Abstract
Transposon-based strategies provide a powerful and unbiased way to study the bacterial stress response1,2,3,4,5,6,7,8, but these approaches cannot fully capture the complexities of network-based behaviour. Here, we present a network-based genetic screening approach: the transcriptional regulator-induced phenotype (TRIP) screen, which we used to identify previously uncharacterized network adaptations of Mycobacterium tuberculosis to the first-line anti-tuberculosis drug isoniazid (INH). We found regulators that alter INH susceptibility when induced, several of which could not be identified by standard gene disruption approaches. We then focused on a specific regulator, mce3R, which potentiated INH activity when induced. We compared mce3R-regulated genes with baseline INH transcriptional responses and implicated the gene ctpD (Rv1469) as a putative INH effector. Evaluating a ctpD disruption mutant demonstrated a previously unknown role for this gene in INH susceptibility. Integrating TRIP screening with network information can uncover sophisticated molecular response programs.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data reported in this paper are available in Supplementary Tables 1–5. The raw TRIP fastq sequence data files are deposited in the Sequence Read Archive database under accession PRJNA483505. The RNA-seq data are deposited in the Gene Expression Omnibus database under accession GSE151991. The TFI strains are available from BEI Resources (https://www.beiresources.org/Home.aspx).
Code availability
The code required to process the TRIP and RNA-seq sequenced reads are available at https://github.com/robertdouglasmorrison/DuffyNGS, https://github.com/robertdouglasmorrison/DuffyTools and https://github.com/DavidRShermanLab/TRIPscreen.
References
Sassetti, C. M., Boyd, D. H. & Rubin, E. J. Comprehensive identification of conditionally essential genes in mycobacteria. Proc. Natl Acad. Sci. USA 98, 12712–12717 (2001).
Sassetti, C. M. & Rubin, E. J. Genetic requirements for mycobacterial survival during infection. Proc. Natl Acad. Sci. USA 100, 12989–12994 (2003).
Griffin, J. E. et al. High-resolution phenotypic profiling defines genes essential for mycobacterial growth and cholesterol catabolism. PLoS Pathog. 7, e1002251 (2011).
Langridge, G. C. et al. Simultaneous assay of every Salmonella Typhi gene using one million transposon mutants. Genome Res. 19, 2308–2316 (2009).
Gallagher, L. A., Shendure, J. & Manoil, C. Genome-scale identification of resistance functions in Pseudomonas aeruginosa using Tn-seq. mBio 2, e00315-10 (2011).
Van Opijnen, T., Bodi, K. L. & Camilli, A. Tn-seq: high-throughput parallel sequencing for fitness and genetic interaction studies in microorganisms. Nat. Methods 6, 767–772 (2009).
Goodman, A. L. et al. Identifying genetic determinants needed to establish a human gut symbiont in its habitat. Cell Host Microbe 6, 279–289 (2009).
Gawronski, J. D., Wong, S. M., Giannoukos, G., Ward, D. V. & Akerley, B. J. Tracking insertion mutants within libraries by deep sequencing and a genome-wide screen for Haemophilus genes required in the lung. Proc. Natl Acad. Sci. USA 106, 16422–16427 (2009).
Global Tuberculosis Report 2016 (World Health Organization, 2016).
Warner, D. F. & Mizrahi, V. Tuberculosis chemotherapy: the influence of bacillary stress and damage response pathways on drug efficacy. Clin. Microbiol. Rev. 19, 558–570 (2006).
Aldridge, B. B., Keren, I. & Fortune, S. M. The spectrum of drug susceptibility in mycobacteria. Microbiol. Spectr. 2, https://doi.org/10.1128/microbiolspec.MGM2-0031-2013 (2014).
Wallis, R. S. et al. Drug tolerance in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 43, 2600–2606 (1999).
Minch, K. J. et al. The DNA-binding network of Mycobacterium tuberculosis. Nat. Commun. 6, 5829 (2015).
Rustad, T. R. et al. Mapping and manipulating the Mycobacterium tuberculosis transcriptome using a transcription factor overexpression-derived regulatory network. Genome Biol. 15, 502 (2014).
