, T. Y. et al. Sampling and definitions of placental lesions: Amsterdam placental workshop group consensus statement. Arch. Pathol. Lab Med 140, 698–713 (2016).
Patras, K. A. & Nizet, V. Group B streptococcal maternal colonization and neonatal disease: molecular mechanisms and preventative approaches. Front. Pediatr. 6, 27 (2018).
O’Sullivan, C. P. et al. Group B streptococcal disease in UK and Irish infants younger than 90 days, 2014–15: a prospective surveillance study. Lancet Infect. Dis. 19, 83–90 (2019).
Kennedy, K. M. et al. Questioning the fetal microbiome illustrates pitfalls of low-biomass microbial studies. Nature 613, 639–649 (2023).
Ohlsson, A. & Shah, V. S. Intrapartum antibiotics for known maternal Group B streptococcal colonization. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD007467.pub4 (2014).
Le Doare, K. et al. Intrapartum antibiotic chemoprophylaxis policies for the prevention of Group B streptococcal disease worldwide: systematic review. Clin. Infect. Dis. 65, S143–S151 (2017).
Seedat, F. et al. Universal Antenatal Culture-Based Screening for Maternal Group B Streptococcus (GBS) Carriage to Prevent Early-Onset GBS Disease (UK National Screening Committee, 2016).
Mancuso, G. et al. Dual role of TLR2 and myeloid differentiation factor 88 in a mouse model of invasive group B streptococcal disease. J. Immunol. 172, 6324–6329 (2004).
Absalon, J. et al. Safety and immunogenicity of a novel hexavalent group B streptococcus conjugate vaccine in healthy, non-pregnant adults: a phase 1/2, randomised, placebo-controlled, observer-blinded, dose-escalation trial. Lancet Infect. Dis. 21, 263–274 (2021).
Moreno, I. et al. Endometrial microbiota composition is associated with reproductive outcome in infertile patients. Microbiome 10, 1 (2022).
Clinical guidance [CG62]. Antenatal care for uncomplicated pregnancies. National Institute for Health and Care https://www.nice.org.uk/guidance/ng201 (2016).
Roberts, A. et al. A recent update on advanced molecular diagnostic techniques for COVID-19 pandemic: an overview. Front. Immunol. 12, 732756 (2021).
Pasupathy, D. et al. Study protocol. A prospective cohort study of unselected primiparous women: the pregnancy outcome prediction study. BMC Pregnancy Childbirth 8, 51 (2008).
Gaccioli, F., Lager, S., Sovio, U., Charnock-Jones, D. S. & Smith, G. C. S. The pregnancy outcome prediction (POP) study: investigating the relationship between serial prenatal ultrasonography, biomarkers, placental phenotype and adverse pregnancy outcomes. Placenta 59, S17–S25 (2017).
Newcombe, R. G. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat. Med. 17, 857–872 (1998).
Fagerland, M. W., Lydersen, S. & Laake, P. Recommended confidence intervals for two independent binomial proportions. Stat. Methods Med. Res. 24, 224–254 (2015).
Acknowledgements
The work was funded by the Medical Research Council (United Kingdom; MR/K021133/1) and supported by the National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre (Women’s Health theme). K.S. is funded by the Cambridge Wellcome Trust PhD Programme for Health Professionals. We thank L. Bibby, S. Ranawaka, K. Holmes, J. Gill, R. Millar, L. Sánchez Busó, J. Warner and K. Vickers for technical assistance during the study. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
G.C.S.S. and D.S.C.-J. conceived and designed the experiments. F.G., K.S. and S.L. performed the experiments. D.S.C.-J. and M.C.d.G. designed the 16S rRNA PCR–qPCR assay. U.S. performed all patient selection for case control studies and performed statistical analyses. H.S.W. performed blinded assessment of the indication for neonatal unit admission. F.J. performed blinded histopathological examination of the umbilical cord and foetal membranes. K.L.D. provided methodological advice on DNA extraction. J.P. and S.J.P. provided advice on GBS gDNA sequence and detection. E.C. managed sample collection and processing and the biobank in which all sample were stored. All authors contributed to writing the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
G.C.S.S. and D.S.C.-J. receive research funding from Pfizer Bacterial Vaccines for studies on the relationship between placental GBS DNA and maternal circulating levels of GBS antibodies. Cambridge Enterprise (United Kingdom) has filed a patent relating to the primers and probe used in the nested PCR–qPCR assay described in this paper with F.G., M.C.d.G., D.S.C.-J. and G.C.S.S. as the named inventors. The competing interests outside the area of the submitted work are as follows: J.P. reports grants from Pfizer and personal fees from Next Gen Diagnostics LLC; S.J.P. reports personal fees from Specific and personal fees from Next Gen Diagnostics; G.C.S.S. and D.S.C.-J. report grants from GlaxoSmithKline Research and Development Limited, grants and non-financial support from Roche Diagnostics Ltd and non-financial support from Illumina Inc; G.C.S.S. reports personal fees from GlaxoSmithKline Research and Development Limited; K.L.D. is an adviser for Pfizer, Minervax and GSK for GBS vaccines; and K.S., U.S., F.J., H.S.W., S.L. and E.C. declare no competing interests.