Galagan, J. E. et al. The Mycobacterium tuberculosis regulatory network and hypoxia. Nature 499, 178–183 (2013).
Motter, A. E., Gulbahce, N., Almaas, E. & Barabasi, A. L. Predicting synthetic rescues in metabolic networks. Mol. Syst. Biol. 4, 168 (2008).
Wytock, T. P. et al. Experimental evolution of diverse Escherichia coli metabolic mutants identifies genetic loci for convergent adaptation of growth rate. PLoS Genet. 14, e1007284 (2018).
Wei, J. R. et al. Depletion of antibiotic targets has widely varying effects on growth. Proc. Natl Acad. Sci. USA 108, 4176–4181 (2011).
Xu, W. et al. Chemical genetic interaction profiling reveals determinants of intrinsic antibiotic resistance in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 61, e01334-17 (2017).
Pym, A. S. et al. Regulation of catalase–peroxidase (KatG) expression, isoniazid sensitivity and virulence by furA of Mycobacterium tuberculosis. Mol. Microbiol. 40, 879–889 (2001).
Zahrt, T. C., Song, J., Siple, J. & Deretic, V. Mycobacterial FurA is a negative regulator of catalase–peroxidase gene katG. Mol. Microbiol. 39, 1174–1185 (2001).
Zhang, Y., Heym, B., Allen, B., Young, D. & Cole, S. The catalase–peroxidase gene and isoniazid resistance of Mycobacterium tuberculosis. Nature 358, 591–593 (1992).
Santangelo, M. P. et al. Negative transcriptional regulation of the mce3 operon in Mycobacterium tuberculosis. Microbiology 148, 2997–3006 (2002).
Santangelo, M. P. et al. Study of the role of Mce3R on the transcription of mce genes of Mycobacterium tuberculosis. BMC Microbiol. 8, 38 (2008).
De la Paz Santangelo, M. et al. Mce3R, a TetR-type transcriptional repressor, controls the expression of a regulon involved in lipid metabolism in Mycobacterium tuberculosis. Microbiology 155, 2245–2255 (2009).
Karakousis, P. C., Williams, E. P. & Bishai, W. R. Altered expression of isoniazid-regulated genes in drug-treated dormant Mycobacterium tuberculosis. J. Antimicrob. Chemother. 61, 323–331 (2008).
Vilcheze, C. et al. Enhanced respiration prevents drug tolerance and drug resistance in Mycobacterium tuberculosis. Proc. Natl Acad. Sci. USA 114, 4495–4500 (2017).
Schoutrop, E. L. M. et al. The stability of antimycobacterial drugs in media used for drug susceptibility testing. Diagn. Microbiol. Infect. Dis. 92, 305–308 (2018).
Rouse, D. A., DeVito, J. A., Li, Z., Byer, H. & Morris, S. L. Site-directed mutagenesis of the katG gene of Mycobacterium tuberculosis: effects on catalase–peroxidase activities and isoniazid resistance. Mol. Microbiol. 22, 583–592 (1996).
Liu, Y. et al. Immune activation of the host cell induces drug tolerance in Mycobacterium tuberculosis both in vitro and in vivo. J. Exp. Med. 213, 809–825 (2016).
Ma, S. et al. Integrated modeling of gene regulatory and metabolic networks in Mycobacterium tuberculosis. PLoS Comput. Biol. 11, e1004543 (2015).
Mawuenyega, K. G. et al. Mycobacterium tuberculosis functional network analysis by global subcellular protein profiling. Mol. Biol. Cell 16, 396–404 (2005).
Raimunda, D., Long, J. E., Padilla-Benavides, T., Sassetti, C. M. & Arguello, J. M. Differential roles for the Co2+/Ni2+ transporting ATPases, CtpD and CtpJ, in Mycobacterium tuberculosis virulence. Mol. Microbiol. 91, 185–197 (2014).
Lew, J. M., Kapopoulou, A., Jones, L. M. & Cole, S. T. TubercuList—10 years after. Tuberculosis (Edinb.) 91, 1–7 (2011).
Patel, S. J. et al. Fine-tuning of substrate affinity leads to alternative roles of Mycobacterium tuberculosis Fe2+-ATPases. J. Biol. Chem. 291, 11529–11539 (2016).
Bulatovic, V. M. et al. Oxidative stress increases susceptibility of Mycobacterium tuberculosis to isoniazid. Antimicrob. Agents Chemother. 46, 2765–2771 (2002).
Slayden, R. A. & Barry, C. E. 3rd. The genetics and biochemistry of isoniazid resistance in Mycobacterium tuberculosis. Microbes Infect. 2, 659–669 (2000).
Kohanski, M. A., Dwyer, D. J., Hayete, B., Lawrence, C. A. & Collins, J. J. A common mechanism of cellular death induced by bactericidal antibiotics. Cell 130, 797–810 (2007).
Hu, J., Zhao, L. & Yang, M. A GntR family transcription factor positively regulates mycobacterial isoniazid resistance by controlling the expression of a putative permease. BMC Microbiol. 15, 214 (2015).
Zhou, L., He, Z. G. & Li, W. AraR, an l-arabinose-responding transcription factor, negatively regulates resistance of Mycobacterium smegmatis to isoniazid. Biochem. (Mosc.) 84, 540–552 (2019).
Ehrt, S. et al. Controlling gene expression in mycobacteria with anhydrotetracycline and Tet repressor. Nucleic Acids Res. 33, e21 (2005).
Ehrt, S. & Schnappinger, D. Controlling gene expression in mycobacteria. Future Microbiol. 1, 177–184 (2006).
Guo, M. et al. Dissecting transcription regulatory pathways through a new bacterial one-hybrid reporter system. Genome Res. 19, 1301–1308 (2009).
Klotzsche, M., Ehrt, S. & Schnappinger, D. Improved tetracycline repressors for gene silencing in mycobacteria. Nucleic Acids Res. 37, 1778–1788 (2009).
BEI Resources (American Type Culture Collection, 2020); www.beiresources.org
Rock, J. M. et al. Programmable transcriptional repression in mycobacteria using an orthogonal CRISPR interference platform. Nat. Microbiol. 2, 16274 (2017).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 9, 357–359 (2012).
Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
Ma, S. et al. Transcriptomic signatures predict regulators of drug synergy and clinical regimen efficacy against tuberculosis. mBio 10, e02627-19 (2019).
Rustad, T. R., Harrell, M. I., Liao, R. & Sherman, D. R. The enduring hypoxic response of Mycobacterium tuberculosis. PLoS ONE 3, e1502 (2008).
Nandakumar, M., Prosser, G. A., De Carvalho, L. P. & Rhee, K. Metabolomics of Mycobacterium tuberculosis. Methods Mol. Biol. 1285, 105–115 (2015).
Garcia, B. J., Datta, G., Davidson, R. M. & Strong, M. MycoBASE: expanding the functional annotation coverage of mycobacterial genomes. BMC Genomics 16, 1102 (2015).
Mi, H. et al. PANTHER version 11: expanded annotation data from Gene Ontology and Reactome pathways, and data analysis tool enhancements. Nucleic Acids Res. 45, D183–D189 (2017).
Acknowledgements
We gratefully acknowledge J. Rock for kindly providing us with the pJR965 plasmid encoding a tetracyline-inducible dCas9 and kanamycin-selectable marker. We also thank J. Winkler, J. Lohmiller and R. Liao for technical assistance and S. Shen for helpful discussions. This work was supported by the National Institutes of Health (grant nos. U19 AI106761; U19 AI111276; U19 AI135976 and 5T32AI007509).
Author information
Authors and Affiliations
Contributions
S.M., T.R.R. and D.R.S. conceived of the study, led the design, generated data, analysed the results and drafted the manuscript. R.M. developed the software to convert raw sequencing data into abundance values for each TFI strain. S.J.H. generated data and assembled the pooled TFI library cultures. J.F.-J. assisted with sample preparation for sequencing. V.S. and K.Y.R. generated, analysed and interpreted the metabolite profiling data. A.F., N.F. and C.G. generated the CRISPRi strain.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
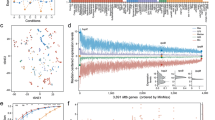
Extended Data Fig. 1 Comparing TFI pool growth between experimental conditions.