Peer review
Peer review information
Nature Microbiology thanks Sing Sing Way, David N. Fredricks and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Selection of participants for the studies.
Patients in the discovery study have been previously described5. Cases (n = 41) and controls (n = 395) are defined as pregnancies with an infant admitted or not admitted, respectively, to neonatal unit within 48 hours of birth and for 48 hours or more. In the validation study cases are defined as pregnancies with an infant admitted to neonatal unit without time limits for admission or duration of stay. The control group is represented by a cohort of random controls selected within the POP study where the baby was not admitted for neonatal care. The validation study excluded any patient who was included in the discovery study. In total, 1,361 patients were included in the current analyses. PTBs, preterm births.
Extended Data Fig. 2 Nested PCR-qPCR assay to detect the 16S GBS gene.
a, Schematic diagram of the nested PCR-qPCR assay. b, Multiple sequence alignment of the amplicons generated with the nested PCR-qPCR assay and the 16S GBS gene sequence (SnapGene Viewer 6.1). The sequences of the PCR amplicons (n = 6 from 4 placentas positive for 16S and sip, and 2 placentas positive for 16S) were determined by Sanger sequencing using the second-round (inner) reverse and forward primers. This analysis confirmed that the sequence of the qPCR products perfectly aligned to the GBS 16S gene sequence. c, Multiple sequence alignment of the 16S gene from various Streptococci: S. agalactiae (GBS) (NR_040821.1), S. dysgalactiae (MH393517.1), S. salivarius (KM221948.1), S. anginosus (MF578782.1), S. vestibularis (NR_042777.1), S. pyogenes (NR_028598.1), S. suis (NR_115737.1), S. urinalis (NR_115738.1), S. equi (NR_116010.1), S. uberis (U41048.1). The position of the inner primers, outer primers and Taqman probe of the nested PCR-qPCR assay are indicated. The red frames highlight regions that differ between species amplified using the qPCR inner primers.
Extended Data Fig. 3 Sensitivity of the sip qPCR and 16S PCR-qPCR assays for GBS detection.
Genomic Streptococcus agalactiae (GBS) DNA was used at 4000, 400, 40, or 4 copies/reaction in the unnested qPCR and the nested PCR-qPCR assays targeting the sip and 16S GBS genes, respectively. The two curves are described by semi-log equations, which were used to calculate the GBS genome copies at 25 Ct (3,855 and 11 copies required for the sip unnested and 16S nested assay, respectively). Means ± standard deviation are shown; n = 4 independent experiments with 2 technical replicates/each. Ct denotes cycle threshold and it is inversely associated with the relative abundance of the target.
Extended Data Fig. 4 Temporal distribution of deliveries with GBS positive placenta in the validation study.
The figure represents the number of weekly deliveries with GBS positive placenta (n = 36 in total). Day 1 of the first week of each year is indicated. n numbers of GBS positive and total deliveries per week are listed in Supplementary Table 4.
Extended Data Fig. 5 Spatial distribution of placental samples and controls in the qPCR plates.
The qPCR plates include all the placental samples from the validation study, which were run in triplicate. All the plates had a similar layout with the triplicate wells organized in a L-shape, except for plate 5a which had the triplicate wells organized horizontally. GBS positive samples (in red) had a detectable 16S signal. Positive controls contained decreasing quantities of GBS genomic DNA (4000, 400, 40, or 4 copies/well) added at the outer PCR (blue color gradient) or the inner qPCR (green color gradient) step. Negative controls contained H2O added at the outer PCR (darker grey) or the inner qPCR (lighter grey) step. DNA extraction blanks (tissue lysis buffer carried through the entire experimental workflow) are indicated in black. Our analysis included: 200 and 112 positive control wells for the PCR and qPCR, respectively, and they all had 16S and sip signal; 50 and 28 negative control wells for the PCR and qPCR, respectively, and they were all 16S- and sip-negative; 51 wells containing DNA extraction blanks, which were all 16S- and sip-negative. In total, we ran 129 negative control wells added at different stages of the experimental workflow and none of them had a detectable signal by either Taqman assay.
Extended Data Fig. 6 RT-qPCR assay to detect GBS 16S rRNA.
a, Schematic diagram of the RT-qPCR strategy. b, qPCR amplification plot representing 3 positive samples with signal for GBS 16S rRNA (green, blue and red curves), 1 negative sample with no 16S signal (yellow curve) and 2 negative controls samples (H2O or without the reverse transcriptase enzyme in the RT reaction in black and grey, respectively). Placental samples were run in duplicate and were considered GBS positive if both wells had signal for 16S rRNA. The relative abundance of the target is expressed using the Ct (cycle threshold) value, which is inversely associated with the signal. Rn (normalized reporter value) represents the fluorescence of the reporter dye normalized to the signal of the passive reference dye for a given reaction. The ΔRn is the Rn value of an experimental reaction minus the Rn value of the baseline signal generated by the instrument. This parameter indicates the magnitude of the fluorescent signal generated in the qPCR assay. RT denotes reverse transcriptase.
Extended Data Fig. 7 Comparison of sip and 16S PCR-qPCR signals for GBS in placental samples.
Correlation between the sip and 16S Ct values obtained in the nested PCR-qPCR assays targeting the two GBS genes (n = 44) using the data from the validation study. Samples with undetectable sip signal are plotted with Ct = nd (not detected, n = 8). Where samples were positive using both methods, the Ct count was higher for sip than for the 16S rRNA PCR-qPCR (mean difference = 2.4, 95% CI = 1.0 to 3.7, P = 0.0009). Pearson’s correlation coefficients (r) and two-tailed p values are reported for 16S Ct <30 (p < 0.0001) and Ct >30 (p = 0.56). Ct denotes cycle threshold.
Extended Data Fig. 8 Representative amplification plots of the 16S and sip PCR-qPCR assays in a placental DNA sample.
Amplification plots were obtained using the multiplex qPCR assay targeting the sip (green) and 16S (red) GBS genes and the human RNaseP (RPPH1, blue) gene. The relative abundance of the target is expressed using the Ct (cycle threshold) value, which is inversely associated with the signal. Rn (normalized reporter value) represents the fluorescence of the reporter dye normalized to the signal of the passive reference dye for a given reaction. The ΔRn is the Rn value of an experimental reaction minus the Rn value of the baseline signal generated by the instrument. This parameter indicates the magnitude of the fluorescent signal generated in the qPCR assay.
Extended Data Fig. 9 Sensitivity analysis of the association between placental GBS and cord cytokine levels.
In this analysis, GBS positives were defined as placental samples with one or more of the following: GBS identified by the 16S PCR-qPCR assay, GBS read identified by deep sequencing, or GBS 16S amplicons >0.1% of all reads (as compared to >1% in primary analysis). Cytokine levels were measured in 145 cord serum samples from term pregnancies with GBS positive (n = 16) and negative (n = 129) placentas, using the Ella platform (Bio-Techne). Cytokine levels are expressed as the multiple of the median (MoM) of control samples analysed in the same batch. For graphical purposes, samples with MoM=0 for interleukin-1β (n = 27) have been plotted using a value of MoM=0.0126 (the lowest MoM in the dataset). GBS negative controls are defined as pregnancies with GBS negative placentas on all tests completed and with babies not requiring NNU admission. The dotted line represents an elevation of MoM >10. IL-1β, interleukin-1β; IL-6, interleukin-6; IL-8, interleukin-8; TNF-α, Tumour Necrosis Factor alpha.
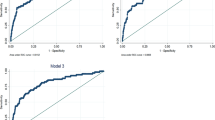
Extended Data Fig. 10 Power calculations for the secondary outcomes studied in this work.
Plots illustrate the power calculations for the cytokine storm (a), probable (b) and proven (c) sepsis, chorioamnionitis (d) and funisitis (e) outcomes and for a range of different odds ratios (OR). Calculations were based on the observed numbers of GBS positive and GBS negative placentas in the validation study, the observed proportion of the given outcome in the GBS negative group of the validation study, and a range of possible odds ratios. Alpha two sided and threshold = 0.05 were applied.
Supplementary information
Source data
Source Data Fig. 2
Contingency tables (for Fig. 1a,c) and cytokine levels (for Fig. 1b,d,e).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gaccioli, F., Stephens, K., Sovio, U. et al. Placental Streptococcus agalactiae DNA is associated with neonatal unit admission and foetal pro-inflammatory cytokines in term infants. Nat Microbiol 8, 2338–2348 (2023). https://doi.org/10.1038/s41564-023-01528-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-023-01528-2