Number of doublings for TFI strain pool over duration of TRIP experiments in the untreated vs. INH treated conditions, estimated from the change of OD600 over the course of the experiment. Data show mean ± SD of four biological replicates from a representative experiment (three independent experiments were performed in total).
Extended Data Fig. 2 Chemical induction triggers mce3R expression change.
Expression fold change of mce3R relative to the housekeeping gene sigA, assessed by qPCR. Data show mean ± SD of 4 biological replicates from a representative experiment (two were performed in total). Conditions compared are in absence (white bars) and presence (black bars) of anhydrous-tetracycline (ATc) inducer, and presence and absence of INH exposure. Results show at least 8-fold activation of mce3R expression upon induction with ATc in both absence and presence of INH (p = 0.00035, two-sided t-test for -ATc untreated vs. +ATc untreated; p = 0.0036, two-sided t-test for -ATc + INH vs. +ATc + INH).
Extended Data Fig. 3 mce3Rind metabolic viability after 7 days INH.
Viability upon TFI induction (blue) is compared to uninduced (white), as measured by luminescence (see Methods). Data presented as mean Error bars show ± SD from four biological replicates. ** indicates significant differences between induction states (p = 8.3 x 10-6 comparing uninduced vs. TFI induced at 1.6 μM; p = 5.7 x 10-6 comparing uninduced vs. TFI induced at 1.8 μM; p = 1.3 x 10-3 comparing uninduced vs. TFI induced at 2.1 μM; p = 4.3 x 10-4 comparing uninduced vs. TFI induced at 2.4 μM; p = 7.6 x 10-3 comparing uninduced vs. TFI induced at 2.8 μM; p = 6.9 x 10-3 comparing uninduced vs. TFI induced at 3.2 μM; p = 4.6 x 10-4 comparing uninduced vs. TFI induced at 3.6 μM). Each p-value was calculated based on a two-sided t-test.
Extended Data Fig. 4 Overlap of genes regulated by mce3R that also modulate expression in baseline response to INH exposure.
a, Network diagram depicts the genes differentially expressed upon induction of mce3R expression (left), and upon exposure to INH (right). Three genes alter expression under both these conditions. b, Table summarizes the expression fold-changes of the genes perturbed both by mce3R induction and INH exposure.
Extended Data Fig. 5 Association between ctpD expression and INH sensitivity.
a, CFU/mL at 0 days and 7 days of H37Rv (black bar) and a ctpD CRISPRi-knockdown strain without (yellow) and with (red) chemical induction of CRISPRi activity. Both strains were exposed to 3.6 µM INH or no drug. There was no significant difference between the growth of strains without drug, and the average untreated CFU/mL is plotted in the gray bar. Data show mean ± SD of three biological replicates from two independent experiments (for H37Rv conditions) or one experiment (pJR965-ctpD conditions). There is a significant difference between the CRISPRi knockdown and wildtype strains (p = 0.00027 for Day 7 H37Rv + INH vs. Day 7 pJR965-ctpD – ATc + INH, Wilcoxon ranksum test with continuity correction; p = 0.00027 for Day 7 H37Rv + INH vs. Day 7 pJR965-ctpD + ATc + INH, Wilcoxon ranksum test with continuity correction; p = 0.0012 for Day 7 pJR965-ctpD – ATc + INH vs. Day 7 pJR965-ctpD + ATc + INH, Wilcoxon ranksum test with continuity correction). b, qPCR quantification of ctpD expression levels relative to the wildtype H37Rv in the CRISPRi knockdown strain with and without chemical induction of activity. The CRISPRi strain exhibited marked repression even in the absence of chemical induction. Data shown are from two biological replicates for the CRISPRi knockdown strain, uninduced and four biological replicates for the CRISPRi knockdown strain with induction. The experiment was performed once.
Extended Data Fig. 6 Comparing the effect of in vitro INH on mce3R and ctpD perturbation strains.
We measured the effect of mce3R induction in the CDC1551 strain background (blue) and in the ctpD::Himar1 strain background (orange) on Mtb survival in INH (3.6 μM), added on Day 0, as quantified by CFU/mL. Solid blue and orange lines indicate TFI induction and dashed blue and orange lines indicate TFI uninduced. As additional controls, we also compared survival of the CDC1551 wildtype strain (gray), as well as the ctpD::Himar1 strain (red). The data suggest that mce3R induction conveys significant additional fitness defect relative to ctpD::Himar1 strain at day 14 (p = 0.00058, two-sided t-test comparing ctpD::Himar1:: mce3Rind TFI induced vs. ctpD::Himar1; p = 0.0024, two-sided t-test comparing mce3Rind (CDC1551) TFI induced vs. CDC1551). There appears to be a modest (though not statistically significant) difference in the extent of INH-mediated killing at 7 days between the ctpD::Himar strain (red) and the ctpD::Himar1 strain with mce3R induction (orange solid) (p = 0.09, two-sided t-test). Data show mean ± SD of three biological replicates from one experiment.
Extended Data Fig. 7 Association between mce3R, ctpD expression and abundance of INH and INH-NAD adduct during drug exposure.
Relative abundance of INH and INH-NAD adduct in Mtb lysate (panels a, b, d, e, or supernatant (panels c, f) of strains exposed to 7.2μM INH for 24 hours. Panels a, b, and c show effect of ctpD transposon disruption and complementation with episomally ATc-inducible ctpD expression. Panels d, e, and f show the effect of mce3R induction with or without ctpD transposon disruption. ctpD disruption conveyed increased intracellular INH and INH-NAD levels and concomitant decreased levels of INH in the supernatant. Induction of mce3R also increases intracellular INH and INH-NAD levels, but does not convey additional accumulation increase in the ctpD transposon strain background. Bars plot mean ± SD for 3 biological replicates.
Supplementary information
Supplementary Tables
Supplementary Table 1: Detailed results of TRIP screens in the presence and absence of 3.6 µM INH. Tab 1 reports the mean log2[abundance fold change] for each TFI strain relative to no induction. Tab 2 reports the log2[RPM] values for each sample analysed for the study. Supplementary Table 2: Detailed regulon and accompanying Gene Ontology term enrichment information of transcription factors that convey altered fitness under different conditions. The Gene Ontology annotations are from ref. 52. Tab 1 provides information for transcription factors conveying the growth phenotype under log-phase growth conditions. Tab 2 provides information for transcription factors conveying the conditional resistance to INH (group A). Tab 3 provides information for transcription factors conveying the hypersusceptibility to INH but no growth defect in the absence of drug (group B). Tab 4 provides information for transcription factors conveying hypersusceptibility to INH and a growth defect in the absence of drug (group C). Tab 5 provides information for all transcription factors conveying hypersusceptibility to INH (groups B and C combined). The regulon information is based on data generated from refs. 13,14. The essentiality information is based on data generated from refs. 7,19. Supplementary Table 3: Overlap of TFI regulons with the INH growth phenotype and genes with the INH fitness phenotype in a Tn-seq assay measured by ref. 19. Supplementary Table 4: Correlation between ctpD regulation and INH response phenotype. Shown is a summary of the regulatory impact and TRIP abundance fold change upon INH exposure for the transcription factors that regulate ctpD. Note that Rv1990c and Rv0022c do not have TRIP values associated because the raw sequence data had poor detection of these TFI strains under all conditions. Expression fold-change values were assembled from ref. 14. Supplementary Table 5: Correlation between Rv0119 regulation and INH response phenotype. Shown is a summary of the regulatory impact and TRIP abundance fold change upon INH exposure for the transcription factors that regulate Rv0119, the other gene induced during basal INH exposure in H37Rv and repressed by mce3R.
Rights and permissions
About this article
Cite this article
Ma, S., Morrison, R., Hobbs, S.J. et al. Transcriptional regulator-induced phenotype screen reveals drug potentiators in Mycobacterium tuberculosis. Nat Microbiol 6, 44–50 (2021). https://doi.org/10.1038/s41564-020-00810-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-020-00810-x
This article is cited by
-
Expanding the search for small-molecule antibacterials by multidimensional profiling
Nature Chemical Biology (2022)
-
2021 in review
Nature Microbiology (2021)